Abstract
To investigate the associations between dementia, the use of long-term care (LTC) services, and the deterioration of care-needs levels of elderly persons in Japan.
Using a retrospective cohort study, we analyzed 50,268 insurance beneficiaries aged 65 years and older who had utilized LTC services between 2010 and 2011 in Kyoto prefecture, Japan. Logistic regression analyses were used to identify predictors of care-needs level deterioration.
Dementia, facility care services, the male sex, older age, and lower baseline care-needs levels were associated with care-needs level deterioration. The disparity between odds ratios of home care services, dementia diagnoses, and facility care services on care-needs level deterioration diminished with increasing baseline care-needs levels. The other risk factors of care-needs level deterioration showed stronger associations as care-needs levels and age increased.
The effects of baseline care-needs levels and dementia should be considered when developing LTC policies.
INTRODUCTION
Japan's long life expectancy1 has resulted in the emerging need for effective and efficient long-term care (LTC). In 2000, long-term care insurance (LTCI) Act was implemented for citizens above 65 years of age, as well as for citizens above 40 years of age deemed to require LTC services.
Eligibility for the LTCI Act is determined by municipalities, and is categorized into 7 distinct levels: these levels are designated support levels 1 to 2 and care-needs levels 1 to 5. The Act is provided by the Health and Welfare Bureau for the Elderly.2 Under this Act, individuals who are able to live almost completely independently are classified as support levels 1 or 2. In contrast, insured individuals who have difficulties in living independently are classified as care-needs levels 1 to 5, with the higher care-needs levels indicating greater deterioration of health and higher requirements for care.
Surveys conducted by the Japanese Health and Social Statistics Division, Statistics and Information Department3–5 have shown that there was a rapid increase in the demand for LTC services in older individuals with dementia from 2004 to 2010. As dementia has been identified as the strongest independent predictor of medical and LTC utilization and expenditure among older individuals,6,7 recent years have seen a rise in studies addressing its risk factors. Age, sex, smoking and alcohol consumption habits, body functions, cerebrovascular disease, and other factors have demonstrated associations with dementia incidence.8–11 In addition, dementia severity and the rate of deterioration have been shown to significantly influence the rates of institutionalization, disability, and death.12,13
The primary goal of LTCI is to maintain each beneficiary's independence in daily life and to obviate further deterioration of their conditions. The Japanese government implemented reforms to the LTCI Act to create a community-based, prevention-oriented long-term care system in 2005.14 Baseline care-needs levels, respite stays in nursing homes, medical plans by physicians, living with spouse, use of home help/bathing services, day care services, short stays, and age have been identified as factors associated with care-needs level changes.15–19
The correlation between dementia and the deterioration of LTC service users is still unclear. It is therefore necessary to investigate this association to prevent further deterioration of LTC care-needs levels in insured elderly people with dementia. However, most of the existing studies have focused on the risk factors of incident dementia.
Therefore, the objective of this study was to investigate the possible effects of dementia and use of LTC care services on the deterioration of care-needs levels of elderly persons in Japan.
METHODS
We conducted a retrospective cohort study, and analyzed 50,268 insurance beneficiaries aged 65 years and older who had utilized LTC services between 2010 and 2011 in Kyoto prefecture, Japan. Logistic regression analyses were used to identify predictors of care-needs level deterioration. This study was approved by the Ethics Committee of Kyoto University Graduate School of Medicine (Number E1023).
Subjects
All subjects were selected from LTCI beneficiaries aged 65 years and above who had utilized LTC services in June 2010 in Kyoto prefecture, Japan.
Subjects were excluded from analysis if they had fulfilled any of the following criteria: first, subjects classified as support levels 1 and 2 were excluded from analysis. Next, subjects who had not utilized LTC services in June 2011 and had been classified as care needs level 5 in June 2010 were also excluded, unless their death (deterioration) could be determined from the data. The deteriorating conditions could not be identified in care-needs level 5 unless the subjects were beneficiaries of National Healthcare Insurance, in which case we were able to identify if the patients had died. Furthermore, as diagnoses of dementia were identified using the relevant International Classification of Disease (ICD)-10 codes available in the National Healthcare Insurance Database and Old-Old Adults Medical Care Program Database (hereinafter, the 2 databases are collectively referred to as the “NHIDB”), service users who were not beneficiaries of National Healthcare Insurance were excluded from analysis. Also, people younger than 65 years were excluded. After employing these exclusion criteria, the study sample for analysis comprised 50,268 subjects, as shown in Figure 1.
FIGURE 1.
