Abstract
Background:
Osteochondritis dissecans (OCD) can progress to loose body formation, with or without subchondral bone attachment to the lesion. The efficacy of internal fixation of chondral loose bodies has not been determined.
Hypothesis:
Operative fixation of cartilaginous loose bodies would result in (1) healed OCD at second-look arthroscopy, (2) restored cartilage appearance on magnetic resonance imaging (MRI), and (3) nearly normal knee function, as determined by patient-reported outcome scores.
Study Design:
Retrospective case series; Level of evidence, 4.
Methods:
Five patients who underwent cartilaginous loose body fixation were identified. Lesions were located on the lateral trochlea (n = 2) and medial femoral condyle (n = 3) (mean size, 2.5 cm2). Loose bodies were reattached with compression screws through mini-arthrotomy or arthroscopy. Patients were nonweightbearing for 12 weeks postoperatively. After 12 weeks, screws were removed arthroscopically, and OCD stability was evaluated. Three patients underwent MRI to determine articular cartilage status. Images were evaluated using the magnetic resonance observation of cartilage repair tissue (MOCART) score. Patients were interviewed and completed the Knee injury and Osteoarthritis Outcome Score (KOOS) questionnaire.
Results:
Four patients had stable lesions at 12 weeks after surgery. One patient had slight motion to one-third of the lesion and stability to the remaining two-thirds. Three patients underwent an MRI. The mean time from surgery to MRI was 3.1 years. Mean MOCART score was 72.0 ± 10.4. One patient required repeat arthroscopy 1 year after initial fixation for debridement and arthroscopic drilling of an incompletely healed area of the lesion. Four patients completed the KOOS questionnaire. The mean time to KOOS completion was 4.6 years. Mean KOOS subscales for knee pain (91.0 ± 8.9), knee symptoms (83.0 ± 7.9), and function in activities of daily living (91.9 ± 10.6) were similar to published age-matched controls; however, scores for sports and recreation function (70.0 ± 17.8) and knee-related quality of life (67.2 ± 12.9) were lower.
Conclusion:
Operative fixation of chondral loose bodies, without macroscopically visible subchondral bone attachment, resulted in lesion stability at second-look arthroscopy. At final follow-up, patients had no substantial pain and normal function in activities of daily life compared with controls; however, knee-related quality of life and sport and recreation function were reduced, and 1 patient required reoperation for an unhealed portion of the lesion.
Keywords: osteochondritis dissecans, OCD, knee, chondral loose body, operative fixation, functional outcome
Osteochondritis dissecans (OCD) is an idiopathic lesion of the subchondral bone that can secondarily compromise the articular cartilage if healing fails to occur.19,43 This condition most commonly affects juveniles and young adults,23 and approximately 75% of cases involve the knee.8 While the exact etiology of OCD is unknown, both clinical3,6 and basic science2,41 studies support trauma as a contributing factor. Other less substantiated etiologic theories include inflammation,40 ossification abnormalities,38 and ischemia.13
Treatment for OCD is dictated by skeletal maturity and stage of the lesion at the time of presentation. The goal of treatment is to preserve the articular cartilage through healing of the OCD fragment.
Guhl16 developed a 4-stage classification system for OCD based on the degree of fragment separation observed during arthroscopic examination. Grade 1 lesions are intact and stable to probing, grade 2 lesions show early signs of separation with intact cartilage, grade 3 lesions are partially detached, and grade 4 lesions are loose bodies with a crater defect.
Histologic analysis of OCD has determined lesions can be either cartilaginous, without attached subchondral bone, or osteochondral.31,44 Most surgeons recommend replacement and stabilization of grade 4 lesions with adequate subchondral bone,6,16,24,25 because treatment of the fragment by excision has generally led to suboptimal results.3,7,17,49 When a grade 4 lesion has inadequate subchondral support, treatment typically consists of extraction of the fragment followed by a marrow-stimulating or resurfacing procedure.5,9,19,45
Reports of replacement and fixation of chondral loose bodies in the literature are rare and lack patient-reported outcome data.22,32 We hypothesized that operative fixation of cartilaginous loose fragments, without visible evidence of bone attached, would result in (1) healed OCD at second-look arthroscopy, (2) restored cartilage appearance on magnetic resonance imaging (MRI), and (3) nearly normal knee function, as determined by patient-reported outcome scores.
Materials and Methods
Identification of Patients
This was a retrospective case series study. Institutional review board approval was obtained. We searched the billing records at our institution to identify all patients who underwent operative fixation of OCD lesions by the senior author between January 1, 1991, and December 31, 2006. Specifically, we searched for Current Procedural Terminology (CPT) codes 29885 (drilling for OCD with bone grafting with or without internal fixation) and 29887 (drilling for intact OCD lesion with internal fixation) and identified 36 patients. A review of medical records led to the exclusion of 19 patients whose lesions had not progressed to a loose body (n = 14) or who had undergone drilling of the lesion without fixation of the loose body (n = 5). The remaining 17 patients had grade 4 defects and underwent fixation of the loose body into the defect. Twelve of these patients underwent fixation of osteochondral loose bodies. The remaining 5 underwent fixation of chondral fragments and represent the current study group. As an extension of the grading system proposed by Guhl,16 we classified chondral loose bodies without attached bone as grade 5 lesions.
