Abstract
Background:
The optimal treatment of Hill-Sachs injuries is difficult to determine and is potentiated by the finding that a Hill-Sachs injury becomes more important in the setting of glenoid bone loss, making engagement of the humeral head on the glenoid inherently easier. The “glenoid track” concept was developed to biomechanically quantify the effects of a combined glenoid and humeral head bony defects on instability.
Purpose:
To clinically evaluate humeral head engagement on the glenoid by utilizing glenoid track measurements of both humeral head and glenoid bone loss.
Study Design:
Retrospective cohort.
Methods:
A total of 205 patients with recurrent anterior shoulder instability were evaluated, and of these, 140 patients (68%; 9 females [6%] and 131 males [94%]) with a Hill-Sachs lesion and a mean age of 27.6 years (range, 15-47 years; standard error of mean [SEM], 0.59) were included in the final magnetic resonance angiogram [MRA]) analysis. Bipolar bone loss measures of glenoid bone loss (sagittal oblique MRA) and multiple size measures of the Hill-Sachs injury (coronal, axial, and sagittal MRA) were recorded. Based on the extent of the bipolar lesion, patients were classified with glenoid track as either outside and engaging of the glenoid on the humeral head (OUT-E) or inside and nonengaging (IN-NE). The 2 groups were then compared with clinical evidence of engagement on examination under anesthesia (EUA) using video arthroscopy, number of dislocations, length of instability, and patient age.
Results:
The mean glenoid bone loss was 7.6% (range, 0%-29%; SEM, 1.20%), and 31 of 140 (22%) patients demonstrated clinical engagement on EUA. Radiographically, 19 (13.4%) patients were determined to be OUT-E, while 121 (86.6%) were IN-NE and not expected to engage. Of those 19 patients with suggested radiographic engagement (OUT-E), 16 (84.5%) had clinical evidence of engagement versus only 12.4% that clinically engaged (15/121) without radiographic evidence of engagement (IN-NE) (P < .001). Younger age and a greater number of recurrence events were jointly predictive of a patient being classified as OUT-E (11.8 vs 6.4 dislocations; P = .015).
Conclusion:
This study demonstrates that glenohumeral engagement was well predicted based on preoperative glenoid and humeral head bone loss measurements using the glenoid track method. In addition, younger age and a greater number of recurrences were predictive of engagement. The glenoid track concept may be important to fully assess the overall risk for engagement prior to surgery and may help guide surgical decision making such as bony augmentation procedures.
Keywords: Hill-Sachs lesion, glenoid bone loss, shoulder instability, glenohumeral engagement
The Hill-Sachs lesion is classically described as a compression fracture of the posterosuperolateral humeral head in association with anterior instability or dislocation of the glenohumeral joint. Joseph-François Malgaigne first documented this lesion in his 1855 thesis, and Eve7 expounded on it with the first case report and its association with a glenohumeral dislocation. It was radiographically described by Hill and Sachs as a line of condensation on the internal rotation shoulder radiograph and was attributed to the impression of the dense cortical glenoid on the humeral head during an anterior dislocation event.8 The incidence of Hill-Sachs lesions in anterior shoulder instability ranges from 38% to 88% and is associated with up to 100% of recurrent dislocations.3,8–10,19,24,28,33 Plain radiographs are useful for the initial identification of the humeral defect; a combination of internal rotation and Stryker notch views are 92% accurate.5,20 However, magnetic resonance imaging (MRI) is imperative for determining the exact location and extent of the lesion, as it has a 97% sensitivity and 91% specificity in the detection of Hill-Sachs lesions.31
Though the detection, location, and relationship of a Hill-Sachs lesion to anterior instability are well described, little is known about its prognostic implications or relationship to glenoid bone loss. The effect of a bony glenoid defect on the risk of recurrent instability after a Bankart repair has been well established.1 Burkhart et al1 found that defects involving over 25% of the glenoid width had unacceptably high failure rates, and Itoi et al used a cadaveric model to demonstrate that defects greater than 21% would fail without bone grafting.15 However, though many classification systems exist for Hill-Sachs lesions, the same prognostic and therapeutic parameters have not been clearly established for this defect.
