Abstract
Posterior reversible encephalopathy syndrome (PRES) is a neurological condition with a combination of clinical and radiological features. Clinical symptoms include headaches, confusion, seizures, disturbed vision or an altered level of consciousness. Classic magnetic resonance imaging (MRI) findings indicate subcortical and cortical oedema, affecting mainly the posterior cerebral region. We report two paediatric cases of PRES with underlying renal diseases presenting at the Sultan Qaboos University Hospital in Muscat, Oman, in April 2010 and August 2011. The first case was an 11-year-old girl diagnosed with systemic lupus erythematosus and the second was a six-and-a-half-year-old boy on peritoneal dialysis due to multi-drug-resistant nephrotic syndrome. Both patients were hypertensive and treated with blood pressure control medications. No residual neurological dysfunction was noted in the patients at a one-year follow-up and at discharge, respectively. The role of hypertension in paediatric PRES cases, among other important risk factors, is emphasised. Additionally, MRI is an important diagnostic and prognostic tool. Prompt diagnosis and aggressive management is fundamental to preventing permanent neurological damage.
Keywords: Posterior Reversible Encephalopathy Syndrome, Pediatrics, Peritoneal Dialysis, Systemic Lupus Erythematosus, Magnetic Resonance Imaging, Case Report, Oman
Posterior reversible encephalopathy syndrome (PRES) is a neurological condition that combines a number of clinical and radiological features. Clinical symptoms include headaches, confusion, seizures, disturbed vision and an altered level of consciousness.1 The classic magnetic resonance imaging (MRI) findings are subcortical and cortical oedema, mainly affecting the posterior cerebral region.2
The following two cases are, to the best of the authors’ knowledge, the first reported cases of paediatric PRES with underlying renal diseases in the Omani population. The aim of this report was to increase awareness among physicians and emphasise early recognition of this condition in order to improve management and outcomes. Common renal risk factors that may cause PRES are also elucidated, as well as the important role of MRI as a diagnostic and prognostic tool.
Case 1
An 11-year-old girl with systemic lupus erythematosus (SLE) presented to the Sultan Qaboos University Hospital (SQUH) in Muscat, Oman, in October 2009. The immunological diagnosis of SLE was confirmed by positive tests for antinuclear, anti-double-stranded DNA, anti-histone and anti-Smith antibodies. Pathology assessment of a renal biopsy indicated class IV diffuse lupus nephritis with a focal crescent formation.
The course of the first six months of the illness was severe. Initially, she responded to mycophenolate mofetil, oral prednisolone and hydroxychloroquine. However, the patient had severe hypertension which was difficult to control. This was eventually regulated with four antihypertensive medications (lisionpril, frusemide, hydralazine and amlodipine). The hypertension was monitored at the patient’s local health centre and peripheral hospital.
At a follow-up visit in April 2010, the patient’s blood pressure (BP) was high at 180/100 mmHg (normal age- and gender-matched range: 95th percentile, 119/78 mmHg; 99th percentile, 126/86 mmHg). During the follow-up visit, the patient suddenly developed severe headaches while showing signs of agitation and abnormal behaviour. In addition, she began having generalised tonic-clonic seizures. A central nervous system examination revealed an impaired attention span, good coordination and normal cranial nerve activity. No meningeal or cerebellar signs and no focal neurological deficit were observed. However, there was a marked weakness in the proximal muscle group, which was associated with normal tone and increased reflexes in the lower limbs. An eye examination showed equal pupils reactive to light, while a fundus examination showed small retinal and conjunctival haemorrhages with no signs of papilloedema. Other clinical systemic examinations were normal. The child was admitted to the SQUH Paediatric Intensive Care Unit (PICU) for respiratory support, due to recurrent seizures that led to altered sensorium. In addition, she had very high BP readings (200/130 mmHg) [Table 1].
Table 1:
Summary of the clinical characteristics and risk factors for the two presented patients with posterior reverse encephalopathy syndrome
| Characteristic | Case one | Case two |
|---|---|---|
| Age in years/gender | 11/female | 6.5/male |
| Diagnosis | SLE with multisystem involvement | ESRD on renal replacement therapy and CAPD |
| Clinical findings | Headaches, partial seizures, agitated behaviour and altered sensorium | Headaches and partial seizures |
| SBP in mmHg | 200 | 180 |
| DBP in mmHg | 130 | 120 |
| Risk factors | Hypertension, cyclophosphamide and steroid use | Hypertension and renal failure |
SLE = systemic lupus erythematous; ERSD = end-stage renal disease; CAPD = continuous ambulatory peritoneal dialysis; SBP = systolic blood pressure; DBP = diastolic blood pressure.
