Introduction
Our goals in medicine are (i) to improve the quality of patients' lives, (ii) help them to live longer, and (iii) to do so at a reasonable cost. These are our true endpoints: health status, survival, and cost. It is thus entirely consistent with this point of view that these are the fundamental concepts that can be united in a formal cost–utility analysis.1 These endpoints remain the best measures of efficacy in clinical trials comparing a new therapy to placebo or to an active control. All other measures may then be seen as surrogate endpoints or surrogates. Thus, even serious events such as myocardial infarction and stroke may be considered surrogates, as their effect is to adversely affect the critical endpoints of health status, survival, and cost. However, in common usage a surrogate is a relatively easy to measure endpoint, available over a relatively short timeframe that is used in place of the true endpoints.
Generally, surrogates are not events, but rather measurements (physiological, laboratory, or test results, e.g. biomarkers) that predict events. Thus, surrogates are most commonly measures that we can record, often with much shorter timescales than is necessary for events.2 Surrogates are usually continuous variables, often but not necessarily with reasonable approximations of a normal distribution. Continuous variables, especially if approximating a normal distribution, will allow for much smaller sample sizes than dichotomous variables as well as shorter periods of follow-up and lower costs. Thus, compared with clinical outcome trials, studies with surrogate endpoints can be conducted rapidly and with much less resource use and expense than endpoint studies. Surrogates can be used in observational studies as well as in randomized trials. For instance, low-density lipoprotein cholesterol could be used as a surrogate for cardiovascular events in a non-interventional observational study. However, the most common and perhaps most critical issue is the use of surrogate endpoints in randomized trials comparing different therapies.
Potential surrogates
Any surrogate should be consistently measurable and sensitive to the intervention.3 In Table 1, we reproduce and modify a list of potential surrogates including physical exam as well as haemodynamic, blood, imaging, and other testing.2 This list is not meant to be exhaustive, but rather to reflect potential surrogates in different areas of cardiovascular medicine: Hypertension, lipid disorders, diabetes, coronary artery disease, acute coronary syndromes, heart failure, and ECG abnormalities. We give an approximate, perhaps somewhat arbitrary rank to each variable's validity as a true surrogate. A surrogate is most useful when it (i) consistently predicts events in the future and (ii) if the response of the surrogate to an intervention predicts the response to the intervention in an endpoints trial.
Table 1.
Potential surrogate endpoints in clinical trials
| Disease area | Potential surrogate endpoint | Validity as a true surrogate |
|---|---|---|
| Hypertension/vascular physiology | Blood pressure8 | ++++ |
| Carotid intima-media thickness8 | ++ | |
| Microalbuminuria8,15 | ++/? | |
| Flow-mediated dilatation58,59 | ++ | |
| Left ventricular hypertrophy8 | ++ | |
| Lipid disorders/atherosclerosis | Low-density lipoprotein cholesterol9,10,15,57 | ++++ |
| High-density lipoprotein cholesterol11,12 | − | |
| Carotid magnetic resonance imaging60 | ++ | |
| Intravascular ultrasound20 | ++ | |
| Coronary computed tomography61 | ? | |
| Optical coherence tomography62 | ? | |
| Diabetes | Serum glucose | ++ |
| Haemoglobin A1c | ++ | |
| Microalbuminuria | ++ | |
| Obstructive coronary artery disease | Quantitative coronary angiography63 | ++ |
| Intravascular ultrasound20 | ++ | |
| Coronary computed tomography61 | ? | |
| Optical coherence tomography62 | ? | |
| Restenosis after PCI28–30 | ++ | |
| Angiographic variables to predict restenosis31,32 | + | |
| Acute coronary syndromes | Troponins64 | ++ |
| Brain natriuretic peptide64 | ++ | |
| Infarct size65 | ? | |
| Return of TIMI flow66,67 | ? | |
| Resolution of ST elevation67 | ? | |
| Heart failure | Exercise capacity68,69 | − |
| Haemodynamics (e.g. cardiac output)69 | − | |
| Ejection fraction33 | ++ | |
| Remodelling (e.g. LV volume)70 | ++ | |
| Brain natriuretic peptide69,71 | − | |
| Electrophysiology | Premature ventricular beats36 | − |
| Late potentials72 | − | |
| Non-sustained ventricular tachycardia36 TTaTachycardia | − |
The symbols ‘−‘ and ‘+’ to ‘+ ++ +’ indicate the reliability of the potential surrogate; the symbol ‘?’ indicates currently unknown. A valid surrogate or true surrogate will be on the causal path to and have a strong, consistent statistical relationship with the clinical endpoint.
Hypertension
The variable perhaps most often thought of as a consistently useful surrogate in interventional trials is the simple measurement of blood pressure. Lowering blood pressure using different therapies has consistently resulted in reduced events, in particular stroke.4 However, even this relationship is not straight forward. For instance, while blood pressure is related to event rates to pressures <120 mmHg systolic, there is insufficient evidence that lowering blood pressure with pharmaceutical in patients with hypertension to <140 mmHg systolic will reduce event rates.5 Furthermore, in some trials similar blood pressure reduction led to different effects on hard endpoints such as mortality and stroke.6,7 Other measures of vascular physiology are less reliable. Despite its limitations, blood pressure remains a useful surrogate as recognized in the current guidelines from the Joint National Committee as well as the European Society of Cardiology; blood pressure level remains a therapeutic goal.4,8 However, blood pressure may not be useful in all clinical situations. For instance, blood pressure will fall in patients with a history of hypertension who develop heart failure. In this common clinical scenario, blood pressure will no longer be a useful surrogate.
