Abstract
The association between the physician's first clinical impression of a patient with nonspecific complaints and morbidity and mortality is unknown. The aim was to evaluate the association of the physician's first clinical impression with acute morbidity and mortality.
We conducted a prospective observational study with a 30-day follow-up. This study was performed at the emergency departments (EDs) of 1 secondary and 1 tertiary care hospital, from May 2007 to February 2011. The first clinical impression (“looking ill”), expressed on a numerical rating scale from 0 to 100, age, sex, and the Charlson Comorbidity Index (CCI) were evaluated. The association was determined between these variables and acute morbidity and mortality, together with receiver operating characteristics, and validity.
Of 217,699 presentations to the ED, a total of 1278 adult nontrauma patients with nonspecific complaints were enrolled by a study team. No patient was lost to follow-up. A total of 84 (6.6%) patients died during follow-up, and 742 (58.0%) patients were classified as suffering from acute morbidity. The variable “looking ill” was significantly associated with mortality and morbidity (per 10 point increase, odds ratio 1.23, 95% confidence interval [CI] 1.12–1.34, P < 0.001, and odds ratio 1.19, 95% CI 1.14–1.24, P < 0.001, respectively). The combination of the variables “looking ill,” “age,” “male sex,” and “CCI” resulted in the best prediction of these outcomes (mortality: area under the curve [AUC] 0.77, 95% CI 0.72–0.82; morbidity: AUC 0.68, 95% CI 0.65–0.71).
The physician's first impression, with or without additional variables such as age, male sex, and CCI, was associated with morbidity and mortality. This might help in the decision to perform further diagnostic tests and to hospitalize ED patients.
INTRODUCTION
Nonspecific complaints are frequent reasons for emergency department (ED) presentations, and almost 20% of elderly nontrauma patients present to the ED with a generally impaired condition.1 Moreover, acute presentation of weakness is associated with a broad spectrum of underlying diseases, and with mortality.2–5 Because history-taking in patients with nonspecific complaints often fails to reveal information that clearly points toward a diagnosis,6 the physician's first clinical impression and heuristics might help in the initial assessment of these patients.7,8
The role of heuristics has been examined in nursing,9–11 but little is known about the role of the physician's heuristics in decision-making.12 Nevertheless, physicians have been advised against relying on judgments based on first impressions,13–16 even if they appear to rely on heuristic processes.17
To explore the association of the physician's first impression of patients with nonspecific complaints, with acute morbidity and mortality, we performed a prospective observational study with a 30-day follow-up. Moreover, we evaluated the role of the variables age and sex, and the Charlson Comorbidity Index (CCI), which is an easily determined measure used as a predictor of mortality in patients with a wide range of comorbidities.18
METHODS
Study Design
This study was conducted at the EDs of the University Hospital of Basel, Switzerland, and the University-affiliated Hospital of Liestal, Switzerland. University Hospital Basel is a 700-bed tertiary care facility, with about 46,000 patients presenting to its ED per year. Liestal Hospital is a 400-bed secondary care facility with about 20,000 ED presentations each year.
The local ethics committee (Ethikkommission beider Basel) approved the study protocol, and all participating patients signed an informed consent form.
A team of certified, experienced triage nurses screened patients for study inclusion using a reliable and internationally validated triage tool, the Emergency Severity Index (ESI). This 5-level triage algorithm allows clinically relevant stratification of patients presenting to EDs.
Level 1 patients require immediate lifesaving interventions, level 2 patients are in a high-risk situation, are lethargic, confused, or have severe pain, and levels 3, 4, and 5 patients need many, 1, or no resources, respectively.19 All adult (ie, ≥18 years of age) nontrauma patients were eligible for inclusion to the study, if they had an ESI score of 2 or 3 and vital signs within the normal range and presented in 1 of the 2 EDs between May 24, 2007, and February 8, 2011. Excluded were patients referred from other hospitals, patients with recently performed external laboratory examinations, patients with specific complains, patients with specific electrocardiogram changes, moribund patients, patients who needed surgery, and patients who did not sign the informed consent form. Eligible patients were enrolled by a study team.
Definitions
Nonspecific complaints were defined as complaints for which there were no evidence-based management protocols for emergency physicians, on the basis of which no initial diagnosis could be made after the first assessment, with various possible or potential interpretations, or with little discriminative power in establishing a diagnosis.4
Acute morbidity was defined as any condition that was potentially life-threatening; required swift intervention to prevent deterioration of the patient's current or future health status (ie, permanent disability or death), or resulted to death within 30 days of the initial ED presentation. This definition covered a comprehensive list of conditions, details of which have been published previously.4 The numbers for acute morbidity correspond to the presentation, as adjudicated by the experts. The CCI predicts the 10-year mortality of patients by adding scores assigned to various comorbidities, such as heart disease, AIDS, or cancer.
The total score per patient is a valid predictor of both 1- and 10-year mortality.18
Data Collection and Measurements
The study team consisted of physicians employed for the conduct of this study who were instructed on how to ensure comprehension on the side of the patients. At the outset of the physician–patient interaction and before history-taking and physical examination, the physician was asked by a member of the study team to evaluate the patient's overall clinical condition by answering the following question: “How ill does this patient look?” Physicians were instructed to give their responses on a numerical rating scale ranging from 0 to 100 points, such that a patient who appeared to be in excellent health would receive 0 points and a patient who looked extremely ill would receive 100 points. They were not informed that this first assessment would be used to predict the patients’ outcomes. Baseline characteristics of all included patients were retrieved from patient records.
