Abstract
Objectives:
An outbreak of acute gastroenteritis due to Shigella flexneri occurred in August 2012 in the catchment area of the Wadi Sahtan Health Center in Rustaq, Al Batinah South Governorate, Oman. The aim of this study was to discover possible causes of this outbreak in the villages of Fassa, Rogh and Amk and to measure the risk of exposure among cases and controls.
Methods:
A case-control study was conducted in September 2012 in Fassa, Rogh and Amk. All households in the three villages were interviewed. Case and control households were compared to determine possible exposure avenues, including place of residence, source of drinking water, hand hygiene levels and practices related to drinking water, food preparation and environmental sanitation.
Results:
Residing in Fassa (P <0.0001; odds ratio [OR] = 4.86, 95% confidence interval [CI] = 2.22–10.63) and average hand hygiene practices (P = 0.008; OR = 13.97, 95% CI = 1.58–123.36) were associated with an increased risk of contracting shigellosis. No significant differences were found with regards to the other exposure avenues.
Conclusion:
This was the first study conducted in Oman regarding an outbreak of shigellosis in a community setting. The only variables that significantly impacted the risk of acute gastroenteritis were residing in Fassa and average hand hygiene practices. The source of the outbreak could not be identified. However, septic tank sanitation and water and food consumption practices were not satisfactory in the studied villages. These need to be addressed to prevent similar outbreaks of acute gastroenteritis in this region in the future.
Keywords: Case-Control Study, Disease Outbreaks, Shigellosis, Transmission, Risk Factors, Oman
Advances in Knowledge
- This is the first study conducted in Oman regarding a shigellosis outbreak in a community setting and investigating sources and risks of exposure.
Application to Patient Care
- The findings of this study will aid the implementation of preventative measures to protect against outbreaks of shigellosis in Oman and among other communities.
Shigellosis is an important public health problem and outbreaks have been reported both in developed and developing countries.1,2 Person-to-person contact and contaminated food and water are the major modes of transmission.3–5 While waterborne outbreaks of shigellosis have been reported in many countries, to the best of the authors’ knowledge, there have been no published studies of shigellosis outbreaks in Oman to date.2,5
The Wadi Sahtan Health Center is located nearly 45 km from Rustaq Hospital in the wilayat (district) of Rustaq, Al Batinah South Governorate, Oman. There are 51 villages in the catchment area of the health centre, with a total population of 10,304 people, of which 9,944 are Omani (96.5%).6 In August 2012, an outbreak of acute gastroenteritis due to Shigella flexneri occurred in this catchment area.7 A total of 142 cases of acute gastroenteritis were reported from the villages of Fassa, Rogh and Amk. Of these cases, 26 were admitted to Rustaq Hospital. Stool samples were collected from 21 out of the 26 admitted cases; 7 of these were positive for S. flexneri. All of the isolates had the same antibiotic sensitivity pattern (sensitive to nalidixic acid, ciprofloxacin, cefotaxime, co-trimoxazole and resistant to ampicillin, augmentin and chloramphenicol).
Households from the three affected villages shared a common desalinated water source—a three-tank water storage system—which contained a mixture of water originally pumped from four tube wells and water from a desalination plant in Rustaq which had been transported to the villages by water tankers.7 The desalinated water had been chlorinated at a facility in Barka, a city approximately 96 km away, before being transmitted via pipeline to the desalination plant in Rustaq. Other sources of drinking water included personal mineral and well water supplies and water supplied through tankers to individual households.
