Abstract
Titanium dioxide nanoparticles (TiO2NPs) suspensions (concentration 1.0 g/L) in synthetic sweat solution were applied on Franz cells for 24 h using intact and needle-abraded human skin. Titanium content into skin and receiving phases was determined. Cytotoxicity (MTT, AlamarBlue® and propidium iodide, PI, uptake assays) was evaluated on HaCat keratinocytes after 24 h, 48 h, and seven days of exposure. After 24 h of exposure, no titanium was detectable in receiving solutions for both intact and damaged skin. Titanium was found in the epidermal layer after 24 h of exposure (0.47 ± 0.33 μg/cm2) while in the dermal layer, the concentration was below the limit of detection. Damaged skin, in its whole, has shown a similar concentration (0.53 ± 0.26 μg/cm2). Cytotoxicity studies on HaCaT cells demonstrated that TiO2NPs induced cytotoxic effects only at very high concentrations, reducing cell viability after seven days of exposure with EC50s of 8.8 × 10−4 M (MTT assay), 3.8 × 10−5 M (AlamarBlue® assay), and 7.6 × 10−4 M (PI uptake, index of a necrotic cell death). Our study demonstrated that TiO2NPs cannot permeate intact and damaged skin and can be found only in the stratum corneum and epidermis. Moreover, the low cytotoxic effect observed on human HaCaT keratinocytes suggests that these nano-compounds have a potential toxic effect at the skin level only after long-term exposure.
Keywords: titanium dioxide, nanoparticles (NPs), in vitro, human skin absorption, cytotoxicity
1. Introduction
Titanium dioxide nanoparticles (TiO2NPs) are being widely used in industrial and consumer products due to their strong catalytic activity as compared to their fine-particle counterpart. This characteristic has been attributed to their larger surface area per unit mass, given their smaller size [1].
TiO2 is in the top five NPs used in a wide array of consumer products [2], including cosmetics, toothpaste [3], sunscreens [4], and skin treatments for acne vulgaris, condyloma acuminata, atopic dermatitis, hyper-pigmented skin lesions, and other non-dermatologic diseases [5]. TiO2 is the most widely used nanomaterial in dermal consumer products [6]. It is also present in paints, foods, and pigments [7]. TiO2 appears as a white powder and its nanoparticle formulation is preferred in the cosmetics industry because it avoids white coloration of the skin after application.
Chronic toxicity studies on TiO2 focus on the respiratory system, but more effort should be put into studying chronic exposure for topically applied consumer goods, especially with the increase in consumer use of sunscreens that contain TiO2NPs [1].
TiO2NPs present in cosmetics have the potential to penetrate through the stratum corneum into viable skin layers via intercellular channels, hair follicles, and sweat glands [8]. Several authors have studied the possible penetration of TiO2NPs into the skin, using both naked and coated titania samples [9,10,11,12,13], finding that TiO2 does not penetrate the skin and the underlying living tissue, remaining on the skin surface or only impregnating the first layers of the stratum corneum. Monterio-Riviere et al. [14] showed minimal penetration after UVB exposure in vitro and in vivo skin. In 2010, Kiss et al. [15] investigated the in vivo penetration of TiO2 on human skin transplanted to immunodeficent mice. They demonstrated in vivo that TiO2NPs do not penetrate the intact epidermal membrane, but exposed directly to cell culture in vitro, they exert significant effects on cell viability. The cytotoxicity of TiO2NPs was demonstrated in keratinocytes, using different tests and exposures, with or without UV exposure [1,16,17,18,19], but many in vivo experiments on animals did not confirm this effect [1]. More recently, Adachi et al. [20] and Wu et al. [21] found signs of irritant dermatitis with focal parakeratosis in the stratum corneum and epidermal spongiosis after applying uncoated TiO2NPs for long time. Wu et al. [21] found that these NPs can penetrate into the deep layer of the viable epidermis in pig ears after 30 days of exposure and into the hairless skin mouse, inducing pathological changes in major organs after 60 days. However, these results were contested by Jonaitis et al. [22] who reported methodological deficiencies. Also Sadrieh et al. [23] found TiO2 in the dermis after 22 days of application of sunscreen creams containing TiO2NPs in miniature pigs, but they suspected a contamination.
In most of available study results, after TiO2NP dermal exposure, TiO2NPs are not significantly systematically available [1]. The lack of penetration through the epidermis is also the main reason for the absence of skin carcinogenesis-promoting effects [24,25]. However, other studies such as Tan et al. [26] found, via tape stripping technique, that, levels of TiO2NPs in the epidermis and dermis of subjects who applied a sunscreen containing 8% TiO2NPs were higher than the levels found in controls,. This difference was not statistically significant given the small sample size. Bannat and Müller-Goymann [27] (applying an oil-in-water emulsion with 5% TiO2NPs) found that TiO2NPs may be able to penetrate the surface through hair follicles or pores, but no details are given on the fate of such particles.
Adachi et al. [20] applied an emulsion containing 10% wt% TiO2NPs to the dorsal skin of hairless rats for 56 days and found that the particles were only located in the stratum corneum layer of the epidermis and follicular epithelium. They did not find any evidence of TiO2 penetration into viable areas. Moreover, these authors did not find titanium in the internal organ using inductively coupled plasma mass spectroscopy. An increased titanium concentration was found only in the lung samples, probably due to the inhalation of TiO2NPs.
It is unlikely that metal oxide nanoparticles penetrate intact human skin under normal conditions, given the tough layer of the stratum corneum, but the impairment of the stratum corneum could increase the skin penetration of nanoparticles [8,28]. Previous in vitro data on pig skin treated with tape stripping to remove the stratum corneum [11] did not demonstrate TiO2NP skin absorption. However, no data are available on TiO2NP absorption using a needle-abraded skin protocol in human skin. It is important to verify if, in a damaged skin condition, TiO2NPs fails to cross the skin barrier, as an impairment of the stratum corneum is very common in workers (i.e., wet workers, construction workers, healthcare workers) [29].
To increase the knowledge on this topic, we studied the in vitro skin absorption of TiO2NPs on intact and damaged human skin with the protocol defined in the European project EDETOX [30] which is used to study other kinds of NPs [31,32,33]. To complete our study, we tested TiO2NPs used in skin penetration tests to evaluate their toxicity on short- and long-term exposures (24–48 h and seven days) on keratinocytes.