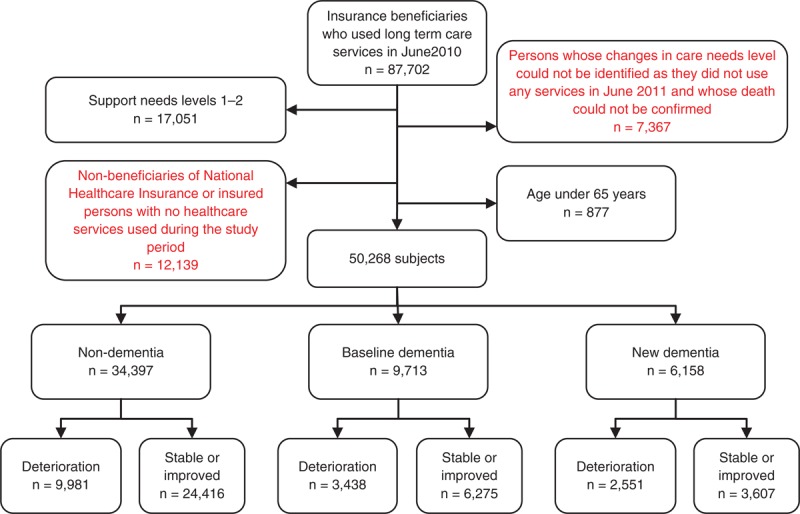
Subject selection. Flowchart detailing subject selection, the study sample for analysis comprised 50,268 subjects.
Dependent Variable
The care-needs levels within the LTCI system are determined by each municipality in Kyoto. The respective LTC approval boards investigate the mental and physical condition of each insured individual and make judgments based on preliminary screenings and physician diagnoses. For this study, changes in care-needs levels were divided into 2 categories: stable or improved and deteriorated. The care-needs levels for long-term care services were categorized into the following 7 levels: support needs levels 1 and 2, and care needs levels 1 to 5. Higher care-needs levels indicate more severe conditions that require greater levels of care. Using data from 2 time points (June 2010 and June 2011), changes in care-needs levels for each patient were calculated by subtracting the baseline care-needs level in June 2010 from the care-needs level in June 2011. If the numerical difference was negative or equal to 0, the care-needs level was designated as stable or improved; a positive difference indicated a deteriorated care-needs level. In addition, individuals who had died before June 2011 were also designated as having deteriorated care-needs levels.
The deterioration in care-needs level was utilized as the dependent variable in the statistical analysis.
Independent Variables
Sex, age (65–74, 75–84, 85–94, >95 years), baseline care-needs level, the type of LTC service used, and diagnosis of dementia were used as independent variables.
We collected service use data from June 2010 to May 2011. As recommended by the Ministry of Health, Labor, and Welfare, Japan, we categorized services into 3 main types according to their service characteristics. First, as individuals who use facility care services would not use the other types of services at the same time, individuals who had used facility care services during the observation period were classified as users of facility care services. Next, since home care services comprised the largest proportion of services used by individuals, and community-based care services had been established relatively recently in 2006 and were therefore not as widespread as home care services in our study region, we classified individuals as users of home care services if they had used these services during the observation period. Finally, all other individuals were classified as users of community-based care and other care services.
With regard to the identification of dementia cases, subjects were categorized into 3 distinct categories: non-dementia (individuals who had no diagnosis of dementia during the observation period); baseline dementia (individuals with dementia diagnoses at the baseline); and new dementia (individuals who were not dementia patients at baseline, but received a diagnosis of dementia during the observation period).
Statistical Analysis
We first conducted a descriptive analysis of the total study sample and of the subgroups according to change in care-needs levels. This descriptive analysis included age, sex, baseline care-needs level, dementia status, and type of LTC service used. Chi-square tests were used to compare the variables (including sex, age, baseline care-needs level, type of service use, and dementia diagnoses) between the deteriorated and stable or improved groups (Table 1). All these variables were also included as independent variables in the multivariable binary logistic regression.