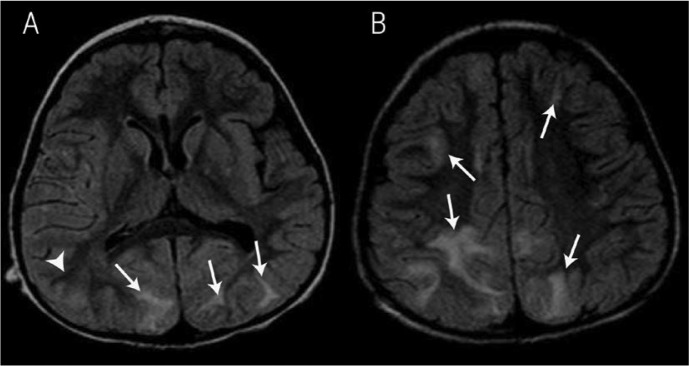
The differential diagnosis for the patient included hypertensive encephalopathy, intracranial bleeding, a cerebrovascular stroke and cerebral vasculitis. On admission to the PICU, urgent brain scans were performed in order to correlate the patient’s clinical deterioration and neurological manifestations. Initial MRI brain examinations revealed hyperintense areas in the bilateral cortical and subcortical white matter, observed at the frontal-parietal and parietal-occipital junctions. Mild cortical involvement was also noted [Figure 1]. Diffusion images and apparent diffusion coefficient mapping displayed no evidence of diffusion restriction. The radiological findings indicated a diagnosis of PRES.
Figure 1A & B:

Axial fluid-attenuated inversion recovery magnetic resonance images of an 11-year-old girl diagnosed with systemic lupus erythematosus showing bilateral cortical and subcortical white matter. Hyperintense areas can be seen in the frontal, posterior temporal, parietal and occipital regions (arrows). Based on clinical and radiological findings, a diagnosis of posterior reversible encephalopathy syndrome was made.
Electroencephalography showed bilateral slow wave activity and no epileptic discharges. The laboratory investigations indicated anaemia with a haemoglobin level of 10 g/dL, a normal coagulation profile and the following other blood levels: sodium of 138 mmol/L (normal range: 135–145 mmol/L); potassium of 3.5 mmol/L (normal range: 2.5–5.1 mmol/L); creatinine of 45 μmol/L (normal range: 15–31 μmol/L); urea of 6.5 mmol/L (normal range: 2.1–7.1 mmol/L); calcium of 2.45 mmol/L (normal range: 2.15–2.55 mmol/L); and serum magnesium of 0.9 mmol/L (normal range 0.7–0.95 mmol/L).
Methylprednisolone and low-dose cyclophosphamide were prescribed for the control of SLE activity and labetalol and hydralazine infusions were administered for BP control. The patient was weaned from the ventilator after the hypertension had been controlled and she was shifted gradually to oral antihypertensive medications. A follow-up MRI showed a significant improvement, with residual abnormally hyperintense areas at the superior frontal and left parietal regions. Clinical and radiological assessments after one year showed no residual neurological dysfunction.
Case 2
A six-and-a-half-year-old boy presented to SQUH in Muscat, Oman, in August 2011 with end-stage renal disease secondary to multi-drug-resistant nephrotic syndrome. The diagnosis of nephrotic syndrome had been established at the age of 14 months when the patient presented to a regional hospital in Oman with proteinuria, haematuria and hypertension. He showed no response to pulse methylprednisolone, cyclophosphamide or mycophenolate mofetil. The patient started continuous ambulatory peritoneal dialysis at the age of six years due to a progressive deterioration of renal function, fluid overload and hypertension. He continued on dialysis for six months with other renal replacement medications, including vitamin D and darbepoetin alfa.