Field staff from the Communicable Disease Control Center of the Ministry of Health in Al Batinah South Governorate collected 15 water samples in August 2012 for bacteriological examinations from either transporting tankers, mosques, other public facilities or from houses as collection was not possible from the tube wells or overhead storage tanks.8 Samples were tested for Escherichia coli and coliforms and determined to be either satisfactory or not suitable for human consumption. Samples collected from water tankers were found to be satisfactory. Three water samples collected from households, one water sample collected from a public cooler and one water sample collected from a mosque were not suitable for human consumption. Faecal coliforms were found in two water samples and coliform bacilli were present in three samples.8
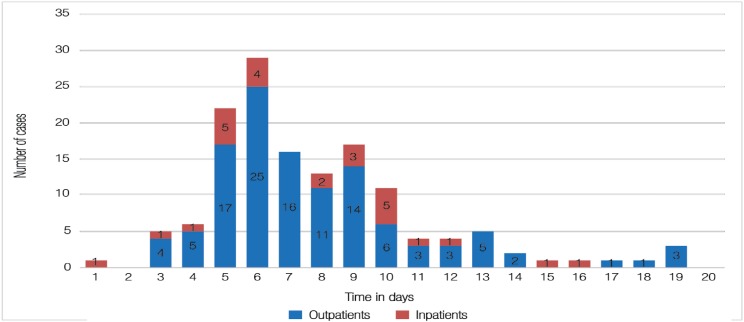
The epidemic curve [Figure 1], clinical data and geographical distribution of cases with similar symptoms, greater number of cases in children and the isolation of S. flexneri with the same antibiotic sensitivity profile from stool samples all indicated that this was an outbreak of shigellosis with a common source. This study was conducted in order to describe the outbreak and estimate the risk of certain exposure factors in the development of shigellosis in this community setting in the wilayat of Rustaq, Oman.
Figure 1:
Epidemic curve chart of a shigellosis outbreak in Rustaq, Al Batinah South Governorate, Oman (N = 142). A total of 114 outpatients presented to the Wadi Sahtan Health Center between mid-August and the beginning of September 2012. In addition, 26 inpatients were admitted to Rustaq Hospital during the same 20-day period.
Methods
This case-control study was carried out in the villages of Fassa, Rogh and Amk in September 2012 to identify the cause of the August 2012 shigellosis outbreak. Face-to-face interviews were conducted with all households in the three villages by 12 health educators and school health nurses working in six teams. Interviewers had received a one-day training course from a regional epidemiologist and regional infection control specialist and were trained on interview techniques and questionnaire completion procedures in order to ensure uniformity and minimise any potential bias in the data collection. Demographic details and data on possible exposures were collected, including sources of both drinking water and water for washing fruit/vegetables. Other variables included the presence of houseflies and practices related to water consumption; hand hygiene; food preparation and consumption; household waste collection and disposal; and septic tank maintenance.
Households were considered to be case households if any member of the household had had diarrhoea ≥3 times per day (with or without vomiting, fever, abdominal pain and dehydration) between the date of the interview in September and two days before the first reported case of shigellosis in August. If no members were reported to have been affected, the household was considered a control household.
During the interview, households were asked questions related to water consumption and storage practices. These questions focused on whether drinking water was boiled and cooled before consumption; the frequency of water storage tank cleaning in the previous six months; whether water purifying filters were used and, if so, the frequency of changing these filters in the previous six months and the type of filters used. With regards to hand hygiene practices, household members were asked to report whether they washed their hands with soap and water before preparing food and eating and after using the toilet and changing diapers. If all of these practices were carried out by all members of the household, then hand hygiene practices were considered good. Practices were considered unsatisfactory if household members indicated that they did not wash their hands after using the toilet or changing diapers. Other combinations of responses were considered to indicate average practices.
Household members were asked whether raw vegetables and fruits were washed before they were eaten or used in salads and, if so, the source of the water used. Additionally, interviewers enquired as to whether meals were prepared fresh before consumption. If meals were not prepared immediately before consumption, interviewers asked where the food was stored and whether it was reheated before consumption.
Information about household waste collection was also obtained during the interview. Specifically, household members were asked whether waste was disposed of in open or closed containers and the frequency with which household waste was dumped in the community bin (either on a daily basis, once every 2–3 days or every three days or longer). The frequency of collection of household waste from the community bin by the municipality was also assessed (either on a daily basis, every 2–3 days, every 4–7 days, every 8–14 days or every 14 days or longer). The presence of any houseflies in the house during the interview was noted by interviewers.
Full or clogged septic tanks in close proximity to water supply lines places the population at risk for acute gastroenteritis via possible contamination of the drinking water sources. Households were therefore asked about the presence of septic tanks and, if present, the frequency with which the septic tanks were emptied. This was an open-ended question. Additionally, interviewers observed and noted the presence of any overflowing or leaking septic tanks in the households during the interview.
