Abstract
Background:
Anterior cruciate ligament (ACL) rupture is a significant injury in male Major League Soccer (MLS) players in the United States.
Purpose:
To determine (1) return-to-sport (RTS) rate in MLS following ACL reconstruction (ACLR), (2) timing of RTS, (3) performance upon RTS, and (4) the difference in RTS and performance between players who underwent ACL reconstruction (ACLR) and controls.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
MLS players undergoing ACLR between 1996 and 2012 were evaluated. Player data were extracted from publically available sources. All demographic data were analyzed. A control group of players matched by age, body mass index (BMI), sex, position, performance, and MLS experience (occurred at 2.6 years into career, designated “index year”) was selected from the MLS during the same years as those undergoing ACLR. The RTS and performance in the MLS were analyzed and compared between cases and controls. Student ttests were performed for analysis of within- and between-group variables.
Results:
A total of 52 players (57 knees) that met inclusion criteria underwent ACLR while in the MLS. Mean player age was 25.6 ± 3.98 years. Forty players were able to resume play (77%). Of the 40 players (45 knees), 38 (43 knees; 95%) resumed play the season following ACLR (mean, 10 ± 2.8 months after surgery). Mean career length in the MLS after ACLR was 4.0 ± 2.8 years. The revision rate was 10%. There was a significant increase in the incidence of ACL tears in the MLS by year (P < .001), and there was a significantly (P= .002) greater number of ACL tears on the left knee as opposed to the right. Performance in the MLS upon RTS after ACLR was not significantly different versus preinjury. There was no significant difference in survival in the MLS between cases and controls after ACLR or index year. The only significant performance differences between cases and controls were that cases had significantly greater shots taken per season (P= .005) and assists (P= .005) than did controls after the index year.
Conclusion:
There is a high RTS rate in the MLS following ACLR. Nearly all players resumed play the season after surgery. Performance was not significantly different from preinjury. Only 2 performance measures (shots taken and assists) were significantly different between cases and controls. A significantly greater number of ACL tears occur in the left versus the right knee.
Keywords: anterior cruciate ligament, Major League Soccer, return to sport, knee
Anterior cruciate ligament (ACL) tears are one of the most common injuries in both contact and noncontact sports.5,6,17 It is estimated that there will be approximately 250,000 ACL tears in the United States this year alone,1,11 over half of which will be reconstructed.8 Soccer is the most popular sport worldwide. Approximately 40% of all knee injuries in soccer are ACL related.15 While many studies report a high success rate after ACL reconstruction (ACLR),9 the data concerning professional athletes in United States Major League Soccer (MLS) and their ability to return to sport (RTS) and perform in the league after an ACL tear are sparse. To our knowledge, there have been no published studies to date that have reported the RTS rate for MLS players or that have analyzed their in-game performance before and after ACLR. Although multifactorial, it is well known that the risk of degenerative knee arthritis after ACL tear is significantly increased.10,18
The primary purposes of this investigation were to determine (1) the rate of RTS in the MLS after ACLR, (2) the timing of RTS after ACLR, (3) the performance upon RTS after ACLR, and (4) the difference in RTS and performance between players who sustained an ACL tear and control players matched by age, body mass index (BMI), sex, and MLS experience. We hypothesized that MLS players who sustain an ACL tear and undergo reconstruction would have a high RTS rate, with RTS the season following surgery; that there would be no difference in performance upon RTS between pre- and postsurgery but performance would decline with time; and that there would be no difference in the rate of RTS or performance between cases (ACLR) and controls (no ACL tear).
Materials and Methods
This study evaluated MLS players who sustained an ACL tear and who underwent reconstruction between 1996 (the inception of the league) and 2012. These players were identified through MLS team websites, publically available Internet-based injury reports, player profiles and biographies, and press releases. The search was conducted manually by an orthopaedic surgery resident and a board-eligible orthopaedic surgeon in sports medicine fellowship training. Searches were performed for all MLS teams and players. All players identified were included in this study as it related to RTS rate. A player was deemed to have successfully resumed sport if he played in any MLS game after surgery. Players with less than 1 season (8 months) of follow-up after ACLR were not included in RTS rate. Subject inclusion criteria were any male MLS player having been drafted into the league or having played at least 1 MLS game prior to acute ACL tear. Certain concomitant knee injuries, when known, were deemed acceptable (articular cartilage injury, meniscal tear, and medial collateral ligament [MCL] OR lateral collateral ligament tear [but not both at same time]). Subject exclusion criteria were female sex, collegiate players (National Collegiate Athletic Association [NCAA]), and bicruciate (ACL and complete posterior cruciate ligament [PCL]) or combined ACL and bicollateral ligament injury. Players for whom no RTS or performance data could be found were also excluded.
