Abstract
Background
The association between influenza vaccination and implantable cardiac defibrillator (ICD) therapies during influenza season is not known and is described in this study. Understanding this association is important since reduction in ICD therapies during influenza season via use of influenza vaccination would benefit patients physically and psychologically.
Methods
Patients presenting to the Sunnybrook Health Sciences Center ICD clinic between September 1st, 2011 and November 31st, 2011 were asked to complete a survey evaluating their use of the influenza vaccine. The number of patients with any ICD therapy and the total number of ICD therapies in the six months before and the three months during the 2010–2011 influenza season were determined. Poisson regression analysis was employed to assess differences in the average number of ICD therapies received during the influenza season based on vaccine status (vaccinated vs. unvaccinated). The analysis was repeated after limiting the cohort to patients with a left ventricular ejection fraction ≤35%.
Results
A total of 229 patients completed the survey, 78% of whom received the influenza vaccine. Four patients had more than one ICD shock during the study period. Electrical storm was rare (n=2). A trend toward more ICD therapies (unadjusted incident rate ratio (IRR)=3.2; P=0.07) and appropriate ICD shocks (unadjusted IRR=9.0; P=0.17) was noted for unvaccinated compared to vaccinated patients. This association persisted when analysis was limited to patients with a left ventricular ejection fraction ≤35% (all ICD therapies: unadjusted IRR=5.8; P=0.045; adjusted IRR=2.6; P=0.33). No patient who received the influenza vaccine, and had a reduced ejection fraction, received an approprite ICD shock during influenza season (unadjusted P<0.002).
Conclusion
A trend toward more ICD therapies during influenza season was observed in patients who did not receive the influenza vaccine compared to those who did. The association was stronger in patients who received appropriate ICD shocks and in patients with left ventricular systolic dysfunction. Further work to confirm these findings is recommended.
Keywords: Implantable cardiac defibrillators, Ventricular tachycardia, Supraventricular tachycardia, Preventive vaccination, Influenza
1. Introduction
The association between influenza-like illness and adverse cardiac events has been reported in several observational studies [1,2], prompting the American Heart Association and Canadian Cardiovascular Society to recommend annual influenza vaccination for patients with cardiac disease [3,4]. However, there has been no study on the association between influenza vaccination and cardiac arrhythmia, an underappreciated contributor of cardiac morbidity and mortality. In this exploratory retrospective study of 229 patients, we assessed the association between influenza vaccination and implantable cardioverter defibrillator (ICD) therapies in the six months before and the three months during the 2010–2011 influenza season.
2. Materials and methods
All patients with an ICD presenting for routine follow up at the Sunnybrook Health Sciences Center ICD clinic, Toronto, Canada between September 1st and November 30th, 2011 were asked to participate in a survey assessing their use of the influenza vaccination in the previous influenza season.
Patient demographics, co-morbidities, and medication use were ascertained from responses to survey questions and a review of each patient׳s hospital chart. Each patient׳s ICD chart was reviewed to confirm the incidence of any ICD therapy (appropriate and inappropriate shock or antitachycardia pacing) for an arrhythmic event between June 1st, 2010 and March 1st, 2011. Inappropriate ICD therapies secondary to lead or device malfunctions were excluded, as they do not reflect arrhythmic events. The type of each ICD therapy was adjudicated by two individuals (R.K. and S.M.S.). December 1st, 2010–March 1st, 2011 was considered influenza season, consistent with the peak of influenza season in Canada [5], whereas June 1st, 2010–November 30th, 2010 was deemed “pre”-influenza season. Of note, a good match between the influenza vaccine and globally circulating influenza strains was noted during this influenza season [6].
Patients were divided into two groups: those that received the influenza vaccine and those that did not. Patient characteristics for each group were reported as proportions, mean±standard deviation or median with range where appropriate. Student׳s t-, Fisher׳s exact, and Wilcoxon Rank-Sum tests were used to assess differences between the two groups.
The number of vaccinated or unvaccinated individuals receiving any ICD therapy (defined as appropriate shock or antitachycardia pacing for ventricular arrhythmias or inappropriate shock or antitachycardia pacing for supraventricular arrhythmias) or any appropriate ICD shock during the “pre”-influenza season (defined as the two 3 month periods preceding influenza season) and during the influenza season (3 month period) was determined. Any ICD therapy was considered to be reflective of the total arrhythmia burden, and appropriate ICD shock was considered to be reflective of the malignant ventricular arrhythmia burden.