Lipids
Low-density lipoprotein (LDL) cholesterol is the most useful surrogate lipid measure, given the many trials with statins that demonstrated both reduced LDL cholesterol as well as cardiovascular events. While, the efficacy of other agents to reduce event rates by reducing LDL cholesterol is not as well established, recent data have shown both LDL and event rate reduction with ezetimibe as well as early data with PCSK9 antibodies.9–12 Nonetheless, it is possible that the mechanism by which statins reduce event rates may not be entirely by their effects on LDL cholesterol alone; statins also exert pleiotrophic effects on small G proteins among other effects.13 Of importance, there remains some uncertainty about target levels for LDL as the endpoint trials did not include target levels for LDL; leading to target levels no longer being recognized in the 2013 Guidelines from the American College of Cardiology and the American Heart Association.14 However, the European Society of Cardiology guidelines have maintained such an approach.15,16
High-density lipoprotein (HDL) cholesterol plasma levels have been shown to predict events in epidemiological studies, but the event outcome data on pharmaceuticals to raise HDL have been unconvincing. Indeed, it appears that the biological activity of HDL cholesterol changes in patients with diabetes, coronary artery disease, and acute coronary syndromes, most likely due to a change on its proteome composition.17–19 Surrogates related to atherosclerosis, including imaging such as calcium scoring and carotid ultrasound are also at best uncertain.20,21
Diabetes
Diabetes is clearly a risk factor for cardiovascular events.22,23 However, there is little evidence that tight control of diabetes will reduce cardiovascular events.24 Indeed, recent trials showed that lowering haemoglobin 1Ac with blood sugar lowering drugs such as DDP-4 inhibitors or strict lifestyle measures did not reduce cardiovascular events.25–27
Coronary disease
Measures of the extent and severity of coronary artery disease noted in Table 1 are also mixed as surrogates. While the extent of coronary artery disease noted on angiograms has been shown to positively correlate with cardiovascular events, the angiogram is more useful as a guide to therapy than as a surrogate outcome. Other measures of coronary disease are also uncertain surrogates. Measures of acute coronary syndromes, such as troponins are useful diagnostically to guide therapy, but have not proven useful as surrogate endpoint for events in randomized trials. Restenosis after PCI is a surrogate for quality of life and myocardial infarction.28–30 Various angiographic measures have also been used as surrogates for restenosis or target lesion revascularization.31,32
Heart failure
There are inadequate potential surrogates in heart failure.33 In particular, changes in exercise capacity, haemodynamic variables, and ejection fraction have failed to predict clinical outcome. Thus, although the ejection fraction predicts outcome, changes thereof under treatment with inotropes may even be associated with an increase in mortality.34 Somewhat paradoxically, β-blockers, in spite of their negative inotropic effects, result in a slightly improved ejection fraction over time, and improved survival.35 Thus, we cannot use ejection fraction or any other measure of improved left ventricular performance as a reliable surrogate in heart failure trials.
Electrocardiogram
Findings on the ECG may also predict events, but have not been reliable as guides to effectiveness of therapy. Perhaps the best known failure is this endpoint is that suppression of premature ventricular contractions (PVCs) post-MI by class I anti-arrhythmic agents will not reduce events, but rather enhanced mortality.36
Why surrogates fail
A potential surrogate is often considered as an intermediate endpoint in a clinical trial because it is found to predict outcome in observational studies. Thus, blood pressure and LDL cholesterol are well known (and in fact accepted by regulatory agencies such as the Federal Drug Administration or the European Medical Agency) to predict outcome, and have been used as surrogate endpoints in clinical trials. Indeed, clinical outcome studies did show that interventions which favourably affected these surrogates did in general reduce the incidence of cardiovascular events.
However, there are also many examples where a therapy was shown to favourably affect a surrogate, but was not found to reduce cardiovascular events. Thus, serum HDL cholesterol level has an inverse relationship with cardiovascular events. Furthermore, both niacin and cholesterol ester transfer protein blockers have been shown to increase serum HDL cholesterol.11,12,37 Nonetheless, recent trials with these agents have not shown efficacy in reducing cardiovascular events; indeed, one of them even increased mortality in spite of marked increases in HDL cholesterol.12
As noted above, while PVCs noted on the ECG post myocardial infarction predict events, a trial of anti-arrhythmic agents which reduce PVCs failed to show efficacy in preventing events.36
As a third example, hormone replacement therapy in post-menopausal women will favourably affect the serum lipid profile. However, randomized trials of hormone replacement therapy have not been shown to reduce cardiovascular events.38 It is also possible that the problem with a therapy that works on a surrogate but failed in an outcomes trial was due to inadequate dosing, too short a time period, an inappropriate patient population or too small a population.
