Abstract
BACKGROUND/OBJECTIVE
Antimicrobials are frequently prescribed in long-term care facilities (LTCFs). In order to develop effective stewardship interventions, there is a need for data on current patterns of unnecessary antimicrobial prescribing among LTCF residents. The objective of this study was to examine the frequency of, reasons for, and adverse effects of unnecessary antimicrobial use in our Veterans Affairs (VA) LTCF.
DESIGN
Retrospective chart review.
SETTING
Cleveland VA Medical Center LTCF.
PARTICIPANTS
Randomly selected patients receiving antimicrobial therapy from October 1, 2008 to March 31, 2009.
MEASUREMENTS
Days of necessary and unnecessary antimicrobial therapy determined using Infectious Diseases Society of America guidelines, syndromes treated with unnecessary antimicrobials, and the frequency of development of Clostridium difficile infection (CDI), colonization or infection with antimicrobial resistant pathogens, and other adverse effects.
RESULTS
Of 1351 days of therapy prescribed in 100 regimens, 575 days (42.5%) were deemed unnecessary. Of the 575 unnecessary days of therapy, 334 (58%) were for antimicrobial regimens that were entirely unnecessary (n=42). Asymptomatic bacteriuria was the most common reason for entirely unnecessary regimens (n=21), resulting in 173 days of unnecessary therapy. Regimens that were partially unnecessary resulted in 241 (42%) days of unnecessary therapy, with longer than recommended treatment duration accounting for 226 (94%) unnecessary days of therapy. Within 30 days of completing the antimicrobial regimens, 5 patients developed CDI, 5 had colonization or infection with antimicrobial-resistant pathogens, and 10 experienced other adverse drug events.
CONCLUSIONS
In our VA LTCF, 43% of all days of antimicrobial therapy were unnecessary. Our findings suggest that antimicrobial stewardship interventions in LTCFs should focus on improving adherence to recommended treatment durations and eliminating inappropriate treatment of asymptomatic bacteriuria.
Keywords: anti-bacterial agents, long-term care, bacteriuria, Clostridium difficile, antimicrobial stewardship
INTRODUCTION
Antimicrobials are frequently prescribed in long-term care facilities (LTCFs). In a survey of Maryland nursing homes, the point-prevalence of antimicrobial treatment was 8%, and 54% of patients received at least 1 course of antimicrobial therapy during a 1-year period.1 Recently, Daneman et al.2 reported a 6% point-prevalence of antimicrobial use among elderly LTCF residents of 363 institutions in Ontario, Canada, with substantial variability in usage patterns across facilities. Unfortunately, previous studies have also shown that a significant proportion of antimicrobial use in LTCFs is inappropriate. For example, in an assessment of 42 skilled nursing facilities in New York, Zimmer et al.3 found that there was inadequate documented evidence that antimicrobials were indicated for 38% of prescriptions.
Antimicrobial use can lead to emergence of antimicrobial resistance, development of Clostridium difficile infection (CDI), and other adverse effects.4-7 In Ohio, more than half of all CDI cases in 2006 had their onset in LTCFs.4 In our Veterans Affairs (VA) LTCF, we found that one-third of patients diagnosed with CDI had received unnecessary antimicrobial therapy in the preceding six weeks (authors’ unpublished data), suggesting that antimicrobial stewardship interventions could be beneficial as a control measure for CDI in LTCFs. Some recent studies have demonstrated that educational interventions with or without use of diagnostic and treatment algorithms can be effective in improving antimicrobial prescribing in public LTCFs.8-10 In order to develop effective stewardship interventions, there is a need for additional data on current patterns of unnecessary antimicrobial prescribing among LTCF residents, particularly in VA facilities. Therefore, we performed a retrospective study to determine the frequency of, reasons for, and adverse effects of unnecessary antimicrobial use in our VA LTCF.
METHODS
Setting
The Louis Stokes Cleveland VA Medical Center is a 215-bed hospital with an affiliated 160-bed skilled nursing facility that offers post-acute rehabilitation and long-term care services and houses a dementia care unit. The facilities did not have a formal antimicrobial stewardship program at the time of this study.
Study Design
We performed retrospective study to evaluate the necessity of oral and parenteral antimicrobial regimens administered to LTCF residents during the 6-month period from October 1, 2008 to March 31, 2009. Antiviral and antifungal therapy regimens were excluded. One-hundred antimicrobial regimens were randomly selected for review from a list of all antimicrobial prescriptions during the study period. Patients were located in one of four units that serve veterans for respite care, post-acute and long-term care, dementia care, palliative care and hospice. Information regarding patient demographics, admitting ward, clinical syndrome being treated, laboratory data, radiologic tests and complications of therapy was obtained through the Computerized Patient Record System and recorded on a standardized data collection form.