It is intuitive that the instability due to a Hill-Sachs injury is potentiated in the setting of glenoid bone deficiency; however, this has not been verified clinically. Yamamoto et al32 conceptualized the “glenoid track” concept to biomechanically quantify the effects of combined glenoid and humeral head bony defects on instability in a cadaveric model. The optimal treatment of Hill-Sachs injuries is difficult to determine and is potentiated by the finding that a Hill-Sachs injury becomes more important in the setting of glenoid bone loss, making engagement of the humeral head on the glenoid inherently easier. It is thought to be important to determine if a Hill-Sachs lesion is at high risk of engaging the glenoid, thus changing potential treatment options.
Thus, the purpose of this study was to clinically evaluate humeral head engagement on the glenoid by utilizing glenoid track measurements of combined humeral head and glenoid bone injuries. Our null hypothesis was that there is no association between the glenoid track system and examination findings for engagement or other demographic factors in a patient population with recurrent anterior instability.
Materials and Methods
A total of 205 patients treated consecutively for recurrent anterior shoulder instability over a 2-year period (2006-2008) were reviewed. Of these, a total of 173 (80.8%) shoulders had an adequate shoulder magnetic resonance (MR) evaluation, and Hill-Sachs lesions were identified on 140 (80.9%). Therefore, a total of 140 patients (68% of the cohort) were included in the final radiographic analysis and grading of Hill-Sachs lesions, including 9 females (6%) and 131 males (94%) with a mean age of 27.6 years (range, 15-47 years; standard error of mean [SEM], 0.59), mean length of instability of 43.4 months (range, 0-360 months; SEM, 5.27), and a mean 7.2 dislocations (range, 0-100; SEM, 1.53). These demographics are comparable with other large anterior instability series, which include a preponderance of young males (20-30 years old, 81%-90% male).6,11,21 Prior to data collection, the study protocol was reviewed by the hospital institutional review board and approved as an exempt protocol (Table 1).
Table 1.
Patient Demographicsa
| Mean | Range | SEM | |
|---|---|---|---|
| Age, y | 27.6 | 15-47 | 0.59 |
| Length of instability, mo | 43.4 | 0-360 | 5.27 |
| Number of dislocations | 7.2 | 0-100 | 1.53 |
aSEM, standard error of mean.
Three independent examiners investigated all radiographic parameters and were blinded to patient demographic and clinical information. A sports fellowship–trained senior surgeon standardized the radiographic parameters and then instructed 3 orthopaedic residents on the technique for taking the measurements. These examiners then completed measurements on all patients independently. Measurements were based on the patient’s first MR evaluation (96% of patients had an MR angiogram [MRA] [n = 134] and 4% had an MRI [n = 6] with a shoulder coil and 1.5-T magnet; Siemens Healthcare, Munich, Germany) and were completed once by each examiner, who was blinded to the results of the other 2 investigators. All radiographic measurements were made using an IMPAX digital viewing system (Agfa Healthcare, Mortsel, Belgium). Distance measurements were made to the nearest tenth of a millimeter, and degree measurements were made to the nearest degree using digital measuring software provided with the system. A separate researcher collected patient demographic and clinical data based on a chart review.
Yamamoto et al32 developed a novel approach to describe Hill-Sachs lesions that was based on both the location and size of the humeral head defect as well as the amount of glenoid bone loss. They used a cadaveric model to study bipolar bone loss of the humeral head and glenoid concomitantly. The authors brought the cadaveric glenohumeral joint through a predetermined range of motion, measuring the distance of the articular contact area to the rotator cuff footprint, and noted that it was 84% the width of the glenoid (Figure 1), hence the concept of a “glenoid track.” It was postulated that a Hill-Sachs lesion outside this track was at high risk for engagement and thus recurrent instability.32 In this model, the location of the glenoid track on the humeral head is based solely on the glenoid width. Thus, the classification is intimately related to not only the location and size of the humeral defect but also the amount of glenoid bone loss. With increasing size of a bony Bankart lesion, the glenoid track decreases accordingly, potentiating the risk for engagement.