Causality
Why do some potential surrogates seem to work well, while others fail? We can gain insight by considering the nature of causality.39,40 A true surrogate should be in the causal path of a true endpoint. Thus, LDL cholesterol is a good candidate true surrogate, as high LDL causes more events by directly augmenting atherosclerotic plaque formation, a prime culprit for myocardial infarction and cardiovascular death. On the other hand, lowering LDL causes the event rate to be lower as it reduces the lipid content of plaques and hence the vulnerability of plaques. To establish causation requires a deep understanding of the pathophysiology of the disease process and hence is a stronger criterion than just noting an association. If there is association but not causation, then the relationship between a surrogate and outcome events may be confounded. A confounder is a variable that predicts outcomes and has higher prevalence in the group with the potential surrogate of interest.39 Thus, PVCs may be confounded by left ventricular function, whereby patients with left ventricular dysfunction have more PVCs, and it may be the left ventricular dysfunction which causes increased mortality. If this is the case, a drug which decreases PVCs may have no effect on left ventricular function and thus may not exert any effect on subsequent mortality.36
A true surrogate will always be affected before the clinical endpoint as it often precedes late disease states that lead to myocardial infarction, stroke, or death. However, it is wrong to think that a temporal relationship is all that is necessary to establish causality. This has been recognized since ancient times as noted by the famous humorous statement – ‘post hoc ergo propter hoc’, which is Latin for ‘after this, therefore because of this’. Temporality is just one component of what is necessary to consider causal relationship.
This was considered by pioneering British epidemiologist and statistician Austin Bradford Hill. In the 1950s Doll and Hill41,42 published a pair of sentinel papers showing the association between cigarette smoking and lung cancer. These papers, plus data from Framingham on the impact of cigarette smoking on cardiovascular disease risk,43 helped move the US Federal Government in 1964 to issue the first Surgeon General's Report on Smoking and Health.44,45 Nonetheless, before the 1960s there was controversy over whether cigarette smoking was causally related to lung cancer as opposed to just being an association. Hill considered the steps necessary to establish a causal relationship between any risk factor, i.e. surrogate, and future events.46 The Bradford Hill criteria are: (i) temporal relationship, the cause must always come before the effect, (ii) strength of association, (iii) dose–response relationship, (iv) consistency of the relationship, (v) biological plausibility, (vi) consideration of alternatives, (vii) experimental verification, (viii) specificity, that is a specific cause for a specific effect, and (ix) coherence, that is compatible with existing knowledge.39,46 Specificity is often omitted as it is generally not fulfilled for diseases which may have multiple causes. Establishing causality requires consideration of these criteria, and then general acceptance by the scientific community and society at large. Now a surrogate need not be the root cause of the endpoint, but it should be on the causal path. The Bradford Hill criteria can provide useful guidance in this respect. For instance, if we consider whether LDL cholesterol, we may note that it fulfils these criteria, perhaps with the exception of specificity.
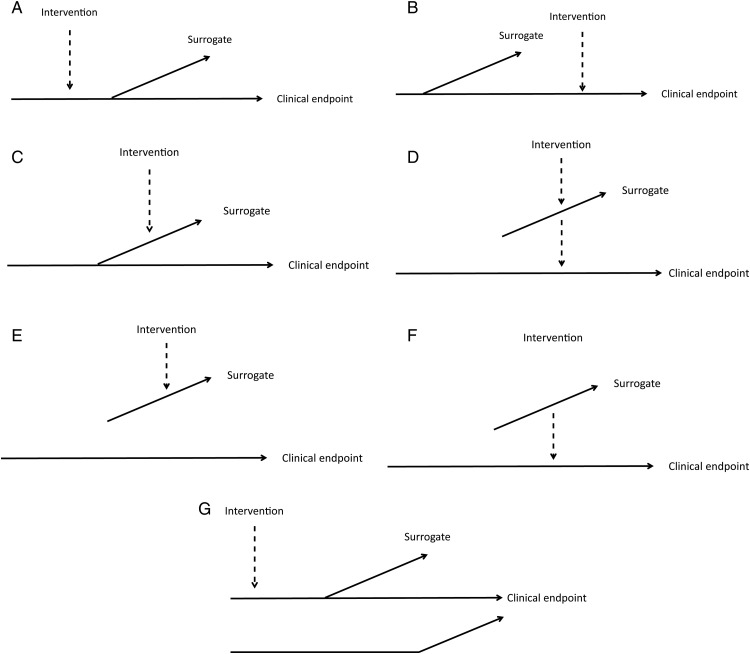
In Figure 1, we offer a conceptual model of the various ways in which the relationship between a potential surrogate and a clinical endpoint on a causal path can occur. In Figure 1A, we have a true surrogate which is in the causal path, with the intervention occurring earlier in the causal path, and thus eliciting a response in both the surrogate and endpoint. This is the only type of relationship in which the surrogate will be reliable. This is perhaps most clearly demonstrated in therapy for hypertension, where pharmaceutical therapy reduces blood pressure and reduces the incidence of strokes. The Bradford Hill criteria would also suggest that a blood pressure response to treatment is in the causal path to cardiovascular events. In Figure 1B, the potential surrogate is in the causal path, but the intervention is downstream of the surrogate. In this case, the intervention affects the outcome but not the surrogate. For instance, coronary atherosclerosis is in causal path leading to cardiovascular death. However, an intervention such as aspirin may occur downstream, preventing the outcome but not affecting the surrogate. In Figure 1C, the potential surrogate is in the causal path, but the intervention only affects the surrogate. This could explain why ventricular tachycardia is in the causal path to sudden death, but anti-arrhythmic drugs may only affect the surrogate and not prevent the endpoint. In Figure 1D, the intervention elicits a response in both the surrogate and the endpoint, but the surrogate is not in the causal path. This type of situation may be unstable, and not consistently reproducible. In Figure 1E and F, the potential surrogate is not in the causal. In Figure 1E, the intervention only affects the surrogate and not the endpoint, and in Figure 1F, the intervention only affects the endpoint and not the surrogate. In these latter two circumstances, the potential surrogate is not really a surrogate at all. Figure 1G shows a more complex scenario: a potential surrogate is in the causal pathway, but there are other pathways to the endpoint that are independent of the surrogate. For instance, while statins will lower LDL cholesterol and decrease cardiovascular mortality secondary to atherosclerotic disease, cardiovascular mortality may occur independently of therapy with statins and independently of LDL cholesterol. Similarly, blood pressure elevation is on the pathway to myocardial infarction, but there are other pathways with myocardial infarction occurring independently of hypertension. In this setting, blood pressure control may decrease the incidence of myocardial infarction without eliminating it. Empiric data from clinical trials can show whether an intervention affects both the surrogate and the clinical endpoint. However, without clear understanding of the biologic mechanisms involved it cannot be certain if the surrogate is in the causal path. This framework around causality is conceptually helpful, but not necessarily practical as it is often not clear for any potential surrogate whether it is in the causal path. Thus, a more practical empirical approach is needed.