Infectious diseases specialists (C.J.D and R.L.P.J) determined whether the antimicrobial regimens were necessary or unnecessary. If an antimicrobial regimen was necessary, additional assessments were made regarding whether all of the components of the regimen were necessary. Components of a regimen were classified as unnecessary if it was continued after culture results demonstrated that it was unnecessary (adjustment of therapy not made in a timely manner) or if the duration of therapy was longer than necessary. Therapy was defined as longer than necessary if the length of therapy exceeded standard recommendations for treatment duration or if empiric antimicrobials were continued despite negative evaluations for infectious syndromes and/or a noninfectious condition was demonstrated to be responsible for the clinical syndrome.
The determination of the necessity of the prescribed antimicrobials was based on standard practice guidelines for management of infectious diseases developed and/or endorsed by the Infectious Diseases Society of America.11 For example, current guidelines for asymptomatic bacteriuria recommend treatment only for pregnant women or individuals undergoing invasive urologic procedures.12 If standard practice guidelines were not available, diagnostic and treatment recommendations from a current textbook of infectious diseases were used.13
Statistical Analyses
Bivariate analyses were performed to compare necessary and unnecessary treatment regimens. The parameters entered into the database were analyzed for all patients and for those given necessary or unncessary antimicrobials using R (version 2.14.2; Vienna, Austria).14 Differences between patients given necessary or unncessary antimicrobials were determined using the Chi-square test for nominal data and the Wilcoxon signed-rank test for continuous data. Bonferroni’s correction was applied when multiple comparisons were made. The hospital’s institutional review board approved the study protocol.
RESULTS
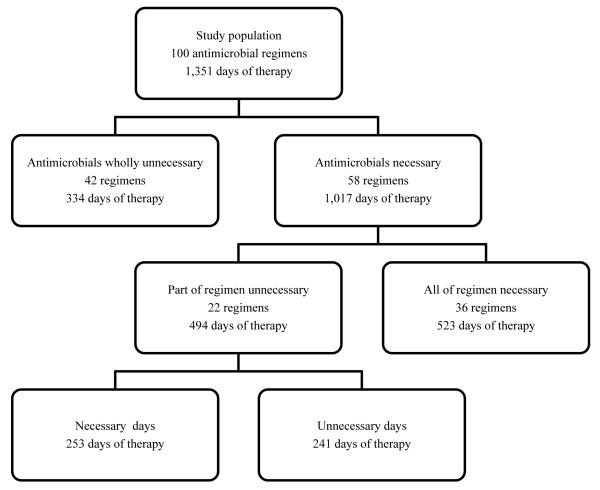
The 100 randomly-selected antimicrobial regimens were prescribed to 70 LTCF residents for a total of 1,351 days of antimicrobial therapy. Figure 1 summarizes the findings regarding the necessity of antimicrobial regimens. Overall, 575 (43%) of the 1,351 days of antimicrobial therapy were deemed unnecessary and 34 (49%) of the 70 study patients received at least one day of unnecessary antimicrobial therapy.
Figure 1.
Overview of decisions regarding necessity of antimicrobial therapy
The most commonly prescribed antimicrobials in this study doubled as the most commonly prescribed unnecessary antimicrobials and are detailed in Table 1. Two of these agents (i.e., ciprofloxacin and metronidazole) are indicated for the treatment of urinary tract infections.
Table 1.
Necessity of most commonly prescribed antimicrobial agents
| Antimicrobial agent | Regimens including the agent (n) |
Total days of therapy (n) |
Unnecessary days of therapy (n) |
Unnecessary days/total days (%) |
|---|---|---|---|---|
| Ciprofloxacin | 19 | 176 | 119 | 68 |
| Amoxicillin or amoxicillin/clavulanate |
19 | 148 | 71 | 48 |
| Piperacillin/tazobactam | 10 | 217 | 85 | 39 |
| Metronidazole | 8 | 128 | 51 | 40 |
| Vancomycin | 7 | 151 | 46 | 30 |
Table 2 provides a comparison of the characteristics of patients receiving necessary versus unnecessary antimicrobial regimens. Patients receiving unnecessary antimicrobial regimens were significantly more likely to be those with concerns for a urinary tract infection, to be older, and to have their antimicrobials started at the LTCF. Patients with fewer days of antimicrobial therapy were more likely to have received unnecessary antibiotics versus those with longer courses.