Figure 1.
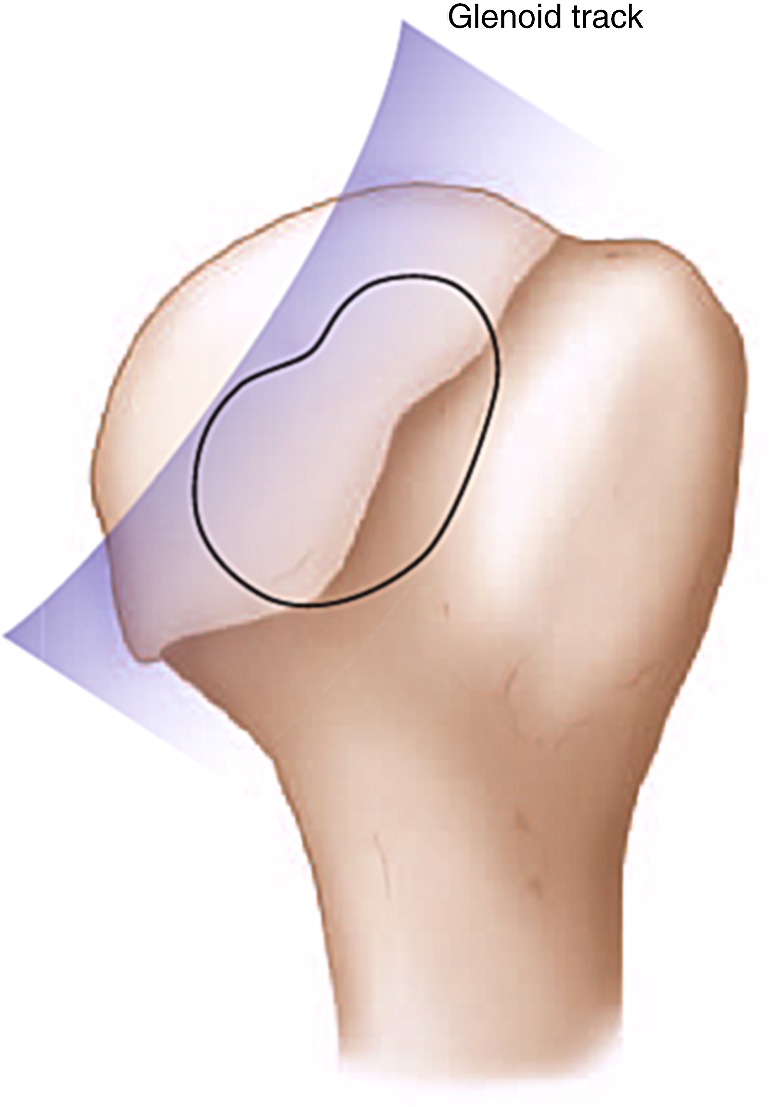
The glenoid track concept describes Hill-Sachs lesions based on both the location and size of the humeral head defect as well as the amount of glenoid bone loss. Using a cadaveric model, a zone of contact was measured between the glenoid rim and the humeral head. With the shoulder in 60° of abduction and maximum external rotation to simulate anterior apprehension, the distance from the contact area to the medial margin of the footprint was found to be 84% of the glenoid width. Reprinted with permission from Provencher and Romeo.22
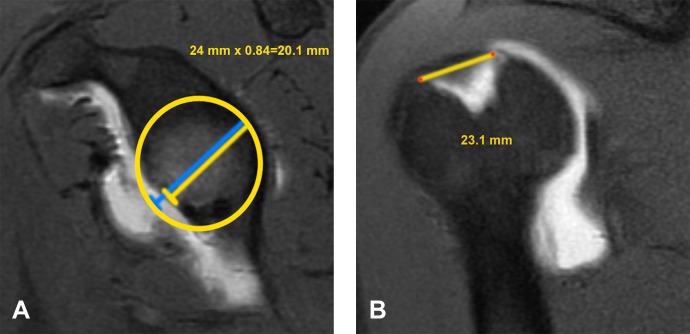
In the current study, the original glenoid track model was modified to quantify it based on MR images of patients. The glenoid width was measured based on the technique described by Huysmans et al,13 the bare spot was identified on a sagittal oblique MR image, and the glenoid width was measured using this central reference point. Then, to determine the expected glenoid width, a best-fit circle was placed on the inferior third of the glenoid centered on the bare spot and the diameter of the circle was measured to calculate the expected width prior to bone loss (Figure 2).12 Therefore, both percentage of glenoid bone loss and glenoid track were determined from these measurements. The glenoid track was calculated as 84% of the actual glenoid width, which was the expected glenoid width minus any bone loss.32
Figure 2.
(A) The glenoid track is calculated as 84% of the actual glenoid width measured on the sagittal oblique magnetic resonance (MR) image. A best-fit circle is placed on the glenoid to calculate the expected width prior to bone loss. Therefore, both percentage of bone loss and glenoid track can be determined. In this case, the actual glenoid width is 24 mm, with 4 mm of bone loss (17% bone loss). The glenoid track is 84% of 24 mm, or 20.1 mm. (B) The distance from the rotator cuff footprint to the medial margin of the Hill-Sachs lesion is measured on the coronal MR. In this case, it is 23.1 mm. Since the Hill-Sachs width to the footprint (23.1 mm) is greater than the glenoid track measurement (20.1 mm), it is considered outside the glenoid track and at high risk for engaging.