Figure 1.
Conceptual model of the various possible relationships between a potential surrogate and a clinical endpoint. Only (A) is a true surrogate. See text for explanation of the panels. Reprinted with permission from Elsevier (The Lancet 2010;376:1673).
The relationship of surrogates to clinical endpoints
The statistical relationship of surrogates to clinical endpoints is multi-faceted and needs careful explanation. Surrogates, such as biomarkers, are usually continuous variables while events are generally binary or categorical. The relationship of a surrogate to the clinical endpoint is more complex than that of a risk factor to an endpoint in that a therapy's value is based on its effect on the clinical endpoint. If a surrogate was considered only as a risk factor, then standard methods of discrimination (e.g. the c statistic or R2), calibration and validation could be used. However, the key issue is whether therapeutic efficacy as assessed by the surrogate captures therapeutic efficacy on the clinical endpoint. The mathematical expression of this relationship has several aspects. Prentice proposed that a surrogate must capture any statistical relationship between the treatment and the true endpoint.47 This would be consistent with Figure 1A, where the surrogate and the clinical endpoint are clearly on the causal path after the intervention. However, it is recognized that a surrogate may not explain all of the relationship between the intervention and the endpoint.48 This more complex relationship would be consistent with Figure 1G.3 How can this relationship be explained? An early proposal was the proportion of treatment effect (PTE) of a clinical endpoint explained by a surrogate endpoint. Proportion of treatment effect may be defined as (β-βa)/β where β and βa are, respectively, the differences between treatments in a trial without and with adjustment for the potential surrogate endpoint.49 However, PTE is not a valid proportion as it can have values outside of the range 0–1 (e.g. where βa is negative).49–51 Buyse and Molenberghs52 built on these ideas to develop a pair of metrics, RE (relative effect), which is the effect of treatment on the true endpoint relative to that of treatment on the surrogate, and γa, which is the association between the surrogate and true endpoint after adjustment for treatment. A surrogate is perfect at the individual level if there is perfect association between the surrogate and the true endpoint after adjustment for treatment. A surrogate is said to be perfect at the population level if RE = 1. Buyse and Molenberghs52 initially considered the case where the outcomes of both surrogate and true endpoint were jointly normal or jointly binary in a single trial. Buyse et al.53 extended this to meta-analyses and then Molenberghs et al.54 extended this to mixed discrete and continuous outcomes. The metrics which follow from these analyses are , which is the quality of a surrogate at the trial level, and , which is the individual patient-level association between the surrogate and true endpoint after adjustment for trial and treatment effects. These R2 values range from 0 (a useless surrogate) to 1 (a perfect surrogate). Furthermore, these values are independent of the strength of the effect of treatment on either endpoint. A practical issue is that it is necessary to have large datasets from randomized trials to achieve good precision for these values, which is critical to permit reliable prediction of the treatment effect on the true endpoint given the treatment effect on the surrogate.32 Finally, estimates of these values should be validated across a number of trials to ensure consistency of the relationship.32,50,54 Such mathematical expressions of the relationship between a surrogate and true endpoint have been rarely developed in practice.32 Further insights concerning the statistical relationship between surrogate and clinical endpoint are offered by Weir and Walley55 for a mathematical review and by Hughes49 for a narrative review.
How can surrogates be used?