Operative Technique and Postoperative Protocol
A diagnostic arthroscopy was performed in each case to localize the OCD lesion and find and assess the loose body. In 4 patients, the anteromedial or anterolateral portal was extended into a mini-arthrotomy to visualize and access the OCD defect; the remaining patient had arthroscopic surgery. In each case, the loose body was extracted from the knee and examined macroscopically. Any remaining fibrous tissue was removed from the undersurface of the fragment. The OCD defect was curetted to bleeding bone and drilled with a Kirschner wire. The loose body was then positioned in the defect to assess its relative size. If the loose body was larger than the defect, it was trimmed to allow congruency with the surrounding articular surface. If the defect was larger than the loose body, cancellous autograft was obtained from the distal femur (n = 1) or proximal tibia (n = 3) and packed into the lesion until the size of the defect matched that of the loose body. The loose body was provisionally secured with Kirschner wires and fixed using 2 or 3 metal cortical screws 1.5 to 2.7 mm (Synthes USA, West Chester, Pennsylvania, USA), depending on the lesion size and shape. Screws were countersunk until the head was recessed just below the articular surface (Figures 1B, 1C, and 2C).
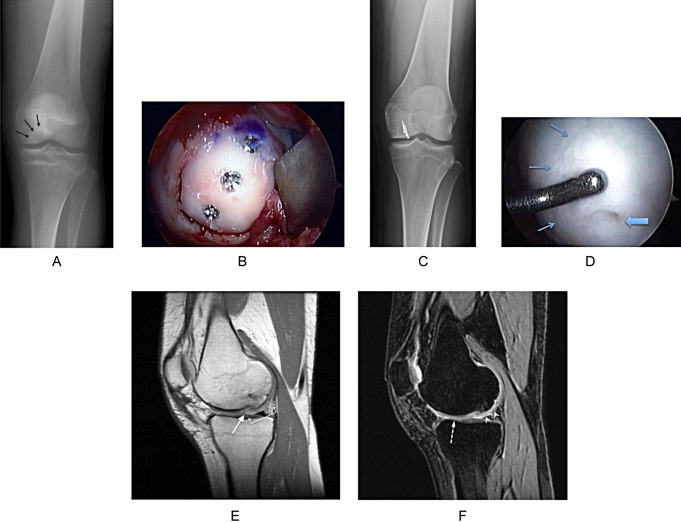
Figure 1.
Patient 4. (A) Preoperative anteroposterior (AP) radiograph showing the osteochondritis dissecans (OCD) lesion of the medial femoral condyle (black arrows). (B) Medial femoral condyle after arthrotomy, bone grafting of the OCD defect, and fixation of the cartilage fragment using 1.5 × 16–mm mini-fragment screws. (C) AP radiograph 1 week after surgery, demonstrating the position of the mini-fragment screws used for fixation of the cartilage fragment. (D) Arthroscopic image 3 months after operative fixation, demonstrating outlining of the cartilage fragment (small blue arrows) with a smooth, stable surface. A residual small defect is seen (large blue arrow) where the mini-fragment screw was removed. (E) A 3-T sagittal proton-density-weighted MRI 1 year after bone grafting and fixation of the cartilage fragment. The cartilage fragment healed, and complete filling of the defect was noted (white double arrow); however, incomplete split-like integration into the border zone can be seen (long white arrow). (F) A 3-T sagittal 3-dimensional spoiled gradient echo MRI 1 year after surgery, showing the fixed fragment with a smooth articular surface (white arrowheads) and a similar appearance to normal cartilage (dashed arrow).
Postoperatively, patients were allowed full range of motion but were instructed to not bear weight on the operative knee for 12 weeks. Continuous passive motion devices were not utilized.
Hardware Removal
Patients returned to the operating room 12 weeks after the index procedure for diagnostic arthroscopy and screw removal. After removal of the implant, the repaired lesion was probed and the stability of the repaired loose body noted (Figure 1D).
Magnetic Resonance Imaging
High-resolution MR images were obtained for research purposes to evaluate postoperative healing (Figures 1E, 1F, and 2E). All studies were performed on a 3.0-T General Electric Signa Excite MRI system (GE Healthcare, Milwaukee, Wisconsin, USA) utilizing a dedicated quadrature or 8-channel HD transmit/receive knee coil (GE Healthcare). Routine sequences included sagittal fast spin-echo (FSE) proton density-weighted, sagittal FSE T2-weighted, coronal and axial FSE proton density-weighted with fat saturation, and sagittal 3-dimensional spoiled gradient echo. Minor variations in the parameters, including the repetition and echo delay times, occurred with adjustments in technique that occurred over the dates of acquisition from January 2003 through May 2010.
