Abstract
Vitamin B12 deficiency is common in developing countries and should be suspected in patients with unexplained anaemia or neurological symptoms. Dermatological manifestations associated with this deficiency include skin hyper- or hypopigmentation, angular stomatitis and hair changes. We report a case of a 28-year-old man who presented to the Sultan Qaboos University Hospital in Muscat, Oman, in November 2013 with localised hyperpigmentation of the palmar and dorsal aspects of both hands of two months’ duration. Other symptoms included numbness of the hands, anorexia, weight loss, dizziness, fatigability and a sore mouth and tongue. There was no evidence of hypocortisolaemia and a literature search revealed a possible B12 deficiency. The patient had low serum B12 levels and megaloblastic anaemia. An intrinsic factor antibody test was negative. A gastric biopsy revealed chronic gastritis. After B12 supplementation, the patient’s symptoms resolved. Family physicians should familiarise themselves with atypical presentations of B12 deficiency. Many symptoms of this deficiency are reversible if detected and treated early.
Keywords: Vitamin B12 Deficiency, Hyperpigmentation, Atrophic Gastritis, Case Report, Oman
Vitamin B12 deficiency is common among individuals in developing countries.1 Its prevalence is often underestimated as it is believed to occur only in strict vegetarians and patients with pernicious anaemia.1 However, vitamin B12 deficiency should be suspected in all patients with unexplained anaemia or neurological symptoms.2 Various dermatological manifestations associated with B12 deficiency are skin hyper- or hypopigmentation, angular stomatitis and hair changes.3 Hyperpigmentation as the primary presenting symptom of B12 deficiency is rarely reported in the literature.4 The case reported below describes a 28-year-old Omani man who presented with brownish-black hyperpigmentation on both hands, which proved to be due to a B12 deficiency caused by chronic atrophic gastritis.
Case Report
A 28-year-old Omani male presented to Sultan Qaboos University Hospital (SQUH) in Muscat, Oman, in November 2013 with hyperpigmentation of both hands. Two months later he developed severe numbness in both hands to the extent that he could no longer carry objects. On further enquiry, he reported symptoms of glossitis and angular stomatitis for the preceding two weeks. He had lost 10 kg within one month (with an initial weight of 86 kg) and was experiencing anorexia, feelings of excessive fatigability and dizziness. His past medical, medication and dietary history was unremarkable. There was no previous history of fever, epigastric pain, diarrhoea, steatorrhea, diabetes mellitus, tuberculosis or use of any over-the-counter medications.
A clinical examination revealed a diffuse brownish-black discolouration on both the palmar and dorsal aspects of both hands which was more pronounced at the distal and proximal interphalangeal joints [Figure 1A & B]. There was ulceration on both sides of the tongue with angular stomatitis. No abnormal pigmentation was found on any other site of the skin or on the buccal mucosa. On neurological examination, the patient was unable to feel a 10 g monofilament on either hand; however, he could feel vibration on the hands and his proprioception was intact. The patient had brisk reflexes in the upper limbs but diminished reflexes in the lower limbs. The plantar reflexes were equivocal and Romberg’s test results were negative. The rest of the physical examination was normal. Serum cortisol and adrenocorticotropic hormone levels were normal, ruling out Addison’s disease. A complete blood count showed macrocytosis with megaloblastic features, although his haemoglobin level was normal [Figure 2].
Figure 1A–D:
Diffuse brownish-black hyperpigmentation on the (A) dorsal and (B) palmar aspects of both hands at presentation. Improved (C) dorsal and (D) palmar hyperpigmentation was noted after vitamin B12 supplementation.
Figure 2A & B:
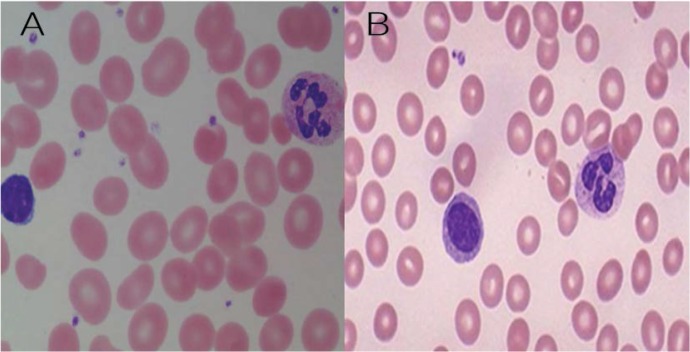
May-Grünwald-Giemsa stain at ×40 magnification showing blood cell morphology (A) before and (B) after treatment with vitamin B12.