Possible endpoints that may differ between vaccinated vs. unvaccinated individuals were considered to be a reduction in the number of vaccinated individuals receiving any ICD therapy compared to unvaccinated individuals or a reduction in the total number of arrhythmic events requiring ICD therapies in vaccinated individuals, the latter of which accounts for clustering of arrhythmia during the winter months [7]. A binomial test for proportions was performed to assess differences in the total number of ICD therapies between the groups during “pre”- and influenza season. The “pre”-influenza season was divided into two 3 month periods for comparison with the 3 month influenza period. Poisson regression analysis [8] was employed to assess differences between groups in the number of ICD therapies received during influenza season. The analysis was repeated for appropriate ICD shocks during influenza season. Results were reported as an incident rate ratio (IRR) comparing the incidence of ICD therapies in unvaccinated vs. vaccinated patients.
Since the patient cohort in this study was small, thereby impacting the validity of multivariate analysis, our primary evaluation of ICD therapy incidence was unadjusted for differences between the two study groups with regard to factors known to impact cardiac arrhythmia, such as patient age, co-morbidity, or history of ventricular arrhythmias. Secondary analyses adjusted for these factors. Finally, when comparing the number of ICD therapies during influenza season between patients who were or were not vaccinated, an adjustment was made for the number of ICD therapies received in the “pre”-influenza period. We repeated the above analysis after restricting the cohort to those with a left ventricular ejection fraction ≤35% to understand the impact of influenza vaccination on all ICD therapies and appropriate ICD shocks in patients with left ventricular systolic dysfunction.
For all analyses, a P-value<0.05 was considered statistically significant. Statistical analyses were carried out using SAS version 9.3 (SAS Institute, Cary, NC). Ethical approval for this study was obtained from the Sunnybrook Health Sciences Center Research Ethics Board (Date of approval August 26th, 2011; Approval number: 258-2011).
3. Results
A total of 229 patients completed the survey, representing 44% of all ICD patients presenting to the Sunnybrook Health Sciences Center ICD clinic during the study period, of which 78% reported receiving the influenza vaccine. Table 1 summarizes the characteristics of patients who did and did not receive the influenza vaccine. Unvaccinated individuals were younger, less likely to have had a family physician for at least 5 years, and more likely to have received a primary prevention ICD. No differences in co-morbidities, left ventricular systolic ejection fraction, use of anti-arrhythmic drugs, or median household income, a marker of socio-economic status [9], were noted between the two groups.
Table 1.
Patient characteristics.
|
Influenza vaccination status |
P-value | ||
|---|---|---|---|
| Vaccinated (N=180) | Not vaccinated (N=49) | ||
| Age (SD) | 71 (10) | 65 (11) | <0.005 |
| Male % | 87 | 79 | 0.3 |
| Median neighborhood income CDN$ (interquartile range) | 27,086 (22,982–32,004) | 26,305 (22,012–32,606) | 0.9 |
| Maintain family physician>5years % | 85 | 71 | 0.03 |
| Coronary artery disease % | 67 | 67 | 1.0 |
| Renal disease % | 7 | 12 | 0.2 |
| Diabetes % | 33 | 31 | 0.7 |
| Stroke % | 16 | 6 | 0.1 |
| Ejection fraction % (SD) | 29 (10) | 29 (10) | 0.8 |
| Primary prevention defibrillator use % | 76 | 86 | 0.04 |
| Use of anti-arrhythmic drugs % | 73 | 72 | 0.6 |
SD=standard deviation; CDN$=Canadian dollar.
The retrospective nature of the study allowed for complete information on ICD therapies to be obtained for all patients during the study period. Overall, 17% of the 229 patients in our cohort received any ICD therapy during the 9-month study period. Two patients had electrical storm during the study period – one patient who received the influenza vaccine had electrical storm in the “pre”-influenza season (4 discrete ventricular tachycardia episodes in 24 h requiring antitachycardia pacing) and one unvaccinated patient had electrical storm during influenza season (4 discrete ventricular tachycardia episodes requiring 4 ICD shocks). Multiple ICD therapies (≥2 appropriate or inappropriate ICD shocks or antitachycardia pacing) were noted in 19 patients, including 4 unvaccinated patients. Multiple ICD shocks (≥2 appropriate or inappropriate ICD shocks) were observed in 4 patients, including 3 unvaccinated patients.
There was no significant difference in the absolute number of individuals receiving any ICD therapy or appropriate ICD shocks when comparing the 3 segments of time (Fig. 1). A non-significant trend toward more appropriate ICD shocks was observed in unvaccinated individuals (Fig. 1, grey bar graph).