2. Experimental Section
2.1. Chemicals
All chemicals were analytical grade. Urea, sodium chloride, sodium hydrogen phosphate, potassium dihydrogenphosphate were purchased from Carlo Erba (Milan, Italy); lactic acid (90% v/v) was bought from Acros Organics (Geel, Belgium); nitric acid (69.5% v/v), hydrogen peroxide (30% v/v), hydrofluoric acid (48% w/v), and ammonium hydroxide (25% w/v) were from Sigma Aldrich (Milan, Italy). Water reagent grade was produced with a Millipore purification pack system (Milli-Q water). The physiological solution used as the receptor phase was prepared by dissolving 2.38 g of Na2HPO4, 0.19 g of KH2PO4, and 9 g of NaCl into 1 L of Milli-Q water (final pH seven.35). The synthetic sweat solution used as donor fluid consisted of 0.5% sodium chloride, 0.1% urea, and 0.1% lactic acid in Milli-Q water; pH 4.5 was adjusted with ammonia.
We used the commercially available TiO2 nanopowder (CAS 13463-67-7, n. 677469 provided by Sigma Aldrich—Milan, Italy).
2.2. Nanoparticle Characterization
The TiO2 NPs were investigated by Transmission Electron Microscopy (TEM) once they were dispersed in synthetic sweat and at the end of the experiments (after the 24 h exposure time) to visualize the dimensions of the NPs and the aggregation state of the donor phase. In addition, by performing electron diffraction experiments the crystalline phases of the TiO2 nanopowder were checked. In agreement with the Raman characterization reported in [34], the dominant phase observed for the NPs is anatase (>90%), while a small amount of the NPs show a rutile structure.
Since the behavior and the aggregation state of the NPs in different mediums depend strongly on the surface charge of the NPs and the ionic strength of the suspension, a further characterization using both Dynamic Light Scattering and Z-potential techniques has been carried out. The investigation was performed using the 90Plus PALS instrument (Brookhaven Corp., Holtsville, NY, USA). In Alinovi et al. 2015 [34] the complete characterization is reported.
Finally, in order to evaluate the ions released from the NPs once they were put in synthetic sweat, 4 mL of the donor phase was ultra-filtered using the Amicon Ultra-4 centrifugal filters (10K MWCO). The ultrafiltration has been performed in centrifuge at 5000 rpm for 30 min in order to remove the NPs, but not eventual titanium ions, from the solution. The solution has been analyzed by ICP-AES to quantify the titanium concentration. The ultrafiltration has been repeated on three different aliquots at the beginning of the permeation experiments and on three other aliquots at the end of the 24-h exposure time. The titanium concentration was always below the limit of detection.
2.3. Preparation of Skin Membranes
Human abdominal full thickness skin was obtained as surgical waste from patients aged 45–65 years. After the skin excision, subcutaneous fat was removed with a scalpel blade and hair shaved from the epidermal layer, then skin samples were stored at −25 °C for a period up to, but not exceeding, 4 months. It has been demonstrated that this procedure does not damage skin barrier properties. At the day of the experiment, skin samples were defrosted in physiological solution at room temperature for a 30 min period and then 4 × 4 cm2 pieces were cut from each skin specimen and mounted separately on the diffusion cells. Damaged skin samples were obtained using a needle-abrasion technique described elsewhere [35]. Skin integrity was tested before and after each experiment using electrical conductibility by means of a conductometer (Metrohm, 660, Metrohm AG Oberdorfstr. 68 CH-9100 Herisau) operating at 300 Hz and connected to two stainless steel electrodes [36]. The conductibility data in µS were converted into KΩ/cm2. Cells with a resistance lower than 3.95 ± 0.27 KΩ/cm2 were considered to be damaged and rejected as suggested by Davies et al. [37].
2.4. In Vitro Diffusion System
Percutaneous absorption studies were performed using static diffusion cells following the Franz method [38]. The receptor compartment had a mean volume of 14.0 mL and was maintained at 32 °C by means of circulation of thermostated water in the jacket surrounding the cell. This temperature value was chosen in order to reproduce the hand physiological temperature at normal conditions. The physiological solution used as the receptor phase was prepared by dissolving 2.38 g of Na2HPO4, 0.19 g of KH2PO4, and 9 g of NaCl into 1 L of Milli-Q water (final pH 7.35).
The concentration of the salt in the receptor fluid was approximately the same that can be found in the blood. The physiological solution used as the receiving phase was continuously stirred using a Teflon-coated magnetic stirrer. Each piece of skin was clamped between the donor and the receptor compartment; the mean exposed skin area was 3.29 cm2 and the average membrane thickness was 1 mm. Two different experiments were conducted using intact (experiment 1) and damaged skin (experiment 2) as described below.
2.5. Experiment 1
The donor phase was prepared just before the experiment using a sonicated suspension of TiO2NPs at a concentration of 1.0 g/L dispersed in synthetic sweat at pH 4.5 to reproduce the in vivo condition. The TiO2 concentration in the donor phase was confirmed by Inductively Coupled Plasma-Atomic Emission Spectroscopy (ICP-AES) analysis prior to the test.
At time 0, the exposure chambers of 6 Franz diffusion cells were mounted with intact skin samples and filled with 2.5 mL of the donor suspension (606 μg/cm2) to ensure an infinite dose. The experiment was run for 24 h, and during this period, 1.5 mL of the dermal bathing solution was removed at selected intervals (4, 8, 16, 24 h) and analyzed. Each receptor sample was immediately replaced with an equal volume of fresh physiological solution. At 24 h the dermal bathing solution and the donor phase of each diffusion cell were recovered for the following analysis.
2.6. Experiment 2
Experiment 1 was repeated using an abraded skin protocol as suggested by Bronaugh and Steward [35]. Skin was abraded by drawing the tip of a 19-gauge hypodermic needle across the surface (20 marks in one direction and 20 perpendicular).
2.7. Blanks
For each experiment, two cells were added as blanks. The blank cells were treated as the other cells with the exception that only synthetic sweat was used in the donor compartment.