Follow-up
For every included patient, 30-day follow-up data for morbidity and mortality were obtained from hospital discharge reports, or from their primary care physicians. Two experts in internal medicine, unaware of patients’ baseline data, evaluated all follow-up data and assigned a final primary diagnosis as well as a final secondary diagnosis and determined the presence of acute morbidity at time of ED presentation based on the 30-day follow-up. In cases of disagreement between the 2 experts, outcomes were reevaluated by an expert panel of 2 physicians, both certified in internal medicine and emergency medicine and with at least 10 years of clinical experience. They discussed the case until a consensus was reached. Diagnoses were classified according to the World Health Organization International Statistical Classification of Diseases and Related Health Problems, 10th Revision.
Statistical Analysis
Statistical analysis was performed by an independent biostatistician. We chose the variables “looking ill,” age, sex, and CCI to be included in multivariate logistic regression models because they are readily available at triage. Age, sex, and CCI have been proved to predict mortality in several populations, and “looking ill” was the main predictor to be validated. Validity was defined as the proportion of correct predictions of outcome that a variable makes out of all possible predictions. Validity thus represents the relative frequency with which a variable correctly predicts the outcome. We called a predictor valid if it was >0.5. A predictor with a high validity is useful only if it can also be employed frequently. Therefore, we also calculated the discrimination rate (DR), that is, the relative frequency with which the predictor discriminates between any 2 patients in our sample, thereby enabling a prediction. Age was dichotomized into a group of 65 years and older, and a group <65 years.
To define the association of independent variables (ie, “looking ill,” “age,” “male sex,” and “CCI”) with outcome measures (ie, acute morbidity and mortality), multivariable logistic regression models were performed. P values of <0.05 were considered to be significant. The effect of the variable “looking ill” was adjusted for all other variables in the model.
We analyzed the independent variable's performance by means of graphical displays, specifically by plotting P(specificity) against P(sensitivity). Used in signal-detection analyses, such displays show the receiver operating characteristics (ROC) of variables, and the [P(specificity), P(sensitivity)] space is referred to as the ROC space. On the basis of the graphical display of the ROC curves and the quantitative area under the curve (AUC), we then used the method of Delong et al20 to determine the association of 3 sets of variables with mortality and acute morbidity. These 3 sets of variables were looking ill; looking ill in combination with age and male sex; and looking ill, age, and male sex in combination with CCI.
We determined the prognostic ability of each variable, independently of the others, by computing its validity. Validity was defined as the proportion of correct predictions of outcome that a variable makes relative to all possible predictions. Validity thus represents the relative frequency with which a variable correctly predicts the outcome. We called a predictor valid if it was >0.5. As a predictor with a high validity is useful only if it can also be employed frequently, we also calculated the DR, that is, the relative frequency with which the predictor discriminates between any 2 patients in our sample, thereby enabling a prediction.
RESULTS
Of 217,699 presentations to the ED from May 24, 2007, through to February 2, 2011, 129,805 were not eligible because of age, dementia, trauma, referrals from other hospitals, external laboratory, in the process of dying, or urgent surgery. Two thousand one hundred eighty patients were not eligible because of lifesaving interventions. Thirty nine thousand two hundred eighty six were not eligible because of being fast tracked as ESI 4 or ESI 5. Thirty two thousand nine hundred sixty four were not screened because of the lack of study physicians during nights and weekends. Twelve thousand one hundred sixty two were not eligible because they presented with specific complaints. One thousand three hundred two were enrolled, and 2 patients did not give informed consent. Twenty-two patients had to be excluded for protocol violations, and 1240 of the included 1278 patients could be analyzed with complete data.
A total of 496 (38.8%) were male, and 782 (61.2%) were female. The median age was 81 years. Male patients were younger than female patients (median 79 vs 83 years). Table 1 shows the baseline characteristics of all included patients. Information about baseline characteristics and follow-up was available for all 1278 patients. A total of 84 (6.6%) patients died during follow-up, and 742 (58.0%) were classified as suffering from acute morbidity.
TABLE 1.