An experienced musculoskeletal radiologist, blinded to lesion type and treatment, graded the images using the magnetic resonance observation of cartilage repair tissue (MOCART) classification system.28,42 The 9 variables used to describe the repaired articular surface include the degree of filling of the defect, integration into bordering cartilage, surface texture, homogeneity and signal intensity compared with surrounding cartilage, status of the subchondral lamina and bone, and presence of adhesions or synovitis.
Patient-Reported Outcome Assessment
We attempted to contact the 5 identified patients by telephone to determine whether they had subsequent surgery on the operative knee. If so, we reviewed the operative reports for those procedures. Additionally, we asked the patients to complete a questionnaire that allowed us to calculate a Knee injury and Osteoarthritis Outcome Score (KOOS)39 and a Marx activity score.29 A minimal perceptible clinical change in KOOS of 10 points indicated a noticeable departure from that of normal controls.11,39
Data Analysis
A KOOS and Marx activity score was calculated for each patient that completed the questionnaire. A mean and standard deviation was calculated for the Marx activity score and the 5 components of the KOOS. The KOOS components were compared with previously published reference data34 for patients in this age group.
Results
Patient Demographics
Most patients included in the study were male (80%) and skeletally mature at the time of the procedure (80%). The mean duration of symptoms was 26.5 months. Three patients developed knee pain gradually over a period of 12 to 48 months (Figure 2A and 2B). One patient developed symptoms acutely after an injury while playing basketball. Another patient had a 3-year history of knee pain that acutely worsened after a fall from a height (Figure 1A). All lesions were chondral loose bodies (grade 5) with no macroscopic evidence of attached subchondral bone noted at surgery. The mean lesion size was 2.5 cm2. Lesions were located on the medial femoral condyle (60%) and lateral trochlea (40%) (Table 1).
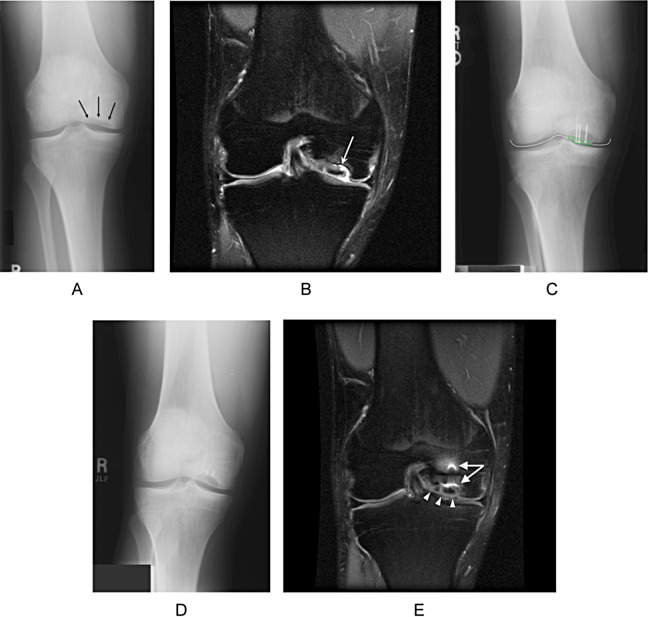
Figure 2.
Patient 5. (A) Preoperative anteroposterior (AP) radiographs demonstrating the osteochondritis dissecans lesion of the medial femoral condyle (black arrows). (B) Coronal proton-density-weighted MRI with fat suppression demonstrates the fragment in situ with fluid signal extending to its undersurface (white arrow). The fragment has a similar signal intensity to normal articular cartilage. At the time of surgery, the fragment was found to be completely disconnected from the underlying crater. (C) AP radiograph 1 week after surgery, showing the mini-fragment screws capturing the articular fragment. The radiograph has been graphically enhanced to show the outline of the radiolucent articular fragment (dashed green line) and demonstrate countersinking of the screws beneath the articular surface (solid white line). (D) AP radiograph 9 months postoperatively. At the time of surgery, the cartilage fragment was found to be thicker than normal articular cartilage. Consequently, bone grafting required to reestablish articular congruity did not reestablish the normal subchondral contour, giving the appearance of a persistent defect. The knee had normal joint spaces and no degenerative changes in the medial compartment. Residual screw tips broken off during removal of hardware were buried within the femoral condyle and caused no sequelae. (E) Coronal proton-density-weighted MRI with fat suppression 9 months after surgery, demonstrating the healed cartilage fragment that has completely filled the defect, has a smooth surface, and is congruent with the remaining portion of the medial femoral condyle (white arrowheads). Metal artifact is visible from the residual hardware (white arrows).
