Abstract
Background
Reducing consumption of food away from home (FAFH) is often targeted during pediatric obesity treatment given associations with weight status and gain. However, the effects of this dietary change on weight loss are unknown.
Objective
Evaluate associations between changes in dietary factors and child anthropometric outcomes after treatment. It is hypothesized that reduced consumption of FAFH will be associated with improved dietary intake and greater reductions in anthropometric outcomes (standardized body mass index [zBMI] and percent body fat), and the relationship between FAFH and anthropometric outcomes will be mediated by improved child dietary intake.
Design
Longitudinal evaluation of associations between dietary changes and child anthropometric outcomes. Child diet (three 24-hour recalls) and anthropometric data were collected at baseline and 16-weeks.
Participants/setting
170 overweight and obese children ages 7–11 who completed 16-week family-based behavioral weight loss treatment (FBT) as part of a larger multi-site (MO and WA) randomized controlled trial (RCT) conducted in two cohorts between 2010–2011. Clinical research trial.
Intervention
Dietary treatment targets during FBT included improving diet quality and reducing FAFH.
Main Outcome Measures
Child relative weight (zBMI) and body composition (percent body fat)
Statistical Analyses Performed
T-tests, bootstrapped single mediation analyses adjusting for relevant covariates.
Results
As hypothesized, decreased FAFH was associated with improved diet quality and greater reductions in zBMI (Ps<0.05) and percent body fat (Ps<0.01). Associations between FAFH and anthropometric outcomes were mediated by changes in diet quality. Specifically, change in total energy intake and added sugars mediated the association between change in FAFH and zBMI, and change in overall diet quality, fiber, added sugars, and added fats mediated the association between change in FAFH and percent body fat. Including physical activity as a covariate did not significantly impact these findings.
Conclusions
These results suggest that reducing FAFH may be an important behavioral target for affecting positive changes in both diet quality and anthropometric outcomes during treatment.
Keywords: pediatric, obesity, food away from home, diet quality
INTRODUCTION
Childhood overweight and obesity rates in the U.S., estimated at 32.6% for children ages 6–11, have reached unprecedented levels.1 To effectively intervene, it is important to identify specific behavioral changes associated with reductions in weight. One such behavioral target, recommended for childhood obesity interventions is reducing the consumption of food away from home (FAFH);2 however, to our knowledge there have been no studies evaluating the impact of this change.
The link between consumption of FAFH and obesity is well-documented. Overweight and obese children eat a higher proportion of meals away from home than their normal-weight counterparts,3 and eating at least one meal/week away from home is associated with risk for obesity in children.4 Prospectively, consuming a higher proportion of FAFH is associated with increases in child relative weight (i.e., standardized body mass index [zBMI]) over time,5 and consuming breakfast away from home is associated with greater increases in body mass index (BMI) than consuming breakfast at home.6 These associations are likely due to the energy-dense nature of FAFH.7,8 Indeed, greater fast food consumption among children is associated with higher energy intake and poorer diet quality,9 and FAFH is typically served in larger portion sizes containing more calories than foods consumed at home.4 However, no previous research has examined the effect of reducing consumption of FAFH on pediatric anthropometric outcomes.
The present study aims to evaluate the associations between change in consumption of FAFH and changes in relative weight, body composition, and diet quality following family-based behavioral weight loss treatment (FBT), and to test the potential mediating role of changes in diet quality on the relationship between FAFH and changes in anthropometric outcomes (zBMI and percent body fat). It is hypothesized that 1) reducing energy from FAFH will be associated with improved diet quality, 2) reducing consumption of FAFH and improving diet quality will be associated with greater improvements in anthropometric outcomes, and 3) the relationship between decreased consumption of FAFH and improvements in anthropometric outcomes will be mediated by improvements in diet quality.
METHODS
Procedure
The present study is a longitudinal evaluation of associations between dietary changes and child anthropometric outcomes. The data were collected as part of a larger multi-site (St. Louis, MO, and Seattle, WA) randomized controlled trial examining the efficacy of different weight/behavioral maintenance programs following FBT. The present study examines only the FBT portion of the trial (conducted in two cohorts between 2010–2011), and all participants received the identical intervention, as randomization was conducted after FBT, when families entered the maintenance portion of the trial. A full description of the methods and procedures for the trial and associated treatment delivery is provided elsewhere.10 In brief, FBT is a multicomponent intervention that targets both dietary and physical activity modifications. Participants are encouraged to follow a low-energy density diet by decreasing consumption of high energy-dense and low nutrient foods (e.g., cookies, sugary drinks) and increasing consumption of low energy-dense and high nutrient foods (e.g., fruits, vegetables, lean proteins), thereby improving diet quality. One mechanism for affecting these changes, included in the present treatment, is to decrease consumption of FAFH (i.e., eat more foods prepared at home, and limit consumption of foods prepared outside of the home (e.g., full-service restaurants, fast food establishments, take-out foods, social or work gatherings, etc.) and treatment content included strategies to help families establish healthy patterns for doing so (e.g., planning home-cooked meals, simplifying food preparation, creating grocery lists).
