Abstract
Objectives:
Although 18F-fluorodeoxyglucose positron emission tomography (PET)/computed tomography (CT) has largely replaced the use of gallium-67 (67Ga) scintigraphy in the evaluation and follow-up of lymphoma patients, 67Ga scans are still of value, particularly in countries where no PET/CT service is available. The current study presents the experience of a tertiary care centre using 67Ga scintigraphy for the evaluation of lymphomas and infections.
Methods:
A retrospective review was conducted of all 67Ga scans performed between 2007 and 2011 at the Royal Hospital in Muscat, Oman. Images and reports of 67Ga scans were compared to clinical and radiological follow-up data including CT and PET/CT scans and biopsies when available.
Results:
A total of 74 patients were referred for 67Ga scintigraphy during this period with 12 patients excluded due to lack of follow-up data, resulting in 62 patients. Among these patients, 90 67Ga scans were performed, including 59 for lymphoma, 29 for infection and two for sarcoidosis assessment. Of the infection assessment scans, 22 were performed to assess pyrexia of unknown origin and seven for follow-up after known infections. Sensitivity and specificity were found to be 80% and 88%, respectively, for the lymphoma assessment scans. For the infection assessment scans, sensitivity and specificity were reported to be 80% and 100%, respectively.
Conclusion:
Results from this study were consistent with other reported rates of 67Ga scan sensitivity and specificity in the evaluation of lymphomas and infections. This indicates that 67Ga scintigraphy is a useful tool for these types of evaluations when PET/CT services are not available.
Keywords: Gallium-67-Citrate, Gallium Radioisotopes, Fluorodeoxyglucose F18, Scintigraphy, Lymphoma, Infection, Fever of Unknown Origin, Oman
Advances in Knowledge
- Results of the current study confirmed that the sensitivity and specificity of gallium-67 (67Ga) scintigraphy in this tertiary centre were consistent with those reported in the international literature.
Application to Patient Care
- 67Ga scintigraphy can help in localising the foci of infection. Scans can also show positive findings in patients with neoplastic disease presenting with pyrexia of unknown origin. Follow-up 67Ga scans can be performed to assess the response to treatment or resolution of the infective process.
- Despite current hybrid and molecular imaging services provided by combined 18F-fluorodeoxyglucose positron emission tomography and computed tomography, this study demonstrated that67 Ga scintigraphy remains a useful tool for the evaluation and follow-up of patients with lymphoma.
The clinical impact and cost-effectiveness of combined 18F-fludeoxyglucose (18F-FDG) positron emission tomography (PET) and computed tomography (CT) is well documented in the literature and this technology has a wide range of applications in both benign diseases and oncology.1 Additionally, the role of PET/CT in the diagnosis and management of lymphomas has been well established for more than a decade.2 Non-PET radiotracers that were previously used for the evaluation of lymphomas and infections are now seldom utilised in current practice. However, despite the advances this technology has brought to patient management, some centres still lack PET/CT facilities. In other institutions where PET/CT is available, not all PET radiotracers are accessible or approved for clinical practice. Hence, the old radiotracers used in nuclear medicine still exist and play a role in today’s modern practice.
One of the most commonly used radioisotopes in tumour imaging, as well as in the imaging of infection and inflammation, is gallium-67 citrate (67Ga).3 This group IIIA metal has been used for decades for the imaging of various solid neoplasms, particularly lymphomas, and in the investigation of acute inflammatory conditions. It is also used to assess infections and to identify the site of disease in patients with pyrexia of unknown origin (PUO).4 67Ga is produced by cyclotron and has a half-life of 78.26 hours and energy abundances of 93 kilo electron volts ([keV] 40%), 184 keV (20%), 300 keV (17%) or 393 keV (5%). For medical radiology purposes, 67Ga is provided in the form of a sterile solution of gallium citrate.3,5,6 The human body reacts to 67Ga similarly to the way that it handles ferric iron. Gallium III ions bind to transferrin glycoproteins, leukocyte lactoferrin, bacterial siderophores, inflammatory proteins and cell membranes in neutrophils and become concentrated in areas of inflammation and rapid cell division.3,7
This retrospective study aimed to evaluate the use of 67Ga in a tertiary care hospital over a period of five years and compare outcomes with available clinical and radiological follow-up data, including CT and PET/CT scans and biopsies.
Methods
This retrospective review included all 67Ga scintigraphy scans performed in the Department of Nuclear Medicine at the Royal Hospital, Muscat, Oman, from 2007–2011. Only patients who were referred to this department and with follow-up appointments at the Royal Hospital were included in the study.