Table 1.
Patient Demographics and Baseline Characteristicsa
| Patient | Age, yb | Sex | Skeletal Maturityc | Duration of Symptoms, mo | Onset of Symptoms | Previous Surgery | Location of Lesion | Lesion Size, cm2 | Graded | Treatment Method | Number of Screws | Bone Graft |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 22 | M | Mature | 36 | Gradual | Plica debridement (2.5 years earlier) | Lateral Trochlea | 1.5 | 5 | ARIF | 2 | No |
| 2 | 13 | M | Immature | 0.5 | Acute | Lateral Trochlea | 3.0 | 5 | ORIF | 2 | LFC | |
| 3 | 18 | M | Mature | 12 | Gradual | MFC | 1.5 | 5 | ORIF | 2 | Proximal tibia | |
| 4 | 17 | F | Mature | 36 | Acute | Drilling of OCD (1 year earlier) | MFC | 2.8 | 5 | ORIF | 3 | Proximal tibia |
| 5 | 25 | M | Mature | 48 | Gradual | MFC | 3.8 | 5 | ORIF | 3 | Proximal tibia | |
| Mean | 19 | 26.5 | 2.5 |
aARIF, arthroscopic reduction internal fixation; LFC, lateral femoral condyle; MFC, medial femoral condyle; ORIF, open reduction internal fixation.
bAge at the time of operative fixation of the loose body.
cMaturity defined as closure of the distal femoral physis.
dGrade 5 lesion = chondral loose bodies without attached bone as an extension of the classification system proposed by Guhl.16
Findings at Removal of Hardware
Four (80%) lesions were stable to probing and had a smooth articular surface (Figure 1D). One lesion (patient 5) was two-thirds healed (2.5 cm2) but had an irregular surface and slight motion with probing of the inferior one-third of the lesion (1.3 cm2).
Magnetic Resonance Imaging
Three patients returned for an MRI after surgery (Figures 1E, 1F, and 2E). The mean time to MRI was 3.1 years. The images showed a range of filling of the defect among patients from complete to incomplete (<50%) (Table 2). All 3 repaired lesions had an intact surface but incomplete integration into the bordering cartilage (Figure 1E). The mean MOCART score was 72 ± 10.4.
Table 2.
MOCART Gradinga
| Patient | Time to Postop MRI, y | Filling of Defect | Integration Into Border Zone | Surface of Repair Tissue | Structure of Repair Tissue | Signal Intensity of Repair Tissue | Subchondral Lamina | Subchondral Bone | Adhesions | Synovitis | MOCART Scoreb |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | — | — | — | — | — | — | — | — | — | — | — |
| 2 | 7.5 | Incomplete, <50% | Incomplete, split-like | Intact | Homogenous | Isointense | Intact | Edema, granulation tissue, sclerosis, mild hypertrophy | No | No | 75 |
| 3 | — | — | — | — | — | — | — | — | — | — | — |
| 4 | 1 | Complete | Incomplete, split-like | Intact | Inhomogenous | Moderate hyperintensity | Not intact | Granulation, microcyst | No | No | 60 |
| 5 | 0.8 | Hypertrophy | Incomplete, split-like | Intact | Homogenous | Isointense | Not Intact | Edema, granulation tissue | No | No | 80 |
| Mean | 3.1 | 72 |
aMOCART (magnetic resonance observation of cartilage repair tissue)28 classification system; MRI, magnetic resonance imaging; Postop, postoperative.28
bMOCART score range = 0-100.42
Repeat Surgery
We were able to contact 80% of patients. The mean time from surgery to contact was 4.6 years. Of the patients contacted, 1 (patient 4) had undergone additional surgery on the index knee for debridement and arthroscopic drilling of an incompletely healed area of the OCD lesion (0.3 cm2; 10% of the total surface area) 1 year after her initial fixation.
Patient-Reported Outcomes
The mean Marx activity score for the 4 patients that completed the questionnaire was 13.5 ± 2.9. The mean KOOS subscale scores for pain (91.0 ± 8.9), knee symptoms (83.0 ± 7.9), and function in activities of daily living (91.9 ± 10.6) were similar to the age-matched controls.34 However, the mean KOOS subscale for sports and recreation function (70.0 ± 17.8) and knee-related quality of life (67.2 ± 12.9) were at least 10 points lower than the age-matched controls (Table 3).34
Table 3.