2.8 Skin Digestion after the Experiment
After the experiment, the skin pieces were washed three times with physiological solution to remove TiO2NPs on the skin, then removed from the diffusion cells and treated as follows: Skin samples from exp. 1 were separated into epidermis and dermis by heat shock immerging in water at 60 °C for 1 min before freezing, while skin samples from exp. 2 were simply stored in a freezer at −25 °C. At the time of the analysis, the skin membranes were dried for 2 h at room temperature, then cut into sections, weighed, and put into 100 mL disposable DigitubesTM with 10 mL of HNO3 and 2 mL of H2O2 for digestion. They were heated for 24 h at 90 °C in a block heater (SPB 100-12, PerkinElmer), then 0.2 mL of HF was added, and heated until the remaining solutions were of 2 mL in volume. The solutions were diluted to a volume of 10 mL with Milli-Q water for the analysis with ICP-AES.
2.9. Analytical Measurements
The metal concentrations in the receiving phase skin were determined by Zeeman corrected graphite furnace atomic absorption spectrophotometry (GF-AAS) using a Varian Duo instrument (GTA 120, AA 240 Z). The calibration standards were prepared by standard solutions of single elements ranging from 0.5 to 1000 µg/L: Titanium in H2O atomic absorption standard solution (Sigma-Aldrich, Milwaukee, WI, USA). The limit of detection (LOD) calculated as three standard deviations of the background signal obtained on 10 blind samples at the operative wavelength of 364.3 nm was 5 µg/L. The precision of the measurements as relative standard deviation (RSD%) for the analysis was always less than 5%.
Total titanium concentration in the donor phases and in the solutions resulting from the mineralization of the skin samples were performed by Inductively Coupled Plasma-Atomic Emission Spectrometry (ICP-AES) using a Spectroflame Modula E optical plasma interface (OPI) instrument (by SPECTRO, Germany). The analyses were conducted using a calibration curve obtained by dilution (range: 0–10 mg/L) of titanium standard solution for ICP-AES analyses (by Teknolab A/S, Norway). The limit of detection (LOD) at the operative wavelength of 334.941 nm was 20 µg/L. The precision of the measurements as relative standard deviation (RSD%) for the analysis was always less than 5%.
2.10. Cell Tests
2.10.1. Cell Culture
The immortalized human keratinocyte HaCaT [39] cell line was purchased from Cell Line Service (DKFZ, Eppelheim, Germany). Cells were cultured in high-glucose Dulbecco’s Modified Eagle’s medium (DMEM) supplemented with 2 mM L-Glutamine, 100 U/mL penicillin-100 µg/mL streptomycin, and 10% fetal bovine serum (FBS) at 37 °C in a 5% CO2 atmosphere. Cells received fresh medium every 3 days and were subcultured every seven days.
Stock solutions of TiO2NPs (1000 µg/mL ethanol) were diluted to the required concentrations (1.5 × 10−7–1.0 × 10−3 M equal to 0.007–50 μg/cm2) in the cell culture medium and sonicated before use.
2.10.2. MTT Assay
Cells (5 × 103 cells/well) were plated in 96-well plates for 24 h and then exposed to TiO2NPs (1.5 × 10−7–1.0 × 10−3 M equal to 0.007–50 μg/cm2). After 24, 48 h, and seven days of exposure, a 10% MTT solution was added and, after 4 h, the insoluble crystals were solubilized with DMSO [40]. Plates were read in a Microplate Autoreader (Bio-Tek Instruments) at 540/630 nm. Data are reported as percentages of control and are the mean ± SE of four independent experiments performed in triplicate.
Unspecific reactions of TiO2NPs with MTT reagents was excluded by preliminary experiments.
Furthermore, two washes were performed after TiO2 cell treatments and before MTT. This procedure should in any case avoid or drastically reduce false positive results deriving from unspecific reactions between TiO2 and the dyes.
2.10.3. AlamarBlue® Assay
Cells (15 × 103 cells/well) were cultured in 96-well plates and, after 24h, exposed to TiO2NPs (1.5 × 107–1.0 × 10−3 M equal to 0.007–50 μg/cm2) for 24, 48 h, and seven days. After 4 h of incubation with the AlamarBlue® reagent, fluorescence intensity was read by a FluoroCount Microplate Fluorometer (Packard, Germany) at an excitation wavelength of 530 nm and emission wavelength of 590 nm. Data are reported as a percentage of control and are the mean ± SE of four independent experiments performed in triplicate.
Unspecific reactions of TiO2NPs with AlamarBlue® reagents were excluded by preliminary experiments.
Furthermore, two washes were performed after TiO2 cell treatments and before AlamarBlue®. This procedure should in any case avoid or drastically reduce false positive results deriving from unspecific reactions between TiO2 and the dyes.
2.10.4. Propidium Iodide Uptake
Cells (1 × 105 cells/well) were seeded in 96-well plates and, after 24 h, exposed to TiO2NPs (1.5 × 10−7–1.0 × 10−3 M equal to 0.007–50 μg/cm2) for seven days. Propidium iodide (PI) uptake was performed as previously described [41,42]. Briefly, after treatment, cells were rinsed with 200 μL of 3.0 × 10−6 M PI in phosphate-buffered saline (PBS) and fluorescence intensity was read by a FluoroCount Microplate Fluorometer (Packard, Germany) at an excitation length of 530 nm and emission length of 590 nm after 30 min.
All samples were subsequently permeabilized with 1% Triton-X for 30 min to obtain total cell content for each sample and fluorescence read. Positive control was obtained by permeabilizing untreated cells with 1% Triton-X. Data are reported as % of positive control (equal to 100% PI uptake) after normalization on total cell content and are the mean ± SE of three independent experiments performed in triplicate.
2.11. Statistical Analysis
Ti concentration data (μg/cm3) in the receptor solution were converted to the total amount that penetrated (μg/cm2), with a correction for dilution due to sample removal.
Data analysis were performed with Excel 2007 for Windows, and Stata Software, version 11.0 (StataCorp LP, College Station, TX, USA). Skin absorption data were reported as mean ± standard deviation (SD). The difference among independent data was assessed by means of the Mann-Whitney test.
Cytotoxicity data were reported as mean ± standard error (SE) of at least three independent experiments performed in triplicate. The concentration giving 50% of the maximal effect (EC50) was calculated using GraphPad software version 4.0 (Prism GraphPad, Inc.; San Diego, CA, USA). A p < 0.05 was considered as significant.