Given the complex relationship between interventions, surrogates, and endpoints, how can surrogates best be used? It is unusual for a surrogate to be so reliable that it can replace clinical endpoints for regulatory approval and medical decision-making purposes. Studies with surrogate endpoints will generally be much less expensive and much more rapid to conduct than studies with clinical endpoints. However, it is very difficult to be confident about the relationship between the surrogate and the clinical endpoint. Studies with surrogates will also generally have a smaller number of patients and a shorter time span. This limits such studies for evaluation of safety, where safety endpoints may have no pathophysiologic relationship with the surrogate. Thus clinical endpoint trials will remain essential, although even endpoint trials may not have adequate power for safety. Given problems that have been noted in the past with regulatory bodies approving therapies based on surrogates, it is likely that the demand for endpoint studies for regulatory approval will be the norm, and use of surrogates for licensing new therapies will be the exception. Trials with surrogate endpoints that do not show efficacy may obviate the need for endpoint trials, saving time, expense, and avoiding unnecessary patient risk. Surrogates will remain of interest in developing new therapies and providing pathophysiologic insight and guiding the development of clinical endpoint trials.
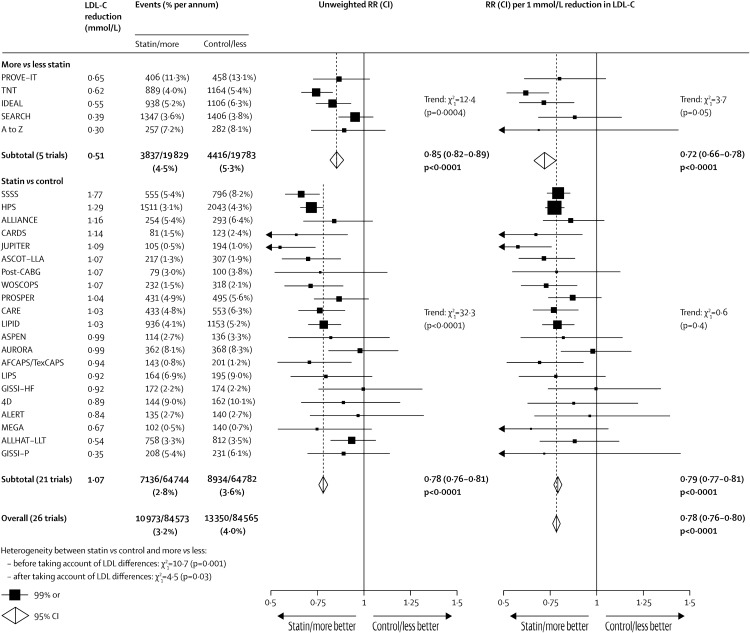
For surrogates to be useful, even if only as a phase II trial rather than a pivotal trial for registration purposes, there are several criteria to consider (Table 2).56 Thus, the potential surrogate should be considered in specific disease states, for specific therapies and for specific clinical outcomes. Thus, LDL cholesterol can be used as a surrogate for statins in patients with hyperlipidaemia and the endpoint is cardiovascular death. Next, there should be epidemiologic evidence of association between the surrogate and events. While blood pressure is an excellent example of this, HDL cholesterol, perhaps unfortunately, is as well. The surrogate should also respond to therapy consistently. Thus, LDL cholesterol is consistently reduced by statins. Next there should be a strong statistical relationship in the reduction of clinical events explained by the surrogate. Although, realistically, surrogates will also generally be developed without the mathematical rigor reviewed above. Finally, the reduction of events across trials is seen to be consistent.32 Thus, statins consistently reduce LDL cholesterol, and consistently reduce events (Figure 2, with permission).57
Table 2.
Criteria for validating a surrogate
|
Figure 2.
The relationship between low-density lipoprotein lowering and cardiovascular events in 26 clinical trials of statins.
Conclusions
The use of surrogates is complex, and there is no single criterion or standard that can readily be applied. An understanding of causality and consideration of the relevant practical criteria is important, but the adoption of a surrogate must always be considered on a case by case basis. The place of surrogates in phase II trials may be reasonable as a guide to pivotal phase three trials. However, the uncertainty of surrogates must limit their use in phase III trials, where the unreliability of surrogates alone for registration is recognized, so as to avoid potential risk to public health.
Funding
Work supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941 (PI: Binder-Macleod).