Players who returned to the MLS and had played in at least 1 game were included in the preinjury and post-ACLR in-game performance statistical analysis. We collected and analyzed demographic data (age at time of injury, BMI [kg/m2], position [forward, midfield, defense, goalie], months from injury to RTS, side of injury [right vs left], games played per season, and if the player returned to the MLS the season following the injury) as well as mean in-game performance data (minutes per game and per-season goals, shots, shots on goal, yellow cards, red cards, fouls committed, and assists). In-game performance variables were analyzed as an average over the preinjury and post-ACLR course of players’ careers. In addition, in-game performance variables were analyzed separately in each of the first 5 subsequent seasons the player returned to the MLS following injury.
A control group was selected to compare the data to the case (ACLR) group. Controls were matched to cases based on sex, age, BMI, position played (midfield, defense, forward, goalie), years of experience in MLS, number of games played per season, minutes played per game, and number of goals scored (Table 1). ACLR occurred at a mean of 2.61 ± 2.59 years into a player’s career. An “index year” was designated for controls, analogous to the ACLR year in cases, as a matched reference year (relative to years of experience in MLS) to compare performance after ACLR or index year. Demographic data (BMI, age, years in the MLS) and in-game performance data were collected and analyzed over the course of players' careers before and after the index year (each season analyzed individually and collectively).
Table 1.
Comparison of Cases and Controls Before ACLR or Index Yeara
| Pre-ACLR | Pre–Index Year | PValue (Paired Samples Student t Test) | |
|---|---|---|---|
| Mean seasons MLS experience | 2.61 ± 2.59 | 2.69 ± 2.66 | .948 |
| Mean games played per season | 17.8 ± 8.55 | 18.3 ± 5.73 | .622 |
| Mean minutes/game | 68.7 ± 19.5 | 65.6 ± 18.2 | .950 |
| Mean goals/season | 3.24 ± 7.04 | 2.20 ± 3.93 | .261 |
| Mean age, y | 25.6 ± 3.98 | 25.6 ± 2.61 | .942 |
| Body mass index, kg/m2 | 23.6 ± 1.35 | 23.6 ± 1.03 | .910 |
aValues are expressed as mean ± standard deviation. ACLR, anterior cruciate ligament reconstruction; MLS, Major League Soccer.
Single-variable analyses for all continuous variables (performance measures) within groups were performed using Student ttests for normally distributed data. One-sample Kolmogorov-Smirnov goodness-of-fit tests for Gaussian data distribution were performed and confirmed normality of all data. Bonferroni correction was used to control for multiple comparisons. Linear regression was used to determine if there was a significant increase in the incidence of ACL tear per year. Comparisons between case and control groups were made using Student ttests. Comparisons were made between cases and controls for survival in MLS and each individual parameter’s overall mean (all years before and all years after ACLR [or index year]), and each individual year (up to 5 years) after ACLR (or index year in controls). All statistical analyses were performed using PASW Statistics Student Version 18.0.0 (IBM, Armonk, New York).