3. Results and Discussion
3.1. Nanoparticles Characterization
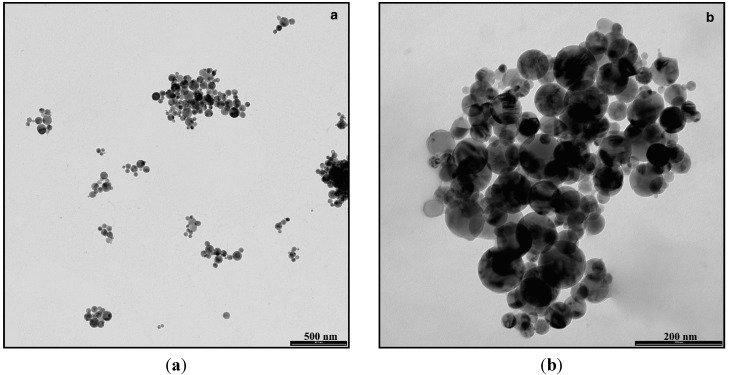
The characterization performed on TiO2NP specimens showed that the NPS have a regular spherical shape and appear as slightly aggregated (Figure 1).
Figure 1.
Representative Transmission Electron Microscopy images of agglomerated TiO2NPs dispersed in synthetic sweat at the beginning of the experiments (Bar: (a) = 500 nm, (b) = 200 nm).
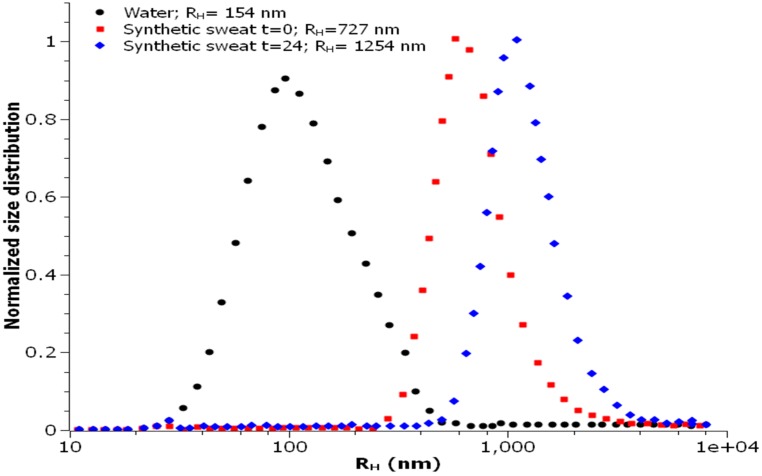
The size distribution is centered on the value of 38 nm. The hydrodynamic radius value (RH) observed in water was centered on 154 nm, while it increased considerably when assessed in synthetic sweat, reaching a value of 727 nm (Figure 2) at time 0 and 1254 nm after 24 h.
Figure 2.
Size distribution of TiO2NPs in water and synthetic sweat suspension, estimated by DLS (Dynamic Light Scattering).
The observed behaviors were in agreement with the measured Z-potential values, reported in Table 1. The measured surface charge values suggest that the NPs dispersed in water are stable thanks to an electrostatic stabilization; for this medium, the small RH value highlighted the presence of small aggregates (RH ≈ 150 nm) constituted by few NPs.
Table 1.
Comparison of Z-potential values in water and in synthetic sweat (mean ± SD).
| Medium Specimen | Water | Synthetic Sweat t = 0 | Synthetic Sweat t = 24 h |
|---|---|---|---|
| TiO2 | −31.7 ± 1.02 mV | −36.8 ± 3.8 mV | −19.0 ± 4.1 mV |
When the nanoparticles were dispersed in synthetic sweat, on the contrary, they immediately started to agglomerate in bigger clusters (RH ≈ 730 nm), as demonstrated by DLS measurements, even if it was not detected by any immediate change in the surface charge.
A remarkable change in the surface charge, due to the absorption of ionic species on the NPs surface, was, however, observed after 24 h. In particular, the significant reduction of the Z-potential was effective in hindering the electrostatic stabilization, thus leading to a strong increase in the mean hydrodynamic radius as detected by DLS measurements (RH ≈ 1260 nm).
3.2. Franz Diffusion Cells Experiments
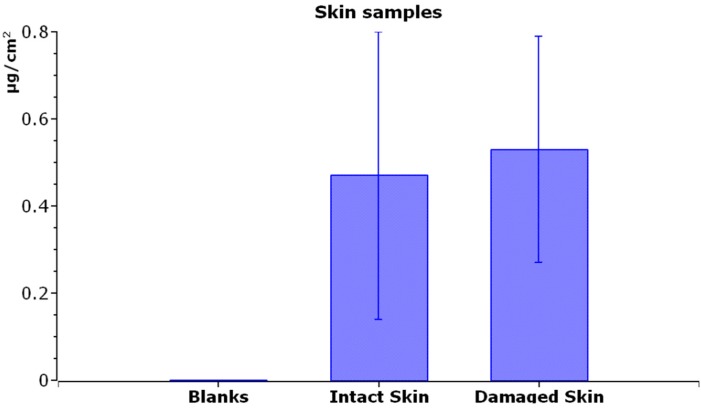
After 24 h of exposure, the average concentration of Ti in the receiving solution was below the level of detection (LOD) of 5 μg/L for both intact and damaged skin.
As shown in Figure 3, the average amount of Ti in intact skin, after 24 h of exposure, was 0.47 ± 0.33 μg/cm2 in the epidermal layer, while the dermal layer concentration was below LOD.
Figure 3.
Titanium content (µg/cm2) inside the skin (epidermis + derma) of blank cells (exposed to physiological solution), intact skin, and damaged skin (exposed to TiO2NPs). Mean and standard deviation of six cells each.
Damaged skin, evaluated as a whole, has shown a similar concentration (0.53 ± 0.26 μg/cm2) to the Ti content of intact skin (Figure 3).