References
- 1.Weintraub WS, Cohen DJ. The limits of cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes 2009;2:55–58. [DOI] [PubMed] [Google Scholar]
- 2.Luscher TF. The bumpy road to evidence: why many research findings are lost in translation. Eur Heart J 2013;34:3329–3335. [DOI] [PubMed] [Google Scholar]
- 3.Fleming TR, Powers JH. Biomarkers and surrogate endpoints in clinical trials. Stat Med 2012;31:2973–2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 5.Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362:1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weber MA, Bakris GL, Jamerson K, Weir M, Kjeldsen SE, Devereux RB, Velazquez EJ, Dahlof B, Kelly RY, Hua TA, Hester A, Pitt B. Cardiovascular events during differing hypertension therapies in patients with diabetes. J Am Coll Cardiol 2010;56:77–85. [DOI] [PubMed] [Google Scholar]
- 7.Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005;366:895–906. [DOI] [PubMed] [Google Scholar]
- 8.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 9.Investigators CCobotII. IMPROVE-IT Trial: a comparison of ezetimive/simvastatin versus simvastatin monotherapy on cardiovascular outcomes after acute coronary syndromes. Circulation 2014;130:2105–2126. [Google Scholar]
- 10.Sabatine MS, Giugliano RP, Wiviott SD, Raal FJ, Blom DJ, Robinson J, Ballantyne CM, Somaratne R, Legg J, Wasserman SM, Scott R, Koren MJ, Stein EA; Open-Label Study of Long-Term Evaluation against LDLCI. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med 2015;372:1500–1509. [DOI] [PubMed] [Google Scholar]
- 11.Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, McBride R, Teo K, Weintraub W. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med 2012;365:2255–2267. [DOI] [PubMed] [Google Scholar]
- 12.Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 2007;357:2109–2122. [DOI] [PubMed] [Google Scholar]
- 13.Fichtlscherer S, Schmidt-Lucke C, Bojunga S, Rossig L, Heeschen C, Dimmeler S, Zeiher AM. Differential effects of short-term lipid lowering with ezetimibe and statins on endothelial function in patients with CAD: clinical evidence for ‘pleiotropic’ functions of statin therapy. Eur Heart J 2006;27:1182–1190. [DOI] [PubMed] [Google Scholar]
- 14.Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, McBride P, Eckel RH, Schwartz JS, Goldberg AC, Shero ST, Gordon D, Smith SC, Jr, Levy D, Watson K, Wilson PW. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2889–2934. [DOI] [PubMed] [Google Scholar]
- 15.Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P, Erdine S, Halcox J, Hobbs R, Kjekshus J, Filardi PP, Riccardi G, Storey RF, Wood D. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2011;32:1769–1818. [DOI] [PubMed] [Google Scholar]
- 16.Ray KK, Kastelein JJ, Boekholdt SM, Nicholls SJ, Khaw KT, Ballantyne CM, Catapano AL, Reiner Z, Luscher TF. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J 2014;35:960–968. [DOI] [PubMed] [Google Scholar]
- 17.Besler C, Heinrich K, Rohrer L, Doerries C, Riwanto M, Shih DM, Chroni A, Yonekawa K, Stein S, Schaefer N, Mueller M, Akhmedov A, Daniil G, Manes C, Templin C, Wyss C, Maier W, Tanner FC, Matter CM, Corti R, Furlong C, Lusis AJ, von Eckardstein A, Fogelman AM, Luscher TF, Landmesser U. Mechanisms underlying adverse effects of HDL on eNOS-activating pathways in patients with coronary artery disease. J Clin Invest 2011;121:2693–2708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luscher TF, Landmesser U, von Eckardstein A, Fogelman AM. High-density lipoprotein: vascular protective effects, dysfunction, and potential as therapeutic target. Circ Res 2014;114:171–182. [DOI] [PubMed] [Google Scholar]
- 19.Riwanto M, Rohrer L, Roschitzki B, Besler C, Mocharla P, Mueller M, Perisa D, Heinrich K, Altwegg L, von Eckardstein A, Luscher TF, Landmesser U. Altered activation of endothelial anti- and proapoptotic pathways by high-density lipoprotein from patients with coronary artery disease: role of high-density lipoprotein-proteome remodeling. Circulation 2013;127:891–904. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Garcia HM, Costa MA, Serruys PW. Imaging of coronary atherosclerosis: intravascular ultrasound. Eur Heart J 2010;31:2456–2469. [DOI] [PubMed] [Google Scholar]
- 21.Erbel R, Lehmann N, Churzidse S, Rauwolf M, Mahabadi AA, Mohlenkamp S, Moebus S, Bauer M, Kalsch H, Budde T, Montag M, Schmermund A, Stang A, Fuhrer-Sakel D, Weimar C, Roggenbuck U, Dragano N, Jockel KH; on behalf of the Heinz Nixdorf Recall Study I. Progression of coronary artery calcification seems to be inevitable, but predictable – results of the Heinz Nixdorf Recall (HNR) studydagger. Eur Heart J 2014;35:2960–2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J 2013;34:2436–2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beckman JA, Paneni F, Cosentino F, Creager MA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part II. Eur Heart J 2013;34:2444–2452. [DOI] [PubMed] [Google Scholar]
- 24.Gerstein HC, Miller ME, Byington RP, Goff DC, Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH, Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med 2013;369:1317–1326. [DOI] [PubMed] [Google Scholar]