Collected data were presented in numbers and percentages and analysed using the Statistical Package for the Social Sciences (SPSS), Version 16 (IBM Corp., Chicago, Illinois, USA). The Chi-squared test of significance was used to compare the case and control groups. Fisher’s exact test was used when there were less than five observations in a group. The odds ratio (OR) and 95% confidence interval (CI) was calculated. A P value of ≤0.05 was considered statistically significant.
This study was approved by the Research & Ethical Committee of the Al Batinah South Governorate in Oman. The purpose of the study was explained to all subjects and oral consent received before the interviews were conducted.
Results
A total of 154 households were included in the study, with 44 (28.6%) classified as cases and 110 (71.4%) as controls. The greatest number of households (48.7%) were located in Fassa, followed by Amk (31.2%) and Rogh (20.1%). Among the case households, Fassa was the village most affected by acute gastroenteritis (n = 33; 75.0%) with only six (13.6%) and five (11.4%) affected households from Rogh and Amk, respectively. The distribution of control households was 42 (38.2%), 25 (22.7%) and 43 (39.1%) households located in Fassa, Rogh and Amk, respectively. The case-to-control ratio was 1:1.3 in Fassa, 1:4.2 in Rogh and 1:8.6 in Amk.
Descriptive data of shigellosis exposure variables from all households are shown in Table 1. The vast majority of households (87.1%) indicated that their drinking water originated from the common water tank which supplied all three villages. Water filters were used for purification purposes in 134 households (87.0%). Fruit/vegetables were washed before consumption in 98.7% of households, with 87.6% using common tank water for this purpose. Only 3.2% of households reported boiling and cooling their drinking water before consumption. The water tanks in 23.4% and water filters in 7.5% of households had not been cleaned or changed at all in the previous six months. Hand hygiene practices were rated as good in 96.1% of households.
Table 1:
Descriptive data of shigellosis exposure variables from households in Rustaq, Al Batinah South Governorate, Oman (N = 154)
| Variable | n (%) |
|---|---|
| Place of residence | |
| Fass | 75 (48.7) |
| Amk | 48 (31.2) |
| Rogh | 31 (20.1) |
| Presence of affected household members | |
| Yes | 44 (28.6) |
| No | 110 (71.4) |
| Source of drinking water | |
| Common tank | 134 (87.1) |
| Personal mineral water | 8 (5.2) |
| Tanker | 5 (3.2) |
| Well | 6 (3.9) |
| Other | 1 (0.6) |
| Use of water filters | |
| Yes | 134 (87.0) |
| No | 20 (13.0) |
| Type of water filters* | |
| Electrical | 119 (77.3) |
| Candle | 15 (9.7) |
| Frequency of changing water filters* | |
| At least once in six months | 124 (92.5) |
| Not changed | 10 (7.5) |
| Water boiled/cooled before drinking† | |
| Yes | 5 (3.2) |
| No | 148 (96.1) |
| Frequency of cleaning water tank | |
| At least once in six months | 114 (74.0) |
| Not clean | 36 (23.4) |
| Not answered | 4 (2.6) |
| Hand hygiene practices | |
| Good | 148 (96.1) |
| Average | 5 (3.2) |
| Unsatisfactory | 1 (0.6) |
| Washing fruit/vegetables before consumption | |
| Yes | 152 (98.7) |
| No | 2 (1.3) |
| Source of water for vegetable washing | |
| Common tank | |
| Filtered | 9 (5.8) |
| Not filtered | 126 (81.8) |
| Tanker | 5 (3.2) |
| Well | 6 (3.9) |
| Other | 8 (5.2) |
| Fresh preparation of food before consumption | |
| Yes | 143 (92.9) |
| No | 11 (7.1) |
| Waste collection container | |
| Open | 93 (60.4) |
| Closed | 61 (39.6) |
| Frequency of waste disposal | |
| Daily | 141 (91.6) |
| Every 2–3 days | 13 (8.4) |
| Every three days or longer | 0 (0.0) |
| Frequency of waste collection by municipality | |
| Daily | 0 (0) |
| Every 2–3 days | 0 (0) |
| Every 4–7 days | 10 (6.5) |
| Every 8–14 days | 6 (3.9) |
| Every 14 days or longer | 138 (89.4) |
| Presence of houseflies | |
| Yes | 65 (42.2) |
| No | 88 (57.1) |
| Not observed | 1 (0.7) |
| Presence of septic tank | |
| Yes | 149 (96.8) |
| No | 5 (3.2) |
| Presence of septic tank overflow/leakage | |
| Yes | 9 (5.8) |
| No | 145 (94.2) |
Total number of households for these variables was 134 as 20 households did not use water filters.