3.3. Effect of TiO2NPs on Cell Viability
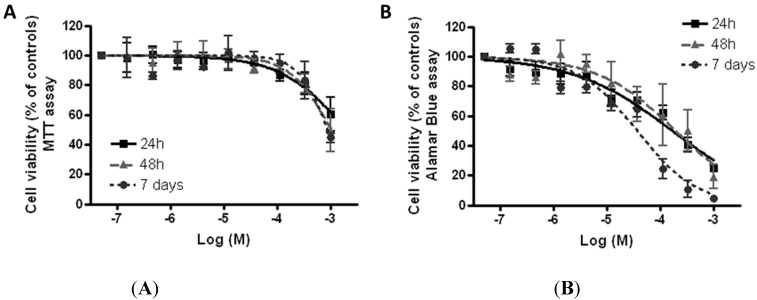
The cytotoxic effect induced by TiO2NPs on HaCaT skin keratinocytes was evaluated using the MTT reduction assay and the AlamarBlue® assay. Figure 4A shows the concentration-response curves obtained after 24, 48 h, and seven days of exposure to TiO2NPs (1.5 × 10−7–1.0 × 10−3 M equal to 0.007–50 μg/cm2) obtained by the MTT assay. TiO2NPs induced a very low cytotoxic effect that was significant (p < 0.05) for concentrations higher than 1.1 × 10−4 M for all the exposure times considered. Intriguingly, cytotoxicity was independent of the length of exposure, since the effects observed after 24, 48 h, or seven days were almost overlapping. After seven of days of exposure, TiO2NPs reduced cell viability with an EC50 equal to 8.8 × 10−4 M (95% confidence limits, CL = 6.2–12.4 × 10−4 M) corresponding to 44 μg/cm2 (95% confidence limits, CL 31–62 μg/cm2).
Figure 4.
Cytotoxicity of TiO2NPs. Cell viability was measured by MTT assay (A) and AlamarBlue® assay (B) after 24 h, 48 h, and seven days of exposure to TiO2NPs (1.5 × 10−7–1.0 × 10−3 M equal to 0.007–50 μg/cm2) on HaCaT cells. Data are reported as % of untreated controls (equal to 100% cell viability) and are the mean ± SE of four independent experiments performed in triplicate.
Figure 4B shows the effect of TiO2NPs on cell viability evaluated by the AlamarBlue® assay. The cytotoxic effect was slightly higher with respect to that evaluated by the MTT assay. In particular, the TiO2NP-induced cytotoxic effect was significant (p < 0.05) at concentrations higher than 1.2 × 10−5 M for all the exposure times considered. The highest effect was achieved after seven days of exposure, after which TiO2NPs reduced cell viability with an EC50 of 3.8 × 10−5 M (95% CL = 2.6–5.3 × 10−5 M), equal to 1.9 μg/cm2 (95% CL = 1.3–2.7 μg/cm2).
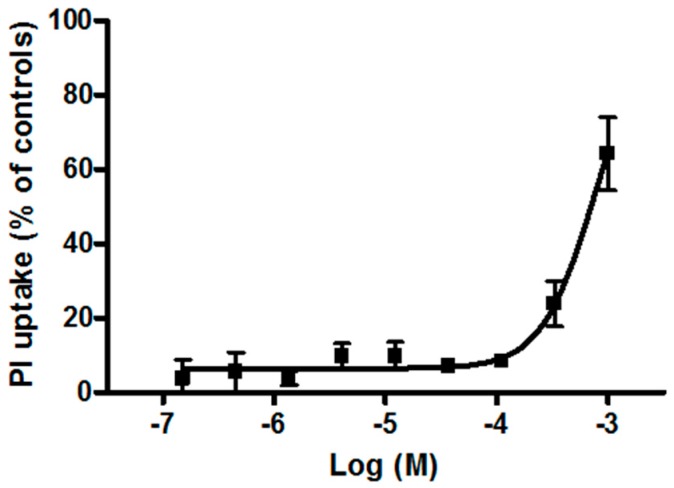
3.4. Effect of TiO2NPs on Membrane Damage
The plasma membrane damage induced by TiO2NPs was evaluated after seven days of NP exposure by propidium iodide (PI) uptake. As shown in Figure 5, TiO2NPs induced a concentration-dependent PI uptake starting from 1.1 × 10−4 M, with an EC50 value of 7.6 × 10−4 M (95% CL = 6.2–9.4 × 10−4 M) equal to 38 μg/cm2 (95% CL = 31–47 μg/cm2).
Figure 5.
PI uptake in HaCaT cells exposed for seven days to TiO2NPs (1.5 × 10−7–1.0 × 10−3 M). Data are reported as mean ± SE of three independent experiments performed in triplicate.
3.5. Discussion
No titanium permeation was demonstrated after 24 h of exposure of the skin to TiO2NPs both in intact and in damaged skin. In the skin, titanium was detectable only in the epidermis. Since the total amount of NPs was similar in both intact and damaged skin, we can assume that lesions do not increase permeation (at least with current limits of detection).
Our study is in accordance with other authors [9,10,11,12,13] who denied the TiO2 capability to permeate the human skin. This is due to the great stability of the TiO2NPs and its negligible ionization in the physiological condition, which leads to an accumulation of NPs on the surface of the skin. Moreover, the big size of the particles and their tendency to form aggregates further reduce the skin absorption capability [8].
To evaluate the toxic potential of TiO2NPs at the skin level, a preliminary study was carried out on human HaCaT keratinocytes, an accepted in vitro model for the screening of the cutaneous toxicity of compounds [43]. On HaCaT cells, TiO2NPs induced a slight cytotoxic effect, reducing cell viability with EC50 values equal to 8.8 × 10−4 M (equal to 44 μg/cm2, MTT assay) and 3.8 × 10−5 M (equal to 41.9 μg/cm2, AlamarBlue® assay) after seven days of exposure. These results are in line with previous studies carried out on HaCaT cells reporting the ability of TiO2NPs to induce oxidative stress and mitochondrial damage [16,19,44]. However, our results suggest a low toxic potential of TiO2NPs since the effects were significant starting from the concentration of 1.1 × 10−4 M (MTT assay).