Results
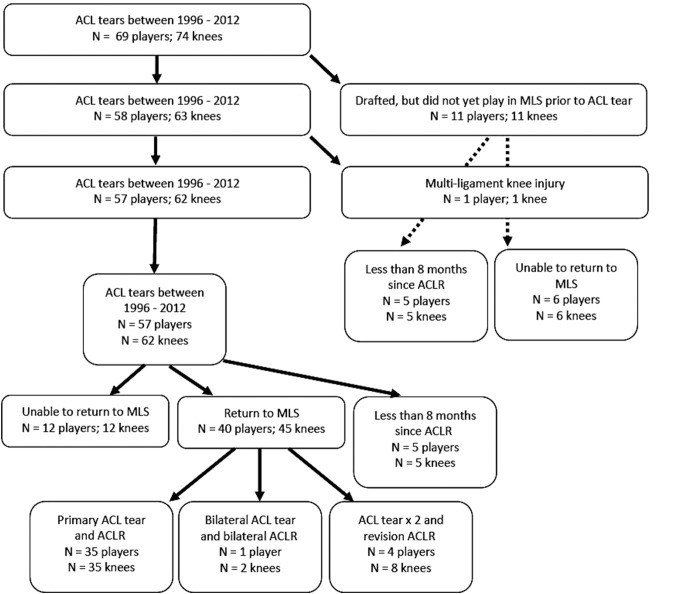
A total of 69 players (74 knees) who sustained ACL tears and underwent ACLR were identified between 1996 (the inception of the MLS) and 2012 (Figure 1). Demographic data of all players undergoing ACLR are reported in Table 2. Fifty-seven players (62 knees) played at least 1 game in the MLS prior to ACL tear (11 players tore their ACL after being drafted but before playing a regular-season MLS game). Since the year 2000, there has been at least 1 ACL tear per year (mean, 4.4 ± 3.1 tears per year) (Figure 2). There was a significant increase in the incidence of ACL tear in the MLS by year (P < .001). There was a significantly greater number of ACL tears of the left versus the right knee (P = .002). Concurrent knee injuries were identified in only 3 subjects (MCL). Graft type for surgical reconstruction was not identified.
Figure 1.
Flow chart of selection process for inclusive Major League Soccer (MLS) players. ACLR, anterior cruciate ligament reconstruction.
Table 2.
Demographic Data of MLS Players Undergoing ACLRa
| Number of players | 69 |
| Number of ACL tearsb | 74b |
| Age, y, mean ± SD | 25.6 ± 3.98 |
| Body mass index, kg/m2, mean ± SD | 23.6 ± 1.35 |
| No. of knees (%) | |
| Right | 24 (32) |
| Left | 50 (68) |
| MLS experience before ACL tear, y, mean ± SD | 2.61 ± 2.59 |
| Position, n | |
| Midfield | 31 |
| Defense | 18 |
| Forward | 16 |
| Goalie | 4 |
| ACL tear timing, n | |
| In-season game | 69 |
| In-season practice | 2 |
| Preseason soccer | 3 |
aACLR, anterior cruciate ligament reconstruction; MLS, Major League Soccer; SD, standard deviation.
bA total of 64 players had primary ACL tear (64 knees), 1 player had bilateral ACL tears (2 knees), 4 players had primary and re-tear of ACL in same knee (8 knees).
Figure 2.
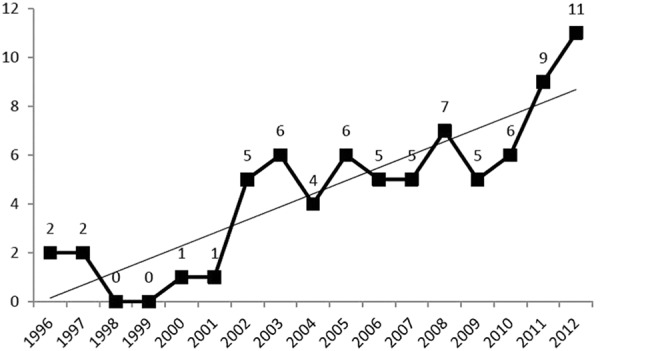
Number of anterior cruciate ligament tears per year in Major League Soccer.
Of the 52 players (57 knees) with at least 1 MLS season of follow-up (8 months) since ACLR, 40 players (45 knees) were able to resume playing in the MLS (77% rate of RTS). Of these 40 players (45 knees), 38 (43 knees, 95%) were able to return the season after their surgery (mean, 10 ± 2.8 months after surgery). Length of career in the MLS following ACLR was 4.0 ± 2.8 years. However, 24 players who underwent ACLR and RTS are still playing in the MLS. Survival within the MLS is illustrated in Figure 3. The rate of revision ACLR was 10% (4 players required revision ACLR for 4 ACL retears). With regard to player position, 75% of goalies returned to play in the MLS after ACLR, versus 81% of defenders, 67% of midfielders, and 91% of forwards. Performance upon RTS following ACLR in the MLS was not significantly different versus preinjury (Table 3). Comparison of performance before and after the index year in controls (Table 4) demonstrated that players participated in significantly fewer games and take significantly fewer total shots and shots on goal.
Figure 3.