At the Royal Hospital, 67Ga scans were performed by nuclear medicine technologists with a Siemens E-Cam Dual-Head Variable Angle Gamma Camera (Siemens Medical Solutions USA Inc., Malvern, Pennsylvania, USA). Adult patients undergoing 67Ga scintigraphy received a dose of 180 megabecquerels (MBq) while the dose for child patients was calculated by multiplying their weight in kg by 180 MBq and dividing the total by 70 kg.8 All patients with excessive bowel activity were given laxatives and scanned one or two days afterward. Whole body imaging for lymphoma patients was performed 48 hours after the 67Ga injection using both detectors with a matrix size of 256 × 1,024 pixels. However, patients with PUO or infections were imaged 24 hours after the injection. Additional imaging was performed after 48 hours or later, if deemed necessary.
Spot views of the chest and abdomen were acquired with both detectors with a matrix size of 256 × 256 pixels. Imaging was halted either after five minutes had elapsed or if 500 kilo counts had been obtained. The whole process usually took 30–45 minutes, although sometimes longer if single photon emission CT images were also required.
The 67Ga images and reports were compared to subsequent clinical and radiological follow-up data, including CT and PET/CT scans and biopsies, if available. These data were collected from hospital records retrospectively.
This study was approved by the Research & Ethical Committee at the Royal Hospital (#MESRC 17/2014).
Results
A total of 74 patients were referred to the Department of Nuclear Medicine at the Royal Hospital for 67Ga scintigraphy between 2007 and 2011; however, 12 patients were excluded due to a lack of follow-up data. As a result, 62 patients were included in the final sample. The mean age of these patients was 43 years old. A total of 28 patients were male (45%). The majority of referrals were from medical oncologists referring lymphoma patients (n = 24; 39%) and infectious diseases specialists referring patients (n = 9; 15%), primarily for the localisation of infection sites. Seven patients (11%) were paediatric haematology cases; the remaining patients were chest medicine, paediatric, rheumatology, nephrology, neurology or acute medicine cases.
A total of 90 67Ga scans were performed during the study period. Assessment of lymphomas constituted the bulk of the referrals, with a total of 59 scans (66%). Of the remaining scans, 29 (32%) were performed for infection assessment and two (2%) were performed for sarcoidosis. Of the 67Ga scans carried out for lymphoma patients, 32 were for Hodgkin’s lymphomas (HL), 23 were for non-Hodgkin’s lymphomas (NHL), three were for mucosa-associated lymphoid tissue lymphomas and one was for T cell lymphoma.
Lymphoma scans were divided into six baseline scans, 10 mid-therapy response assessment scans and 43 post-therapy scans for the assessment of relapse [Table 1]. Of the six baseline studies, five scans yielded true-positive results and one showed a false-negative result. Of the 10 mid-therapy studies performed to assess response to therapy, six were true-negative, three were true-positive and one yielded a false-negative result. The majority of the 67Ga lymphoma scans were performed to assess relapse: 24 scans yielded true-negative results (i.e. no evidence of gallium-avid lesions); 11 scans produced true-positive results (either recurrence in the same sites or relapses in new sites); and five scans gave false-positive results (infection sites which were mistaken for lymphoma lesions). The remaining three scans yielded false-negative results as the lesions were not avid on 67Ga scans but were positive on a subsequent 18F-FDG-PET/CT scan or via biopsy. These results indicated a sensitivity and specificity of 80% and 88%, respectively, for assessing lymphomas using 67Ga scintigraphy.
Table 1:
Comparison of the findings of gallium-67 scintigraphy lymphoma assessment scans to subsequent clinical and radiological follow-up data (N = 59)
| Scan type | Result | Total | |||
|---|---|---|---|---|---|
| True-positive | False-positive | True-negative | False-negative | ||
| Baseline | 5 | 0 | 0 | 1 | 6 |
| Mid-therapy | 3 | 0 | 6 | 1 | 10 |
| Post-therapy | 11 | 5 | 24 | 3 | 43 |
| Total | 19 | 5 | 30 | 5 | 59 |
Infection assessments were carried out either for patients with PUO in order to localise the source of infection (n = 22) or for follow-up of a known infection (n = 7) [Table 2]. For known infection follow-up scans, five yielded true-positive results while two yielded true-negative results. Of the 22 patients who were scanned for PUO, nine indicated positive uptake at different sites and these areas were subsequently targeted during treatment. One of these patients had a positive 24-hour whole body 67Ga scan with pericardial uptake indicating active pericarditis, which turned out to be secondary to tuberculosis [Figure 1]. A further three patients were found to have 67Ga-avid lesions. Of the three, one patient showed suprarenal uptake, with a biopsy revealing neuroblastoma [Figure 2]. The second patient had supraclavicular lymph node uptake revealing HL [Figure 3], while the third patient showed lung uptake which was found to be Wegener’s granulomatosis.