Intriguingly, no dependency on the exposure time was observed in the MTT test, which, on the contrary, was appreciable in the AlamarBlue® assay. This discrepancy could be tentatively ascribed to the relatively higher sensitivity of the AlamarBlue® assay with respect to the MTT test [45]. After seven days of contact, TiO2NPs also induced a significant increase of PI uptake, suggesting a cytotoxic effect related to membrane damage and compatible with necrosis or late-apoptotic cell death, as recently reported [44]. Notably, this effect occurred with an EC50 value (7.6 × 10−4 M, equal to 38 µg/cm2) very close to that obtained in the MTT assay after long-term exposure (i.e., seven days). One speculative explanation could account for the low cytotoxic potential of TiO2NPs that can be appreciable only at very high concentrations and possibly due to induction of oxidative stress followed by cell death. On the whole, the present results are in line with previous studies reporting low toxicity (see references above), as evaluated by cell viability and morphology after short-term exposure to TiO2NPs [46], and lack of phototoxicity, acute cutaneous irritation, or skin sensitization [47], and the results strengthen the notion of the low risk associated to these NPs.
Our study demonstrated that TiO2NPs cannot permeate intact and damaged skin and can exert a low cytotoxicity effect only at a high dose and long exposure. Nevertheless, our study has some limitations. The first limitation is the in vitro design of our study that can verify only passive diffusion through the skin, while active penetration could happen in the in vivo condition. The second is the short-term run of experiments (24 h) while in real conditions workers and consumers are exposed to TiO2NP-containing products for months and years. The third limitation is the use of HaCaT cells instead of normal human epidermal keratinocytes. We chose these cells because they are easy to culture and because our results can be compared with many similar experiments done on testing nanoparticles on these cells. Nevertheless, they are karyotypically/genetically unstable and additional experiments must be done using human epidermal keratinocytes.
Further studies for the safety evaluation of TiO2NPs in sunscreens are needed, simulating real-world exposure conditions (sunburned skin and UV exposure) on users to verify if a long-term exposure can cause local or systemic effects [48].
4. Conclusions
We did not find permeation of TiO2NPs in either intact or damaged skin. We located NPs in the epidermal layer but not in the dermal layer, and the skin concentration was similar in both tests: skin lesions do not appear to alter the permeation of these NPs.
These results can be explained by the great stability and low ionizing capacity of these particles and are in accordance with several studies in the literature. On the whole, the absence of TiO2NP permeation both in intact and in damaged skin, as well as the low cytotoxicity observed on human HaCaT keratinocytes, suggested a low toxic potential of these nano-compounds at the skin level. Moreover, further studies for the safety evaluation of TiO2NPs in sunscreens are needed, simulating real-world scenarios on sunburned skin and with UV exposure in long-term chronic exposure conditions.
Acknowledgments
This study was supported by the Italian Ministry of Health Ricerca Finalizzata 2009 Grant: Integrated approach to evaluating the biological effects on lung, cardiovascular system, and skin of occupational exposure to nanomaterials (NanO I-LuCaS). RF-2009-1472550.
Author Contributions
Matteo Crosera and Andrea Prodi conducted experiments, did data evaluation, and wrote the paper. Marcella Mauro participated in the experiments and data evaluation. Marco Pelin, Chiara Florio, and Francesca Bellomo did experiments with HacaT cells. Gianpiero Adami, Piero Apostoli, and Giuseppe De Palma performed chemical analysis. Marco Campanini performed nanoparticle characterization. Francesca Larese Filon designed the study and corrected the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Shi H., Magaye R., Castranova V., Zhao J. Titanium dioxide nanoparticles: A review of current toxicological data. Part. Fibre Toxicol. 2013;10:15–20. doi: 10.1186/1743-8977-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shukla R., Sharma V., Pandey A., Singh S., Sultana S., Dhawan A. ROS-mediated genotoxicity induced by titanium dioxide nanoparticles in human epidermal cells. Toxicol. In Vitro. 2001;25:231–241. doi: 10.1016/j.tiv.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Kaida T., Kobayashi K., Adachi M., Suzuki F. Optical characteristics of titanium oxide interference film and the film laminated with oxides and their application for cosmetics. J. Cosmet. Sci. 2004;55:219–220. [PubMed] [Google Scholar]
- 4.Wolf R., Matz H., Orion E., Lipozencic J. Sunscreens—The ultimate cosmetic. Acta Dermatovenerol. Croat. 2003;11:158–162. [PubMed] [Google Scholar]
- 5.Wiesenthal A., Hunter L., Wang S., Wickliffe J., Wilkerson M. Nanoparticles: Small and mighty. Int. J. Dermatol. 2011;50:247–254. doi: 10.1111/j.1365-4632.2010.04815.x. [DOI] [PubMed] [Google Scholar]
- 6.Robertson T.A., Sanchez W., Roberts M. Are commercially available nanoparticles safe when applied to the skin? J. Biomed. Nanotechnol. 2010;6:452–468. doi: 10.1166/jbn.2010.1145. [DOI] [PubMed] [Google Scholar]
- 7.Koivisto A.J., Lyyränen J., Auvinen A., Vanhala E., Hämeri K., Tuomi T., Jokiniemi J. Industrial worker exposure to airborne particles during the packing of pigment and nanoscale titanium dioxide. Inhal. Toxicol. 2012;24:839–849. doi: 10.3109/08958378.2012.724474. [DOI] [PubMed] [Google Scholar]