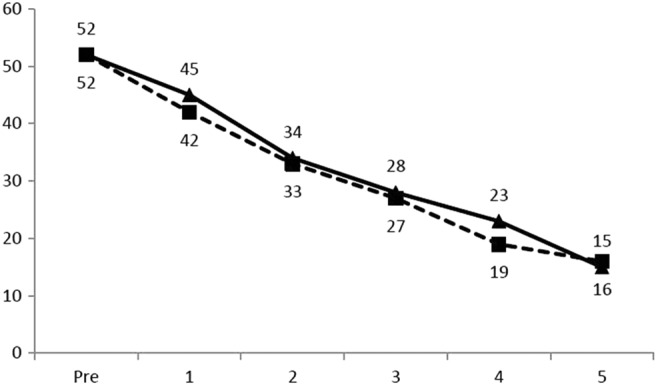
Number of Major League Soccer players before and after anterior cruciate ligament reconstruction (dashed line) or after index year in controls (solid line) (years 1-5).
Table 3.
Performance Comparison Before and After ACLR (40 Players and 45 Knees)a
| Before ACL Tear | After ACLR | PValue (Paired Samples Student tTest)b | |
|---|---|---|---|
| No. of seasons in MLS | 2.61 ± 2.59 | 4.00 ± 2.78 | .011 |
| Games played per season | 17.8 ± 8.55 | 18.8 ± 5.91 | .558 |
| Minutes per game | 68.7 ± 19.5 | 69.0 ± 17.8 | .924 |
| Goals per season | 3.24 ± 7.04 | 3.17 ± 5.75 | .899 |
| Total shots per season | 17.7 ± 17.8 | 19.0 ± 14.9 | .698 |
| Shots on goal per season | 7.48 ± 7.92 | 7.15 ± 6.00 | .794 |
| Assists per season | 2.53 ± 2.75 | 2.18 ± 1.69 | .455 |
| Yellow cards per season | 2.62 ± 2.12 | 2.71 ± 1.87 | .832 |
| Red cards per season | 0.15 ± 0.24 | 0.26 ± 0.36 | .154 |
| Fouls committed per season | 20.0 ± 12.3 | 19.4 ± 11.7 | .800 |
aValues are expressed as mean ± standard deviation. ACLR, anterior cruciate ligament reconstruction; MLS, Major League Soccer.
bNo differences were statistically significant.
Table 4.
Control Population Performance Before and After Index Yeara
| Before Index Year | After Index Year | PValue (Paired Samples Student tTest)b | |
|---|---|---|---|
| No. of seasons in MLS | 2.69 ± 2.66 | 2.52 ± 2.50 | .811 |
| Games played per season | 18.3 ± 5.73 | 14.5 ± 7.98 | .0003 |
| Minutes per game | 65.6 ± 18.2 | 64.7 ± 21.5 | .908 |
| Goals per season | 2.20 ± 3.93 | 1.24 ± 1.91 | .045 |
| Total shots per season | 14.5 ± 12.3 | 9.72 ± 9.70 | .0003 |
| Shots on goal per season | 6.34 ± 5.59 | 3.72 ± 4.20 | .00002 |
| Assists per season | 1.70 ± 1.32 | 1.29 ± 1.45 | .067 |
| Yellow cards per season | 2.75 ± 2.16 | 2.26 ± 1.67 | .055 |
| Red cards per season | 0.17 ± 0.29 | 0.15 ± 0.22 | .618 |
| Fouls committed per season | 21.1 ± 14.8 | 16.4 ± 12.5 | .029 |
aValues are expressed as mean ± standard deviation. MLS, Major League Soccer.
bStatistically significant differences have a Pvalue < .005.
There was no significant difference between cases and controls in survival in the MLS (playing at least 1 game per season) from preinjury (pre–index year in controls) to post-ACLR (post–index year in controls) from years 1 through 5 (Figure 3). After ACLR (or index year [controls]), those undergoing ACLR had a significantly greater number of shots per season and a significantly greater mean number of assists per season versus controls (Table 5). With regard to individual years after ACLR (or index year in controls), there were no significant differences between groups in any performance parameter (see the Appendix).
Table 5.