Table 2.
Comparison of unnecessary and necessary antimicrobial regimens
| Characteristics | Unnecessary regimen (n=42) |
Necessary regimen (n=58) |
|---|---|---|
| Age in years – mean (SD)* | 74 (12) | 68 (12.8) |
| Males – n (%) | 41 (98) | 58 (100) |
| Days of antimicrobial therapy per regimen – mean (SD)* |
7 (3.9) | 14 (10.3) |
| Days in VA long-term care facility prior to receiving antimicrobials – mean (SD) |
383 (1147.3) | 98 (155.4) |
| Location first prescribing antimicrobials – n (%)* | ||
| VA long-term care facility | 35 (83.3) | 21 (36.2) |
| VA acute care hospital or outside hospital | 7 (16.7) | 37 (63.8) |
| Documented infectious diseases consult service recommendation – n (%)* |
1 (2.4) | 13 (22.4) |
| Antimicrobials in the regimen – n (%) | ||
| One | 37 (88.1) | 47 (81) |
| Multiple (2+) | 5 (11.9) | 11 (19) |
| Presence of a urinary catheter device – n (%) | 21 (50) | 22 (37.9) |
| Syndrome treated with antimicrobials – n (%) | ||
| Urinary* | 24 (57.1) | 8 (13.8) |
| Pulmonary | 6 (14.3) | 13 (22.4) |
| Skin and soft tissue | 2 (4.8) | 13 (22.4) |
| Fever or sepsis syndrome | 1 (2.4) | 5 (8.6) |
| Diarrhea/Clostridium difficile infection | 1 (2.4) | 8 (13.8) |
| Pre-/post-operative | 1 (2.4) | 7 (12.1) |
| Bacteremia | 0 | 2 (3.4) |
| Intra-abdominal infection | 0 | 2 (3.4) |
| Leukocytosis | 2 (4.8) | 0 |
| Other (dehydration, infection prophylaxis) | 2 (4.8) | 0 |
| Not documented | 3 (7.1) | 0 |
Denotes statistically significant differences in patient or regimen characteristics between necessary and unnecessary regimens (p<0.05)
SD=standard deviation; VA=Veterans Affairs
Table 3 summarizes the reasons for unnecessary antimicrobial days of therapy. Urinary syndromes, including asymptomatic bacteriuria and pyuria, accounted for 57% of the unnecessary antimicrobial regimens and for 38 of the 241 (16%) days of unnecessary therapy that were prescribed as part of necessary regimens. In total, urinary syndromes accounted for 214 of the 575 (37%) unnecessary days of antimicrobial therapy.
Table 3.
Reasons for unnecessary antimicrobial regimens and days of therapy
| Reasons for unnecessary antimicrobial therapy | Number of regimens affected (Days of unnecessary therapy) |
|---|---|
| Entirely unnecessary antimicrobial regimen (n=42) | |
| Treatment of asymptomatic bacteriuria or pyuria | 22 (176) |
| Non-infectious/non-bacterial syndrome* | 12 (63) |
| Spectrum of activity not indicated (inadequate, redundant or broader than necessary coverage) |
8 (95) |
| Part of necessary antimicrobial regimen unnecessary (n=22) | |
| Duration of treatment too long | 20 (226) |
| Untimely adjustment made to antimicrobials following culture results |
2 (15) |
Non-infectious/non-bacterial syndrome operationally defined by either the identification of a noninfectious origin or failure to identify any source of infection.
Gastrointestinal complaints (n=9) were the most frequently occurring adverse drug events identified within 30 days of completing antimicrobial therapy. Other adverse events were development of CDI (n=5), colonization or infection with antimicrobial-resistant pathogens (n=5), and renal complications (n=1). Two patients who developed CDI received unnecessary antimicrobials prior to CDI diagnosis; one patient received an entirely unnecessary regimen for asymptomatic bacteriuria and the other received a longer than necessary course of therapy for aspiration pneumonia.