- 8.Larese Filon F., Mauro M., Adami G., Bovenzi M., Crosera M. Nanoparticles skin absorption: New aspects for a safety profile evaluation. Regul. Toxicol. Pharmacol. 2015;13:310–322. doi: 10.1016/j.yrtph.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Dussert A.S., Gooris E., Hemmerle J. Characterization of the mineral content of a physical sunscreen emulsion and its distribution onto human stratum corneum. Int. J. Cosmet. Sci. 1997;19:119–129. doi: 10.1111/j.1467-2494.1997.tb00175.x. [DOI] [PubMed] [Google Scholar]
- 10.Durand L., Habran N., Henschel V., Amighi K. In vitro evaluation of the cutaneous penetration of sprayable sunscreen emulsions with high concentrations of UV filters. Int. J. Cosmet. Sci. 2009;31:279–292. doi: 10.1111/j.1468-2494.2009.00498.x. [DOI] [PubMed] [Google Scholar]
- 11.Pflücker F., Hohenberg H., Hölzle E., Will T., Pfeiffer S., Wepf R., Diembeck W., Wenck H., Gers-Barlag H. The outermost stratum corneum layer is an effective barrier against dermal uptake of topically applied micronized titanium dioxide. Int. J. Cosmet. Sci. 1999;21:399–411. doi: 10.1046/j.1467-2494.1999.211924.x. [DOI] [PubMed] [Google Scholar]
- 12.Peira E., Turci F., Corazzari I., Chirio D., Battaglia L., Fubini B., Gallarate M. The influence of surface charge and photo-reactivity on skin-permeation enhancer property of nano-TiO2 in ex vivo pig skin model under indoor light. Int. J. Pharm. 2014;5:90–99. doi: 10.1016/j.ijpharm.2014.03.052. [DOI] [PubMed] [Google Scholar]
- 13.Adachi K., Yamada N., Yamamoto K., Yoshida Y., Yamamoto O. In vivo effect of industrial titanium dioxide nanoparticles experimentally exposed to hairless rat skin. Nanotoxicology. 2010;4:296–306. doi: 10.3109/17435391003793095. [DOI] [PubMed] [Google Scholar]
- 14.Monteiro-Riviere N.A., Wiench K., Landsiedel R., Schulte S., Inman A.O., Riviere J.E. Safety evaluation of sunscreen formulations containing titanium dioxide and zincoxide nanoparticles in UVB sunburned skin: An in vitro and in vivo study. Toxicol. Sci. 2011;123:264–280. doi: 10.1093/toxsci/kfr148. [DOI] [PubMed] [Google Scholar]
- 15.Kiss B., Bíró T., Czifra G., Tóth B.I., Kertész Z., Szikszai Z., Kiss A.Z., Juhász I., Zouboulis C.C., Hunyadi J. Investigation of micronized titanium dioxide penetration in human skin xenografts and its effect on cellular functions of human skin-derived cells. Exp. Dermatol. 2008;17:659–667. doi: 10.1111/j.1600-0625.2007.00683.x. [DOI] [PubMed] [Google Scholar]
- 16.Jaeger A., Weiss D.G., Jonas L., Kriehuber R. Oxidative stress-induced cytotoxic and genotoxic effects of nano-sized titanium dioxide particles in human HaCaT keratinocytes. Toxicology. 2012;296:27–36. doi: 10.1016/j.tox.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Chan J., Ying T., Guang Y.F., Lin L.X., Kai T., Fang Z.Y., Ting Y.X., Xing L.F., Ji Y.Y. In vitro toxicity evaluation of 25-nm anatase TiO2 nanoparticles in immortalized keratinocyte cells. Biol. Trace Elem. Res. 2011;144:183–196. doi: 10.1007/s12011-011-9064-3. [DOI] [PubMed] [Google Scholar]
- 18.Simon M., Barberet P., Delville M.H., Moretto P., Seznec H. Titanium dioxide nanoparticles induced intracellular calcium homeostasis modification in primary human keratinocytes. Towards an in vitro explanation of titanium dioxide nanoparticles toxicity. Nanotoxicology. 2011;5:125–139. doi: 10.3109/17435390.2010.502979. [DOI] [PubMed] [Google Scholar]
- 19.Xue C., Wu J., Lan F., Liu W., Yang X., Zeng F., Xu H. Nano titanium dioxide induces the generation of ROS and potential damage in HaCaT cells under UVA irradiation. J. Nanosci. Nanotechnol. 2010;10:8500–8507. doi: 10.1166/jnn.2010.2682. [DOI] [PubMed] [Google Scholar]
- 20.Adachi K., Yamada N., Yoshida Y., Yamamoto O. Subchronic exposure of titanium dioxide nanoparticles to hairless rat skin. Exp. Dermatol. 2013;22:278–283. doi: 10.1111/exd.12121. [DOI] [PubMed] [Google Scholar]
- 21.Wu J., Liu W., Xue C., Zhou S., Lan F., Bi L., Xu H., Yang X., Zeng F. Toxicity and penetration of TiO2 nanoparticles in hairless mice and porcine skin after subchronic dermal exposure. Toxicol. Lett. 2009;191:1–8. doi: 10.1016/j.toxlet.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 22.Jonaitis T.S., Card J.W., Magnuson B. Concerns regarding nano-sized titanium dioxide dermal penetration and toxicity study. Toxicol. Lett. 2010;192:268–269. doi: 10.1016/j.toxlet.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Sadrieh N., Wokovich A.M., Gopee N.V., Zheng J., Haines D., Parmiter D., Siitonen P.H., Cozart C.R., Patri A.K., McNeil S.E., et al. Lack of significant dermal penetration of titanium dioxide from sunscreen formulations containing nano- and submicron-size TiO2 particles. Toxicol. Sci. 2010;115:156–166. doi: 10.1093/toxsci/kfq041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sagawa Y., Futakuchi M., Xu J., Fukamachi K., Sakai Y., Ikarashi Y., Nishimura T., Suzui M., Tsuda H., Morita A. Lack of promoting effect of titanium dioxide particles on chemically-induced skin carcinogenesis in rats and mice. J. Toxicol. Sci. 2012;37:317–327. doi: 10.2131/jts.37.317. [DOI] [PubMed] [Google Scholar]
- 25.Xu J., Sagawa Y., Futakuchi M., Fukamachi K., Alexander D.B., Furukawa F., Ikarashi Y., Uchino T., Nishimura T., Morita A., et al. Lack of promoting effect of titanium dioxide particles on ultraviolet B-initiated skin carcinogenesis in rats. Food Chem. Toxicol. 2011;49:1298–1302. doi: 10.1016/j.fct.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Tan M., Commens C.A., Burnett L., Snitch P.J. A pilot study on the percutaneous absoprtion of microfine titanium dioxide from sunscreens. Australas. J. Dermatol. 1996;37:185–187. doi: 10.1111/j.1440-0960.1996.tb01050.x. [DOI] [PubMed] [Google Scholar]