Baseline characteristics of included patients
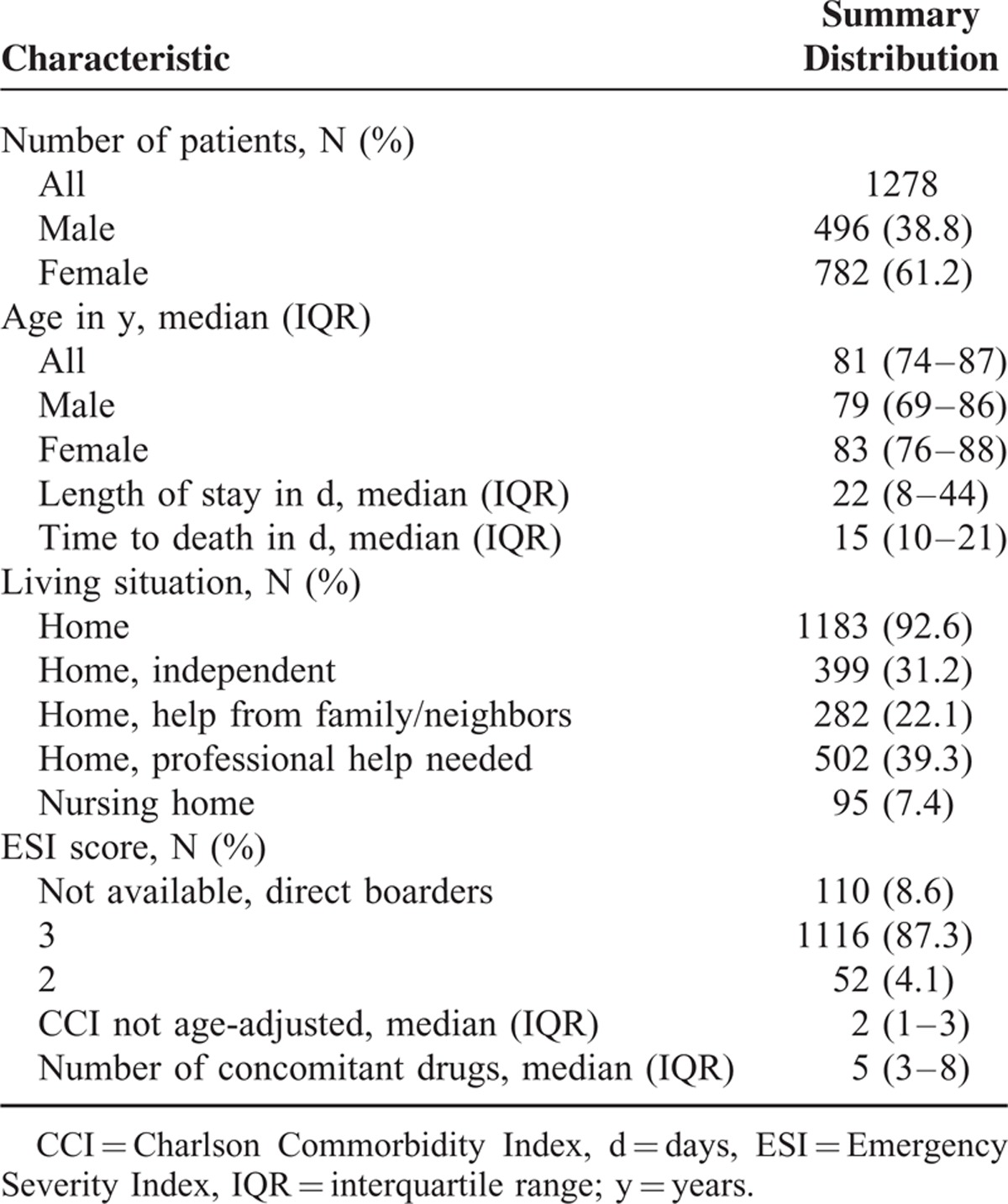
Of these patients, 147 suffered from a metabolic disorder (eg, electrolyte disorder, anemia, intoxication, drug side effects, ketoacidosis, thyroid dysfunction, or cortisol deficiency), 97 from pneumonia, 83 from heart failure, 70 from urinary tract infection, 56 from acute renal failure, 53 from cancer, 44 from dehydration, 39 from an abdominal disorder (eg, gastrointestinal bleeding, pancreatitis, cholecystitis, cholangitis, liver failure, or colitis), 32 from other infections (eg, endocarditis, skin infection, or sepsis without a defined focus), 36 from a neurological disease (eg, epileptic seizure, Parkinson disease, or Wernicke encephalopathy), 34 from stroke (ie, ischemic or intracranial bleeding), 20 from acute myocardial infarction, and 31 from other disorders (eg, pulmonary embolism, pleural effusion, osteoporotic fracture, or rheumatological disease).
First Clinical Impression as Predictor of Outcome
In total, 110 physicians gave their first clinical impression in 1240 patients. On average, each physician judged 11 patients. The average age of the 20 participating senior physicians was 38.4 (±4.7 years). They had an average experience of 13.2 (+4.2 years). The average age of the 90 junior physicians was 28.6 (+2.6 years). They had an average experience of 3.3 (+1.5 years). In logistic regression analyses, the physicians’ first clinical impression (variable “looking ill,” data available in 1240 of 1278 (97%) patients), was significantly associated with mortality and acute morbidity (Odd ratio 1.23, 95% CI 1.12–1.34, P < 0.001, and 1.19, 95% CI 1.14–1.24, P < 0.001, respectively, per 10 point increase on the scale from 0 to 100).
For “looking ill,” the median (interquartile range [IQR]) was 60 (30–80). The optimal sensitivity for acute morbidity was 0.63 (95% CI 0.60–0.66), whereas the optimal specificity was 0.60 (95% CI 0.56–0.65). The optimal sensitivity for mortality was 0.54 (95% CI 0.44–0.65), whereas the optimal specificity was 0.70 (95% CI 0.67–0.73). The external validation of this novel parameter, performed in another population (all-comers) also showed a good linear relationship with morbidity (ρ = 0.97, n = 1196) and a fair median predictability for morbidity (AUC = 0.72, IQR 0.70–0.73) as well as a good interrater reliability between physicians and nurses (intra class correlation = 0.49) (Rohacek et al, accepted for publication in The International Journal of Clinical Practice, Dezember 2014). Moreover, the variables “age,” “male sex,” and “CCI” (data available in all patients) were also significantly associated with these outcomes (Table 2).