Intermediate-Term Follow-up KOOS Subscalesa
| Patient | Time to Follow-up, y | Additional Surgery | Marx Activity Scoreb | Pain | Knee Symptoms | Function in Daily Living | Function in Sport and Recreation | Knee-Related Quality of Life |
|---|---|---|---|---|---|---|---|---|
| 1 | 7.8 | No | 16 | 94 | 86 | 94 | 70 | 81 |
| 2 | 4.5 | No | 16 | 94 | 79 | 97 | 60 | 56 |
| 3 | 4.4 | No | 11 | 78 | 75 | 76 | 55 | 56 |
| 4 | 1.8 | Debridement, drilling | 11 | 97 | 93 | 100 | 95 | 75 |
| 5 | None | — | — | — | — | — | — | — |
| Mean ± SD | 4.6 ± 2.5 | 13.5 ± 2.9 | 91.0 ± 8.9 | 83.0 ± 7.9 | 91.9 ± 10.6 | 70.0 ± 17.8 | 67.2 ±12.9 | |
| Controlsc | 92.2 ± 11.2 | 87.2 ± 13.9 | 94.2 ± 10.0 | 85.1 ± 20.8 | 85.3 ± 19.2 |
aRange 0-100; higher scores indicate less pain and other symptoms and better function. KOOS, Knee injury and Osteoarthritis Outcome Score; SD, standard deviation.
bRange, 0-16; higher scores indicated higher levels of activity.
cMean ± SD scores of age-matched controls.34
Complications
One patient had a surgical complication. The tip of 2 screws broke during hardware removal. The residual screw tips were buried in the femoral bone and left in situ (Figure 2D). The patient experienced no sequelae from this complication.
Discussion
To our knowledge, the current study is the first report of operative fixation of chondral loose bodies without macroscopic evidence of attached subchondral bone that includes patient-reported outcome data. The treatment algorithm for chondral loose bodies detached from their subchondral base (grade 5) is not well defined. For these “unsalvageable” lesions, treatment traditionally consists of extraction of the fragment followed by a marrow-stimulating or resurfacing procedure.5,9,19,45
While favorable short-term results have been reported with fragment excision alone,10,12 long-term results are considerably deficient.1,3,7,17,48,49 Ewing and Voto12 reported that 72% of results were satisfactory at 1 year postsurgery for OCD treated with excision of the fragment and drilling of the crater. Denoncourt et al10 noted the presence of fibrocartilage at second-look arthroscopy in the crater at 5 to 15 months after excision and curettage. Conversely, Anderson and Pagnani7 noted that only 40% of grade 3 and 25% of grade 4 lesions had satisfactory results at a mean 9 years after fragment excision, with 50% (10/20) of knees requiring additional surgery. Wright et al48 reported that 65% of cases had fair or poor results at a mean 8.9 years after fragment excision. The low rate of satisfactory results has been attributed to the formation of fibrocartilage in the base of the crater after excision. Fibrocartilage has inferior biomechanical properties compared with normal hyaline cartilage and lacks long-term durability.4,26
Given the limited long-term success rate associated with isolated fragment excision, many surgeons perform a resurfacing procedure following removal of an OCD lesion. While several different resurfacing techniques have been used, none have been universally successful in the treatment of these lesions. Autologous osteochondral transplantation offers a theoretical advantage over marrow-stimulating procedures by both filling the bony defect and providing a hyaline cartilage covering for the OCD lesion.19,45 Even so, low rates of success have been associated with the treatment of lesions >6 cm2,46 and complications related to morbidity at the donor site have been reported.18,20 Furthermore, in a prospective randomized study, Gudas et al14 noted that outcomes were significantly less successful for OCD compared with full-thickness chondral injuries.
Autologous chondrocyte implantation (ACI) has also been performed in conjunction with loose body excision in OCD, with inconsistent results. Several studies have shown significantly lower rates of success with ACI in the treatment of OCD compared with osteochondral defects from other causes, with failure rates ranging from 14% to 67%.21,35,36 A histologic analysis of failed ACI for the treatment of OCD demonstrated an admixture of fibrous connective tissue and fibrocartilage in all cases.21 Conversely, Peterson et al37 showed ACI to be an effective treatment for various chondral lesions and concluded that OCD had the best subjective results relative to other lesion types.
Previous case reports have described fixation of chondral fragments without attached subchondral bone.22,32 Nakamura and colleagues32 described a case of chondral fragment fixation in an adolescent using bioabsorbable pins. At the time of the index procedure, histologic analysis of the lesion demonstrated fracturing through the deep zone of the articular matrix, with fibrous tissue attached to its undersurface.32 Biopsy after fixation revealed complete lesion healing with restoration of normal articular architecture and a normal cartilage–subchondral junction. Lawrence and Ganley22 described a case of arthroscopic suture bridge fixation of a delaminated chondral fragment in an adolescent. At final follow-up, the patient had no knee symptoms and had returned to sports without disability.22 While these reports have some similarities with the current study, the chondral fragments resulted from acute trauma, not OCD, and it is unknown if the etiology of the lesion has an effect on its healing potential. Even so, similar to the results of Nakamura et al,32 our data also indicate that fixation of chondral lesions without visibly attached bone results in stable union of the fragment at short-term follow-up. Intermediate-term follow-up was not available in the studies by Lawrence and Ganley22 and Nakamura et al32; however, follow-up in the current series at a mean 4.6 years after surgery revealed that some of the replaced lesions did not completely heal and required repeat arthroscopy. Reoperation rates reported in the literature for various resurfacing procedures appear to be similar to the rate observed in our study.15,30
Furthermore, at final follow-up, the patients in this series functioned at a nearly normal level in activities of daily living, without significant pain or knee symptoms. However, scores for the sports and recreation function and knee-related quality of life subscales of the KOOS exceed the 10-point cutoff, indicating a noticeable departure from that of normal controls.11,39 Interestingly, in spite of these limitations, the patients were able to maintain a relatively high activity level, as indicated by the mean Marx activity score.