- 27.Bennat C., Müller-Goymann C.C. Skin penetration and stabilization of formulations containing microfine titanium dioxide as physical UV filter. Int. J. Cosmet. Sci. 2000;22:271–283. doi: 10.1046/j.1467-2494.2000.00009.x. [DOI] [PubMed] [Google Scholar]
- 28.Senzui M., Tamura T., Miura K., Ikarashi Y., Watanabe Y., Fujii M. Study on penetration of titanium dioxide (TiO2) nanoparticles into intact and damaged skin in vitro. J. Toxicol. Sci. 2010;35:107–113. doi: 10.2131/jts.35.107. [DOI] [PubMed] [Google Scholar]
- 29.Bauer A., Schmitt J., Bennett C., Coenraads P.J., Elsner P., English J., Williams H.C. Interventions for preventing occupational irritant hand dermatitis. Cochrane Database Syst. Rev. 2010 doi: 10.1002/14651858.CD004414.pub2. [DOI] [PubMed] [Google Scholar]
- 30.Williams F.M. EDETOX. Evaluations and Predictions of Dermal Absorption of Toxic Chemicals. Int. Arch. Occup. Environ. Health. 2004;77:150–151. doi: 10.1007/s00420-003-0484-z. [DOI] [PubMed] [Google Scholar]
- 31.Larese F.F., D’Agostin F., Crosera M., Adami G., Renzi N., Bovenzi M., Maina G. Human skin penetration of silver nanoparticles through intact and damaged skin. Toxicology. 2009;255:33–37. doi: 10.1016/j.tox.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 32.Filon F.L., Crosera M., Adami G., Bovenzi M., Rossi F., Maina G. Human skin penetration of gold nanoparticles through intact and damaged skin. Nanotoxicology. 2011;5:493–501. doi: 10.3109/17435390.2010.551428. [DOI] [PubMed] [Google Scholar]
- 33.Larese Filon F., Crosera M., Timeus E., Adami G., Bovenzi M., Ponti J., Maina G. Human skin penetration of cobalt nanoparticles through intact and damaged skin. Toxicol. In Vitro. 2013;27:121–127. doi: 10.1016/j.tiv.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 34.Alinovi R., Goldoni M., Pinelli S., Campanini M., Aliatis I., Bersani D., Lottici P.P., Iavicoli S., Petyx M., Mozzoni P., et al. Oxidative and pro-inflammatory effects of cobalt and titanium oxide nanoparticles on aortic and venous endothelial cells. Toxicol. In Vitro. 2015;29:426–437. doi: 10.1016/j.tiv.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 35.Bronaugh R., Stewart R. Methods for in vitro percutaneous absorption studies V: Permeation trough damaged skin. J. Pharm. Sci. 1985;10:1062–1066. doi: 10.1002/jps.2600741008. [DOI] [PubMed] [Google Scholar]
- 36.Fasano W.J., Manning L.A., Green J.W. Rapid assessment of rat and human epidermal membranes for in vitro dermal regulatory testing: Correlation of electrical resistance with tritiated water permeability. Toxicol. In Vitro. 2002;16:731–740. doi: 10.1016/S0887-2333(02)00084-X. [DOI] [PubMed] [Google Scholar]
- 37.Davies D.J., Ward R.J., Heylings J.R. Multi-species assessment of electrical resistance as a skin integrity marker for in vivo percutaneous absorption studies. Toxicol. In Vitro. 2004;18:351–358. doi: 10.1016/j.tiv.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 38.Franz T.J. Percutaneous absorption on the relevance of in vitro data. J. Investig. Dermatol. 1975;64:190–195. doi: 10.1111/1523-1747.ep12533356. [DOI] [PubMed] [Google Scholar]
- 39.Boukamp P., Petrussevska R., Breitkreutz D., Hornung J., Markham A., Fusenig N. Normal keratinization in a spontaneously immortalized aneuploid human keratinocyte cell line. J. Cell Biol. 1988;106:761–771. doi: 10.1083/jcb.106.3.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mosmann T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods. 1983;65:55–63. doi: 10.1016/0022-1759(83)90303-4. [DOI] [PubMed] [Google Scholar]
- 41.Pelin M., Sosa S., Della Loggia R., Poli M., Tubaro A., Decorti G., Florio C. The cytotoxic effect of palytoxin on Caco-2 cells hinders their use for in vitro absorption studies. Food Chem. Toxicol. 2012;50:206–211. doi: 10.1016/j.fct.2011.10.032. [DOI] [PubMed] [Google Scholar]
- 42.Pelin M., Sosa S., Pacor S., Tubaro A., Florio C. The marine toxin palytoxin induces necrotic death in HaCaT cells through a rapid mitochondrial damage. Toxicol. Lett. 2014;229:440–450. doi: 10.1016/j.toxlet.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 43.Gibbs S. In vitro irritation models and immune reactions. Skin Pharmacol. Physiol. 2009;22:103–113. doi: 10.1159/000178869. [DOI] [PubMed] [Google Scholar]
- 44.Gao X., Wang Y., Peng S., Yue B., Fan C., Chen W., Li X. Comparative toxicities of bismuth oxybromide and titanium dioxide exposure on human skin keratinocyte cells. Chemosphere. 2015;135:83–93. doi: 10.1016/j.chemosphere.2015.03.075. [DOI] [PubMed] [Google Scholar]
- 45.Hamid R., Rotshteyn Y., Rabadi L., Parikh R., Bullock P. Comparison of alamar blue and MTT assays for high through-put screening. Toxicol. In Vitro. 2004;18:703–710. doi: 10.1016/j.tiv.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 46.Kocbek P., Teskac K., Kreft M.E., Kristl J. Toxicological aspects of long-term treatment of keratinocytes with ZnO and TiO2 nanoparticles. Small. 2010;6:1908–1917. doi: 10.1002/smll.201000032. [DOI] [PubMed] [Google Scholar]
- 47.Park Y.H., Jeong S.H., Yi S.M., Choi B.H., Kim Y.R., Kim I.K., Kim M.K., Son S.W. Analysis for the potential of polystyrene and TiO2 nanoparticles to induce skin irritation, phototoxicity, and sensitization. Toxicol. In Vitro. 2011;25:1863–1869. doi: 10.1016/j.tiv.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 48.Newman M.D., Stotland M., Ellis J.I. The safety of nanosized particles in titanium dioxide- and zinc oxide-based sunscreens. J. Am. Acad. Dermatol. 2009;61:685–692. doi: 10.1016/j.jaad.2009.02.051. [DOI] [PubMed] [Google Scholar]