Participants
Participants who entered the trial were 241 child-parent dyads. Participants were recruited in the Saint Louis, Missouri and Seattle, Washington areas through local media outlets, schools, organizations, pediatrician referrals, weight management clinics and word-of-mouth. Families were excluded from the trial if either the parent or child had an eating disorder, drug or alcohol dependence, or other mental illness diagnosis; low English comprehension; a physical illness or disability that prohibited following dietary recommendations or engaging in moderate to vigorous PA; or a medication that could affect weight. Children had a BMI≥85th percentile for age and sex, were 7–11 years old, and had at least one parent with a BMI≥25 kg/m2. FBT completers with complete anthropometric and dietary data were included as part of this secondary analysis (N=170 for zBMI, and N=113 for percent body fat). Participants included in the present analyses did not differ from those excluded on any demographic variables. Written informed consent and verbal assent were obtained from parents and children, respectively. Protocols were approved by the Institutional Review Boards at Washington University School of Medicine and Seattle Children’s Research Institute.
Measures
Demographics
At baseline, parents completed brief demographic questionnaires reporting child age, sex, and race/ethnicity. The Barratt Simplified Measure of Social Status11, adapted from the Hollingshead index of social status12, measured socioeconomic status. Higher values indicate higher SES.
Relative Weight
Child weight and height were measured at baseline and following FBT. Weight and height measurements were taken in light clothing with shoes removed on a calibrated electronic scale and stadiometer. Child BMI was calculated (kg/m2) and standardized according to age and sex based on CDC growth curves13 using the LMS method to calculate zBMI.
Body Composition
Children’s percent body fat was assessed via whole-body Dual-Energy X-Ray Absorptiometry (DXA) scans at baseline and post-FBT. DXA is a non-invasive and brief procedure that provides a validated measure of fat and lean mass in children and adults.14 The machines were regularly calibrated using phantoms of known composition, and the same machine was used within-site for all participants.
Dietary intake
A registered dietitian or trained bachelor’s-level nutritionist conducted three telephone-administered 24-hour dietary recalls at baseline and post-FBT using the Nutrition Data System for Research (NDS-R version 2009, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN). Interviews were conducted at both baseline and post-FBT on non-consecutive days, including at least one weekday and one weekend day, following standard protocols using the multiple-pass method.15 Parents completed the dietary recall for the child but were assisted by the child if present. The mean three-day average for each nutrient/food group was computed for both time points. Mean energy intake was categorized as consumed at home or away from home. When there was a discrepancy between where the meal was prepared versus eaten, it was coded for where it was prepared (e.g., if child ate a meal at home, but it was prepared at a restaurant it was coded as FAFH). The proportion of energy consumed from foods prepared away from home was calculated by dividing mean caloric intake consumed away from home by mean total caloric intake.
Diet Quality
Diet quality was assessed using the Healthy Eating Index-2005 (HEI-2005), a valid and reliable measure designed to assess adherence to the 2005 Dietary Guidelines from the United States Department of Agriculture (USDA).16 The scores range from 0–100, with a score of >80 indicating "good" diet quality. The HEI-2005 scores were calculated from the average of the NDS-R data using the method described by Miller et al.,17 with minor modifications for the “oils” category and “solid fats” component of the “Calories from Solid Fat, Alcohol, and Added Sugar” categories, as described by Wiltheiss.18
Physical Activity
Child physical activity was assessed using an Actigraph accelerometer, which has been shown to be a reliable and valid measure of moderate-to-vigorous physical activity (MVPA) in children.19,20 Children wore the Actigraph for seven consecutive days, which is sufficient to obtain an assessment of habitual physical activity.19,20 Age-specific cut-offs were used to determine minutes of MVPA (with 4 METs used as the criterion for moderate activity (a conservative criterion), and 6 and 9 METs for hard and very hard activity, respectively),21 and minutes spent engaging in MVPA were averaged across the collected days.
Statistical Analysis
For change variables, baseline values were subtracted from post-FBT values. Changes in nutrient/food group intake were previously reported from this trial.23 Linear regressions were used to test associations among energy from FAFH, diet quality, nutrients/food groups, and anthropometric outcomes. Nutrients/food groups associated with zBMI change were identified in previous analyses and include total energy, and percent energy from protein and fat. Because the HEI-2005 components are energy-adjusted using a density approach (food group/nutrient per 1000 kcals/d), the analyses did not control for change in total energy when examining associations with HEI-2005 scores.