Total number of households for this variable was 153 due to missing data for one household.
Waste was collected in an open container in 60.4% of households; however, household waste was disposed of on a daily basis in 91.6% of the households. The majority of the households (89.4%) reported that it took more than 14 days for waste in common bins to be collected and disposed of by the local municipality. Houseflies were observed in 42.2% of households. The majority of households (96.8%) had septic tanks, although overflowing/leaking septic tanks were observed in 5.8% of residences. Additionally, 112 households (72.7%) reported that they had never emptied their septic tanks.
Sources of exposure were compared between case and control households [Table 2]. As the greatest number of acute gastroenteritis cases resided in Fassa, households in Fassa were compared to the households from both Amk and Rogh. The risk of shigellosis occurring in a household in Fassa was 4.85 times higher than for the villages of Amk and Rogh combined (OR = 4.857, 95% CI = 2.219–10.631). This was statistically significant (P <0.005). As common tank water was the suspected source of the shigellosis outbreak, drinking water sources were categorised into either common tank or other water sources. The risk of shigellosis was 1.5 times greater in households using water from the common tank water source (OR = 1.579, 95% CI = 0.493–5.053) compared to those using other sources of drinking water; however, this was not statistically significant (P = 0.590).
Table 2:
Comparison of shigellosis exposure variables between case and control households study in Rustaq, Al Batinah South Governorate, Oman (N = 154)
| Variable | n (%) | P value | OR | 95% CI | ||
|---|---|---|---|---|---|---|
| Case | Control | Lower | Upper | |||
| Place of residence | ||||||
| Fassa | 33 (75.0) | 42 (38.2) | <0.0001 | 4.857 | 2.219 | 10.631 |
| Rogh/Amk | 11 (25.0) | 68 (61.8) | ||||
| Source of drinking water | ||||||
| Common tank | 40 (90.9) | 95 (86.4) | 0.590 | 1.579 | 0.493 | 5.053 |
| Other | 4 (9.1) | 15 (13.6) | ||||
| Use of water filters | ||||||
| No | 4 (9.1) | 16 (14.5) | 0.437 | 0.558 | 0.185 | 1.867 |
| Yes | 40 (90.9) | 94 (85.5) | ||||
| Type of filters* | ||||||
| Candle | 4 (10.0) | 11 (11.7) | >0.05 | 0.838 | 0.250 | 2.810 |
| Electrical | 36 (90.0) | 83 (2.8) | ||||
| Frequency of changing water filters* | ||||||
| At least once in six months | 3 (7.9) | 7 (7.3) | >0.05 | 1.090 | 0.267 | 4.454 |
| Not changed | 35 (92.1) | 89 (92.7) | ||||
| Water boiled/cooled before drinking† | ||||||
| No | 42 (95.5) | 106 (97.2) | 0.626 | 0.594 | 0.096 | 3.685 |
| Yes | 2 (4.5) | 3 (2.8) | ||||
| Frequency of cleaning water tank | ||||||
| Not clean | 14 (33.3) | 22 (18.6) | 0.095 | 1.955 | 0.883 | 4.325 |
| At least once in six months | 28 (66.7) | 86 (81.4) | ||||
| Hand hygiene practices | ||||||
| Average/unsatisfactory | 5 (11.4) | 1 (0.9) | 0.008 | 13.974 | 1.583 | 123.369 |
| Good | 39 (88.6) | 109 (99.1) | ||||
| Washing fruit/vegetables before consumption | ||||||
| No | 2 (4.5) | 0 (0.0) | 0.080 | 0.276 | 0.214 | 0.357 |
| Yes | 42 (95.5) | 110 (100.0) | ||||
| Fresh preparation of food before consumption | ||||||
| No | 4 (9.1) | 7 (6.4) | 0.511 | 1.471 | 0.408 | 5.301 |
| Yes | 40 (90.9) | 103 (93.6) | ||||
| Waste collection container | ||||||
| Open | 26 (59.1) | 67 (60.9) | 0.835 | 0.927 | 0.455 | 1.891 |
| Closed | 18 (40.9) | 43 (39.1) | ||||
| Presence of house flies† | ||||||
| Yes | 22 (50.0) | 43 (39.4) | 0.232 | 1.535 | 0.759 | 3.106 |
| No | 22 (50.0) | 66 (60.6) | ||||
| Presence of septic tank | ||||||
| No | 0 (0.0) | 5 (4.5) | 0.322 | 0.000 | 0.000 | 0.000 |
| Yes | 44 (100.0) | 105 (95.5) | ||||
Total number of households for these variables was 134 as 20 households did not use water filters.