Based on prior methods, the distance from the medial margin of the rotator cuff footprint to the medial margin of the Hill-Sachs lesion was then measured in millimeters using the largest distance on a coronal cut.27 If this value was greater than the glenoid track, then the humeral head was said to be outside the glenoid track and at high risk for engaging (OUT-E). Otherwise, if combined glenoid and humeral bone loss was not greater than the track, it was considered inside the track and nonengaging (IN-NE). Each patient was then classified as OUT-E or IN-NE and the number (percentage) of patients in each group was recorded.
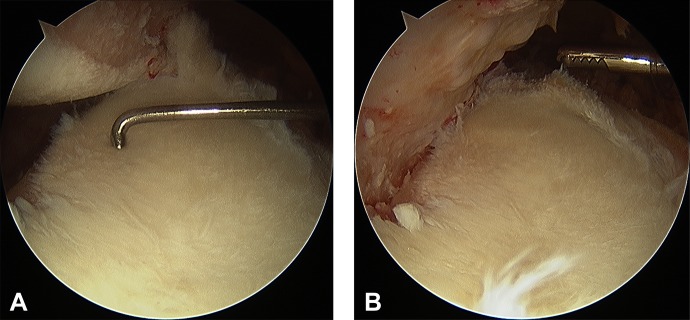
Clinical determination of “engagement” was made for each patient by reviewing the reported intraoperative examination findings and evaluating intraoperative video arthroscopy. A sports fellowship–trained senior surgeon performed the examination on each patient. In order for a lesion to be considered engaging, both portions of the examination had to be positive. First, the examination, completed under anesthesia, was performed based on the technique described by Burkhart et al1 to document any humeral head engagement with the shoulder in 90° of abduction and greater than 0° of external rotation with the patient in the lateral decubitus position. An attempt was made to dislocate the humeral head anterior to the glenoid based on a palpable clunk that required manual manipulation for reduction. In those shoulders that were thought to engage on this initial examination, engagement of the Hill-Sachs lesion was verified under initial diagnostic video arthroscopy before any fluid was introduced into the joint. The number of engaging shoulders in the outside (OUT-E) and inside (IN-NE) glenoid track groups was recorded (Figure 3).