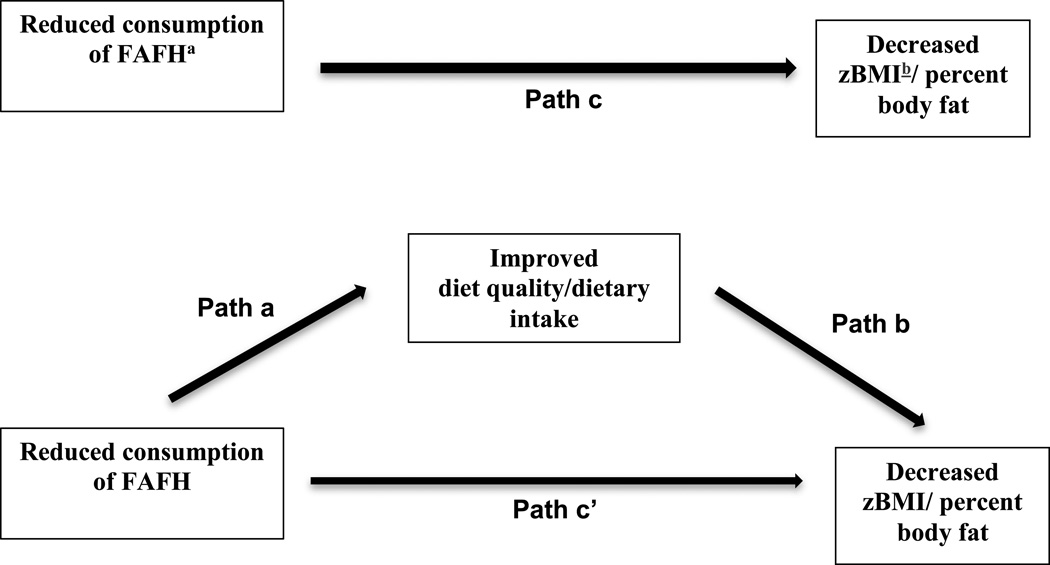
Single mediation models based on the Preacher and Hayes method22 were utilized to test the proposed mediation model (Figure 1). Separate models tested the mediating effects of change in HEI-2005 and each nutrient/food group that was significantly associated with change in energy from FAFH and zBMI (identified in previous analyses23) and percent body fat (identified in the present analyses). Covariates were decided a priori and included child age, race/ethnicity, sex, SES, site, and baseline values of the independent, dependent, and mediation variables. To test whether physical activity influenced the hypothesized associations, additional analyses were conducted in the 129 subjects with complete dietary and physical activity data using change in minutes of MVPA as a covariate. Models for nutrients/food groups, excluding the macronutrients expressed as a percent of total energy, included change in total energy as a covariate. A bootstrapping procedure using 5,000 resamples was conducted to calculate the 95% confidence intervals of each indirect effect. If the confidence interval did not contain zero, the indirect effect was considered to be significant.22 An alpha level of P<0.05 was set to determine significance. All analyses were conducted using SPSS version 19 (SPSS Inc., Chicago, IL).
Figure 1.
Proposed mediation model assessing whether changes in diet quality mediate the relationship between changes in energy from food prepared away from home (FAFH) and changes in anthropometric outcomes (Standardized Body Mass Index (zBMI) and percent body fat). Path c indicates the total effect of the association between reduced FAFH and the outcome variables when no mediator is included in the model. Path a indicates the relation between reduced consumption of FAFH on the mediator (changes in diet quality/dietary intake, included in separate single mediation models). Path b indicates the relation between the mediator and the outcome variable (change in anthropometric outcomes). Path c’ indicates the association between reduced FAFH and anthropometric changes when the mediator is included in the model.
a Food prepared away from home
b Standardized Body Mass Index
RESULTS
Participant characteristics and baseline and post-FBT anthropometrics and dietary intake are included in Table 1. Energy from FAFH and HEI-2005 scores significantly improved from baseline to post-FBT (Ps<0.001). Dietary changes that are associated with positive anthropometric outcomes are considered improvements.
TABLE 1.
Baseline demographic characteristics, and baseline and post-treatment dietary intake, and physical activity expenditure data of 170 children who completed family-based behavioral weight loss treatment.