Total number of households for this variable was 153 due to missing data for one household.
Not changing water filters regularly increased the odds of being a case household but was not statistically significant (OR = 1.090, 95% CI = 0.267–4.454; P >0.05). Water tanks in 33.3% of case and 18.6% of control households had not been cleaned in the previous six months. While the risk of shigellosis was 1.95 times greater among these households (OR = 1.955, 95% CI = 0.883–4.325) compared to those who had cleaned their water tanks at least once during that time period, this was not statistically significant (P = 0.095). When hand hygiene practices were compared, there was a statistically significant risk of acute gastroenteritis among households with average or unsatisfactory hand hygiene practices (P = 0.008). The risk was 13.97 times higher in these households than in those with good hand hygiene practices.
The risk of acute gastroenteritis occurring in a household was 1.47 times higher in residences where food was not freshly prepared compared to those who habitually consumed fresh food (OR = 1.471, 95% CI = 0.408–5.301; P = 0.511). The presence of houseflies increased the risk of shigellosis by 1.5 (OR = 1.535, 95% CI = 0.759–3.106; P = 0.232). These were not statistically significant.
Discussion
Shigellosis is a highly infectious diarrhoeal disease that can lead to explosive, common source or prolonged propogated epidemics.9–14 Studies have linked unboiled water, contaminated food and household contact with shigellosis.15–18 The current study sought to determine the cause of an outbreak of shigellosis occuring in August 2012 in Al Batinah South Governorate, Oman.
Waterborne outbreaks of shigellosis are relatively common. Arias et al. investigated the relationship between an outbreak of S. sonnei and water supplied by the municipal network of Santa Maria de Palautordera in Catalonia, Spain.19 Although the causal agent was not isolated from the water samples taken, various other factors—such as the attack rate (a biostatistical measure of the speed of spread in an at-risk population) and evidence from environmental investigations which showed that the levels of free residual chlorine in the water were not sufficient to prevent the contamination of the water network—suggested that it was a waterborne outbreak.19 A case-control study in Sichuan Province, China, established that a shigellosis outbreak in a rural elementary school was associated with a contaminated well.5 The well was shallow, constructed with stones and one metre away from a pond. Sewage from the school and the surrounding farms was discharged directly into the pond without treatment. The untreated well water was found to yield S. flexneri serotype 2b.5
In the 2012 outbreak in Al Batinah South Governorate, water samples were collected from the villages affected by acute gastroenteritis and tested by disease control specialists.7 The unsatisfactory results of the water samples, which were due to the presence of coliform bacilli and E. coli, were communicated to municipality officials.7,8 Measures were taken to supply an alternate source of drinking water until the common water storage and supply sources were disinfected and the water was fit for consumption again.7 The common water supply source for the three villages and evidence of faecal contamination (due to the presence of coliforms) from bacteriological examinations by the Ministry of Health in Rustaq of drinking water samples collected from households, a publicly accessible community water cooler and a mosque indicate that this shigellosis outbreak was probably waterborne.8 Unfortunately, the exact point of contamination could not be identified. Shigella bacteria are difficult to culture from water and isolation from water is unusual.20–22
The current case-control study investigated other exposures which could have caused this outbreak of shigellosis. No significant differences were found between case and control households with regards to exposure variables related to sources of or practices related to drinking water. Only residence in Fassa and average hand hygiene practices were associated with an increased risk of acute gastroenteritis and statistically significant odds of a household being a case household. It is important to note that the three water samples which were found to have coliforms were collected from Fassa.8 Furthermore, Fassa was the nearest village to the common water source.7 All of the individuals with average hand hygiene practices also lived in Fassa. Therefore, some degree of person-to-person infection could have occurred. A systemic review by Curtis et al. demonstrated that handwashing could reduce the risk of severe intestinal infections by 48% and of shigellosis by 59%.23 Health education on the importance of maintaining hand hygiene before and after food consumption and after toilet use should therefore be provided to households in the wilayat of Rustaq by health educators and community support group members.