Comparison of Case and Control Performance After Surgery or Index Yeara
| After ACLR | After Index Year | P Valueb | |
|---|---|---|---|
| No. of seasons in MLS | 4.00 ± 2.78 | 2.52 ± 2.50 | .473 |
| Games played per season | 18.8 ± 5.91 | 14.5 ± 7.98 | .014 |
| Minutes per game | 69.0 ± 17.8 | 64.7 ± 21.5 | .424 |
| Goals per season | 3.17 ± 5.75 | 1.24 ± 1.91 | .079 |
| Total shots per season | 19.0 ± 14.9 | 9.72 ± 9.70 | .005 |
| Shots on goal per season | 7.15 ± 6.00 | 3.72 ± 4.20 | .011 |
| Assists per season | 2.18 ± 1.69 | 1.29 ± 1.45 | .005 |
| Yellow cards per season | 2.71 ± 1.87 | 2.26 ± 1.67 | .294 |
| Red cards per season | 0.26 ± 0.36 | 0.15 ± 0.22 | .079 |
| Fouls committed per season | 19.4 ± 11.7 | 16.4 ± 12.5 | .520 |
aValues are expressed as mean ± standard deviation. ACLR, anterior cruciate ligament reconstruction; MLS, Major League Soccer.
bStatistically significant differences have a Pvalue < .005.
Discussion
This case-control study of MLS players undergoing ACLR has demonstrated a 77% RTS rate. Nearly all (95%) players who were able to resume their careers in the MLS did so in the season following surgery (mean, 10 months). Performance after ACLR was not significantly worse than preinjury performance, and survival in the MLS was not significantly different between cases and age-, BMI-, position-, performance-, and MLS experience–matched controls. There were only 2 performance measures (total shots taken and assists) that were significantly different between cases and controls. A significantly greater number of ACL tears occurred in the left versus the right knee. All but 1 study hypothesis was confirmed (we had hypothesized that performance would decline with time following ACLR, although this did not occur).
Tears to the ACL are common serious injuries in soccer.14 Although return to elite soccer after ACLR is possible (and demonstrated with a 77% RTS rate in this case-control study), such an injury can also signal the early end to an MLS player's career. Injury can sometimes occur even before the “career” begins (55% [6/11] of players drafted but not yet played a single MLS game were unable to ever play in the MLS). Prior studies have shown both favorable12,13 and unfavorable outcomes4 after ACLR with regard to patient satisfaction, specifically in athletes. A recent cohort study from the Multicenter Orthopaedic Outcomes Network (MOON) group demonstrated a 72% rate of RTS in soccer athletes.3 Although the latter is consistent with the findings in the current investigation, the MOON group cohort had a 3% revision rate (3 players) versus 10% found in the current study. A separate case-control study performed at our institution (currently in press) examined RTS and performance in 64 players for the National Basketball Association (NBA). That study demonstrated a similar return to high-level sports (80% to the NBA and all but 1 player [99%] returned to any level of competitive professional basketball). Similarly, there was a low rate (3.1%) of revision versus the current study (10%). However, in the NBA study, performance significantly declined in several performance parameters (games/season; minutes, points, and rebounds per game; and field goal percentage). This is in contrast to the current investigation, which demonstrated no significant performance differences between preinjury and post-ACLR. Other than games played per season, NBA athletes undergoing ACLR were not significantly different from controls. Similarly, MLS players undergoing ACLR demonstrated only 2 significant differences (number of shots taken and assists) versus controls.
The largest elite soccer (football) ACL injury study in the current literature reflects both men’s and women’s teams in the Union of European Football Associations (UEFA).7,19 Their cohorts reflect similar ages (25.2 years)7,19 versus the current investigation (25.6 years). Additionally, players that RTS did so at 10 months following surgery (similar to the current investigation).7,19 What is different in the current investigation is the lower rate of RTS (77%) versus the UEFA cohort (94%).7,19 The explanation for the RTS difference is unknown. Within the current MLS cohort, graft type is unknown. In the UEFA cohort, “the majority of players underwent ACL reconstruction using a patellar tendon graft.”7,19 No significant difference between patellar tendon and hamstring grafts has been demonstrated with clinical outcomes and/or RTS rates in athletes.16 A comparison of the level of play and its influence before and after ACL injury between the UEFA and MLS is beyond the scope of the current study.