- 26.Wing RR, Bolin P, Brancati FL, Bray GA, Clark JM, Coday M, Crow RS, Curtis JM, Egan CM, Espeland MA, Evans M, Foreyt JP, Ghazarian S, Gregg EW, Harrison B, Hazuda HP, Hill JO, Horton ES, Hubbard VS, Jakicic JM, Jeffery RW, Johnson KC, Kahn SE, Kitabchi AE, Knowler WC, Lewis CE, Maschak-Carey BJ, Montez MG, Murillo A, Nathan DM, Patricio J, Peters A, Pi-Sunyer X, Pownall H, Reboussin D, Regensteiner JG, Rickman AD, Ryan DH, Safford M, Wadden TA, Wagenknecht LE, West DS, Williamson DF, Yanovski SZ. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Cushman WC, Zannad F. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med 2013;369:1327–1335. [DOI] [PubMed] [Google Scholar]
- 28.Weintraub WS, Ghazzal ZM, Douglas JS, Jr, Liberman HA, Morris DC, Cohen CL, King SB., III Long-term clinical follow-up in patients with angiographic restudy after successful angioplasty. Circulation 1993;87:831–840. [DOI] [PubMed] [Google Scholar]
- 29.Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, Detre K, Veltri L, Ricci D, Nobuyoshi M, Cleman M, Heuser R, Almond D, Teirstein PS, Fish RD, Colombo A, Brinker J, Moses J, Shaknovich A, Hirshfeld J, Bailey S, Ellis S, Rake R, Goldberg R, for the Stent Restenosis Study Investigators A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med 1994;331:496–501. [DOI] [PubMed] [Google Scholar]
- 30.Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, Colombo A, Schuler G, Barragan P, Guagliumi G, Molnar F, Falotico R. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med 2002;346:1773–1780. [DOI] [PubMed] [Google Scholar]
- 31.Mauri L, Orav EJ, Candia SC, Cutlip DE, Kuntz RE. Robustness of late lumen loss in discriminating drug-eluting stents across variable observational and randomized trials. Circulation 2005;112:2833–2839. [DOI] [PubMed] [Google Scholar]
- 32.Pocock SJ, Lansky AJ, Mehran R, Popma JJ, Fahy MP, Na Y, Dangas G, Moses JW, Pucelikova T, Kandzari DE, Ellis SG, Leon MB, Stone GW. Angiographic surrogate end points in drug-eluting stent trials: a systematic evaluation based on individual patient data from 11 randomized, controlled trials. J Am Coll Cardiol 2008;51:23–32. [DOI] [PubMed] [Google Scholar]
- 33.Anand IS, Florea VG, Fisher L. Surrogate end points in heart failure. J Am Coll Cardiol 2002;39:1414–1421. [DOI] [PubMed] [Google Scholar]
- 34.Felker GM, O'Connor CM. Inotropic therapy for heart failure: an evidence-based approach. Am Heart J 2001;142:393–401. [DOI] [PubMed] [Google Scholar]
- 35.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147–e239. [DOI] [PubMed] [Google Scholar]
- 36.Echt DS, Liebson PR, Mitchell LB, Peters RW, Obias-Manno D, Barker AH, Arensberg D, Baker A, Friedman L, Greene HL, Huther ML, Richardson DW; the Cast Investigators Mortality and morbidity in patients receiving encainide, flecainide, or placebo. The Cardiac Arrhythmia Suppression Trial. N Engl J Med 1991;324:781–788. [DOI] [PubMed] [Google Scholar]
- 37.Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, Chaitman BR, Holme IM, Kallend D, Leiter LA, Leitersdorf E, McMurray JJ, Mundl H, Nicholls SJ, Shah PK, Tardif JC, Wright RS. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med 2012;367:2089–2099. [DOI] [PubMed] [Google Scholar]
- 38.Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA 2002;288:321–333. [DOI] [PubMed] [Google Scholar]
- 39.Kleinbaum DG, Kupper LL, Morgenstern H. Epidemiologic Research. New York: Van Nostrand Reinhold Company; 1982. [Google Scholar]
- 40.Luscher TF. In search of the right word: a statement of the HEART Group on scientific language. Eur Heart J 2013;34:7–9. [DOI] [PubMed] [Google Scholar]
- 41.Doll R, Hill AB. Smoking and carcinoma of the lung; preliminary report. Br Med J 1950;2:739–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doll R, Hill AB. The mortality of doctors in relation to their smoking habits; a preliminary report. Br Med J 1954;1:1451–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J., III Factors of risk in the development of coronary heart disease – six year follow-up experience. The Framingham Study. Ann Intern Med 1961;55:33–50. [DOI] [PubMed] [Google Scholar]
- 44.Smoking and Health. 1964.
- 45.The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General, 2014. 2014.
- 46.Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Prentice RL. Surrogate endpoints in clinical trials: definition and operational criteria. Stat Med 1989;8:431–440. [DOI] [PubMed] [Google Scholar]
- 48.Fleming TR, Prentice RL, Pepe MS, Glidden D. Surrogate and auxiliary endpoints in clinical trials, with potential applications in cancer and AIDS research. Stat Med 1994;13:955–968. [DOI] [PubMed] [Google Scholar]
- 49.Hughes MD. Evaluating surrogate endpoints. Control Clin Trials 2002;23:703–707. [DOI] [PubMed] [Google Scholar]
- 50.Molenberghs G, Buyse M, Geys H, Renard D, Burzykowski T, Alonso A. Statistical challenges in the evaluation of surrogate endpoints in randomized trials. Control Clin Trials 2002;23:607–625. [DOI] [PubMed] [Google Scholar]
- 51.Freedman LS, Graubard BI, Schatzkin A. Statistical validation of intermediate endpoints for chronic diseases. Stat Med 1992;11:167–178. [DOI] [PubMed] [Google Scholar]
- 52.Buyse M, Molenberghs G. Criteria for the validation of surrogate endpoints in randomized experiments. Biometrics 1998;54:1014–1029. [PubMed] [Google Scholar]