Critically, the current study found that drinking water was boiled and cooled in only 3.2% of households before consumption. This could have been because the majority of households used filters to purify water. Infrequent cleaning of water tanks and changing of water filters as well as the use of open waste collection containers were also observed in the interviewed households. These are all factors that introduce a greater risk of acute gastroenteritis.24–26 The importance of regularly cleaning overhead tanks, changing water filters, using closed containers to collect household waste, emptying full septic tanks and maintaining general hygiene in household surroundings should be stressed in this community setting. Additionally, common houseflies are mechanical vectors of Shigella and, as these organisms cohabitate with humans, they can readily contaminate food and eating utensils.27 Waste collected less frequently than every 14 days (the average life cycle of the common housefly) places residents at risk of contracting acute gastroenteritis. Findings from the current study suggest that municipal waste collection in the wilayat of Rustaq needs to be done regularly and at more frequent intervals.
In a study in First Nation reserves in Manitoba, Canada, Rosenberg et al. found that a lack of piped water and inadequate sewage disposal were significantly associated with an increased incidence of shigellosis.28 When compared to communities with piped water, the rate ratio for shigellosis was 6.0 (95% CI = 3.5–9.1) in communities where trucks delivered water to water barrels, while areas in which 50% of the houses did not have sewage removal had a rate ratio of 2.0 (95% CI = 1.6–2.6) compared with other communities.28 In the current study, the majority of households in the three villages had never emptied their septic tanks. This introduces the possibility that the contents of septic tanks may be diffusing underground and causing underground contamination, since most septic tanks are not leak-proof. With this scenario, a high chance of contaminating drinking water sources exists if there is a break in the water pipeline. Hence, the public should be made aware of the importance of installing leak-proof septic tanks and carrying out regular cleaning.
The current study is subject to a number of limitations. As the frequency of shigellosis cases had declined by the end of August 2012 and interviews were conducted nearly a month after the initial outbreak, there could have been a recall bias. Mild and asymptomatic cases and individuals who did not seek medical care may not have been identified during the interview process, resulting in the potential misclassification of case and control households. For questions related to water, food and environmental hygiene practices, interviewees could have indicated that they were following well-known ‘good’ practices, even if this was not the case. This self-reporting bias could have impacted the significance of findings between case and control households. The contribution of certain demographic characteristics like age and gender to the outbreak of shigellosis was not assessed as the study intended to compare households only and not individuals. These demographic variables could have impacted the findings.