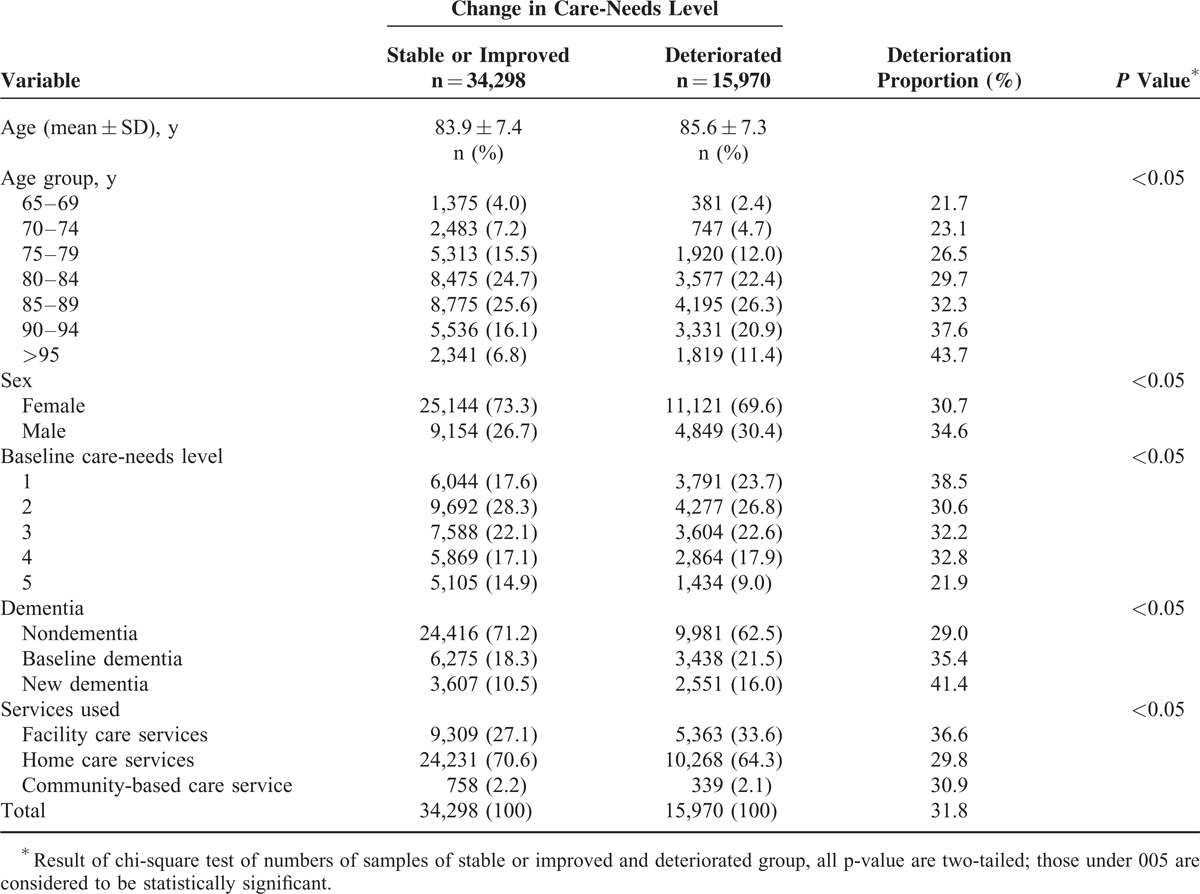
TABLE 1.
Demographic Characteristics of All Subjects According to Changes in Care-needs Levels Between 2010 and 2011
The multivariable logistic regression analyses were conducted for each of the subgroups of different baseline care-needs levels. C-statistics were calculated to indicate goodness-of-fit. Statistical significance was set at P ≤ 0.05. IBM SPSS 20.0J for Windows (SPSS Japan Inc., Tokyo, Japan) was used for all statistical analyses.
RESULTS
Demographic Characteristics
The characteristics of the study subjects are shown in Table 1.
The mean age of the group that showed deterioration in care-needs levels was higher than that of the group that showed stable or improved care-needs levels.
The deterioration proportion refers to the proportion of cases who demonstrated deterioration in care-needs levels among all cases within a specific subgroup. In higher age groups, the proportions of deteriorated cases were observed to increase. In contrast, the proportions of deteriorated cases decreased with increasing care-needs levels. Cases with new diagnoses of dementia demonstrated the highest deterioration proportion (41.4%) when compared with the other 2 dementia groups. Baseline dementia patients showed a higher deterioration proportion (35.4%) than nondementia cases (29.0%).
For the service type categories, individuals who used facility care services had a higher deterioration proportion (35.6%) than the other service groups. The deterioration proportions of cases using home care services and community-based care services were similar at approximately 30%. Overall, the deterioration proportion was 31.8%.
Multivariable Logistic Regression of Care-needs level Deterioration
Table 2 shows the results of a multivariable logistic regression analysis using care needs level deterioration as the dependent variable; age, sex, baseline care needs level, dementia status, and type of services used were the independent variables.
TABLE 2.