Table 2:
Comparison of the findings of gallium-67 scintigraphy infection assessment scans to subsequent clinical and radiological follow-up data (N = 29)
| Scan type | Result | Total | |||
|---|---|---|---|---|---|
| True-positive | True-negative | False-positive | False-negative | ||
| PUO | 12 | 7 | 0 | 3 | 22 |
| Follow-up of known infection | 5 | 2 | 0 | 0 | 7 |
| Total | 17 | 9 | 0 | 3 | 29 |
PUO = pyrexia of unknown origin.
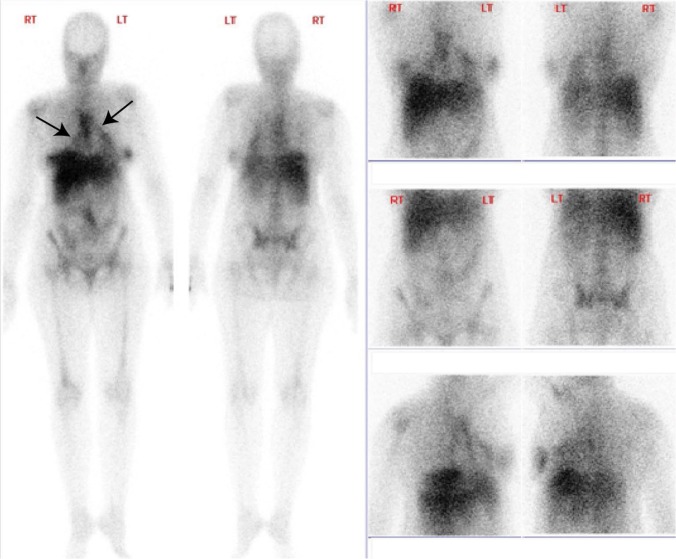
Figure 1:
Gallium-67 scintigraphy images revealing pericardial uptake (arrows) in a patient with pyrexia of unknown origin. Echocardiography and aspiration revealed tuberculosis (TB) pericarditis. The patient was subsequently treated with anti-TB medication.
RT = right; LT = left.
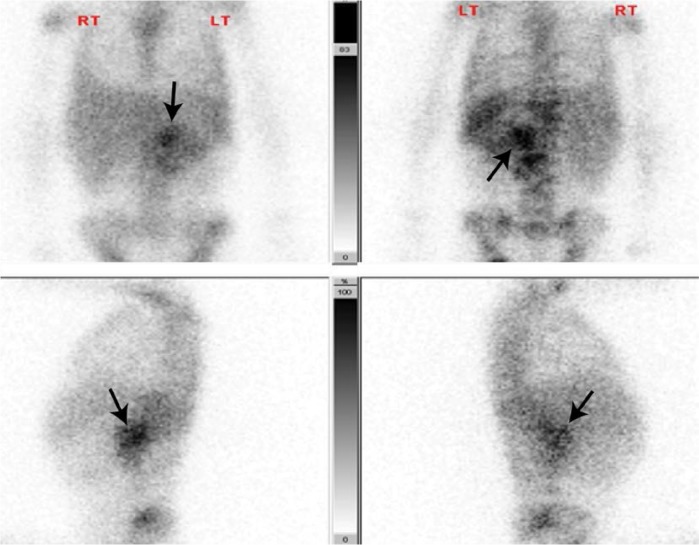
Figure 2:
Gallium-67 scintigraphy images showing left suprarenal uptake (arrows) in a child with pyrexia of unknown origin. Computed tomography and a subsequent biopsy revealed a neuroblastoma.
RT = right; LT = left.
Figure 3:
Gallium-67 scintigraphy images showing mediastinal (red arrow) and thymic uptake (blue arrow) in a patient referred for lymphoma assessment. A biopsy revealed Hodgkin’s lymphoma.
RT = right; LT = left.