| Race/Ethnicity, n. (%) | |
| Non-Hispanic Caucasian/White | 107 (62.9) |
| Non-Hispanic Black/African American | 29 (17.1) |
| Hispanic | 17 (10.0) |
| Othera | 17 (10.0) |
| Sex, n. (%) | |
| Male | 66 (38.8) |
| Female | 104 (61.2) |
| Child age at baseline, mean (SD), y | 9.4 (1.2) |
| Socioeconomic status, mean (SD), range | 43.8 (10.4), 10.0–65.0 |
| Relative weight/body composition | |
| Child zBMIb at baseline, mean (SD) | 2.16 (0.39) |
| Child zBMI post-FBT, mean (SD) | 1.87 (0.56)*** |
| Child percent body fat at baseline, % (SE) | 44.6 (6.5) |
| Child percent body fat post-FBTc, % (SE) | 40.8 (8.0)*** |
| Diet | |
| HEI-2005d score at baseline, mean (SD), range | 59.3 (8.8), 40.6–90.0 |
| HEI-2005 post-FBT, mean (SD), range | 74.5 (9.8)***, 48.8–95.4 |
| FAFHe baseline, mean (SD) | 0.4 (0.2) |
| FAFH post-FBT, mean (SD) | 0.3 (0.3)*** |
| Physical Activity | |
| MVPAf, baseline, mean (SD) | 47.16 (22.0) |
| MVPA post-FBT, mean (SD) | 44.49 (21.3) |
Other races included American Indian or Alaskan Native, Asian, Native Hawaiian or Other Pacific Islander, and “other” [self-reported]
Standardized Body Mass Index
Family-based Behavioral Weight Loss Treatment
Healthy Eating Index-2005
Energy from food prepared away from home
Minutes of Moderate-to-Vigorous Physical Activity
p<0.001
Associations between consumption of FAFH and diet
Decreases in energy from FAFH consumption were associated with increased HEI-2005 scores (p<0.001), fiber (P<0.001), healthy fruits and vegetables (P<0.001), and percent energy from protein (P<0.05) and carbohydrates (P<0.001), and with decreased total energy (P<0.001), added sugars (P<0.01), added fats (P<0.001), sugar-sweetened beverages (P<0.01), and percent energy from fat (P<0.001).
Associations among consumption of FAFH, diet and relative weight/body composition
Decreased consumption of energy from FAFH and increased HEI-2005 scores were associated with decreased zBMI (P<0.001, and P<0.05, respectively). A similar pattern of results was evident for percent body fat (Ps<0.01). In addition, decreased total energy, percent energy from fat, added sugars, and added fats, and increased percent energy from protein, fiber, and healthy fruits and vegetables (Ps<0.05) were associated with greater decreases in percent body fat (Table 2). Results from these models did not change with the inclusion of MVPA as a covariate. To further explore the independent effect of HEI-2005 scores and anthropometric changes, changes in energy balance behaviors were included as covariates in these analyses. After controlling for change in energy balance behaviors (total energy intake and minutes of MVPA), change in HEI-2005 scores remained significantly associated with both zBMI (P<0.05) and percent body fat (P<0.001).
TABLE 2.
Associations between change in proportion of energy consumed from FAFHa, diet quality and change in child relative weight and body compositionb
| Independent Variable | Beta | β |
P value |
|---|---|---|---|
| Main Outcome: Change in zBMIc (N=170)d | |||
| Change in FAFH | 0.269 | 0.273 | <0.001 |
| Change in HEI-2005e scoresf | −0.004 | −0.179 | 0.027 |
| Main Outcome: Change in Percent Body Fat (N=167) | |||
| Change in FAFH | 3.619 | 0.280 | 0.003 |
| Change in HEI-2005 scores | −0.070 | −0.270 | 0.004 |
| Change in total energy, kcals | 0.002 | 0.249 | 0.042 |
| Change in protein, % total energyf | −0.241 | −0.277 | 0.002 |
| Change in fat, % total energyf | 0.104 | 0.227 | 0.014 |
| Change in carbohydrates, % total energyf | −0.032 | −0.072 | 0.437 |
| Change in fiber, gf | −0.145 | −0.272 | 0.002 |
| Change in added sugars, gf | 0.037 | 0.422 | 0.004 |
| Change in healthy fruits and vegetables, svg/df | −0.331 | −0.213 | 0.011 |
| Change in added fats, svg/df | 0.947 | 0.457 | 0.002 |
| Change in sugar-sweetened beverages, svg/df | 1.113 | 0.241 | 0.122 |
Energy from food prepared away from home
Linear regression models were adjusted for child age, race/ethnicity, sex; family socioeconomic status; study site; and baseline values of the independent and dependent variables.
Standardized Body Mass Index
Associations between nutrients/food groups and change in BMI z-score have been previously reported from this trial.23
Healthy Eating Index-2005
Model was also adjusted for change in total energy.
Mediating effects of improved diet
Mediation models testing the effects of dietary changes on the association between changes in consumption of energy from FAFH and anthropometric outcomes were conducted to explore changes that may explain the relationship between decreased energy from FAFH and anthropometric outcomes (Table 3). Change in total energy intake, and added sugars mediated the relationship between changes in energy from FAFH and zBMI. Change in HEI-2005 scores, fiber, added fats, and added sugars mediated the relationship between consumption of energy from FAFH and percent body fat.
Table 3.