Results of Logistic Regression Analysis of Care-needs level Deterioration in all Subjects
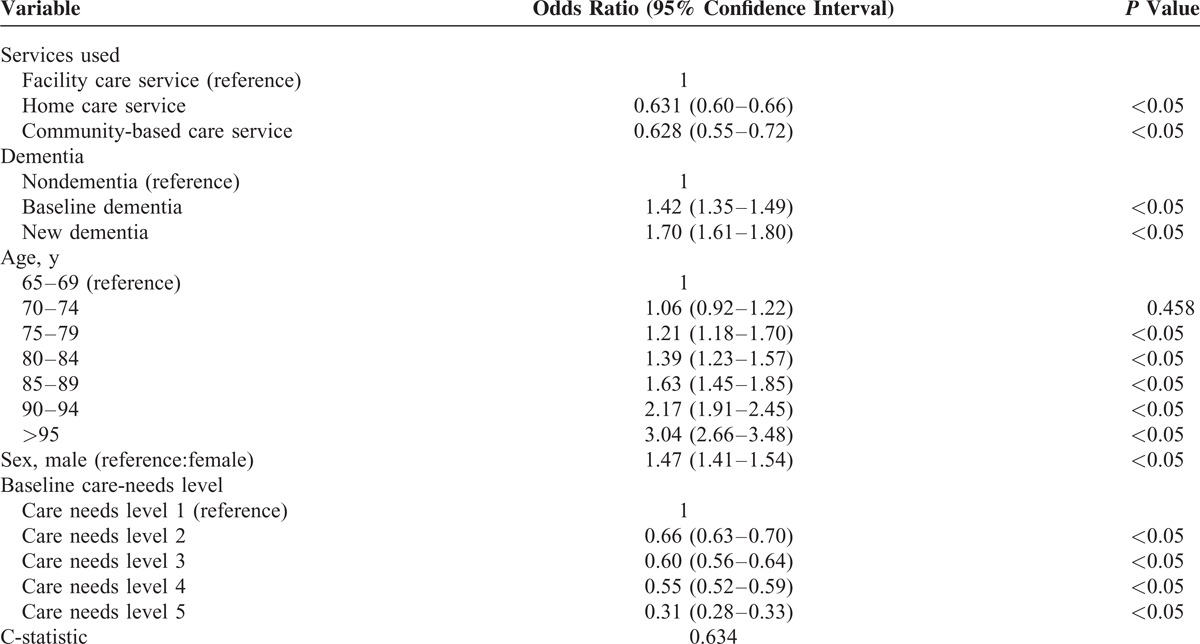
The analysis showed that the factors associated with the deterioration of care-needs levels were the male sex (odds ratio [OR] = 1.47), older age, and lower baseline care-needs level. With regard to the types of LTC services used, facility care services were associated with higher deterioration than other types of services (community-based care services: OR = 0.628; home care services: OR = 0.631). Moreover, New dementia cases (OR = 1.70) and baseline dementia cases (OR = 1.42) had higher risks of care-needs level deterioration than nondementia cases.
Multivariable Logistic Regression of Care-needs level Deterioration by Baseline Care-needs Level Subgroups
Table 3 shows the results of the multivariable logistic regression analyses conducted to clarify the predictors of care-needs level deterioration according to baseline care needs level.
TABLE 3.
Results of Logistic Regression Analysis of Care-needs level deterioration by Baseline Care-needs Level
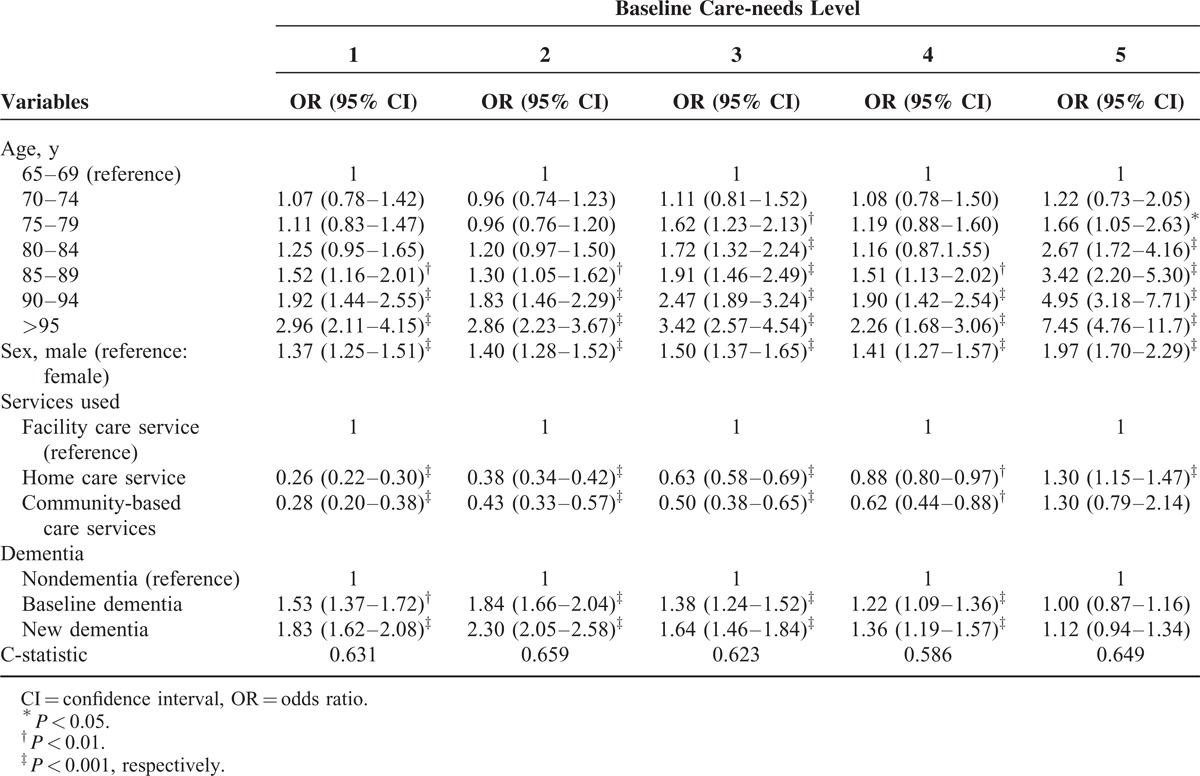
Similar results were observed in the various regression models for each baseline care needs level used to analyze the associations between dementia diagnosis and care-needs level deterioration. The ORs for the various predictors were observed to decrease as care-needs level increased. Factors associated with deterioration among baseline care needs levels 1 to 4 were the male sex, older age, dementia diagnosis, and facility care services use. For care-needs level 5, only the male sex, older age, and home care services use were associated with care-needs level deterioration. Dementia diagnosis showed no association with care-needs level deterioration in baseline care-needs level 5.