The child presented to SQUH with hypertension, generalised oedema, depressed sensorium and generalised tonic-clonic convulsions. BP readings were very high, reaching 180/120 mmHg. While in a state of disturbed consciousness, he was intubated and ventilated in order to secure his respiratory airway. The differential diagnosis was hypertensive or uremic encephalopathy, intracranial bleeding and a cerebrovascular stroke.
In August 2011, the child was transferred with assisted mechanical ventilation to the Department of Child Health at SQUH. On initial clinical assessment, the patient showed signs of dehydration with fair peripheral perfusion and warm extremities. His apex beat was forceful with normal heart sounds, a grade two ejection systolic murmur at the base of the heart and no gallop rhythm. There were no signs suggestive of cardiac failure and no evidence of pericardial effusion. The chest was clear with no crepitation. The central nervous system exam showed no neurological deficits and normal bilateral deep tendon reflexes. A fundus examination showed grade one hypertensive retinopathy.
Laboratory investigations revealed anaemia with a haemoglobin level of 7 g/dL, a normal coagulation profile, normal inflammatory markers and the following other blood levels: sodium of 123 mmol/L (normal range: 135–145 mmol/L); potassium of 3.2 mmol/L (normal range: 2.5–5.1 mmol/L); creatinine of 586 μmol/L (normal range: 15–31 μmol/L); urea of 15.8 mmol/L (normal range: 2.1–7.1 mmol/L); calcium of 2.3 mmol/L (normal range: 2.15–2.55 mmol/L); and serum magnesium of 0.8 mmol/L (normal range: 0.7–0.95 mmol/L).
Echocardiography showed left ventricular hypertrophy with trivial aortic regurgitation and no pericardial effusion. An initial computed tomography scan showed bilateral hypodense areas at the occipital regions with a vasogenic oedema pattern distribution [Figure 2]. MRI brain images showed typical subcortical white matter areas of oedema at the frontal-parietal-temporal-occipital regions [Figure 3]. Based on the clinical and radiological findings, PRES was suspected.
Figure 2A & B:

Axial non-enhanced computed tomography images of a six-and-a-half-year-old boy on peritoneal dialysis due to multi-drug-resistant nephrotic syndrome and with suspected posterior reversible encephalopathy syndrome. Bilateral subcortical hypodense areas were observed in the occipital and posterior parietal regions (arrows). Similar areas can be seen to a lesser extent in the frontal regions (arrowheads).
Figure 3A & B:
Axial magnetic resonance fluid attenuation inversion recovery images of a six-and-a-half-year-old boy on peritoneal dialysis due to multi-drug-resistant nephrotic syndrome showing bilateral subcortical hyperintense areas, mainly at the frontal-occipital-parietal regions (arrows). Similar areas are also seen at the right posterior temporal region (arrowhead). Based on clinical and radiological findings, a diagnosis of posterior reversible encephalopathy syndrome was made.
Management of the patient’s high BP required a labetalol infusion. After controlling the hypertension, the patient was successfully weaned off the ventilator and was started on oral antihypertensive medications. A neurological examination at the time of discharge was normal.
Both of the patients’ guardians gave consent to use the patients’ medical information and images for scientific purposes.