Fig. 1.
Percentage of vaccinated and unvaccinated patients receiving implantable cardioverter defibrillator (ICD) therapies (any and appropriate ICD shocks) in the “pre”- and influenza seasons. Flu+=vaccined against influenza; Flu−=unvaccinated; All ICD therapies=appropriate and inappropriate ICD shocks and antitachycardia pacing. The “pre”-influenza season was divided into two three month periods for comparison with the three month influenza season. There were no significant P-values for any comparisons.
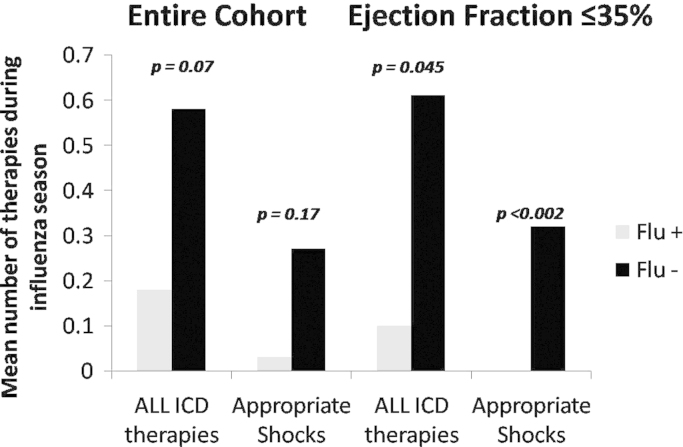
The mean number of all ICD therapies and appropriate ICD shocks during influenza season is shown in Fig. 2. A trend toward a greater average number of ICD therapies received during influenza season (inappropriate and appropriate ICD shocks and antitachycardia pacing) was observed in unvaccinated patients compared to vaccinated patients (unadjusted IRR=3.2; P=0.07). Similar findings were noted when analyzing only appropriate ICD shocks (unadjusted IRR=9.0; P=0.17). The IRRs were not significant after adjusting for age, primary versus secondary prevention indication, use of anti-arrhythmic drugs and the number of “pre”-influenza season ICD therapies (All ICD therapies: adjusted IRR=1.2; P=0.81; Appropriate ICD shocks: adjusted IRR=0.31; P=0.64).
Fig. 2.
Mean number of implantable cardioverter defibrillator (ICD) therapies (any and appropriate shocks) per vaccinated or unvaccinated patient during the influenza season. Flu+=vaccinated against influenza; Flu−=unvaccinated; All ICD therapies=appropriate and inappropriate ICD shocks and antitachycardia pacing. Unadjusted P-values reported.
When the analysis was limited to subjects with a left ventricular ejection fraction ≤35% (Fig. 2), unvaccinated individuals received a significantly greater number of any ICD therapies during influenza season than vaccinated individuals (unadjusted IRR=5.8; P=0.045). However, significance was not reached after adjusting for factors known to impact cardiac arrhythmia (adjusted IRR=2.6; P=0.31). Unvaccinated patients in this specific cohort received a significantly greater number of appropriate ICD shocks (P<0.002) since no vaccinated patients with a left ventricular ejection fraction <35% received an appropriate ICD shock during the influenza season.
4. Discussion
An association between influenza vaccination and ICD therapies was assessed in this single center, retrospective study. To our knowledge this is the first study to assess the impact of influenza vaccination on ICD therapies. The data indicate a trend toward a higher incidence of ICD therapies during influenza season in unvaccinated compared to vaccinated patients, with greater trends in patients receiving appropriate ICD shocks and in patients with left ventricular systolic dysfunction. These findings are suggestive of a beneficial effect of influenza vaccination on the burden of cardiac arrhythmia during influenza season.
An increased incidence of ventricular arrhythmias in winter and spring has been described, although the mechanism is unknown [7,10]. Non-arrhythmic cardiac events also increase in winter, potentially related to acute influenza infection. Possible mechanisms for increased cardiac events with influenza infection include an increase in circulating clotting factors and inflammatory cytokines, which may enhance thrombosis, induce endothelial dysfunction, or inhibit vasodilation [10], all of which may result in ischemia and heart failure, leading to arrhythmia. Prevention of influenza infection may attenuate this cascade, thereby attenuating arrhythmia risk in winter.