Although facility care services demonstrated the highest OR for care-needs level deterioration (relative to the other 2 types of services) among cases certified at care-needs levels 1 to 4, the ORs of both home care services and community-based care services increased together with the baseline care needs levels. The lower the care-needs level, the higher the risk of deterioration was for facility care services use; however, the disparity between facility care services and home care services diminished as care-needs levels increased.
Age was inconsistently associated with care-needs level deterioration. The 70 to 74 years’ age group was not significant for all subjects and for the various baseline care-needs levels, the 75 to 79 years’ age group was only significant in care-needs level 3, and the 80 to 84 years’ age group was only significant in care-needs levels 3 and 5. However, ages above 85 years were significant at all baseline care-needs levels. Furthermore, the ORs of age groups above 85 years and the male sex were the highest in care-needs level 5, followed by care-needs level 3.
DISCUSSION
This study investigated how dementia diagnosis and type of LTC service use can influence care-needs level deterioration. We focused our analysis on National Health Insurance beneficiaries who had utilized LTC services between June 2010 and May 2011 in Kyoto prefecture, Japan.
Our findings showed that LTC service users with new or baseline diagnoses of dementia were strongly associated with care-needs level deterioration; in particular, new dementia cases showed a high OR (1.70) of deterioration of care-needs level relative to nondementia cases. This risk was observed to decrease as the baseline care-needs level increased. Because the main symptom of dementia is disruptive behavior or behavioral disorder,20 cases with care-needs level 5 are frequently bedridden with limited ability for independent activity. This may explain the lack of significant association between dementia and deterioration at care-needs level 5.
Moreover, the disparity between ORs of new dementia (OR = 1.70) and baseline dementia (OR = 1.42) cases was small. Although the causes of dementia can vary, all of them could affect memory, cognition, and the ability to perform instrumental activities of daily living (ADL).21 As such, the distinction between types of dementia is blurred, which may have resulted in the small differences in ORs between baseline dementia and new dementia cases.
Previous studies have tended to focus on baseline dementia. Sauvaget et al11 reported that dementia patients had significantly greater reductions in ADL and instrumental ADL (IADL) scores when compared with non-dementia patients. As the criteria for determining care-needs level include ADL and IADL components in Japan, it is unsurprising that the decline of both ADL and IADL is strongly associated with care-needs level deterioration. Furthermore, our results are consistent with previous studies that report dementia as a significant factor in predicting physical function decline or institutionalization among nursing home residents or in general populations.11,12,22,23
Because of the lack of a significant association between dementia and deterioration at baseline care-needs level 5 (as well as the strong associations in lower care needs levels), we suggest that policymakers should place an emphasis on monitoring beneficiaries suffering from dementia, which may result in the further deterioration of their care-needs level. The LTC service providers need to be aware of the detailed symptoms of their service users who may have dementia to prevent further worsening of their conditions. In this way, there is an important role for LTC service providers to strategically develop and manage appropriative care plans for service users to prevent premature deterioration.
Olivares-Tirado et al17 investigated the predictors of LTC expenditures, and observed that a decline in functional status and use of facility care services were highly associated with higher expenditures. This suggests that the government should plan how to provide sufficient and appropriate facility care and home care services for those with higher requirements for care, and review the eligibility criteria for facility care services to avoid improper institutionalization.