TABLE 2.
P Values, ORs, and 95% CI of the 4 Predictors of Mortality and Acute Morbidity
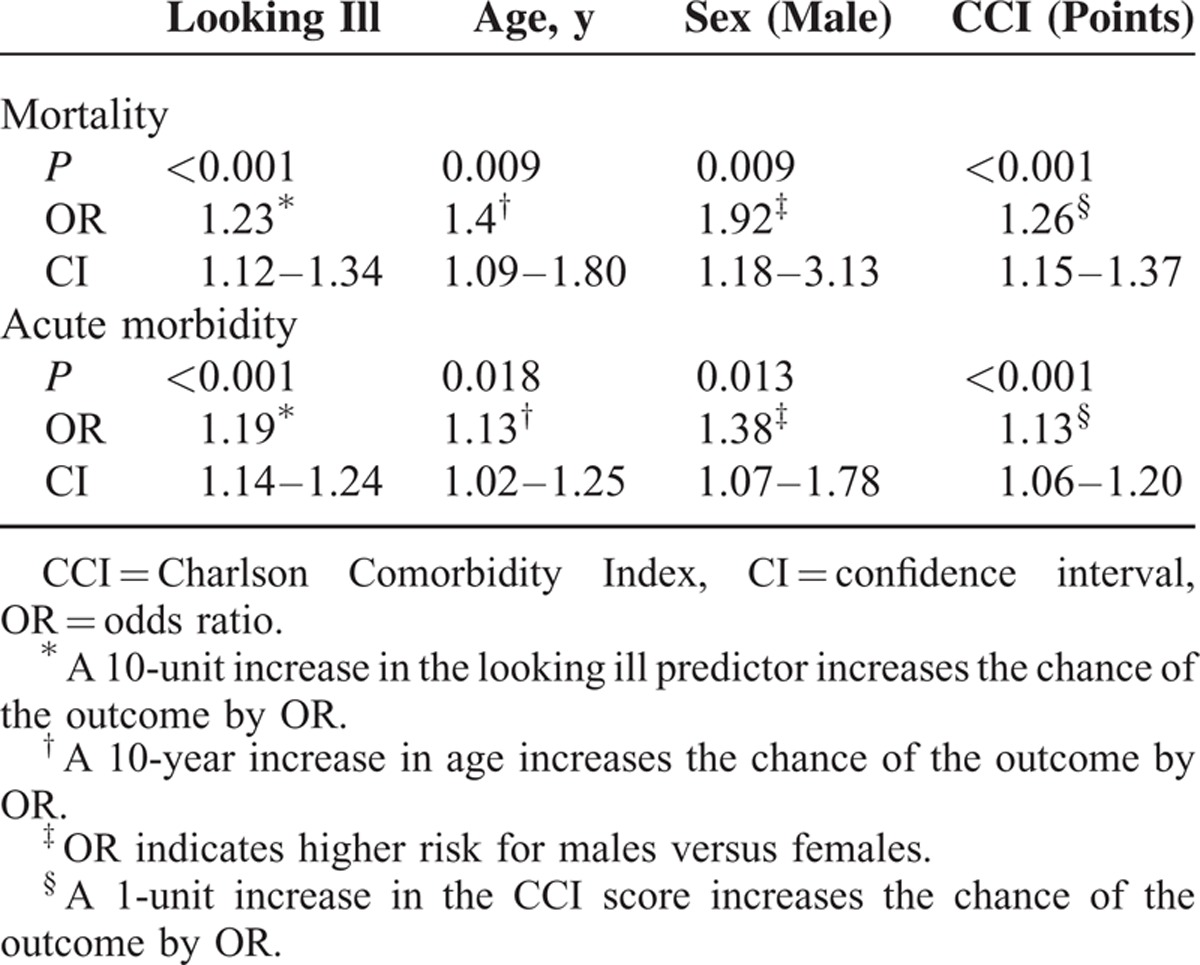
Figure 1 shows the proportions of patients with acute morbidity and mortality, dependent on scale parameters of the variable “looking ill.”
FIGURE 1.