There were no 67Ga-avid lesions found in the remaining 10 PUO assessment scans. In three patients, no source of infection was found and the patients were treated empirically with antibiotics. In another three patients, the negative scans were attributed to prolonged antibiotic therapy (n = 2) and fungal infection (n = 1). In the final four negative 67Ga scans, no source of infection was found and the fevers were attributed to different disease processes, including systemic lupus erythematosus, adult-onset Still’s disease, a connective tissue disease and myelodysplastic syndrome. These results showed sensitivity and specificity rates of 80% and 100%, respectively, in the assessment of infection using 67Ga scintigraphy.
Two patients were known to have sarcoidosis and were referred for an assessment of disease activity. One was negative with no 67Ga-avid uptake related to sarcoidosis, while the other showed bilateral breast uptake which, upon clinical examination, was found to be caused by bilateral mastitis.
Discussion
PET/CT has almost replaced 67Ga scintigraphy in the assessment of both oncology and infection; this imaging modality plays a well-documented and clinically proven role not only in tumour staging, but also in evaluating treatment response and predicting treatment outcomes.1,8,9 In addition, the use of PET/CT in the imaging of inflammation and in the evaluation of patients with PUO is well-known.10,11 In spite of the efficacy of this modality, some nuclear medicine departments may nevertheless lack PET/CT facilities or resources. Hence, 67Ga scintigraphy is still used for tumour and infection imaging. 67Ga uptake is highest in diffuse large cell and high- and intermediate-grade lymphomas due to their high cell division rates.4,5
67Ga citrate was used extensively in the past for several pathological conditions, particularly when the presence of tumours, infection or inflammation was in question.3 In past decades, the role of 67Ga scintigraphy in nuclear oncology mainly focused on assessing the response of lymphoma to therapy. However, it was also used as a baseline for staging and to assess gallium avidity, patient response to treatment and residual disease activity post-therapy.5
In a study evaluating 50 lymphoma patients, 67Ga was used in routine staging and was found to provide information that was missed or equivocal by other diagnostic modalities in 20–25% of patients.12 Another study compared the positive and negative predictive values and disease-free survival rates in 43 patients with HL and 56 patients with NHL.13 A significant difference in disease-free survival was found between patients with positive and negative 67Ga scans. It was concluded that 67Ga was a reliable predictor of clinical outcomes in these cases.13
Regarding the use of 67Ga scintigraphy in evaluating infection and inflammation, high sensitivity has been demonstrated for both infectious as well as non-infectious inflammation processes.14 The most common clinical scenarios where 67Ga is still utilised include PUO, sarcoidosis and in cases of malignant otitis externa. In addition, 67Ga has been successfully utilised in the evaluation of spinal discitis and vertebral osteomyelitis, mainly to assess disease activity.3
Technetium-99m (99mTc) sulesomab is another modality for evaluating infection and can be used instead of 67Ga in most indications.15 This anti-granulocyte antigen-binding fragment has been used for more than a decade to image soft tissue infections and osteomyelitis.15 At the Royal Hospital, 99mTc sulesomab has been used since 2013 to evaluate patients with total knee replacements for septic loosening. It is also valuable in detecting osteomyelitis in patients with sickle cell disease, particularly when a three-phase bone scan might yield a false-positive result in sites with regenerating bone marrow following vaso-occlusive crises.15
18F-FDG-PET/CT imaging is not yet available in Oman.16 Almost all oncology patients from the Royal Hospital are sent abroad for 18F-FDG-PET/CT imaging for initial staging and the evaluation of residual disease and treatment response. Currently, 67Ga citrate is used for the imaging of patients with PUO and the evaluation of patients with malignant otitis externa. In addition to a three-phase bone scan, 67Ga is also used to evaluate patients with total knee replacements for septic loosening.
Conclusion
Although the utilisation of 67Ga citrate has become less common with the introduction of new imaging modalities such as PET/CT and new radiotracers such as 99mTc, the findings of this study confirm that there is a continuing role for this radiotracer in infection and tumour imaging, particularly when PET/CT facilities are not available. Furthermore, the results from this study were consistent with other reported rates of 67Ga scan sensitivity and specificity in the evaluation of lymphomas and infections.