- 53.Buyse M, Molenberghs G, Burzykowski T, Renard D, Geys H. The validation of surrogate endpoints in meta-analyses of randomized experiments. Biostatistics 2000;1:49–67. [DOI] [PubMed] [Google Scholar]
- 54.Molenberghs G, Geys H, Buyse M. Evaluation of surrogate endpoints in randomized experiments with mixed discrete and continuous outcomes. Stat Med 2001;20:3023–3038. [DOI] [PubMed] [Google Scholar]
- 55.Weir CJ, Walley RJ. Statistical evaluation of biomarkers as surrogate endpoints: a literature review. Stat Med 2006;25:183–203. [DOI] [PubMed] [Google Scholar]
- 56.Domanski M, Pocock S, Bernaud C, Borer J, Geller N, Revkin J, Zannad F. Surrogate endpoints in randomized cardiovascular clinical trials. Fundam Clin Pharmacol 2011;25:411–413. [DOI] [PubMed] [Google Scholar]
- 57.Cholesterol Treatment Trialists C Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, Simes J, Collins R. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Charakida M, Masi S, Luscher TF, Kastelein JJ, Deanfield JE. Assessment of atherosclerosis: the role of flow-mediated dilatation. Eur Heart J 2010;31:2854–2861. [DOI] [PubMed] [Google Scholar]
- 59.Luscher TF, Taddei S, Kaski JC, Jukema JW, Kallend D, Munzel T, Kastelein JJ, Deanfield JE. Vascular effects and safety of dalcetrapib in patients with or at risk of coronary heart disease: the dal-VESSEL randomized clinical trial. Eur Heart J 2012;33:857–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Raman SV, Winner MW, III, Tran T, Velayutham M, Simonetti OP, Baker PB, Olesik J, McCarthy B, Ferketich AK, Zweier JL. In vivo atherosclerotic plaque characterization using magnetic susceptibility distinguishes symptom-producing plaques. JACC Cardiovasc Imaging 2008;1:49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Achenbach S, Raggi P. Imaging of coronary atherosclerosis by computed tomography. Eur Heart J 2010;31:1442–1448. [DOI] [PubMed] [Google Scholar]
- 62.Prati F, Regar E, Mintz GS, Arbustini E, Di Mario C, Jang IK, Akasaka T, Costa M, Guagliumi G, Grube E, Ozaki Y, Pinto F, Serruys PW. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Eur Heart J 2010;31:401–415. [DOI] [PubMed] [Google Scholar]
- 63.Lansky AJ, Desai K, Leon MB. Quantitative coronary angiography in regression trials: a review of methodologic considerations, endpoint selection, and limitations. Am J Cardiol 2002;89:4B–9B. [DOI] [PubMed] [Google Scholar]
- 64.Halim SA, Newby LK, Ohman EM. Biomarkers in cardiovascular clinical trials: past, present, future. Clin Chem 2012;58:45–53. [DOI] [PubMed] [Google Scholar]
- 65.Desch S, Eitel I, de Waha S, Fuernau G, Lurz P, Gutberlet M, Schuler G, Thiele H. Cardiac magnetic resonance imaging parameters as surrogate endpoints in clinical trials of acute myocardial infarction. Trials 2011;12:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mehta RH, Ou FS, Peterson ED, Shaw RE, Hillegass WB, Jr, Rumsfeld JS, Roe MT; American College of Cardiology-National Cardiovascular Database Registry I. Clinical significance of post-procedural TIMI flow in patients with cardiogenic shock undergoing primary percutaneous coronary intervention. JACC Cardiovasc Interv 2009;2:56–64. [DOI] [PubMed] [Google Scholar]
- 67.Shah A, Wagner GS, Granger CB, O'Connor CM, Green CL, Trollinger KM, Califf RM, Krucoff MW. Prognostic implications of TIMI flow grade in the infarct related artery compared with continuous 12-lead ST-segment resolution analysis. Reexamining the ‘gold standard’ for myocardial reperfusion assessment. J Am Coll Cardiol 2000;35:666–672. [DOI] [PubMed] [Google Scholar]
- 68.Packer M, Carver JR, Rodeheffer RJ, Ivanhoe RJ, DiBianco R, Zeldis SM, Hendrix GH, Bommer WJ, Elkayam U, Kukin ML, Mallis GI, Sollano JA, Shannon J, Tandon PK, DeMets DL; the PROMISE Study Research Group Effect of oral milrinone on mortality in severe chronic heart failure. The PROMISE Study Research Group. N Engl J Med 1991;325:1468–1475. [DOI] [PubMed] [Google Scholar]
- 69.McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Bohm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Kober L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Ronnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787–1847. [DOI] [PubMed] [Google Scholar]
- 70.Anand I, McMurray J, Cohn JN, Konstam MA, Notter T, Quitzau K, Ruschitzka F, Luscher TF. Long-term effects of darusentan on left-ventricular remodelling and clinical outcomes in the EndothelinA Receptor Antagonist Trial in Heart Failure (EARTH): randomised, double-blind, placebo-controlled trial. Lancet 2004;364:347–354. [DOI] [PubMed] [Google Scholar]
- 71.Gardner RS, Ozalp F, Murday AJ, Robb SD, McDonagh TA. N-terminal pro-brain natriuretic peptide. A new gold standard in predicting mortality in patients with advanced heart failure. Eur Heart J 2003;24:1735–1743. [DOI] [PubMed] [Google Scholar]
- 72.Breithardt G, Cain ME, El-Sherif N, Flowers N, Hombach V, Janse M, Simson MB, Steinbeck G. Standards for analysis of ventricular late potentials using high resolution or signal-averaged electrocardiography. A statement by a Task Force Committee between the European Society of Cardiology, the American Heart Association and the American College of Cardiology. Eur Heart J 1991;12:473–480. [DOI] [PubMed] [Google Scholar]