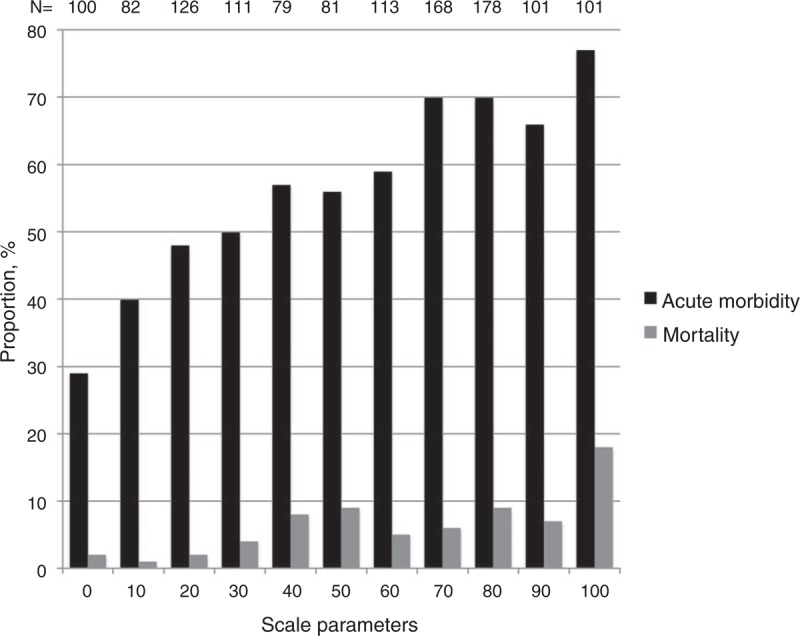
The Proportions of patients with acute morbidity and mortality dependent on the variable “looking ill” from a scale from 0 to 100. Data for the variable “looking ill” was available in 1240 of 1278 (97%) patients.
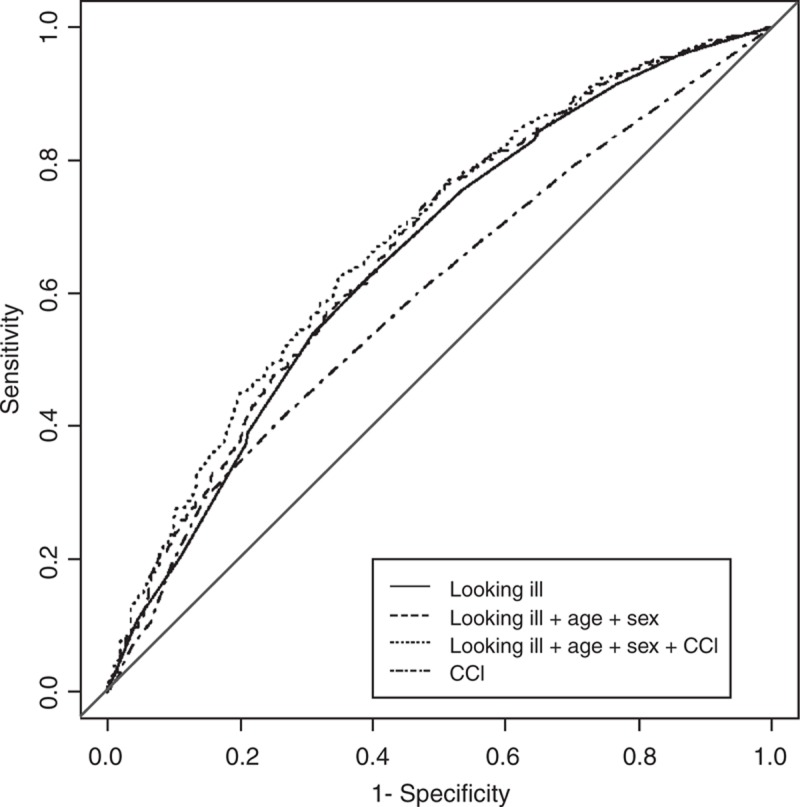
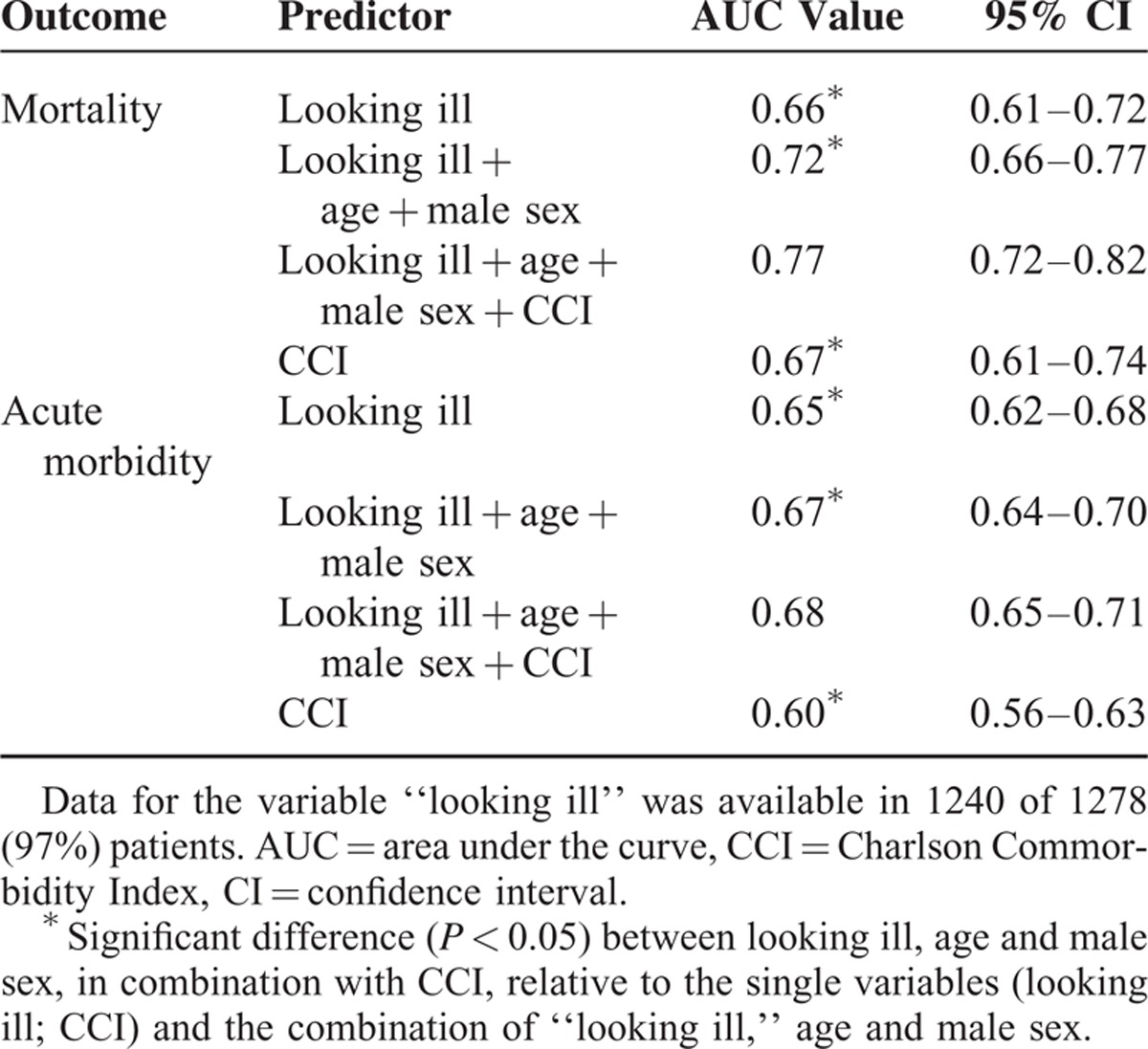
We calculated ROC curves and AUC values, both of which are based on the corresponding logistic regression models, for the 2 outcome measures. Figure 2 shows the ROC curves for mortality based on the variable “looking ill,” “looking ill” in combination with age and male sex, and “looking ill,” age and male sex, in combination with CCI. Figure 3 shows the ROC curves for acute morbidity. Table 3 lists the mean AUC values (with 95% CI) associated with the 3 sets of variables and with CCI alone. According to the AUC values, “looking ill,” age and male sex, in combination with CCI, yielded the best performance on both outcome