Mediation models testing the mediating role of diet in the association between change in proportion of energy consumed from FAFHa and change in child relative weight and body compositionb
| Mediator | Path ac | Path bd | Path ce | Path c’f | Indirect Effects (95% Confidence Interval)g |
%Mediatedh |
|---|---|---|---|---|---|---|
| Main outcome: change in zBMIi (N=170) | ||||||
| Change in HEI-2005j scores | 17.0478*** | −0.0018 | −0.2688*** | −0.2384** | −0.0304 (−0.0922, 0.0240) | N.S.k |
| Change in total energy, kcals | −418.3565*** | 0.0001** | −0.2693*** | −0.2070** | −0.0623 (−0.1272, −0.0230) | 23.1% |
| Change in protein, % total energy | 2.0151 | −0.0130** | −0.2465** | −0.2203** | −0.0263 (−0.0924, 0.0031) | N.S. |
| Change in fat, % total energy | −10.7141*** | 0.0025 | −0.2345** | −0.2079* | −0.0266 (−0.0857, 0.0320) | N.S. |
| Change in added sugars, gl | −25.7489*** | 0.0015o | −0.2463** | −0.2069 | −0.0395 (−0.1057, −0.0031) | 16.0% |
| Change in healthy fruit and vegetables, svg/dl | 3.1064*** | −0.0066 | −0.2518** | −0.2312** | −0.0205 (−0.0698, 0.0299) | N.S. |
| Change in sugar-sweetened beverages, svg/dl | −0.4533** | 0.0317 | −0.2482** | −0.2339** | −0.0144 (−0.0692, 0.0301) | N.S. |
| Main outcome: change in percent body fat (N=167) | ||||||
| Change in HEI-2005 scores | 16.9791*** | −0.0499 | −3.6431** | −2.7967* | −0.8465 (−1.8405, −0.1264) | 27.4% |
| Change in total energy, kcals | −407.7076*** | 0.0011 | −3.6428** | −3.2028* | −0.4400 (−1.2993, 0.2006) | N.S. |
| Change in protein, % total energy | 1.9808 | −0.2224** | −3.6485** | −3.2079** | −0.4406 (−1.5044, 0.0727) | N.S. |
| Change in fat, % total energy | −10.7296*** | 0.0693 | −3.5188** | −2.7755* | −0.7434 (−2.0360, 0.1362) | N.S. |
| Change in fiber, gl | 11.7469*** | −0.1121* | −3.2730** | −1.9566 | −1.3164 (−2.7438, −0.1525) | 40.2% |
| Change in added sugars, gl | −25.9139*** | 0.0281* | −3.6451** | −2.9161* | −0.7290 (−1.6676, −0.1470) | 20.0% |
| Change in healthy fruits and vegetables svg/dl | 3.1932*** | −0.2250 | −3.6234** | −2.9050* | −0.7185 (−1.7704, 0.0069) | N.S. |
| Change in added fats svg/dl | −1.2909*** | 0.7342* | −3.7152** | −2.7675* | −0.9477 (−2.2453, −0.1730) | 25.5% |
Energy from food prepared away from home
Mediation models adjusted for child age, race/ethnicity, sex; family socioeconomic status; study site; and baseline values of the mediator, independent and dependent variables. Unstandardized regression coefficients are reported for each path.
Path a indicates the relation between reduced consumption of FAFH on the mediator
Path b indicates the relation between the mediator and the outcome variable
Path c indicates the total effect of the association between reduced FAFH and the outcome variables when no mediator is included in the model.
Path c’ indicates the association between reduced FAFH and anthropometric changes when the mediator is included in the model.
Bootstrap results for indirect effects with bias-corrected confidence intervals set to 95% confidence (5000 bootstrap resamples).
% Mediated = [1 − (C’/C)] × 100.
Standardized Body Mass Index
Healthy Eating Index-2005
Mediation model not significant
Model also adjusted for total energy change.
P=<0.05,
P=<0.01,
P=<0.001
In the mediation models, the inclusion of MVPA as a covariate had a minor impact on the hypothesized associations with anthropometric outcomes. The mediation model testing change in total energy as a mediator for the association between change in FAFH and change in zBMI remained significant after controlling for change in physical activity (95% CI [−0.1454, −0.0229], 20.4% mediated), however, change in added sugars was no longer a significant mediator. Change in HEI-2005 scores and change in added sugars remained significant mediators for the association between change in FAFH and change in % body fat (95%CI [−2.6864, −0.4275], 34.3% mediated), however, change in fiber and change in added fats were no longer significant.
DISCUSSION
To maximize the efficacy of interventions for pediatric obesity, behavioral targets associated with changes in child anthropometric outcomes must be identified. The present results show that reduced consumption of FAFH was associated with reductions in child zBMI and percent body fat. The potential mechanism through which reducing FAFH is associated with improvements in anthropometric outcomes appears to be changes in diet quality. These results have potential implications for pediatric obesity interventions and suggest that reducing consumption of FAFH may be an important dietary target. Further research is needed to identify the most effective strategies for reducing FAFH (e.g. increased meal planning and preparation skills) and to determine the direct impact of reducing FAFH on anthropometric changes.