We used the MOCART grading system for MRI analysis because it is an accurate, reliable, and reproducible tool for assessing cartilage repair.27 The overall MOCART score42 demonstrated similar outcomes for the 2 patients with short-term and 1 patient with intermediate-term MRI follow-up. Incomplete MRI follow-up limits conclusions that can be made about the radiographic durability of the repair over time. Assessment of the 9 MOCART parameters and overall MOCART score showed differences between the observed repair tissue of these patients and that of normal cartilage. Even so, the mean MOCART score from our series appears comparable to patients treated with matrix-associated ACI (MACI) for OCD.33,47 However, differences between the biomaterial scaffolds used in MACI and the native-repaired cartilage in our series limit comparability between these studies.
This study had several significant limitations. Primarily, the small study size, inhomogenous patient demographics, and lack of a comparison group in this series limit evaluation of the results of this technique relative to other treatment options. However, limited outcome or evidence of osteoarthritis has been observed in 50% to 75% of patients at 5 to 15 years after fragment excision.1,3,7,17,48,49 While we acknowledge that larger studies with longer follow-up times are required to make more definitive treatment recommendations, our preliminary data suggest that operative fixation of an intact chondral loose body is a viable alternative to extraction of the fragment. We were able to obtain 80% follow-up in this series; therefore, we believe that response bias in our study was minimal. However, selection bias could have resulted from inaccurate CPT code documentation, resulting in failure to identify other relevant cases. Furthermore, the lack of pretreatment patient-reported outcome scores limits an analysis of the change in these data after intervention.
Additionally, while macroscopic observation of the loose bodies extracted during surgery revealed chondral lesions with no visible bone attached, a histologic analysis was not performed to substantiate this observation. Consequently, the exact layer of separation of the articular cartilage–subchondral unit could not be determined, and it is unknown if a microscopic layer of bone was present on the undersurface of the lesions. Even so, Uozumi et al44 performed a histological analysis of grade 2 and 3 OCD lesions and determined that 58% of the OCD fragments were composed of cartilage alone. The cartilage fragments were substantially thicker than normal articular cartilage, and, consequently, they hypothesized that the bony base of the fragments likely remodeled into cartilage after the fragment became disassociated from the femoral condyle.44 Furthermore, a histologic analysis by Milgram31 determined that 24 of 50 (48%) OCD lesions classified as grade 4 did not have subchondral bone attached.31 Given the findings of these previous studies and the lack of visible bone on the loose bodies in the current series, it is possible the lesions in our study did not have attached bone on their undersurface.
Conclusion
Operative fixation of chondral loose bodies, without macroscopic evidence of a subchondral bony base, resulted in stable fixation at second-look arthroscopy. At a mean 4.6 years after surgery, patients did not have substantial pain or symptoms and had normal function in activities of daily life; however, they had significantly lower knee-related quality of life and sport and recreation function. Prospective, comparative studies are needed to determine the efficacy of this technique relative to other treatment options.
Acknowledgment
The authors thank Tracey Fine, MS, ELS (Fine Biomedical Communications Inc, Chapel Hill, North Carolina, USA) for editing the manuscript. They also thank Lynn Cain for assistance with manuscript submission.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.F.A. is an associate editor for the Orthopaedic Journal of Sports Medicine (OJSM); R.A.M. has received reimbursement from DePuy Mitek for traveling to an education symposium and is on the editorial board of OJSM; and Vanderbilt Sports Medicine has received funds for research and/or education grants from Smith & Nephew Endoscopy and DonJoy Orthopaedic.