Facility care services use in the baseline care-needs level 5 group showed smaller risk (OR = 1.0) of deterioration than home care services use (OR = 1.3). Facility care services are designed for persons who have difficulties in living independently at home and therefore require intensive nursing care. The average care-needs levels of LTC facility residents have been reported to be ≥3, regardless of type of facility.24 However, there are approximately 179,000 insured individuals with care-needs levels 4 and 5 on waiting lists for admission to LTC facilities,25 indicating that current capacities are inadequate to meet the needs of service users. Consequently, unfulfilled facility care services needs would compel people to turn to home care services or other type of available services instead. However, due to Japanese cultural norms, many elderly people may prefer to live at home and choose home care services rather than facility care services, especially near the end of life.26
Among the lower care-needs levels 1 and 2, those using community-based care services had higher risks of deterioration than those using home care services. In contrast, the risk of deterioration for home care services use was higher than for community-based services use in care-needs levels 3 and 4. However, in persons certified as care needs level 5, the impact of community-based care services relative to facility care services was not significant. Community-based care services were introduced in 2006 with the aim of supporting those who require LTC in communities where they can continue to live in a pleasant and familiar environment.27 Accordingly, community-based care services maybe more appropriate than facility care services for persons with lower care-needs levels. As community-based care services were introduced later than the other types of services, there is currently far less utilization of the former. To the best of our knowledge, there has yet to be a study that has addressed community-based care services in Japan.
Our results suggest that the use of home care services may prevent further deterioration for baseline care needs levels 1 to 4, and that this impact diminishes with increasing care-needs level. The Japanese government has indicated that less severe care-needs level service users who, despite being able to independently live at home, choose to utilize home care services may in fact reduce their levels of physical activity, resulting in the deterioration of their conditions. To prevent this deterioration in those with lower care-needs levels, the LTCI Act was partially revised in 2005 to place an emphasis on preventive measures.27 Koike and Furui have similarly reported that home care services use may prevent the deterioration of care needs level when compared with non-home care services users (but who may use other types of services).16 Ishibashi and Ikegami28 have indicated that beneficiaries with baseline care-needs level 1 who use home help services have lower risk of care-needs level-deterioration than those who use day care services. In addition, Kim and Shiwaku19 report that the use of home help/bathing care services in the lower care-needs level beneficiaries was significantly associated with reduced deterioration in an analysis of 8 kinds of home services. In our study, home care services use was found to have lower risk of deterioration than facility care services use among care needs levels 1 to 4. Although there have been several studies addressing the association between home care services use and care-needs levels or ADL/IADL deterioration, the actual effectiveness of home care services use relative to non-use has yet to be clarified and should be investigated in the near future. Our findings suggest that the appropriate type of LTC services may be different for each care needs level. Further studies are needed to determine the most appropriate care-plan for each care needs level, taking into account dementia diagnoses.
In addition to dementia diagnoses and types of services used, our results showed that, similar to previous studies, sex,29 age,19,30 and lower baseline care-needs levels16 were associated with deterioration in all subjects and care needs level subgroups. Men had a higher risk of deterioration, and the risk increased with higher care-needs levels.
With regard to age, it has been observed that greater frailty is significantly associated with decreased survival,31 and frailty syndrome is associated with aging.32 The increase in frailty that accompanies aging is therefore likely to be an important risk factor leading to the decrease in physical function.
In our study, the risk factors of deterioration in the care-needs level 5 subgroup were dementia diagnosis, sex, older age, and home care services use (OR = 1.30). Few studies have reported the risk factors of care-needs level deterioration in persons with care needs levels 4 or 5: Kato et al15 analyzed samples certified as care-needs levels 1 to 5, but had categorized subjects into 2 groups comprising care-needs levels 1 to 3 and levels 4 to 5. Ishibashi and Ikegami and Tomita et al18,28 only focused on the lower care needs levels, and Koike and Furui investigated subjects with care-needs levels 1 to 4.16 Preventive care is necessary of service users from lower care-needs levels to minimize the deterioration of their conditions. However, the improvement or maintenance of the health conditions and living abilities of service users at care-needs level 5 would also be an important issue for the government to address. Although older age was shown to be highly associated with deterioration, there were no similar significant associations in the younger patients among the lower care-needs levels. Our results suggest that the baseline care-needs level should be considered a fundamental factor when considering LTC policy development.
Although previous studies have investigated the relationships between the deterioration in care-needs levels and types of services used,15,16,19,33 our study examines this relationship while also addressing the effects of dementia diagnoses.
Future research is required to examine whether LTC service resources are appropriately allocated relative to the needs in each medical area and care-needs level, especially for dementia patients.
LIMITATIONS
This study should be interpreted while giving consideration to the following limitations. First, only 2 time points were used to calculate the care-needs level changes; we were unable to confirm whether the beneficiaries were reclassified during the study period.