Previous research has examined the cross-sectional and longitudinal associations between consumption of FAFH and weight status and gain; however, to our knowledge the impact of reducing consumption of FAFH has not been examined. The results from the current study address this important gap in the literature by documenting the effect of this reduction on changes in anthropometric outcomes, including zBMI and percent body fat. At the start of treatment, participants ate approximately 40% of their energy from FAFH, higher than the national average of 35% for all children of this age group,24 and reduced to slightly below the national average, 32%, by the end of FBT. As hypothesized, this reduction in energy from FAFH was associated with improvements in dietary intake and significant reductions in zBMI and percent body fat. Given the demonstrated importance of reducing energy from FAFH on anthropometric outcomes, it is also important to explore mechanisms by which reducing energy from FAFH may affect these changes. These results suggest that improvements in dietary intake mediate the associations with improved anthropometric outcomes. These findings support and extend previous findings that consumption of FAFH is associated with poorer nutrition, specifically higher fat content and greater caloric intake.4,8
Interestingly, the mediation results differed for zBMI and percent body fat. Whereas improved HEI-2005 scores did not mediate the association between changes in energy from FAFH and zBMI as hypothesized, they significantly mediated reductions in percent body fat. In contrast, reduced total energy intake did not mediate the association between change in energy from FAFH and percent body fat, but significantly mediated changes in energy from FAFH and zBMI. It is possible that the significant association between changes in HEI-2005 and percent body fat may have occurred through another energy balance behavior, such as increases in physical activity. Indeed, increased physical activity has been associated with greater reductions in body fat, but not zBMI.25 Research has also shown that FAFH is negatively,26 and diet quality is positively27 associated with exercise in adults, which may suggest that children who increased HEI-2005 scores may also have increased their physical activity. To test this hypothesis, analyses were run in a subsample of subjects who had complete physical activity data (N=129) using the energy balance behaviors as covariates. After controlling for change in physical activity in the mediation model, the results strengthened, and p-values for path b approached significance (P=0.08), suggesting that physical activity may be impacting the relationship between percent body fat and HEI-2005. It should be noted that a sizeable portion of the sample size failed to complete the physical activity data and therefore a loss of power occurred with its inclusion, thus these results should be interpreted with caution and additional research with larger sample sizes is needed to further explore this finding.
The results in the present study also indicate that improvement in diet quality, as measured by the HEI-2005, was independently associated with decreased child zBMI and percent body fat, and these results held when controlling for changes in total energy and MVPA, indicating that improvements in diet quality elicited positive changes in percent body fat independent of changes in energy balance behaviors. While the observed finding is novel and has implications for treatment, the current study was not designed to test these associations. Further research is needed to explore this finding and to examine the mechanisms by which improved diet quality is associated with greater changes in body composition, and the degree to which reducing FAFH facilitates improvements in diet quality.
Overall, our findings indicate that reducing FAFH is associated with improved diet quality, total energy intake, and weight loss. In order to achieve this target, interventions may focus on helping families increase at-home meal preparation by teaching skills and strategies to overcome barriers to engaging in this behavior (e.g., help families learn how to plan meals, shop for groceries, prepare foods, identify ways to minimize costs and time associated with preparing food at home).
There are limitations to this study. Consumption of FAFH and diet quality were measured at the same timepoint, which limits the ability to determine temporality for the observed associations. The present sample is both treatment-seeking and -completing; thus, they may have higher motivation for change than other populations, and thus these findings may not generalize to other populations. Also, the dietary data were obtained through self-report/parent-report on child, allowing for the possibility of recall bias. However, this form of report has been validated and is considered the most accurate assessment method for children aged 4–11 years.15 Strengths include a large sample size, three days of high-quality recall data that were averaged to provide a comprehensive evaluation of child diet, and high-quality body composition data.
CONCLUSION
Limiting the amount of food consumed outside of the home at restaurants or fast food venues is frequently recommended for weight management. The current study found evidence to support this recommendation and a potential mechanism for the effects. These results suggest that reducing consumption of FAFH may lead to improvements in diet quality and weight loss. Additional research is needed to replicate this finding, determine whether changes in FAFH cause improvements in diet quality and anthropometric outcomes and mechanisms for this occurrence, and determine the most effective intervention strategies to achieve this target.
Acknowledgments
Sources of funding and support: This work was supported by National Institutes of Health (NIH) Grants
5-RO1HD036904 (National Institute of Child Health and Human Development), 5K24MH070446 (National Institute of Mental Health), and 5T32HL007456 (National Heart, Lung, and Blood Institute [NHLBI]). Some authors were supported by NIH Grant 5T32HL007456 (NHLBI), and KL2RR024994 (National Center for Research Resources). This work was also made possible by NIH Grant UL1 RR024992 (National Center for Research Resources).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure of conflicts of interest: None reported
Contributor Information
Myra Altman, Washington University in St. Louis, Department of Psychology, Campus Box 8134, 660 S. Euclid, St. Louis, MO 63110, Phone: 314-286-2108, Fax: 314-286-2091, altmanm@psychiatry.wustl.edu.