References
- 1. Aglietti P, Ciardullo A, Giron F, Ponteggia F. Results of arthroscopic excision of the fragment in the treatment of osteochondritis dissecans of the knee. Arthroscopy. 2001;17:741–746. [DOI] [PubMed] [Google Scholar]
- 2. Aichroth P. Osteochondral fractures and their relationship to osteochondritis dissecans of the knee. An experimental study in animals. J Bone Joint Surg Br. 1971;53:448–454. [PubMed] [Google Scholar]
- 3. Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg Br. 1971;53:440–447. [PubMed] [Google Scholar]
- 4. Akeson WH, Bugbee W, Chu C, Giurea A. Differences in mesenchymal tissue repair. Clin Orthop Relat Res. 2001;(391 suppl):S124–S141. [DOI] [PubMed] [Google Scholar]
- 5. Anderson AF, Anderson CN. Management of osteochondritis dissecans of the knee. Techn Knee Surg. 2005;4(1):23–35. [Google Scholar]
- 6. Anderson AF, Lipscomb AB, Coulam C. Antegrade curettement, bone grafting and pinning of osteochondritis dissecans in the skeletally mature knee. Am J Sports Med. 1990;18:254–261. [DOI] [PubMed] [Google Scholar]
- 7. Anderson AF, Pagnani MJ. Osteochondritis dissecans of the femoral condyles. Long-term results of excision of the fragment. Am J Sports Med. 1997;25:830–834. [DOI] [PubMed] [Google Scholar]
- 8. Clanton TO, DeLee JC. Osteochondritis dissecans. History, pathophysiology and current treatment concepts. Clin Orthop Relat Res. 1982;(167):50–64. [PubMed] [Google Scholar]
- 9. Crawford DC, Safran MR. Osteochondritis dissecans of the knee. J Am Acad Orthop Surg. 2006;14(2):90–100. [DOI] [PubMed] [Google Scholar]
- 10. Denoncourt P, Patel D, Dimakkopoulos P. Arthroscopy updated #1. Treatment of osteochondrosis dissecans of the knee by arthroscopic curettage, follow-up study. Orthop Rev. 1986;15:652–657. [PubMed] [Google Scholar]
- 11. Ehrich EW, Davies GM, Watson DJ, Bolognese JA, Seidenberg BC, Bellamy N. Minimal perceptible clinical improvement with the Western Ontario and McMaster Universities osteoarthritis index questionnaire and global assessments in patients with osteoarthritis. J Rheumatol. 2000;27:2635–2641. [PubMed] [Google Scholar]
- 12. Ewing JW, Voto SJ. Arthroscopic surgical management of osteochondritis dissecans of the knee. Arthroscopy. 1988;4:37–40. [DOI] [PubMed] [Google Scholar]
- 13. Green WT, Banks HH. Osteochondritis dissecans in children. J Bone Joint Surg Am. 1953;35-A:26–47. [PubMed] [Google Scholar]
- 14. Gudas R, Kalesinskas RJ, Kimtys V, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21:1066–1075. [DOI] [PubMed] [Google Scholar]
- 15. Gudas R, Simonaityte R, Cekanauskas E, Tamosiūnas R. A prospective, randomized clinical study of osteochondral autologous transplantation versus microfracture for the treatment of osteochondritis dissecans in the knee joint in children. J Pediatr Orthop. 2009;29:741–748. [DOI] [PubMed] [Google Scholar]
- 16. Guhl JF. Arthroscopic treatment of osteochondritis dissecans. Clin Orthop Relat Res. 1982;(167):65–74. [PubMed] [Google Scholar]
- 17. Hefti F, Beguiristain J, Krauspe R, et al. Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231–245. [PubMed] [Google Scholar]
- 18. Jakob RP, Franz T, Gautier E, Mainil-Varlet P. Autologous osteochondral grafting in the knee: indication, results, and reflections. Clin Orthop Relat Res. 2002;(401):170–184. [DOI] [PubMed] [Google Scholar]
- 19. Kocher MS, Tucker R, Ganely TJ, Flynn JM. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34:1181–1191. [DOI] [PubMed] [Google Scholar]
- 20. LaPrade RF, Botker JC. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20:e69–e73. [DOI] [PubMed] [Google Scholar]
- 21. LaPrade RF, Bursch LS, Olson EJ, Havlas V, Carlson CS. Histologic and immunohistochemical characteristics of failed articular cartilage resurfacing procedures for osteochondritis of the knee: a case series. Am J Sports Med. 2008;36:360–368. [DOI] [PubMed] [Google Scholar]
- 22. Lawrence JT, Ganley TJ. All arthroscopic suture-bridge fixation of a delaminated chondral fragment. Unv Penn Orthopaedic Jour. 2010;21:83–86. [Google Scholar]
- 23. Lindén B. The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand. 1976;47:664–667. [DOI] [PubMed] [Google Scholar]
- 24. Lipscomb PR, Jr, Lipscomb PR, Sr, Bryan RS. Osteochondritis dissecans of the knee with loose fragments. Treatment by replacement and fixation with readily removed pins. J Bone Joint Surg Am. 1978;60:235–240. [PubMed] [Google Scholar]