A unique exploratory finding in the current investigation is that a significantly greater number (68%) of ACL tears in MLS players occurred in their left knee. In the previously reported NBA player case-control study, the side distribution (right vs left) was nearly equal (51% vs 49%, respectively). We speculate that right-footed kickers have a higher propensity of tearing their left ACL since the plant foot is the left leg. When the players are preparing to strike a ball with their right foot, they load their left leg with a significant amount of torque and stress to ensure maximal force distribution to the ball with their contralateral foot. The axial load, in combination with valgus angulation and rotational torque, potentially plays a major role in these ACL tears. However, this hypothesis was recently tested in 93 soccer athletes at an outpatient orthopaedic clinic.2 There were 58 noncontact injuries within that cohort, and male athletes were found to be significantly more likely to injure their kicking leg (right leg) (74% vs 26%), while females were more likely to injure their support leg (left leg) (68% vs 32%). In the current investigation, foot dominance could not be identified, and so this conclusion is extrapolated from the hypothesis that most players are right-foot dominant. We did attempt to locate videos of each player’s ACL injury via Google, ESPN, MLS, and YouTube searches to investigate this theory; however, we were unable to locate any to corroborate. Further, the mechanism of injury (contact vs noncontact) was unable to be elucidated in the current investigation.
Although this study is the most comprehensive analysis on how ACLR in MLS players affects performance, there are several limitations. First, there may have been MLS players whose ACL tears were not discovered because of the search methodology. Although both an orthopaedic surgery resident and a board-eligible orthopaedic surgeon in sports medicine fellowship training conducted separate searches to look for all MLS players between 1996 and 2012 who tore their ACLs, some may have been missed. However, the same players were identified in each independent search. We acknowledge the limitation of publically available data sources, with reliability and accuracy only as good and reputable as the source. The MLS does not currently have an injury database (as opposed to that of the National Football League’s Combine). It is our hope that studies similar to the current one may instigate team physicians to lead an initiative to gather player data in an electronic system so that future research may be done on this unique patient population. Because of this limitation, the publically available sources mentioned are the best that currently exist. The high-profile nature of these athletes means they are unable to be easily contacted. Their concomitant knee injury status was known only if reported in the same publically available sources that reported the ACL injury. Further, the current investigation has shown that the incidence of ACL tear increased by year. Three reasons may account for this: (1) the less common utilization of electronic reporting of injury during the early years of the study, (2) the less common divulgence of player injury information and status during the early years of the study, and (3) the more common use of social media in sports medicine by athletes themselves disclosing their injury (eg, Twitter and Facebook). Additionally, we were unable to identify and report any validated clinical outcome scores in these players. Further, patient satisfaction and personal perception of knee pain, function, and stability were unable to be assessed versus preinjury. These factors may influence RTS performance. Surgical technique information (single- vs double-bundle, 1- vs 2-incision, bone–patellar tendon–bone vs hamstring, autograft vs allograft, transtibial vs accessory anteromedial femoral tunnel drilling, meniscal and articular cartilage concomitant injury) was unobtainable from publically available sources. Similarly, postoperative physical examination (eg, Lachman, pivot-shift), instrumented laxity (KT-1000 and KT-2000 arthrometers), and imaging (radiographic assessment of degenerative changes, magnetic resonance imaging assessment of meniscal and/or chondral damage) outcomes were unavailable. This relevant information is important as it is well known that soccer players that sustain ACL tear have significantly increased rates of radiographic osteoarthritis.10,18 Additionally, the rehabilitation program utilized postoperatively was unavailable. Even though some players were unable to return to play in the MLS following ACLR, the inability to return cannot solely be attributed to ACL injury and surgery, as other confounders inevitably coexist. Further, although all performance-based measures were used to compare pre- and postoperative outcomes and between cases and controls, other intangibles (team leadership, teammate motivation, etc) cannot be assessed for relationships. Selection of the control group was matched by sex, age, BMI, position, performance, and MLS experience. Despite the detail of the control-matching process, the groups are inevitably not exactly the same and unquantifiable differences certainly exist.
Conclusion
There is a high RTS rate in the MLS for players after undergoing ACLR; nearly all players returned the season following surgery. In-game performance was not significantly different from preinjury. Only 2 performance measures (shots taken and assists) were significantly different between cases and controls. A significantly greater number of ACL tears occur in the left versus the right knee.