DISCUSSION
We found that 42% of the antimicrobial regimens reviewed during the study period were entirely unnecessary. These unnecessary regimens accounted for 25% of all antimicrobial days of therapy reviewed. Although most unnecessary regimens were prescribed in the LTCF, it is notable that 17% of unnecessary regimens were prescribed in the hospital and continued in the LTCF. The most common reasons for unnecessary regimens were administration of antimicrobials for asymptomatic bacteriuria or pyuria and treatment of other non-infectious or non-bacterial syndromes. These findings are consistent with previous data indicating that urinary tract syndromes account for 20-60% of systemic antimicrobials prescribed in LTCFs.15 Randomized trials have demonstrated that treatment of asymptomatic bacteriuria is not beneficial in LTCF residents.16-17 The unnecessary treatment of asymptomatic bacteriuria could potentially be addressed by educating prescribers and nursing staff members on diagnosis and treatment guidelines (e.g., criteria for sending urine cultures) and potential adverse effects of unnecessary antimicrobial use (e.g., promotion of antimicrobial resistance), as described by Zabarsky et al.18
Nearly half of all unnecessary days of antimicrobial therapy (241 of 575 unnecessary days of therapy) occurred when only part of a treatment regimen was unnecessary. The most common reason for part of a regimen being unnecessary was administration of antimicrobials for longer than necessary durations, either because treatment duration was longer than is recommended in current guidelines or because therapy was not discontinued when there was no evidence of infection. Notably, for seven regimens in which longer than recommended durations of therapy were prescribed, recommendations on duration of therapy from the hospital’s infectious diseases consult service were documented in the medical record but not followed. For example, the infectious diseases consult service recommended 14 days of linezolid therapy for a patient with vancomycin-resistant enterococcal peritonitis, but linezolid was continued for 33 days total with all 19 unnecessary days of therapy having been given at the LTCF. This error was identified during a treatment team meeting, but some unnecessary days of therapy could potentially have been avoided if the appropriate stop date for the drug had been entered upon the patient’s transfer to the LTCF. A recent hospital-based LTCF educational intervention study, teaching sessions and booklets with institutional-specific guidelines for treating common infectious syndromes was also shown to improve the quality and reduce the quantity of antimicrobial prescribing.19
We found that those receiving fewer days of antimicrobial therapy were more likely to have received unnecessary antimicrobials versus those with longer treatment courses. This finding may reflect involvement of the infectious diseases consult service; the upper range of days of therapy among necessary antimicrobial regimens was 47, consistent with the duration of treatment for endocarditis or osteomyelitis. Our study did not seek to identify the reasons for antimicrobial prescribing, but it is reasonable to speculate that perhaps LTCF providers believe they are demonstrating some aspect of antimicrobial stewardship by prescribing shorter courses versus longer ones. Fear of doing more harm than good by not treating a suspected infection could also be of concern to prescribers, leading them to order short courses of antimicrobial therapy despite limited time and data to thoroughly evaluate their choice.
While it may not be unusual to find that nearly half of all days of antimicrobial therapy in our LTCF were unnecessary,20 it is certainly alarming. With more than 60% of the regimens initiated in our LTCF being unnecessary, there is a clear need for educational interventions, like the ones described above, and an on-site antimicrobial stewardship program focused on improving provider recognition of and adherence to recommended treatment durations and eliminating inappropriate treatment of asymptomatic bacteriuria.
One limitation of our study is that categorization of therapy as necessary or unnecessary was based on retrospective review of medical records, and therefore it is possible that some regimens were misclassified due to inadequate documentation of the indications for treatment. This study was conducted in a single VA LTCF; additional studies are needed in other settings to determine the generalizability of these findings.
CONCLUSIONS
In conclusion, nearly half of all days of antimicrobial therapy were unnecessary in our LTCF. The most common reasons for unnecessary therapy were administration of antimicrobials for asymptomatic bacteriuria or pyuria and administration of antimicrobials for longer than recommended durations. These results suggest that antimicrobial stewardship interventions in LTCFs should focus on improving provider recognition of and adherence to recommended treatment durations and eliminating inappropriate treatment of asymptomatic bacteriuria.
ACKNOWLEDGEMENTS
The authors wish to acknowledge Jon Laich for his assistance with acquisition of a listing of potential subjects. At the time of this study, Dr. Peron was a PGY-2 geriatric pharmacy resident at the Louis Stokes Cleveland VA Medical Center.
Sponsor’s role: This study was unfunded.
Footnotes
Poster presentation: 50th Interscience Conference on Antimicrobial Agents and Chemotherapy, Boston, MA, September 2010
Conflicts of interest: None of the authors have relevant financial interest in this article.
Author contributions: Dr. Peron was responsible for the study design; acquisition, analysis, and interpretation of data; and drafting and final preparation of the manuscript. Dr. Hirsch, Ms. Jury, and Dr. Jump were involved in the study design, analysis and interpretation of data, and final preparation of the manuscript. Dr. Donskey was responsible for the study conception and design; acquisition, analysis, and interpretation of data; and editing and final preparation of the manuscript.