variables. Using the Delong method to compare AUCs, we found that the performance levels of the 3 sets of variables were significantly different from one another at the 5% α level, with the “looking ill,” age and male sex, in combination with CCI, predicting the outcomes significantly better than the other 2 variable sets or CCI alone.
FIGURE 2.
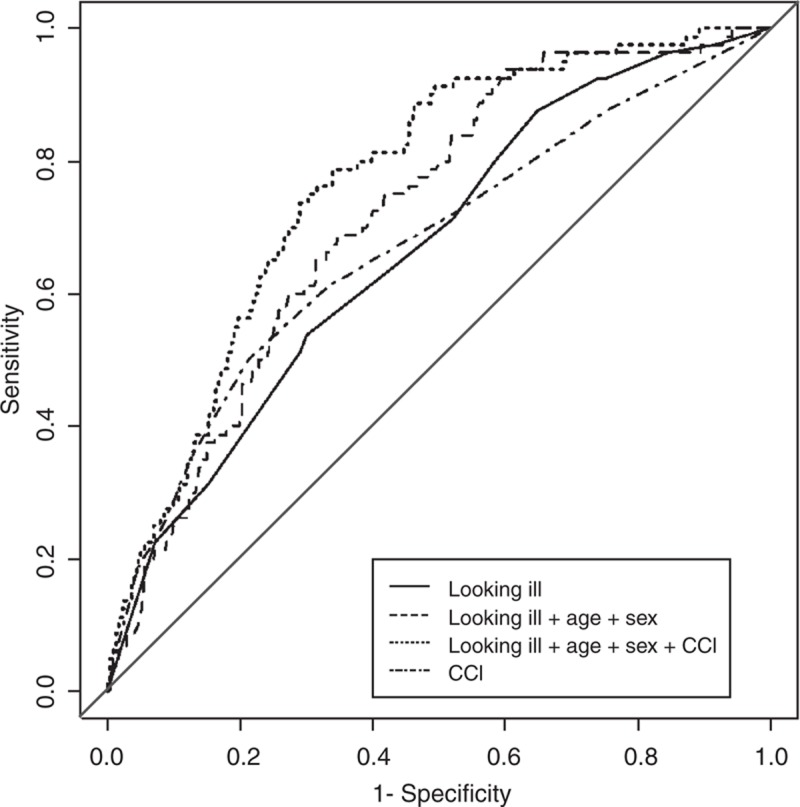
The performance of 2 single variables (looking ill and CCI) and 2 sets of predictors (looking ill, age and male sex, in combination with or without CCI) in the ROC space for the outcome variable mortality. CCI = Charlson Comorbidity Index, ROC = receiver operating characteristic.
FIGURE 3.
The performance of 2 single variables (looking ill and CCI) and 2 sets of predictors (looking ill, age and male sex, in combination with or without CCI) in the ROC space for the outcome variable acute morbidity. CCI = Charlson Commorbidity Index, ROC = receiver operating characteristic.
TABLE 3.