The presence of an ICD allowed us to determine the precise number of arrhythmic events. Our work suggests a trend toward a higher cardiac arrhythmia burden, including malignant cardiac arrhythmia requiring appropriate ICD therapies, during influenza season in unvaccinated patients. Our findings suggest a potential benefit of influenza vaccination on cardiac arrhythmia burden. The lack of statistical significance in most of our findings likely reflects the lack of power in our small, exploratory study. However, the trend toward a benefit of influenza vaccination for decreasing the total number of ICD therapies and the number of appropriate ICD shocks adds credibility to our hypothesis that influenza vaccination reduces cardiac arrhythmia. Furthermore, the larger trend observed in patients with left ventricular systolic dysfunction and, in particular, the larger trend observed when limiting the analysis to appropriate ICD shocks, adds additional support to our hypothesis.
The observed increase in the number of ICD therapies during influenza season is consistent with prior reports describing increased cardiac arrhythmia burden in winter [9], possibly requiring a larger number of ICD therapies. Influenza vaccination may attenuate this. The low incidence of electrical storms observed in our study is likely a reflection of the small sample size and milder influenza season in 2011. Given the larger trend toward a benefit of influenza vaccination when analyzing appropriate ICD therapies, we speculate that vaccination may reduce the burden of electrical storm in ICD patients.
Our findings support the current Class I recommendations by the American Heart Association and the Canadian Cardiovascular Society for influenza vaccination in patients with heart failure. There is currently little direct evidence supporting the benefit of influenza vaccination in heart failure patients and the recommendation to vaccinate these patients is based on consensus opinion or small studies [3,4]. Our exploratory study adds to existing literature supporting the potential cardiac benefits of influenza vaccination in patients with stable cardiovascular disease. We advocate for larger scale studies to better appreciate the magnitude of cardiac benefit associated with influenza vaccination.
Our findings, particularly if confirmed by other groups, should be communicated to ICD patients to ensure their universal influenza vaccination. Despite the current recommendations for patients with heart failure to be vaccinated against influenza, over 20% of patients in our cohort did not receive the intervention. This less than optimal vaccination rate in cardiac patients has also been demonstrated by others [11]. The potential benefits of a reduction in cardiac arrhythmia suggested by our work, proven non-cardiac benefits of influenza vaccination in adult patients [12], and current Class I recommendations by various Societies should prompt consideration of the influenza vaccination rate as a performance measure in cardiac electrophysiology.
This study has limitations. First, the sample size was small and the event rate was low, reducing the power to detect statistically significant differences between the two groups. Second, we were unable to assess differences between those who completed the survey and those who did not; unmeasured differences between survey responders and non-responders may have introduced bias and compromised the generalizability of our findings. Third, vaccination status was determined by survey. While this approach may be subject to “recall” bias, it is considered the current gold standard for ascertaining vaccination status [13]. Fourth, clinical details such as hospitalization for a respiratory illness or serologic evidence of acute influenza infection at the time of receipt of ICD therapies were not available, thereby preventing us from further commenting on the association between ICD therapies and acute influenza infection. Finally, although we adjusted for other predictors of ICD therapies, we cannot exclude a “healthy-user” bias – that is this possibility that inherently healthier patients chose to receive the influenza vaccine [14]. This possibility is well known in retrospective studies evaluating use of the influenza vaccine [15] and is unlikely to be overcome outside of a randomized clinical trial, which is likely unethical given the current Class I recommendations for use of this intervention.
5. Conclusion
In conclusion, the data suggest that influenza vaccination may reduce the incidence of ICD therapies during influenza season, particularly appropriate ICD therapies. The effect is more pronounced in patients with left ventricular systolic dysfunction. We suggest an additional, larger scale study on the benefits of influenza vaccination in this patient population to confirm our findings.
Author contributions
Concept/design: Sheldon M. Singh, MD, Russell J. de Souza, ScD, RD, Ramanan Kumareswaran, MD.
Data analysis/interpretation: Sheldon M. Singh, MD, Russell J. de Souza, ScD, RD, Ramanan Kumareswaran, MD.
Drafting article: Sheldon M. Singh, MD.
Critical revision of article: Sheldon M. Singh, MD, Russell J. de Souza, ScD, RD, Ramanan Kumareswaran, MD.
Approval of article: Sheldon M. Singh, MD, Russell J. de Souza, ScD, RD, Ramanan Kumareswaran, MD.
Statistics: Russell J. de Souza, ScD.
Funding secured by: Not applicable.
Data collection: Sheldon M. Singh, MD, Ramanan Kumareswaran, MD.