Conclusion
This is the first study conducted in Oman on a shigellosis outbreak in a community setting. Possible exposure variables behind the shigellosis outbreak in three villages in the wilayat of Rustaq in Oman were assessed. The only variables that were significantly associated with an increased risk of contracting acute gastroenteritis were residence in Fassa and average hand hygiene practices. No significant difference between households with acute gastroenteritis cases and those without cases were noted with regards to other exposure avenues, including sources of drinking water and practices related to drinking water, food preparation and environmental sanitation. While the source of the outbreak could not be identified, the study found that practices related to water tank and septic tank maintenance and the consumption of freshly cooked food were not satisfactory in these villages. These need to be addressed regularly to prevent similar outbreaks of acute gastroenteritis in this community in the future.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Sjölund Karlsson M, Bowen A, Reporter R, Folster JP, Grass JE, Howie RL, et al. Outbreak of infections caused by Shigella sonnei with reduced susceptibility to azithromycin in the United States. Antimicrob Agents Chemother. 2013;57:1559–60. doi: 10.1128/AAC.02360-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saha T, Murhekar M, Hutin YJ, Ramamurthy T. An urban, water-borne outbreak of diarrhoea and shigellosis in a district town in eastern India. Natl Med J India. 2009;22:237–9. [PubMed] [Google Scholar]
- 3.el Bushra HE, Bin Saeed AA. Intrafamilial person-to-person spread of bacillary dysentery due to Shigella dysenteriae in southwestern Saudi Arabia. East Afr Med J. 1999;76:255–9. [PubMed] [Google Scholar]
- 4.Guzman-Herrador B, Vold L, Comelli H, MacDonald E, Heier BT, Wester AL, et al. Outbreak of Shigella sonnei infection in Norway linked to consumption of fresh basil. Euro Surveill. 2011;16:20007. [PubMed] [Google Scholar]
- 5.He F, Han K, Liu LG, Sun W, Zhang LJ, Zhu B, et al. Shigellosis outbreak associated with contaminated well water in a rural elememtary school: Sichuan Province, China, June 7–16, 2009. PloS One. 2012;7:e47239. doi: 10.1371/journal.pone.0047239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Planning, Al Batinah South Governorate, Oman Ministry of Health . Wadi Sahtan catchment population 2012: Estimated population based on population data from the National Center for Statistics and Information (NCSI) Al Batinah South. Oman: Oman Ministry of Health; 2012. [Google Scholar]
- 7.Vaidya SK. Gastroenteritis cases in Oman village on decline: Ffah village in Rustaq area hit by outbreak believed to be due to water supply. Gulf News. From: www.m.gulfnews.com/news/gulf/oman/gastroenteritis-cases-in-oman-village-on-decline-1.1068296 Accessed: Jan 2015.
- 8.Department of Laboratories, Directorate General of Health Affairs, Oman Ministry of Health . Bacteriological examination of water samples: Laboratory reports 1–7 #M-168 Al Batinah South. Oman: Oman Ministry of Health; 2012. [Google Scholar]
- 9.Levine MM, DuPont HL, Formal SB, Hornick RB, Takeuchi A, Gangarosa EJ, et al. Pathogenesis of Shigella dysenteriae 1 (Shiga) dysentery. J Infect Dis. 1973;127:261–70. doi: 10.1093/infdis/127.3.261. [DOI] [PubMed] [Google Scholar]
- 10.Egoz N, Shmilovitz M, Kretzer B, Lucian M, Porat V, Raz R. An outbreak of Shigella sonnei infection due to contamination of a municipal water supply in northern Israel. J Infect. 1991;22:87–93. doi: 10.1016/0163-4453(91)91122-E. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control (CDC) Hospital-associated outbreak of Shigella dysenteriae type 2: Maryland. MMWR Morb Mortal Wkly Rep. 1983;32:250–2. [PubMed] [Google Scholar]
- 12.Benny E, Mesere K, Pavlin BI, Yakam L, Ford R, Yoannes M, et al. A large outbreak of shigellosis commencing in an internally displaced population, Papua New Guinea, 2013. Western Pac Surveill Response J. 2014;5:18–21. doi: 10.5365/WPSAR.2014.5.2.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sorvillo FJ, Waterman SH, Vogt JK, England B. Shigellosis associated with recreational water contact in Los Angeles County. Am J Trop Med Hyg. 1988;38:613–17. doi: 10.4269/ajtmh.1988.38.613. [DOI] [PubMed] [Google Scholar]