Appendix
Years 1 to 5 After ACL Reconstruction (Cases) Versus Index Year (Controls)a
| Case Group (Year 1 After ACLR) | Control Group | P Value | |
|---|---|---|---|
| Games played per season | 16.5 ± 8.44 | 15.4 ± 9.51 | .543 |
| Minutes per game | 61.6 ± 25.4 | 65.5 ± 20.9 | .413 |
| Goals per season | 3.05 ± 6.71 | 1.34 ± 2.24 | .120 |
| Total shots per season | 16.1 ± 16.9 | 10.9 ± 12.1 | .090 |
| Shots on goal per season | 6.15 ± 7.39 | 4.50 ± 6.15 | .243 |
| Assists per season | 1.82 ± 2.38 | 1.48 ± 2.18 | .478 |
| Yellow cards per season | 2.05 ± 2.09 | 2.17 ± 1.99 | .788 |
| Red cards per season | 0.26 ± 0.50 | 0.19 ± 0.48 | .488 |
| Fouls committed per season | 16.6 ± 13.5 | 18.7 ± 15.8 | .506 |
| Case Group (Year 2 After ACLR) | Control Group | P Value | |
| Games played per season | 20.2 ± 8.29 | 15.6 ± 9.81 | .008 |
| Minutes per game | 72.4 ± 20.1 | 64.6 ± 25.0 | .164 |
| Goals per season | 4.42 ± 8.11 | 1.42 ± 2.57 | .032 |
| Total shots per season | 23.6 ± 22.4 | 13.1 ± 19.3 | .014 |
| Shots on goal per season | 9.22 ± 10.3 | 5.55 ± 9.83 | .049 |
| Assists per season | 3.17 ± 2.67 | 1.61 ± 2.19 | .013 |
| Yellow cards per season | 2.91 ± 2.95 | 2.42 ± 2.13 | .253 |
| Red cards per season | 0.13 ± 0.34 | 0.21 ± 0.41 | .917 |
| Fouls committed per season | 21.4 ± 12.3 | 20.1 ± 19.0 | .377 |
| Case Group (Year 3 After ACLR) | Control Group | P Value | |
| Games played per season | 15.4 ± 7.65 | 18.3 ± 9.96 | .943 |
| Minutes per game | 77.2 ± 17.1 | 71.3 ± 22.7 | .473 |
| Goals per season | 2.71 ± 3.02 | 1.34 ± 1.72 | .053 |
| Total shots per season | 19.2 ± 14.0 | 15.6 ± 15.5 | .120 |
| Shots on goal per season | 8.47 ± 7.18 | 6.28 ± 7.18 | .123 |
| Assists per season | 3.13 ± 3.66 | 1.86 ± 2.01 | .094 |
| Yellow cards per season | 2.13 ± 2.20 | 3.00 ± 2.62 | .455 |
| Red cards per season | 0.33 ± 0.49 | 0.24 ± 0.44 | .686 |
| Fouls committed per season | 16.7 ± 10.6 | 22.4 ± 15.5 | .418 |
| Case Group (Year 4 After ACLR) | Control Group | P Value | |
| Games played per season | 19.2 ± 5.73 | 14.3 ± 7.58 | .088 |
| Minutes per game | 73.8 ± 16.6 | 71.6 ± 34.6 | .609 |
| Goals per season | 5.00 ± 11.4 | 1.26 ± 1.54 | .087 |
| Total shots per season | 14.7 ± 12.9 | 10.7 ± 9.42 | .139 |
| Shots on goal per season | 6.22 ± 5.74 | 4.27 ± 4.15 | .173 |
| Assists per season | 1.78 ± 1.39 | 1.27 ± 2.12 | .259 |
| Yellow cards per season | 2.56 ± 1.67 | 1.82 ± 1.47 | .131 |
| Red cards per season | 0.33 ± 0.50 | 0.23 ± 0.53 | .390 |
| Fouls committed per season | 23.2 ± 14.7 | 13.0 ± 7.72 | .012 |
| Case Group (Year 5 After ACLR) | Control Group | P Value (Paired Samples Student t Test) | |
| Games played per season | 16.3 ± 10.2 | 15.2 ± 10.1 | .704 |
| Minutes per game | 75.7 ± 15.9 | 64.3 ± 27.3 | .164 |
| Goals per season | 7.17 ± 15.6 | 1.00 ± 1.35 | .098 |
| Total shots per season | 10.8 ± 10.0 | 9.50 ± 10.1 | .406 |
| Shots on goal per season | 2.20 ± 2.68 | 3.50 ± 3.55 | .622 |
| Assists per season | 1.80 ± 1.64 | 0.75 ± 0.75 | .089 |
| Yellow cards per season | 2.00 ± 2.35 | 1.83 ± 2.98 | .990 |
| Red cards per season | 0.20 ± 0.45 | 0.25 ± 0.62 | .938 |
| Fouls committed per season | 15.0 ± 13.1 | 12.9 ± 11.0 | .518 |
aValues are expressed as mean ± standard deviation. Statistically significant differences had a P value < .0055. ACLR, anterior cruciate ligament reconstruction.