Conflict of interest
Drs. Singh and Kumareswaran have no conflicts of interest to disclose. Dr. de Souza is a recipient of a Canadian Institutes of Health Research post-doctoral fellowship and has been a co-investigator on unrestricted, investigator-initiated research grants awarded to his institution from the Calorie Control Council, Canadian Institutes of Health Research, and The Coca-Cola Company. Preliminary results of this study were presented at the 2012 Canadian Cardiovascular Congress.
Acknowledgments
We would like to acknowledge the dedicated defibrillator clinic staff at the Sunnybrook Health Sciences Center.
References
- 1.Collins S.D. Excess Mortality from Causes Other than Influenza and Pneumonia During Influenza Epidemics. Public Health Weekly Reports for November 11, 1932. Public Health Rep. 1932;47:2159–2179. [Google Scholar]
- 2.Madjid M., Miller C.C., Zarubaev V.V. Influenza epidemics and acute respiratory disease activity are associated with a surge in autopsy confirmed coronary heart disease death: results from 8 years of autopsies in 34,892 subjects. Eur Heart J. 2007;28:1205–1210. doi: 10.1093/eurheartj/ehm035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnold J.M., Liu P., Demers C. Canadian cardiovascular society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006;22:23–45. doi: 10.1016/s0828-282x(06)70237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis M.M., Taubert K., Benin A.L. Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. Circulation. 2006;114:1549–1553. doi: 10.1161/CIRCULATIONAHA.106.178242. [DOI] [PubMed] [Google Scholar]
- 5.Public Health Agency of Canada. Canadian communicable disease report: statement on seasonal influenza vaccine for 2011–2012; October 2011. Available from: 〈http://www.phac-aspc.gc.ca/publicat/ccdr-rmtc/11vol37/acs-dcc-5/index-eng.php〉.
- 6.World Health Organization Recommended composition of influenza virus vaccines for use in the 2011–2012 northern hemisphere influenza season. Wkly Epidemiol Rec. 2011;86:86–90. [PubMed] [Google Scholar]
- 7.Suport.sas.com [Internet]. Carey: SAS Institute; c2009-10 [updated April 30th 2010; cited July 1st 2014]. Available from: 〈http://support.sas.com/documentation/cdl/en/statug/63033/HTML/default/viewer.htm#genmod_toc.htm〉.
- 8.Alter D.A., Austin P.C., Naylor C.D. Factoring socioeconomic status into cardiac performance profiling for hospitals: does it matter? Med Care. 2002;40:60–67. doi: 10.1097/00005650-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Stuber T., Eigenmann C., Delacretaz E. Seasonal variations of ventricular arrhythmia clusters in defibrillator recipients. Pacing Clin Electrophysiol. 2006;29:816–820. doi: 10.1111/j.1540-8159.2006.00446.x. [DOI] [PubMed] [Google Scholar]
- 10.Page R.L., Zipes D.P., Powell J.L. Seasonal variation of mortality in Antiarrhythmics Versus Implantable Defibrillators (AVID) study registry. Heart Rhythm. 2004;1:435–440. doi: 10.1016/j.hrthm.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 11.Hebert K., Marzouka G., Arcement L. Prevalence of vaccination rates in systolic heart failure: a prospective study of 549 patients by age, race, ethnicity, and sex in a heart failure disease management program. Congest Heart Fail. 2010;16:278–283. doi: 10.1111/j.1751-7133.2010.00190.x. [DOI] [PubMed] [Google Scholar]
- 12.Kostova D., Reed C., Finelli L. Influenza illness and hospitalizations averted by influenza vaccination in the United States, 2005–2011. PLoS One. 2013;8:e66312. doi: 10.1371/journal.pone.0066312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong K., Campitelli M.A., Stukel T.A. Estimating influenza vaccine effectiveness in community-dwelling elderly patients using the instrumental variable analysis method. Arch Intern Med. 2012;172:484–491. doi: 10.1001/archinternmed.2011.2038. [DOI] [PubMed] [Google Scholar]
- 14.Shrank W.H., Patrick A.R., Brookhart M.A. Healthy user and related biases in observational studies of preventive interventions: a primer for physicians. J Gen Intern Med. 2011;26:546–550. doi: 10.1007/s11606-010-1609-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson L.A., Jackson M.L., Nelson J.C. Evidence of bias in estimates of influenza vaccine effectiveness in seniors. Int J Epidemiol. 2006;35:337–344. doi: 10.1093/ije/dyi274. [DOI] [PubMed] [Google Scholar]