- 14.Mahoney FJ, Farley TA, Moriniere BJ, Winsor DK, Silberman RL, McFarland LM. Evaluation of an intervention program in the control of an urban outbreak of shigellosis. Am J Prev Med. 1991;7:292–7. [PubMed] [Google Scholar]
- 15.Taylor DN, Bodhidatta L, Brown JE, Echeverria P, Kunanusont C, Naigowit P, et al. Introduction and spread of multi-resistant Shigella dysenteriae I in Thailand. Am J Trop Med Hyg. 1989;40:77–85. doi: 10.4269/ajtmh.1989.40.77. [DOI] [PubMed] [Google Scholar]
- 16.Swaddiwudhipong W, Karintraratana S, Kavinum S. A common-source outbreak of shigellosis involving a piped public water supply in northern Thai communities. J Trop Med Hyg. 1995;98:145–50. [PubMed] [Google Scholar]
- 17.Hoge CW, Bodhidatta L, Tungtaem C, Echeverria P. Emergence of nalidixic acid resistant Shigella dysenteriae type 1 in Thailand: An outbreak associated with consumption of a coconut milk dessert. Int J Epidemiol. 1995;24:1228–32. doi: 10.1093/ije/24.6.1228. [DOI] [PubMed] [Google Scholar]
- 18.Gaudio PA, Sethabutr O, Echeverria P, Hoge CW. Utility of a polymerase chain reaction diagnostic system in a study of the epidemiology of shigellosis among dysentery patients, family contacts, and well controls living in a shigellosis-endemic area. J Infect Dis. 1997;176:1013–18. doi: 10.1086/516531. [DOI] [PubMed] [Google Scholar]
- 19.Arias C, Sala MR, Domínguez A, Bartolomé R, Benavente A, Veciana P, et al. Waterborne epidemic outbreak of Shigella sonnei gastroenteritis in Santa Maria de Palautordera, Catalonia, Spain. Epidemiol Infect. 2006;134:598–604. doi: 10.1017/S0950268805005121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morera MA, Espejo E, Coll P, Simó M, Uriz MS, Llovet T, et al. [Epidemic outbreak of shigellosis following water intake] Enferm Infecc Microbiol Clin. 1995;13:160–5. [PubMed] [Google Scholar]
- 21.Samonis G, Elting L, Skoulika E, Maraki S, Tselentis Y. An outbreak of diarrhoeal disease attributed to Shigella sonnei. Epidemiol Infect. 1994;112:235–45. doi: 10.1017/S0950268800057642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention (CDC) Shigellosis outbreak associated with an unchlorinated fill-and-drain wading pool—Iowa, 2001. MMWR Morb Mortal Wkly Rep. 2001;50:797–800. [PubMed] [Google Scholar]
- 23.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect Dis. 2003;3:275–81. doi: 10.1016/S1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 24.Weissman JB, Craun GF, Lawrence DN, Pollard RA, Saslaw MS, Gangarosa EJ. An epidemic of gastroenteritis traced to a contaminated public water supply. Am J Epidemiol. 1976;103:391–8. doi: 10.1093/oxfordjournals.aje.a112238. [DOI] [PubMed] [Google Scholar]
- 25.Mwabi JK, Mamba BB, Momba MN. Removal of Escherichia coli and faecal coliforms from surface water and ground water by household water treatment devices/systems: A sustainable solution for improving water quality in rural communities of the Southern African development community region. Int J Environ Res Public Health. 2012;9:139–70. doi: 10.3390/ijerph9010139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gebru T, Taha M, Kassahun W. Risk factors of diarrhoeal disease in under-five children among health extension model and non-model families in Sheko district rural community, Southwest Ethiopia: Comparative cross-sectional study. BMC Public Health. 2014;14:395. doi: 10.1186/1471-2458-14-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levine OS, Levine MM. Houseflies (Musa domestica) as mechanical vectors of shigellosis. Rev Infect Dis. 1991;13:688–96. doi: 10.1093/clinids/13.4.688. [DOI] [PubMed] [Google Scholar]
- 28.Rosenberg T, Kendall O, Blanchard J, Martel S, Wakelin C, Fast M. Shigellosis on Indian reserves in Manitoba, Canada: Its relationship to crowded housing, lack of running water, and inadequate sewage disposal. Am J Public Health. 1997;87:1547–51. doi: 10.2105/AJPH.87.9.1547. [DOI] [PMC free article] [PubMed] [Google Scholar]