Mean AUC Values for the 2 Outcomes
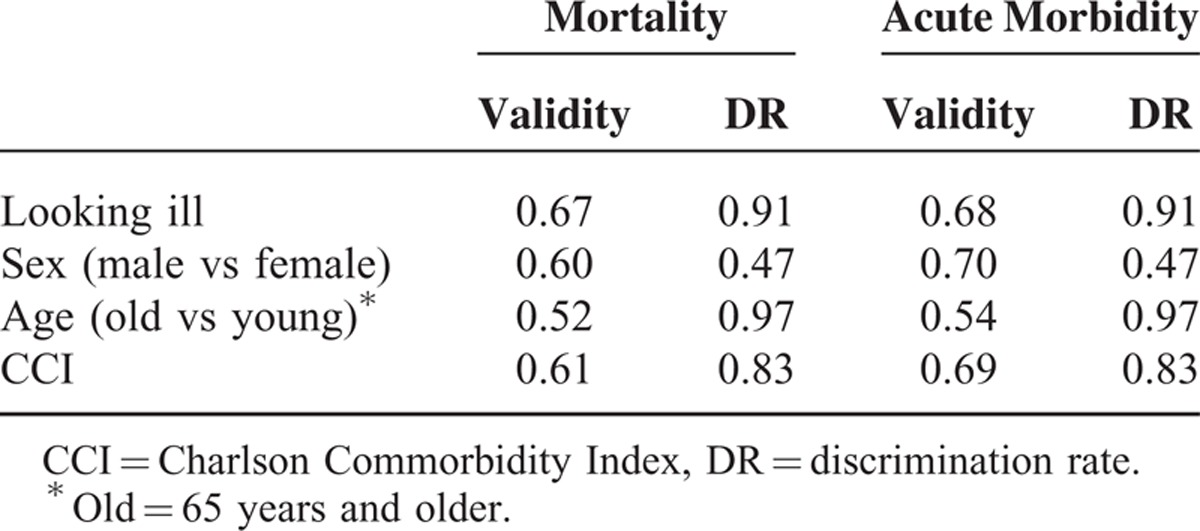
Finally, we determined the validities of the variables and DRs (Table 4). In predicting mortality, the variable “looking ill” proved to have highest validity, followed by “CCI.” In contrast, “age” had little predictive power. Interestingly, the variable “looking ill” discriminated in 91% of the complete set of 816,003 pair comparisons, whereas “CCI” discriminated in 83% of comparisons. In predicting acute morbidity, 3 of the 4 variables—namely, “looking ill,” “male sex,” and “CCI”—proved to be nearly equally valid, whereas age alone had low validity.
TABLE 4.
Validities and DRs for Mortality and Acute Morbidity
DISCUSSION
In this prospective study including a 30-day follow-up, we found that the physician's first clinical impression was associated with acute morbidity and mortality in elderly patients with nonspecific complains presenting to the ED. The combination of “looking ill,” with age, male sex, and the CCI resulted in the best prediction of these outcomes. Physicians appear to rely on heuristic processes in the context of their mental library of clinical signs and complaints, with pattern recognition being the most common process.17 In emergency situations time is essential, and the use of pattern recognition and other nonanalytical processes is likely to be important. However, in patients with non-specific complaints, the success of pattern recognition may be hampered because key predictors may initially be ignored due to their apparent insignificance. Because it is difficult to foresee which combination of cues will provide a path to the correct diagnosis in these patients, diagnostic accuracy may suffer.6 Thus, readily available information such as “looking ill,” age, and male sex, might help during the initial assessment of such patients.
To the best of our knowledge, this is the first prospective study to investigate the use of the physician's first clinical impressions to predict outcomes in patients with nonspecific complaints in the ED. However, similar work has been performed in different settings. One study noted that the patient's facial expression, handshake, and entry into the consultation room can convey information indicative of outcomes such as mortality.21 One study showed that conversational dynamics during the first 5 minutes of a negotiation could predict negotiated outcomes.22 Finally, a recent prospective study showed that nurses and physicians in a medical admission unit could accurately predict mortality of acutely admitted patients upon the patient's arrival.23
Although these studies were performed in other circumstances and with other subjects, an association between received visual information of subjects and different outcomes could be shown, as in our study. This underscores the relevance of our findings.
Our study had several limitations. First, over a hundred different physicians took part in the initial clinical assessments of patients. We did not correlate characteristics of the participating physicians with outcome prediction. Thus, the effect of physician-dependent factors such as sex, function, or experience, could not be included in the analysis. However, external validity may be enhanced by the fact that there was a wide distribution of age and experience, and a low number of judgments by the individual physicians, minimizing a “learning bias.”
Second, information reported by paramedics, such as comorbidities and previous hospitalizations, or information about vital parameters, might have influenced the physician's first clinical impression, and could have interfered with the physician's rating of the first impression. However, our study physicians were instructed to record the first impression at the earliest time point possible.
Third, we did not perform an interrater reliability testing, and the scoring system was not validated at the time the study was conducted. However, validity and reliability was tested in an all-comer cohort and proved to be useful. Fourth, the number of not included patients who were potentially eligible was not assessed due to the availability of study physicians on weekdays only. Thus, the dimension of a possible selection bias could not be determined. Finally, this study was performed in EDs, and most patients were elderly.