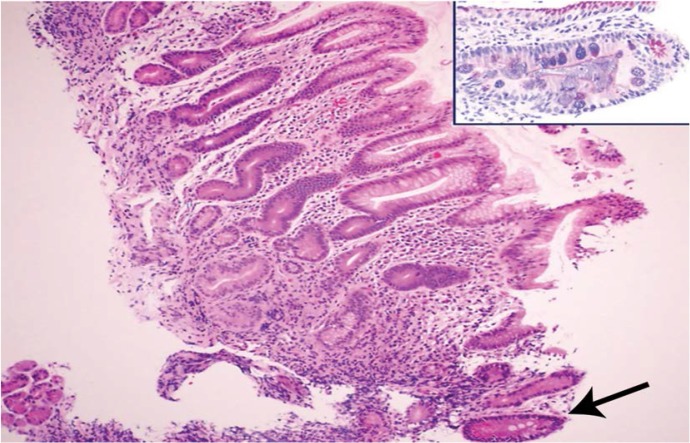
The patient’s B12 and folate levels were subsequently assessed; his B12 level was found to be significantly low [Table 1]. As B12 plays a pivotal role in many metabolic pathways, further metabolic work-up showed high levels of both methylmalonic acid and homocystiene. Multiple biopsies from an endoscopy were consistent with a fungal infection at the lower end of the oesophagus and chronic gastritis including focal intestinal metaplasia without any evidence of Helicobacter pylori [Figure 3]. The duodenal biopsy also revealed mild chronic inflammation and focal villous blunting. An autoimmune work-up was negative, including antiparietal cell, intrinsic factor antibody (IFA), transglutaminase and anti-gliadin antibody tests. A skin biopsy of the hyperpigmented lesions showed dermal vessels with mild lymphocytic cuffing and ectatic capillaries.
Table 1:
Summary of haematological, biochemical and other investigation results for the current patient with localised skin hyperpigmentation
| Investigation | Value | Normal range |
|---|---|---|
| Haemoglobin | 12.2 g/dL | 11.5–15.5 g/dL |
| Mean corpuscular volume | 115 fL ↑↑ | 78–96 fL |
| Red cell distribution width | 17.2% ↑ | 11.5–16.5% |
| C-reactive protein | 2 mg/L | 0–8 mg/L |
| Vitamin B12 | 75 pmol/L ↓↓ | 133–675 pmol/L |
| Folate | 20.4 mmol/L | 7.0–45.1 mmol/L |
| Cortisol at 10 am | 422 nmol/L | 185–624 nmol/L |
| Adrenocorticotropic hormone at 8 am | 98 ug/L | 24–336 ug/L |
| Homocysteine plasma | 36 µmol/L ↑↑ | <15 µmol/L |
| Methylmalonic acid | 3.4 µmol/L ↑↑ | <0.5 µmol/L |
| Anti-deamidated gliadin antibody 1gA and immunoglobulin G | 1 µ/mL | 0–25 µ/mL |
| Transglutaminase antibody immunoglobulin A | 1 µ/mL | 0–20 µ/mL |
| Human immunodeficiency virus serology | Negative | Negative |
Figure 3:
Haematoxylin and eosin stain of a gastric biopsy sample from the antrum showing crypt disarray and moderate chronic inflammation of the lamina propria with foci of intestinal metaplasia (arrow) at ×100 magnification. Inset: Periodic acid-Schiff-alcian blue stain showing foci of intestinal metaplasia with alcianophilic mucinous cells at ×400 magnification.
The patient was prescribed 1,000 µg of intramuscular B12 every day for one week, followed by the same dose once a week for four weeks and then once a month for two months. Following the treatment, the patient underwent remarkable symptomatic improvement. His skin pigmentation completely normalised within eight weeks of treatment with B12 [Figure 1C & D].
Written informed consent was obtained from the patient for publication of this case report and the accompanying images.
Discussion
Vitamin B12 deficiency was considered to be the cause of localised hyperpigmentation in the reported patient, due to the fact that the hyperpigmentation disappeared following the normalisation of serum B12 levels with treatment. The most common causes of B12 deficiency are either a strict vegetarian diet or malabsorption of B12 due to inadequate gastric production or defective functioning of IFA.1,2 Other causes include a gastrectomy, surgical resection of the terminal ileum, bacterial overgrowth of the small intestine, diverticulitis, coeliac disease, Crohn’s disease, chronic alcoholism, human immunodeficiency virus, Diphyllobothrium infestation, giardiasis and medications such as metformin and colchicine.1,2 In addition, malabsorption of B12 has been associated with long-term (>4 years) use of histamine type 2 receptor antagonists and proton-pump inhibitors.5 Of these potential causes of B12 deficiency, the only one applicable to this patient was the possibility of inadequate IFA production by the stomach due to histologically-proven chronic atrophic gastritis.