- 25. Magnussen RA, Carey JL, Spindler KP. Does operative fixation of an osteochondritis dissecans loose body result in healing and long-term maintenance of knee function? Am J Sports Med. 2009;37:754–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mandelbaum BR, Browne JE, Fu F, et al. Articular cartilage lesions of the knee. Am J Sports Med. 1998;26:853–861. [DOI] [PubMed] [Google Scholar]
- 27. Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S. Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol. 2006;57:16–23. [DOI] [PubMed] [Google Scholar]
- 28. Marlovits S, Striessnig G, Resinger CT, et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol. 2004;52:310–319. [DOI] [PubMed] [Google Scholar]
- 29. Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–218. [DOI] [PubMed] [Google Scholar]
- 30. McNickle AG, L'Heureux DR, Yanke AB, Cole BJ. Outcomes of autologous chondrocyte implantation in a diverse patient population. Am J Sports Med. 2009;37:1344–1350. [DOI] [PubMed] [Google Scholar]
- 31. Milgram JW. Radiological and pathological manifestations of osteochondritis dissecans of the distal femur. A study of 50 cases. Radiology. 1978;126:305–311. [DOI] [PubMed] [Google Scholar]
- 32. Nakamura N, Horibe S, Iwahashi T, Kawano K, Shino K, Yoshikawa H. Healing of a chondral fragment of the knee in an adolescent after internal fixation. A case report. J Bone Joint Surg Am. 2004;86-A:2741–2746. [DOI] [PubMed] [Google Scholar]
- 33. Ochs BG, Muller-Horvat C, Albrecht D, et al. Remodeling of articular cartilage and subchondral bone after bone grafting and matrix-associated autologous chondrocyte implantation for osteochondritis dissecans of the knee. Am J Sports Med. 2011;39:764–773. [DOI] [PubMed] [Google Scholar]
- 34. Paradowski PT, Bergman S, Sundén-Lundius A, Lohmander LS, Roos EM. Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord. 2006;7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A. Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med. 2002;30:2–12. [DOI] [PubMed] [Google Scholar]
- 36. Peterson L, Minas T, Brittberg M, et al. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res. 2000;(374):212–234. [DOI] [PubMed] [Google Scholar]
- 37. Peterson L, Vasiliadis HS, Brittberg M, Lindahl A. Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med. 2010;38:1117–1124. [DOI] [PubMed] [Google Scholar]
- 38. Ribbing S. The hereditary multiple epiphyseal disturbance and its consequences for the aetiogenesis of local malacias—particularly the osteochondrosis dissecans. Acta Orthop Scand. 1955;24:286–299. [DOI] [PubMed] [Google Scholar]
- 39. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Smillie IS. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39-B:248–260. [DOI] [PubMed] [Google Scholar]
- 41. Tallqvist G. The reaction to mechanical trauma in growing articular cartilage. An experimental study on rabbits and a comparison of the results with the pathological anatomy of osteochondritis dissecans. Acta Orthop Scand Suppl. 1962;53:1–112. [PubMed] [Google Scholar]
- 42. Trattnig S, Ba-Ssalamah A, Pinker K, Plank C, Vecsei V, Marlovits S. Matrix-based autologous chondrocyte implantation for cartilage repair: noninvasive monitoring by high-resolution magnetic resonance imaging. Magn Reson Imaging. 2005;23:779–787. [DOI] [PubMed] [Google Scholar]
- 43. Twyman RS, Desai K, Aichroth PM. Osteochondritis dissecans of the knee. A long-term study. J Bone Joint Surg Br. 1991;73:461–464. [DOI] [PubMed] [Google Scholar]
- 44. Uozumi H, Sugita T, Aizawa T, Takahashi A, Ohnuma M, Itoi E. Histologic findings and possible causes of osteochondritis dissecans of the knee. Am J Sports Med. 2009;37:2003–2008. [DOI] [PubMed] [Google Scholar]
- 45. Wall E, Von Stein D. Juvenile osteochondritis dissecans. Orthop Clin North Am. 2003;34:341–353. [DOI] [PubMed] [Google Scholar]
- 46. Wang CJ. Treatment of focal articular cartilage lesions of the knee with autogenous osteochondral grafts. Arch Orthop Trauma Surg. 2002;122:169–172. [DOI] [PubMed] [Google Scholar]
- 47. Welsch GH, Mamisch TC, Zak L, et al. Evaluation of cartilage repair tissue after matrix-associated autologous chondrocyte transplantation using a hyaluronic-based or a collagen-based scaffold with morphological MOCART scoring and biochemical T2 mapping: preliminary results. Am J Sports Med. 2010;38:934–942. [DOI] [PubMed] [Google Scholar]
- 48. Wright RW, McLean M, Matava MJ, Shively RA. Osteochondritis dissecans of the knee: long-term results of excision of the fragment. Clin Orthop Relat Res. 2004;(424):239–243. [PubMed] [Google Scholar]
- 49. Zarzycki W. Evaluation of treatment results for osteochondritis dissecans of the knee joint [in Polish]. Chir Narzadow Ruchu Ortop Pol. 2001;66:61–66. [PubMed] [Google Scholar]