Thus, generalization of our findings to other settings might not be adequate. In conclusion, we found that physicians’ first clinical impression may help to predict morbidity and mortality of elderly patients presenting with nonspecific complaints to the ED. This might help in the decision to perform further diagnostic tests or to hospitalize ED patients.
Acknowledgments
We thank dipl. Math. Andy Schötzau, EUDOX, Basel, Switzerland, for performing statistical analysis, and Dr Rodney Yeates for language editing. A. Schötzau and R. Yeates received wages for their contributions.
Footnotes
RB had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The hypothesis of this study arouse before the beginning of the collection of the data. The study protocol was written before the beginning of the collection of the data.
No author received support from any organization for the submitted work; there was no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; there was no other relationships or activities that could appear to have influenced the submitted work.
Sponsor of this study was the Swiss National Science Foundation. The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Vanpee D, Swine C, Vandenbossche P, et al. Epidemiological profile of geriatric patients admitted to the emergency department of a university hospital localized in a rural area. Eur J Emerg Med 2001; 8:301–304. [DOI] [PubMed] [Google Scholar]
- 2.Safwenberg U, Terent A, Lind L. The Emergency department presenting complaint as predictor of in-hospital fatality. Eur J Emerg Med 2007; 14:324–331. [DOI] [PubMed] [Google Scholar]
- 3.Nickel CH, Nemec M, Bingisser R. Weakness as presenting symptom in the emergency department. Swiss Med Wkly 2009; 139:271–272. [DOI] [PubMed] [Google Scholar]
- 4.Nemec M, Koller MT, Nickel CH, et al. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med 2010; 17:284–292. [DOI] [PubMed] [Google Scholar]
- 5.Nickel CH, Ruedinger J, Misch F, et al. Copeptin and peroxiredoxin-4 independently predict mortality in patients with nonspecific complaints presenting to the emergency department. Acad Emerg Med 2011; 18:851–859. [DOI] [PubMed] [Google Scholar]
- 6.Hertwig R, Meier N, Nickel C, et al. Correlates of diagnostic accuracy in patients with nonspecific complaints. Med Decis Making 2013; 33:533–543. [DOI] [PubMed] [Google Scholar]
- 7.Balla J, Heneghan C, Thompson M, et al. Clinical decision making in a high-risk primary care environment: a qualitative study in the UK. BMJ open 2012; 2:e000414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stolper E, van Bokhoven M, Houben P, et al. The diagnostic role of gut feelings in general practice. A focus group study of the concept and its determinants. BMC Fam Pract 2009; 10:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rew L, Barrow EM., Jr State of the science: intuition in nursing, a generation of studying the phenomenon. ANS. Adv Nurs Sci 2007; 30:E15–E25. [DOI] [PubMed] [Google Scholar]
- 10.McCutcheon HHI, Pincombe J. Intuition: an important tool in the practice of nursing. J Adv Nurs 2001; 35:342–348. [DOI] [PubMed] [Google Scholar]
- 11.Edwards B. Walking in—initial visualisation and assessment at triage. Accid Emerg Nurs 2007; 15:73–78. [DOI] [PubMed] [Google Scholar]
- 12.Greenhalgh T. Intuition and evidence—uneasy bedfellows? Br J Gen Pract 2002; 52:395–400. [PMC free article] [PubMed] [Google Scholar]
- 13.Hall KH. Reviewing intuitive decision-making and uncertainty: the implications for medical education. Med Educ 2002; 36:216–224. [DOI] [PubMed] [Google Scholar]
- 14.Croskerry P. Critical thinking and decisionmaking: avoiding the perils of thin-slicing. Ann Emerg Med 2006; 48:720–722. [DOI] [PubMed] [Google Scholar]
- 15.Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med 2003; 78:775–780. [DOI] [PubMed] [Google Scholar]
- 16.Klein JG. Five pitfalls in decisions about diagnosis and prescribing. Br Med J 2005; 330:781–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andre M, Anden A, Borgquist L, et al. GPs’ decision-making—perceiving the patient as a person or a disease. BMC Fam Pract 2012; 13:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40:373–383. [DOI] [PubMed] [Google Scholar]
- 19.Grossmann FF, Nickel CH, Christ M, et al. Transporting clinical tools to new settings: cultural adaptation and validation of the Emergency Severity Index in German. Ann Emerg Med 2011; 57:257–264. [DOI] [PubMed] [Google Scholar]
- 20.Delong ER, Delong DM, Clarkepearson DI. Comparing the areas under 2 or more correlated receiver operating characteristic curves—a nonparametric approach. Biometrics 1988; 44:837–845. [PubMed] [Google Scholar]
- 21.Thomas JL. The causes of acute abdominal pain in the healthy exclusive of traumatism. Br Med J 1903; 1903:186–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curhan JR, Pentland A. Thin slices of negotiation: predicting outcomes from conversational dynamics within the first 5 minutes. J Appl Psychol 2007; 92:802–811. [DOI] [PubMed] [Google Scholar]
- 23.Brabrand M, Hallas J, Knudsen T. Nurses and physicians in a medical admission unit can accurately predict mortality of acutely admitted patients: a prospective cohort study. PLoS One 2014; 9:e101739. [DOI] [PMC free article] [PubMed] [Google Scholar]