Furthermore, there are multiple possible reasons for losing cases to follow-up that we could not determine whether the care needs level improved or deteriorated in such cases. These censored cases may therefore affect the generalizability of our findings. In the study, 7367 individuals (approximately 8.5% of the overall sample) were censored due to their lack of service use in June 2011 and as their deaths (deterioration) could not be confirmed in the NHIDB. As the dependent variable of our study was the change in care needs level, individuals whose changes in care-needs levels could not be calculated from the 2 time points (June 2010 and June 2011) were not included in our study sample. Furthermore, 12,139 samples who were nonbeneficiaries of National Healthcare Insurance were excluded from our analysis. After we examined the censored cases, individuals younger than 75 years with baseline care-needs levels >3 was found to account for 7.7% of our sample, but this proportion was approximately doubled (14.6%) in the censored cases. People younger than 75 years may be enrolled in other medical insurance systems, instead of National Healthcare Insurance. However, since age groups and baseline care-needs levels were independent variables in this study and their effects had therefore been accounted for in the regression model, we think that there would be no substantial bias due to the exclusion of the censored cases in our study.
Next, our sample was limited to insurance beneficiaries with baseline care-needs levels 1 to 5 who had utilized LTC services between June 2010 and May 2011. Therefore, people with care-needs levels below these classifications or who had not used any LTC services during our study period were not included in our analysis.
Finally, this study utilized a cross-sectional design, which prevents us from making conclusions about the causal directionalities of the relationships observed.
CONCLUSIONS
Our findings showed that dementia diagnosis, the use of facility care services, the male sex, and older age were associated with higher risk of care-needs level deterioration. In comparison to home care services and community-based care services, the use of facility care services had stronger associations with care-needs level deterioration among persons with lower care needs. Moreover, the impact of baseline dementia on care-needs level deterioration diminished with increasing baseline care-needs levels. Our study suggests that the baseline care-needs level and dementia diagnosis should be considered important factors when developing LTC policies.
Footnotes
Abbreviations: LTC = long-term care, LTCI = long-term care insurance, NHIDB = National Healthcare Insurance Database and Old-Old Adults Medical Care Program Database.
Huei-Ru Lin is a recipient of a scholarship from Otsuka Toshimi Scholarship Foundation (Osaka, Japan). Other 2 authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.World Health Organization. WESTERN PACIFIC Country Health Information Profiles 2011 REVISION: World Health Organization; 2011. [Google Scholar]
- 2.Health and Welfare Bureau for the Elderly. Long-term Care for the Elderly in 2015. 2003; http://www.mhlw.go.jp/topics/kaigo/kentou/15kourei/index.html Accessed March 31, 2014. [Google Scholar]
- 3.Health and Social Statistics Division of Statistics and Information Department Comprehensive Survey of Living Conditions. 2004; http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa04/4–2.html Accessed September 17, 2013. [Google Scholar]
- 4.Health and Social Statistics Division of Statistics and Information Department Comprehensive Survey of Living Conditions. 2007; http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa07/4–2.html Accessed September 17, 2013. [Google Scholar]
- 5.Health and Social Statistics Division of Statistics and Information Department Comprehensive Survey of Living Conditions. 2010; http://www.mhlw.go.jp/toukei/saikin/hw/k-tyosa/k-tyosa10/4-2.html Accessed September 17, 2013. [Google Scholar]
- 6.Arling G, Tu W, Stump TE, et al. Impact of dementia on payments for long-term and acute care in an elderly cohort. Med Care 2013; 51:575–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Langa KM, Larson EB, Wallace RB, et al. Out-of-pocket health care expenditures among older Americans with dementia. Alzheimer Dis Assoc Disord 2004; 18:90–98. [DOI] [PubMed] [Google Scholar]
- 8.Anstey KJ, Mack HA, Cherbuin N. Alcohol consumption as a risk factor for dementia and cognitive decline: meta-analysis of prospective studies. Am J Geriatr Psychiatry 2009; 17:542–555. [DOI] [PubMed] [Google Scholar]
- 9.Luck T, Luppa M, Wiese B, et al. Prediction of incident dementia: impact of impairment in instrumental activities of daily living and mild cognitive impairment-results from the German study on ageing, cognition, and dementia in primary care patients. Am J Geriatr Psychiatry 2012; 20:943–954. [DOI] [PubMed] [Google Scholar]