References
- 1.Krause BJ, Schwarzenböck S, Souvatzoglou M. FDG PET and PET/CT. Recent Results Cancer Res. 2013;187:351–69. doi: 10.1007/978-3-642-10853-2_12. [DOI] [PubMed] [Google Scholar]
- 2.Morton KA, Jarboe J, Burke EM. Gallium-67 imaging in lymphoma: Tricks of the trade. J Nucl Med Technol. 2000;28:221–32. [PubMed] [Google Scholar]
- 3.Khan MU, Usmani MS. Radionuclide infection imaging: Conventional to hybrid. In: Gholamrezanezhad A, editor. 12 Chapter on Nuclear Medicine. Rijeka, Croatia: InTech; 2011. pp. 73–96. [Google Scholar]
- 4.Bartold SP, Donohoe KJ, Haynie TP, Henkin RE, Silberstein EB, Lang O. Society of Nuclear Medicine procedure guideline for gallium scintigraphy in the evaluation of malignant disease. From: snmmi.files.cms-plus.com/docs/pg_ch23_0403.pdf Accessed: Mar 2015. [PubMed]
- 5.Bombardieri E, Aktolun C, Baum RP, Bishof-Delaloye A, Buscombe J, Chatal JF, et al. 67Ga scintigraphy: Procedure guidelines for tumour imaging. Eur J Nucl Med Mol Imaging. 2003;30:BP125–31. doi: 10.1007/S00259-003-1356-1. [DOI] [PubMed] [Google Scholar]
- 6.Seabold JE, Palestra CJ, Brown ML, Datz FL, Forstrom LA, Greenspan BS, et al. Procedure guideline for gallium scintigraphy in inflammation: Society of Nuclear Medicine. J Nucl Med. 1997;38:994–7. [PubMed] [Google Scholar]
- 7.Love C, Palestro CJ. Radionuclide imaging of infection. J Nucl Med Technol. 2004;32:47–57. [PubMed] [Google Scholar]
- 8.Gelfand MJ, Parisi MT, Treves ST, Pediatric Nuclear Medicine Dose Reduction Workgroup Pediatric radiopharmaceutical administered doses: 2010 North American consensus guidelines. J Nucl Med. 2011;52:318–22. doi: 10.2967/jnumed.110.084327. [DOI] [PubMed] [Google Scholar]
- 9.Vranjesevic D, Filmont JE, Meta J, Silverman DH, Phelps ME, Roa J, et al. Whole-body (18)F-FDG PET and conventional imaging for predicting outcome in previously treated breast cancer patients. J Nucl Med. 2002;43:325–9. [PubMed] [Google Scholar]
- 10.Ben-Haim S, Ell P. 18F-FDG PET and PET/CT in the evaluation of cancer treatment response. J Nucl Med. 2009;50:88–99. doi: 10.2967/jnumed.108.054205. [DOI] [PubMed] [Google Scholar]
- 11.Gotthardt M, Bleeker-Rovers CP, Boerman OC, Oyen WJ. Imaging of inflammation by PET, conventional scintigraphy, and other imaging techniques. J Nucl Med. 2010;51:1937–49. doi: 10.2967/jnumed.110.076232. [DOI] [PubMed] [Google Scholar]
- 12.Seabold JE, Votaw ML, Keyes JW, Jr, Foley WD, Balachandran S, Gill SP. Gallium citrate Ga 67 scanning: Clinical usefulness in lymphoma patients. Arch Intern Med. 1976;136:1370–4. doi: 10.1001/archinte.1976.03630120022010. [DOI] [PubMed] [Google Scholar]
- 13.Front D, Ben-Haim S, Israel O, Epelbaum R, Haim N, Even-Sapir E, et al. Lymphoma: Predictive value of Ga-67 scintigraphy after treatment. Radiology. 1992;182:359–63. doi: 10.1148/radiology.182.2.1732950. [DOI] [PubMed] [Google Scholar]
- 14.Keidar Z, Gurman-Balbir A, Gaitini D, Israel O. Fever of unknown origin: The role of 18F-FDG PET/CT. J Nucl Med. 2008;49:1980–5. doi: 10.2967/jnumed.108.054692. [DOI] [PubMed] [Google Scholar]
- 15.Skehan SJ, White JF, Evans JW, Parry-Jones DR, Solanki CK, Ballinger JR, et al. Mechanism of accumulation of 99mTc-sulesomab in inflammation. J Nucl Med. 2003;44:11–18. [PubMed] [Google Scholar]
- 16.Al-Bulushi NK, Bailey D, Mariani G. The medical case for a positron emission tomography and X-ray computed tomography combined service in Oman. Sultan Qaboos Univ Med J. 2013;13:491–501. doi: 10.12816/0003307. [DOI] [PMC free article] [PubMed] [Google Scholar]