Figure 3.
During standardized examination under anesthesia, as described by Burkhart et al,1 a palpable clunk was noted with the shoulder abducted to 90° and external rotation greater than 0°, as this large Hill-Sachs lesion engaged the anterior glenoid. The examination was verified arthroscopically. (A) The shoulder is abducted 45° and is brought into a few degrees of external rotation. It is close to engaging due to a large amount of anterior glenoid bone loss (28%). (B) The shoulder is brought into further external rotation and easily engages the glenoid.
For each of the 3 observers, the frequency of each categorical variable as well as the mean and SEM of each continuous variable were taken. Interobserver reliability between the 3 observers was then determined for each variable. Correlation coefficients were then calculated between independent variables, and multiple regression analysis was used to determine the relationship between patient demographic factors (age, length of instability, number of dislocations) and the glenoid track system.
Results
Of the 140 Hill-Sachs lesions, 19 (13.4%) were determined to be outside (OUT-E) the glenoid track and at higher risk of functional glenohumeral engagement; the remaining 121 (86.6%) were inside (IN-NE) the track. Interobserver reliability between the 3 observers was 0.43 (κ). Clinically, 16 of 19 (84.5%) lesions outside (OUT-E) the glenoid track engaged in a functional position when the shoulder was externally rotated in 90° of abduction versus only 15 of 121 (12.4%) inside (IN-NE) the glenoid track (P < .001). Furthermore, the mean distance from the footprint to the medial margin of the Hill-Sachs lesion on coronal MR was 22.1 mm (SEM, 1.12 mm) for the OUT-E group compared to 14.5 mm (SEM, 0.45 mm) for those in the IN-NE group (P < .001). Also, the mean glenoid bone loss was 13.7% (SEM, 1.74%) for those shoulders OUT-E versus 6.5% (SEM, 0.65%; P < .001) for those IN-NE (Table 2). For all patients, the mean glenoid bone loss was 2.2 mm or 7.6% of the glenoid width.
Table 2.
Glenoid Track Results
| Inside Track (IN) | Outside Track (OUT) | |
|---|---|---|
| Number of patients, n (%) | 121 (86.6) | 19 (13.4) |
| Glenoid track, mm | 22.2 | 20.2 |
| Percentage engaging, % | 12.4 | 84.5 |
| Mean Hill-Sachs size, mm | 14.5 | 22.1 |
| Mean glenoid bone loss, % | 6.5 | 13.7 |
| Mean number of dislocations | 6.4 | 11.8 |
From regression analysis, younger patient age and greater number of recurrent instability events were jointly predictive of being outside (OUT-E) the glenoid track (P = .015). The mean number of dislocations in this group was 11.8 (SEM, 5.48) versus 6.4 (SEM, 1.38) for those inside (IN-NE) the track.
Other findings from regression analysis included that number of dislocations was predictive of glenoid bone loss (P = .01), and more dislocations also correlated with larger Hill-Sachs lesions as well as larger extent of combined glenoid and humeral bone loss (P < .001). Length of instability also correlated with patient age and number of dislocations.
Discussion
The principal findings of this study demonstrated that approximately 13% of instability patients with a Hill-Sachs injury were felt to be at increased risk of glenohumeral engagement with bipolar bone loss calculations outside the glenoid track. This system correlated well with clinical findings during surgery, where 85% of these patients also demonstrated functional glenohumeral engagement during examination under anesthesia. Also, these patients had significantly greater glenoid bone loss than those with lesions within the glenoid track (14% vs 7%). This is the key to this classification system because it indicates that irrespective of total Hill-Sachs size, the likely most important factor for risk of engagement and recurrent instability is humeral lesion location related to the glenoid rim. This is defined by glenoid width, which is significantly affected by the amount of glenoid bone loss. Therefore, this study demonstrates the importance of viewing bone loss problems in the shoulder as a bipolar issue, where glenoid and humeral losses potentiate each other and increase the risk of recurrent instability. This is a principle that no prior grading system has taken into account. In addition, there is an association of the glenoid track with age and number of dislocations, which indicates that this classification system may have both prognostic and therapeutic value.