- 10.Rakowski DA, Caillard S, Agodoa LY, et al. Dementia as a predictor of mortality in dialysis patients. Clin J Am Soc Nephrol 2006; 1:1000–1005. [DOI] [PubMed] [Google Scholar]
- 11.Sauvaget C, Yamada M, Fujiwara S, et al. Dementia as a predictor of functional disability: a four-year follow-up study. Gerontology 2002; 48:226–233. [DOI] [PubMed] [Google Scholar]
- 12.Matsuda S, Tanaka M, Kubo T, et al. Factors associated with length of stay of the elderly patient in the japanese long term care wards. Asian Pacific J Dis Manag 2009; 3:75–81. [Google Scholar]
- 13.Murtaugh CM, Spillman BC, Wang XD. Lifetime risk and duration of chronic disease and disability. J Aging Health 2011; 23:554–577. [DOI] [PubMed] [Google Scholar]
- 14.Tsutsui T, Muramatsu N. Japan's universal long-term care system reform of 2005: containing costs and realizing a vision. J Am Geriatr Soc 2007; 55:1458–1463. [DOI] [PubMed] [Google Scholar]
- 15.Kato G, Tamiya N, Kashiwagi M, et al. Relationship between home care service use and changes in the care needs level of Japanese elderly. BMC Geriatr 2009; 9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koike S, Furui Y. Long-term care-service use and increases in care-need level among home-based elderly people in a Japanese urban area. Health Policy 2013; 110:94–100. [DOI] [PubMed] [Google Scholar]
- 17.Olivares-Tirado P, Tamiya N, Kashiwagi M. Effect of in-home and community-based services on the functional status of elderly in the long-term care insurance system in Japan. BMC Health Serv Res 2012; 12:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tomita N, Yoshimura K, Ikegami N. Impact of home and community-based services on hospitalisation and institutionalisation among individuals eligible for long-term care insurance in Japan. BMC Health Serv Res 2010; 10:345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim J-N, Shiwaku K. The effect of utilization of in-home services and the changes in levels of care needs of frail persons (2002–2004): results of a two-year follow-up study. J Rural Med 2012; 7:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norton MJ, Allen RS, Snow AL, et al. Predictors of need-driven behaviors in nursing home residents with dementia and associated certified nursing assistant burden. Aging Ment Health 2010; 14:303–309. [DOI] [PubMed] [Google Scholar]
- 21.National Collaborating Centre for Mental H. National Institute for Health and Clinical Excellence: Guidance. Dementia: A NICE-SCIE Guideline on Supporting People With Dementia and Their Carers in Health and Social Care. Leicester (UK): British Psychological Society. The British Psychological Society & The Royal College of Psychiatrists; 2007. [PubMed] [Google Scholar]
- 22.Carpenter GI, Hastie CL, Morris JN, et al. Measuring change in activities of daily living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatr 2006; 6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gaugler JE, Yu F, Krichbaum K, et al. Predictors of nursing home admission for persons with dementia. Medical Care 2009; 47:191–198.110.1097/MLR.1090b1013e31818457ce. [DOI] [PubMed] [Google Scholar]
- 24.Health and Social Statistics Division of Statistics and Information Department. Survey of Long-term Care Benefit Expenditures, 2012. 2012; http://www.mhlw.go.jp/english/database/db-hss/soltcbe2012.html Accessed June 19, 2014. [Google Scholar]
- 25.Ministry of Health Labour and Welfare. Status of the applicant's admission of nursing home. 2010; http://www.mhlw.go.jp/stf/houdou/2r98520000003byd.html Accessed March 25, 2014. [Google Scholar]
- 26.Health and Welfare Bureau for the Elderly. The opinion of Long-Term Care Insurance Committee in social security council. Health and Welfare Bureau for the Elderly; Tokyo: 2013. [Google Scholar]
- 27.Ministry of Health Labour and Welfare. Annual Health, Labour and Welfare Report 2006: Ministry of Health, Labour and Welfare; 2006. [Google Scholar]
- 28.Ishibashi T, Ikegami N. Should the provision of home help services be contained?: validation of the new preventive care policy in Japan. BMC Health Serv Res 2010; 10:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kashiwagi M, Tamiya N, Sato M, et al. Factors associated with the use of home-visit nursing services covered by the long-term care insurance in rural Japan: a cross-sectional study. BMC Geriatr 2013; 13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ho HK, Matsubayashi K, Wada T, et al. Factors associated with ADL dependence: a comparative study of residential care home and community-dwelling elderly in Japan. Geriatr Gerontol Int 2002; 2:80–86. [Google Scholar]
- 31.Klei BEK, Klein R, Knudtson MD, et al. Frailty, morbidity and survival. Arch Gerontol Geriatr 2005; 41:141–149. [DOI] [PubMed] [Google Scholar]
- 32.Ahmed N, Mandel R, Fain MJ. Frailty: an emerging geriatric syndrome. A J Med 2007; 120:748–753. [DOI] [PubMed] [Google Scholar]
- 33.Fukuma M, Shiwaku K. Changes of care levels of frail elderly individuals after introduction of long-term nursing care insurance system. J Jpn Association of Rural Medicine 2010; 58:516–525. [Google Scholar]