Discussion
PRES is a neurological syndrome with a combination of clinical and radiological features. Clinical presentations include seizures, headaches, visual disturbance and focal neurological signs.1 Headaches are the main clinical presentation followed by confusion and drowsiness. Focal neurological deficit is an uncommon association with PRES.2 The typical radiological findings are subcortical and cortical oedema in the posterior cerebral regions. Hypertension is the main triggering factor for PRES while other risk factors that predispose to hypertension can also be present.2
PRES is a reversible condition if it is managed early and appropriately, but can otherwise be fatal.1,2 The underlying mechanism that triggers this disease is not well understood and two conflicting theories exist regarding its pathogenesis. Both postulated mechanisms are based on the central role of hypertension. The first theory suggests that hypertension could cause a breakdown of the autoregulatory system in cerebral circulation, leading to brain oedema. According to the second theory, hypertension causes activation of the autoregulatory system, which results in vasoconstriction of the brain vessels with hypoperfusion, ischaemia and subsequent fluid leakage.3,4 However, a large number of patients with PRES do not have hypertension.3,4 Consequently, Marra et al. recently described the endothelial hypothesis; this theory differs from those earlier as it asserts that hypertension does not necessarily have to be present for PRES to develop.4 The hypothesis suggests that an immune-related cascade can cause PRES through the weakening of brain vessels, leading to fluid leakage and oedema.4
PRES has been extensively described in both adults and children. The most common risk factor is a hypertensive crisis.5 Therefore, any condition that predisposes to hypertension can lead to the development of PRES. This includes many renal conditions affecting the glomerulus, such as lupus nephritis;6,7 the renal vessels, such as renal artery stenosis;8 and those conditions with renal anatomical defects such as grade four vesicoureteral reflux.9 In addition, many medications like steroids and cyclosporine can raise BP and therefore increase the risk of PRES.10,11 Patients on dialysis can also develop PRES if they become hypertensive.12,13 Seizures are a common and frequently encountered symptom of PRES, among a wide range of other neurological symptoms.5
In the first case presented in the current report, the patient had multiple risk factors that contributed to the onset of PRES. These included lupus nephritis confirmed by renal biopsy, the use of methylprednisone for disease control and extremely high BP. The patient also presented with headaches, drowsiness and seizures, which are the most common clinical signs of PRES.1 The second case emphasised the role of hypertension in patients on peritoneal dialysis. However, darbepoetin alfa may also be a contributing factor to the development of PRES, as it may have contributed to the raised BP. Both of the cases were managed promptly and appropriately, which led to favourable outcomes for both patients.
MRI can be used as a diagnostic and prognostic tool for PRES. The classic MRI feature in PRES cases is subcortical oedema in the parietal-occipital region.14 However, in recent years, more atypical findings of PRES have been described. Kastrup et al. reported that the frontal region was the area most commonly affected in a study of PRES cases.15 The MRI brain scans of the two patients in the current report confirm this, as the frontal region was involved in both cases. Reversibility of MRI findings is suggestive of a good prognosis.16 Thus, leukoencephalopathy with severe hypertension is reversible both clinically and radiologically in the majority of children after the control of hypertension.17 However, the literature has shown that a few patients may have residual damage and need to be followed-up.17
The present report highlights the role of risk factors such as hypertension in the development of PRES in two paediatric renal cases. Strict monitoring is mandatory for such critical patients, including the use of BP measurement devices with appropriate paediatric cuffs for the child’s age. It is important to recognise such cases early to allow for prompt treatment and potential reversal of the syndrome. The two cases presented here demonstrated that regions other than the posterior brain can be affected in PRES and that MRI is a useful diagnostic tool. More MRI devices are needed in hospitals throughout Oman, as well as more training for physicians in diagnosing typical and atypical forms of PRES. Finally, prompt diagnosis and aggressive management is the cornerstone for the prevention of permanent neurological damage in PRES patients.
Conclusion
Hypertension is known to be one of the most important risk factors leading to PRES but is uncommon among patients with renal diseases. To the best of the authors’ knowledge, these two paediatric PRES cases with underlying renal diseases are the first reported among the Omani population. The findings from these two cases suggest that an increased awareness of effective BP monitoring in peripheral hospitals in Oman is necessary. MRI scanning is also recommended as a valuable diagnostic and prognostic tool. PRES is under-recognised and requires multidisciplinary care because of its potentially severe consequences. Prompt diagnosis and treatment of risk factors are critical in helping to prevent permanent neurological damage among these patients.