Jodi Cahill Holland, At time of completion of work: Postdoctoral Fellow, Washington University School of Medicine, Department of Psychiatry, Campus Box 8134, 660 S. Euclid, St. Louis, MO 63110, Phone: 512-740-5188, Fax: 314-286-2091, jodicahill@austin.rr.com. At present: no affiliation.
Delaney Lundeen, At time of completion of work: Graduate Student, Saint Louis University, Department of Nutrition and Dietetics, dlundeen@slu.edu
Rachel P. Kolko, Washington University in St. Louis, Department of Psychology, Campus Box 8134, 660 S. Euclid, St. Louis, MO 63110, Phone: 314-286-0253, Fax: 314-286-2091, kolkor@psychiatry.wustl.edu.
Richard I. Stein, Medicine, Washington University School of Medicine, Department of Internal Medicine, Campus Box 8083 660 S. Euclid Ave., St. Louis, MO 63110, Phone: 314-286-0077, Fax: 314-286-2085, rstein@dom.wustl.edu.
Brian E. Saelens, Pediatrics and Psychiatry and Behavioral Sciences, University of Washington, Seattle Children’s Research Institute, CW8-6 - Child Health, Behavior and Development, 2001 Eighth Ave Seattle, WA 98121, Phone: 206-884-7800, brian.saelens@seattlechildrens.org.
R. Robinson Welch, Psychiatry, Washington University School of Medicine, Department of Psychiatry, Campus Box 8134, 660 S. Euclid, St. Louis, MO 63110, Phone: 314-286-2117, Fax: 314-286-2091, welchr@psychiatry.wustl.edu.
Michael G. Perri, Robert G. Frank Professor of Clinical and Health Psychology, College of Public Health and Health Professions, University of Florida, 1225 Center Drive, HPNP Suite 4101, Gainesville, FL 32611, Phone: 352-273-6214, Fax: 325-273-6199, mperri@phhp.ufl.edu
Kenneth B. Schechtman, Washington University School of Medicine, Division of Biostatistics, Box 8067, 660 S. Euclid Avenue, St. Louis, MO 63110-1093, Phone: 3l4-362-2271, Fax: 314-362-2693, ken@wubios.wustl.edu.
Leonard H. Epstein, Behavioral Medicine, University at Buffalo School of Medicine and Biomedical Sciences, Department of Pediatrics, Phone: 716-829-3400, Fax: 716-829-3993, lhenet@buffalo.edu.
Denise E. Wilfley, Psychiatry, Medicine, Pediatrics, and Psychology, Washington University School of Medicine, Department of Psychiatry, Campus Box 8134, 660 S. Euclid, St. Louis, MO 63110, Phone: 314-286-2117, Fax: 314-286-2091, wilfleyd@psychiatry.wustl.edu.
References
- 1.Ogden Cl, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among us children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spear BA, Barlow SE, Ervin C, et al. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007 Dec;120(Suppl 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 3.Gillis LJ, Bar-Or O. Food Away from Home, Sugar-Sweetened Drink Consumption and Juvenile Obesity. J Am Coll Nutr. 2003;22(6):539–545. doi: 10.1080/07315724.2003.10719333. [DOI] [PubMed] [Google Scholar]
- 4.Ayala GX, Rogers M, Arredondo EM, et al. Away-from-home food intake and risk for obesity: examining the influence of context. Obesity (Silver Spring) 2008 May;16(5):1002–1008. doi: 10.1038/oby.2008.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson OM, Ballew C, Resnicow K, et al. Food purchased away from home as a predictor of change in BMI z-score among girls. Int J Obes Relat Metab Disord. 2004 Feb;28(2):282–289. doi: 10.1038/sj.ijo.0802538. [DOI] [PubMed] [Google Scholar]
- 6.Tin SP, Ho SY, Mak KH, Wan KL, Lam TH. Location of breakfast consumption predicts body mass index change in young Hong Kong children. Int J Obesity. (2005) 2012 Jul;36(7):925–930. doi: 10.1038/ijo.2011.262. [DOI] [PubMed] [Google Scholar]
- 7.Ries CP, Kline K, Weaver SO. Impact of commercial eating on nutrient adequacy. J Am Diet Assoc. 1987 Apr;87(4):463–468. [PubMed] [Google Scholar]
- 8.Guthrie JF, Lin B-H, Frazao E. Role of Food Prepared Away from Home in the American Diet, 1977–78 versus 1994–96: Changes and Consequences. JNEB. 2002;34(3):140–150. doi: 10.1016/s1499-4046(06)60083-3. [DOI] [PubMed] [Google Scholar]
- 9.Powell LM, Nguyen BT. Fast-food and full-service restaurant consumption among children and adolescents: effect on energy, beverage, and nutrient intake. JAMA Pediatrics. 2013 Jan;167(1):14–20. doi: 10.1001/jamapediatrics.2013.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Best JR, Theim KR, Gredysa DM, et al. Behavioral economic predictors of overweight children’s weight loss. J Consult Clin Psych. 2012;80(6):1086–1096. doi: 10.1037/a0029827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hollingshead AB. Four-Factor Index of Social Status. 1975 Unpublished manuscript. [Google Scholar]