Amarapurkar et al. reported that there was no statistically significant difference in haematological, biochemical and histological parameters in IFA-positive and IFA-negative gastritis.6 These may be part of the spectrum for the same disease, with H. pylori as the agent responsible for initiating the process. It has been reported that patients who are IFA-negative are classified as chronic atrophic gastritis cases.6 In the current patient, the associated Candida infection at the lower part of the oesophagus may also be explained by a B12 deficiency, as vitamin B group deficiencies have been reported as one of the causes for a Candida albicans infection.7
Pigmentation in B12 deficiency can also masquerade as pigmentation due to Addison’s disease.4,8–12 There are few reported cases of vitamin B12 deficiency in which mucocutaneous lesions predate other manifestations.4,8–12 In these cases, the skin changes were characterised by Addisonian brownish-black hyperpigmentation which affected more than one area of the body, including sun-exposed sites, such as the palmar and dorsal aspects of the hands and feet and the knuckles, flexures, tongue, oral mucosa, palmar creases, nails and gluteal region.4,8–12 The pigmentation observed in the current patient differs from these reported cases in that it was localised only to the hands, which may possibly be due to an early diagnosis of the condition. Kannan et al. described a similar case of B12 deficiency where the patient presented over a short period of time (1.5 months) with localised hyperpigmented macular lesions on the dorsum of the middle phalanges of both feet.3
From the current case, it is obvious that skin signs and symptoms, specifically hyperpigmentation, can precede the typical neurological signs and symptoms of B12 deficiency. Mori et al. proposed that skin hyperpigmentation can be an important clue in diagnosing B12 deficiency and that dermatologists need to be familiar with the clinical appearance of this disorder.10 The mechanism of hyperpigmentation is not well understood. It has been suggested that the lack of B12 causes depletion in intracellular glutathione levels which normally inhibit tyrosinase activity in melanogenesis; the lack of this inhibitor would lead to an increase in melanogenesis.13 Mori et al. reported that the dominant mechanism of hyperpigmentation due to B12 deficiency is not a defect in melanin transport but rather an increase in melanin synthesis.10
Conclusion
B12 deficiency should be considered as an underlying cause of unexplained hyperpigmentation. In the current case, a patient presented with localised hyperpigmentation of the palmar and dorsal aspects of both hands which resolved rapidly after B12 supplementation. It is essential for family physicians to familiarise themselves with atypical presentations of B12 deficiency, as early detection and adequate treatment of the condition can prevent neurological complications.
References
- 1.Allen LH. How common is vitamin B-12 deficiency. Am J Clin Nutr. 2009;89:693S–6S. doi: 10.3945/ajcn.2008.26947A. [DOI] [PubMed] [Google Scholar]
- 2.Hvas AM, Nexo E. Diagnosis and treatment of vitamin B12 deficiency: An update. Haematologica. 2006;91:1506–12. [PubMed] [Google Scholar]
- 3.Kannan R, Ng MJ. Cutaneous lesions and vitamin B12 deficiency: An often-forgotten link. Can Fam Physician. 2008;54:529–32. [PMC free article] [PubMed] [Google Scholar]
- 4.Jithendriya M, Kumaran S, P IB. Addisonian pigmentation and vitamin B12 deficiency: A case series and review of the literature. Cutis. 2013;92:94–9. [PubMed] [Google Scholar]
- 5.Allen LH. Causes of vitamin B12 and folate deficiency. Food Nutr Bull. 2008;29:S20–34. doi: 10.1177/15648265080292S105. [DOI] [PubMed] [Google Scholar]
- 6.Amarapurkar DN, Amarapurkar AD. Intrinsic factor antibody negative atrophic gastritis: Is it different from pernicious anaemia? Trop Gastroenterol. 2010;31:266–70. [PubMed] [Google Scholar]
- 7.Akpan A, Morgan R. Oral candidiasis. Postgrad Med J. 2002;78:455–9. doi: 10.1136/pmj.78.922.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agrawala RK, Sahoo SK, Choudhury AK, Mohanty BK, Baliarsinha AK. Pigmentation in vitamin B12 deficiency masquerading Addison’s pigmentation: A rare presentation. Indian J Endocrinol Metab. 2013;17:S254–6. doi: 10.4103/2230-8210.119591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoffman CF, Palmer DM, Papadopoulos D. Vitamin B12 deficiency: A case report of ongoing cutaneous hyperpigmentation. Cutis. 2003;71:127–30. [PubMed] [Google Scholar]
- 10.Mori K, Ando I, Kukita A. Generalized hyperpigmentation of the skin due to vitamin B12 deficiency. J Dermatol 200l. 28:282–5. doi: 10.1111/j.1346-8138.2001.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 11.Cherqaoui R, Husain M, Madduri S, Okolie P, Nunlee-Bland G, Williams J. A reversible cause of skin hyperpigmentation and postural hypotension. Case Rep Hematol. 2013;2013:680459. doi: 10.1155/2013/680459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Srivastava N, Chand S, Bansal M, Srivastava K, Singh S. Reversible hyperpigmentation as the first manifestation of dietary vitamin B12 deficiency. Indian J Dermatol Venereol Leprol. 2006;72:389–90. doi: 10.4103/0378-6323.27766. [DOI] [PubMed] [Google Scholar]
- 13.Niiyama S, Mukai H. Reversible cutaneous hyperpigmentation and nails with white hair due to vitamin B12 deficiency. Eur J Dermatol. 2007;17:551–2. doi: 10.1684/ejd.2007.0285. [DOI] [PubMed] [Google Scholar]