REFERENCES
- 1.Warren JW, Palumbo FB, Fitterman L, et al. Incidence and characteristics of antibiotic use in aged nursing home patients. J Am Geriatr Soc. 1991;39:963–972. doi: 10.1111/j.1532-5415.1991.tb04042.x. [DOI] [PubMed] [Google Scholar]
- 2.Daneman N, Gruneir A, Newman A, et al. Antibiotic use in long-term care facilities. J Antimicrob Chemother. 2011;66:2856–2863. doi: 10.1093/jac/dkr395. [DOI] [PubMed] [Google Scholar]
- 3.Zimmer JG, Bentley DW, Valenti WM, et al. Systemic antibiotic use in nursing homes. A quality assessment. J Am Geriatr Soc. 1986;34:703–710. doi: 10.1111/j.1532-5415.1986.tb04301.x. [DOI] [PubMed] [Google Scholar]
- 4.Campbell RJ, Gijahn L, Machesky K, et al. Clostridium difficile infection in Ohio hospitals and nursing homes during 2006. Infect Control Hosp Epidemiol. 2009;30:526–533. doi: 10.1086/597507. [DOI] [PubMed] [Google Scholar]
- 5.Dellit TH, Owens RC, McGowan JE, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clin Infect Dis. 2007;44:159–157. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 6.Paterson DL. “Collateral damage” from cephalosporin or quinolone antibiotic therapy. Clin Infect Dis. 2004;38(Suppl 4):S341–S345. doi: 10.1086/382690. [DOI] [PubMed] [Google Scholar]
- 7.Rice LB. The Maxwell Finland Lecture: for the duration-rational antibiotic administration in an era of antimicrobial resistance and Clostridium difficile. Clin Infect Dis. 2008;15:491–496. doi: 10.1086/526535. [DOI] [PubMed] [Google Scholar]
- 8.Monette J, Miller MA, Monette M, et al. Effect of an educational intervention on optimizing antibiotic prescribing in long-term care facilities. J Am Geriatr Soc. 2007;55:1231–1235. doi: 10.1111/j.1532-5415.2007.01250.x. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz DN, Abiad H, DeMarais PL, et al. An educational intervention to improve antimicrobial use in a hospital-based long-term care facility. J Am Ger Soc. 2007;55:1236–1242. doi: 10.1111/j.1532-5415.2007.01251.x. [DOI] [PubMed] [Google Scholar]
- 10.Loeb M, Brazil K, Lohfeld L, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomized controlled trial. BMJ. 2005;331:669–672. doi: 10.1136/bmj.38602.586343.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Infectious Diseases Society of America [Accessed April 24, 2012];Standards, practice guidelines, and statements developed and/or endorsed by IDSA. Available at: http://www.idsociety.org/Index.aspx.
- 12.Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643–654. doi: 10.1086/427507. [DOI] [PubMed] [Google Scholar]
- 13.Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th Ed Churchill Livingstone; New York: 2010. [Google Scholar]
- 14.R Development Core Team . R: a language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2012. Available at http://www.R-project.org. [Google Scholar]
- 15.Nicolle LE. Urinary tract infections in long-term-care facilities. Infect Control Hosp Epidemiol. 2001;22:167–175. doi: 10.1086/501886. [DOI] [PubMed] [Google Scholar]
- 16.Nicolle LE, Bjornson J, Harding GK, et al. Bacteriuria in elderly institutionalized men. N Engl J Med. 1983;309:1420–1425. doi: 10.1056/NEJM198312083092304. [DOI] [PubMed] [Google Scholar]
- 17.Nicolle LE, Mayhew JW, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987;83:27–33. doi: 10.1016/0002-9343(87)90493-1. [DOI] [PubMed] [Google Scholar]
- 18.Zabarsky TF, Sethi AK, Donskey CJ. Sustained reduction in inappropriate treatment of asymptomatic bacteriuria in a long-term care facility through an educational intervention. Am J Infect Control. 2008;36:476–480. doi: 10.1016/j.ajic.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Schwartz DN, Abiad H, DeMarais PL, et al. An educational intervention to improve antimicrobial use in a hospital-based long-term care facility. J Am Geriatr Soc. 2007;55:1236–1242. doi: 10.1111/j.1532-5415.2007.01251.x. [DOI] [PubMed] [Google Scholar]
- 20.Nicolle LE, Bentley DW, Garibaldi R, Neuhaus EG, Smith PW. Antimicrobial use in long-term-care facilities. Infect Control Hosp Epidemiol. 2000;21:537–545. doi: 10.1086/501798. [DOI] [PubMed] [Google Scholar]