- 12.Barratt W. The Barratt Simplified Measure of Social Status. 2006 Unpublished manuscript. [Google Scholar]
- 13.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- 14.TODAY Study Group. Treatment options for type 2 diabetes in adolescents and youth: a study of the comparative efficacy of metformin alone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatr Diabetes. 2007 Apr;8(2):74–87. doi: 10.1111/j.1399-5448.2007.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burrows TLMR, Collins CE. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J Am Diet Assoc. 2010;110:1501–1510. doi: 10.1016/j.jada.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 16.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1854–1864. doi: 10.1016/j.jada.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Miller PE, Mitchell DC, Harala PL, Pettit JM, Smiciklas-Wright H, Hartman TJ. Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutr. 2011 Feb;14(2):306–313. doi: 10.1017/S1368980010001655. [DOI] [PubMed] [Google Scholar]
- 18.Wiltheiss GA, Lovelady CA, West DG, Brouwer RJN, Krause KM, Østbye T. Diet Quality and Weight Change among Overweight and Obese Postpartum Women Enrolled in a Behavioral Intervention Program. J Acad Nutr Diet. 2013;113(1):54–62. doi: 10.1016/j.jand.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janz KF, Witt J, Mahoney LT. The stability of children's physical activity as measured by accelerometry and self-report. Med Sci Sports Exerc. 1995;27(9):1326–1332. [PubMed] [Google Scholar]
- 20.Trost SG, Ward DS, Moorehead SM, Watson PD, Riner W, Burke JR. Validity of the computer science and applications (CSA) activity monitor in children. Med Sci Sports Exerc. 1998;30(4):629–633. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- 21.Freedson PS, Sirard J, Debold E, Pate R, Dowda M, Trost S, Sallis JF. Calibration of the Computer Science and Applications, Inc. (CSA) accelerometer. Med Sci Sports Exerc. 1997;29(suppl):45. [Google Scholar]
- 22.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008 Aug;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 23.Cahill Holland J, Kolko RP, Stein IR, et al. Modifications in parent feeding practices and child diet during family-based behavioral treatment improve child zBMI. Obesity. 2014;22(5):E119–E126. doi: 10.1002/oby.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poti JM, Popkin BM. Trends in energy intake among US children by eating location and food source, 1977–2006. J Am Diet Assoc. 2011 Aug;111(8):1156–1164. doi: 10.1016/j.jada.2011.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen DA, Ghosh-Dastidar B, Conway TL, et al. Energy balance in adolescent girls: The trial of activity for adolescent girls cohort. Obesity (Silver Spring) 2013 Jun 26; doi: 10.1002/oby.20536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fuglestad PT, Jeffery RW, Sherwood NE. Lifestyle patterns associated with diet, physical activity, body mass index and amount of recent weight loss in a sample of successful weight losers. Int J Behav Nutr Phys Act. 2012;9:79. doi: 10.1186/1479-5868-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin CT, Gao Z, Lee JY. Associations between self-reported weight management methods with diet quality as measured by the Healthy Eating Index-2005. Prev Med. 2013 Jun 6; doi: 10.1016/j.ypmed.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 28.Jennings A, Welch A, van Sluijs EMF, Griffin SJ, Cassidy A. Diet Quality Is Independently Associated with Weight Status in Children Aged 9–10 Years. J Nutr. 2011 Mar 1;141(3):453–459. doi: 10.3945/jn.110.131441. 2011. [DOI] [PubMed] [Google Scholar]
- 29.Kranz S, Findeis JL, Shrestha SS. Use of the Revised Children's Diet Quality Index to assess preschooler's diet quality, its sociodemographic predictors, and its association with body weight status. J Pediatr. 2008 Jan-Feb;84(1):26–34. doi: 10.2223/JPED.1745. [DOI] [PubMed] [Google Scholar]
- 30.Raynor HA, Looney SM, Steeves EA, Spence M, Gorin AA. The effects of an energy density prescription on diet quality and weight loss: a pilot randomized controlled trial. J Acad Nutr Diet. 2012 Sep;112(9):1397–1402. doi: 10.1016/j.jand.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 31.Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007 Jun 1;85(6):1465–1477. doi: 10.1093/ajcn/85.6.1465. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ludwig DS, Friedman MI. Increasing adiposity: Consequence or cause of overeating? JAMA. 2014;311(21):2167–2168. doi: 10.1001/jama.2014.4133. [DOI] [PubMed] [Google Scholar]