References
- 1.McCoy B, King M, Gill D, Twomey E. Childhood posterior reversible encephalopathy syndrome. Eur J Paediatr Neurol. 2011;15:91–4. doi: 10.1016/j.ejpn.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Prasad N, Gulati S, Gupta RK, Sharma K, Gulati K, Sharma RK, et al. Spectrum of radiological changes in hypertensive children with reversible posterior leucoencephalopathy. Br J Radiol. 2007;80:422–9. doi: 10.1259/bjr/81758556. [DOI] [PubMed] [Google Scholar]
- 3.Ishikura K, Hamasaki Y, Sakai T, Hataya H, Mak RH, Honda M. Posterior reversible encephalopathy syndrome in children with kidney diseases. Pediatr Nephrol. 2012;27:375–84. doi: 10.1007/s00467-011-1873-2. [DOI] [PubMed] [Google Scholar]
- 4.Marra A, Vargas M, Striano P, Del Guercio L, Buonanno P, Servillo G. Posterior reversible encephalopathy syndrome: The endothelial hypotheses. Med Hypotheses. 2014;82:619–22. doi: 10.1016/j.mehy.2014.02.022. [DOI] [PubMed] [Google Scholar]
- 5.Chen TH, Lin WC, Tseng YH, Tseng CM, Chang TT, Lin TJ. Posterior reversible encephalopathy syndrome in children: Case series and systematic review. J Child Neurol. 2013;28:1378–86. doi: 10.1177/0883073813500714. [DOI] [PubMed] [Google Scholar]
- 6.Gatla N, Annapureddy N, Sequeira W, Jolly M. Posterior reversible encephalopathy syndrome in systemic lupus erythematosus. J Clin Rheumatol. 2013;19:334–40. doi: 10.1097/RHU.0b013e3182a21ffd. [DOI] [PubMed] [Google Scholar]
- 7.Chan DY, Ong YS. Posterior reversible encephalopathy syndrome: An acute manifestation of systemic lupus erythematous. Singapore Med J. 2013;54:193–5. doi: 10.11622/smedj.2013182. [DOI] [PubMed] [Google Scholar]
- 8.Benoist G, Dossier C, Elmaleh M, Dauger S. Posterior reversible encephalopathy syndrome revealing renal artery stenosis in a child. BMJ Case Rep. 2013;23:2013. doi: 10.1136/bcr-2013-010110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma S, Gupta R, Sehgal R, Aggarwal KC. Atypical presentation of posterior reversible encephalopathy: In a child with bilateral grade IV vesicoureteric reflux. J Trop Pediatr. 2014;60:331–3. doi: 10.1093/tropej/fmu019. [DOI] [PubMed] [Google Scholar]
- 10.İncecik F, Hergüner MÖ, Yıldızdaş D, Yılmaz M, Mert G, Horoz ÖO, et al. Posterior reversible encephalopathy syndrome due to pulse methylprednisolone therapy in a child. Turk J Pediatr. 2013;55:455–7. [PubMed] [Google Scholar]
- 11.Jennane S, Mahtat el M, Konopacki J, Malfuson JV, Doghmi K, Mikdame M, et al. Cyclosporine-related posterior reversible encephalopathy syndrome after cord blood stem cell transplantation. Hematol Oncol Stem Cell Ther. 2013;6:71. doi: 10.1016/j.hemonc.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Girişgen I, Tosun A, Sönmez F, Ozsunar Y. Recurrent and atypical posterior reversible encephalopathy syndrome in a child with peritoneal dialysis. Turk J Pediatr. 2010;52:416–19. [PubMed] [Google Scholar]
- 13.Ermeidi E, Balafa O, Spanos G, Zikou A, Argyropoulou M, Siamopoulos KC. Posterior reversible encephalopathy syndrome: A noteworthy syndrome in end-stage renal disease patients. Nephron Clin Pract. 2013;123:180–4. doi: 10.1159/000353731. [DOI] [PubMed] [Google Scholar]
- 14.Stevens CJ, Heran MK. The many faces of posterior reversible encephalopathy syndrome. Br J Radiol. 2012;85:1566–75. doi: 10.1259/bjr/25273221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kastrup O, Schlamann M, Moenninghoff C, Forsting M, Goericke S. Posterior reversible encephalopathy syndrome: The spectrum of MR imaging patterns. Clin Neuroradiol. 2015;25:161–71. doi: 10.1007/s00062-014-0293-7. [DOI] [PubMed] [Google Scholar]
- 16.Moon SN, Jeon SJ, Choi SS, Song CJ, Chung GH, Yu IK, et al. Can clinical and MRI findings predict the prognosis of variant and classical type of posterior reversible encephalopathy syndrome (PRES)? Acta Radiol. 2013;54:1182–90. doi: 10.1177/0284185113491252. [DOI] [PubMed] [Google Scholar]
- 17.Prasad N, Gulati S, Gupta RK, Kumar R, Sharma K, Sharma RK. Is reversible posterior leukoencephalopathy with severe hypertension completely reversible in all patients? Pediatr Nephrol. 2003;18:1161–6. doi: 10.1007/s00467-003-1243-9. [DOI] [PubMed] [Google Scholar]