Footnotes
One or more of the authors has declared the following potential conflict of interest of source of funding: Dr Cole receives royalties from Arhtrex, DJO, Elsevier, Lippincott, and WB Saunders; is a member of the Genzyme speakers bureau; is a paid consultant for Zimmer, Arthrex, Carticept, Biomimetic, Allosource, and Depuy; receives research support from Regentis, Arthrex, Smith & Nephew, Linvatec, Ossur, DJO, Zimmer, Depuy, and Johnson and Johnson; is on medical publishing boards for JBJS, AJSM, Cartilage, JSES, AJO, and Elsevier; and is on the International Committee AANA, Education Committee AANA, and the AAOS Board. Dr Bach receives royalties from SLACK Inc and institutional research support from Arhtrex, Ossur, Linvatec, and Smith & Nephew. Dr Bush-Joseph receives institutional research support from Arthrex, Ossur, Linvatec, and Smith & Nephew.
References
- 1. Arendt EA, American Orthopaedic Society for Sports Medicine, American Academy of Orthopaedic Surgeons OKU Orthopaedic Knowledge Update. Sports Medicine 3. 3rd ed Rosemont, IL: American Academy of Orthopaedic Surgeons; 2004. [Google Scholar]
- 2. Brophy R, Silvers HJ, Gonzales T, Mandelbaum BR. Gender influences: the role of leg dominance in ACL injury among soccer players. Br J Sports Med. 2010;44:694–697. [DOI] [PubMed] [Google Scholar]
- 3. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40:2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J. Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy. 2009;25:825–830. [DOI] [PubMed] [Google Scholar]
- 5. DeHaven KE, Lintner DM. Athletic injuries: comparison by age, sport, and gender. Am J Sports Med. 1986;14:218–224. [DOI] [PubMed] [Google Scholar]
- 6. Dragoo JL, Braun HJ, Durham JL, Chen MR, Harris AH. Incidence and risk factors for injuries to the anterior cruciate ligament in National Collegiate Athletic Association football: data from the 2004-2005 through 2008-2009 National Collegiate Athletic Association Injury Surveillance System. Am J Sports Med. 2012;40:990–995. [DOI] [PubMed] [Google Scholar]
- 7. Ekstrand J. A 94% return to elite level football after ACL surgery: a proof of possibilities with optimal caretaking or a sign of knee abuse? Knee Surg Sports Traumatol Arthrosc. 2011;19:1–2. [DOI] [PubMed] [Google Scholar]
- 8. Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79:1556–1576. [DOI] [PubMed] [Google Scholar]
- 9. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. [DOI] [PubMed] [Google Scholar]
- 10. Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. [DOI] [PubMed] [Google Scholar]
- 11. Marrale J, Morrissey MC, Haddad FS. A literature review of autograft and allograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:690–704. [DOI] [PubMed] [Google Scholar]
- 12. McAllister DR, Tsai AM, Dragoo JL, et al. Knee function after anterior cruciate ligament injury in elite collegiate athletes. Am J Sports Med. 2003;31:560–563. [DOI] [PubMed] [Google Scholar]
- 13. Mitsou A, Vallianatos P. Reconstruction of the anterior cruciate ligament using a patellar tendon autograft. A long term follow up. Int Orthop. 1996;20:285–289. [DOI] [PubMed] [Google Scholar]
- 14. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 15. Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995;3:261–267. [DOI] [PubMed] [Google Scholar]
- 16. Samuelsson K, Andersson D, Karlsson J. Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy. 2009;25:1139–1174. [DOI] [PubMed] [Google Scholar]
- 17. Swenson DM, Collins CL, Best TM, Flanigan DC, Fields SK, Comstock RD. Epidemiology of knee injuries among US high school athletes, 2005/06-2010/11. Med Sci Sports Exerc. 2013;45:462–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Waldén M, Hagglund M, Magnusson H, Ekstrand J. Anterior cruciate ligament injury in elite football: a prospective three-cohort study. Knee Surg Sports Traumatol Arthrosc. 2011;19:11–19. [DOI] [PubMed] [Google Scholar]