Yamamoto et al32 utilized a novel cadaveric model to map the rim of the glenoid in relation to the humeral head in various degrees of abduction. Thus, the glenoid track concept advanced the understanding of engagement and recurrent instability by not only including the humeral head deficiency but also defining it in relation to the glenoid width and bone loss. They were also able to verify their model in 3 patients with anterior instability using 3-dimensional reconstruction computed tomography (CT) images.32 However, to date, no other study has translated this concept to a large case series or correlated it to demographic or injury-specific factors. Thus, the current study applies the glenoid track classification to a clinical model using MRA and verifies its usefulness as a potential prognostic tool.
Prior studies have characterized the typical orientation of a Hill-Sachs lesion based on the position of the humeral head on the glenoid during the dislocation event and differentiated its location from the bare spot based on the correlation of a cadaveric model to MR imaging.1,23 Therefore, though there have been prior discussions of Hill-Sachs engagement based on orientation, with the arm in a functional position of external rotation and abduction, none of these studies looked at their findings in relation to glenoid bone loss or, more importantly, with regard to clinical outcomes.18
Other studies have attempted to identify an association between the risk of recurrent shoulder instability and severity of Hill-Sachs lesion. A number of studies have looked at factors associated with failed anterior stabilization procedures and have included Hill-Sachs lesion size as a potential cause. A few of these graded Hill-Sachs lesions based on Rowe grade, and none found a significant association between grade and risk for recurrent instability.24,26,29 Therefore, even though some prior Hill-Sachs grading schemes may correlate highly with each other, they are potentially of limited value to the clinician.
If a lesion is noted to be outside the glenoid track and therefore at increased risk for instability, there are a number of potential surgical treatment options that utilize the principles of this concept. One can augment anterior glenoid bone loss with a Latarjet procedure or an iliac crest bone graft to, in effect, increase the glenoid track size and prevent engagement.1,2,4,16 Another treatment strategy is to shift the glenoid track so that it contains the entire Hill-Sachs lesion and thus prevents engagement. This can be accomplished using a rotational humeral osteotomy or by tightening the anterior soft tissue structures to limit external rotation and shift the glenoid track medially and superiorly.17,24,25,30
There were a number of limitations to this study. First, the original glenoid track study utilized direct measurements with a caliper and correlated the cadaveric model to 3-dimensional CT images in live patients. In the current study, these images were not available for all patients; therefore, the classification was adapted to MRA using coronal images for the footprint to lesion measurement and sagittal oblique images to measure glenoid width for glenoid track calculations. However, these measurements have been well validated in prior bone loss models.23,31 In this group of patients, MRA was available for most patients and has been shown to be a precise method of measuring glenoid and humeral-sided bone loss.12 In addition, we feel that MRA is superior for measuring the distance from the Hill-Sachs lesion to the rotator cuff footprint, given that the footprint is a soft tissue structure that is more precisely identified using this modality than CT. Another limitation was the study design as a retrospective case series. The retrospective nature of the study was a potential source of bias, in particular, selection bias. However, all consecutive patients within a 2-year period were included in the study, and the inclusion rate was over 80% for all instability patients in this time period. Video arthroscopy was reviewed to determine engagement through the functional range of motion. Also, a control group was not available against which to compare data because there were too few patients who lacked Hill-Sachs lesions. In addition, there was no gold standard against which to compare the results. Finally, the majority of patients in this cohort were males; therefore, extrapolation of these results to female patients should be done with caution. However, this cohort is consistent with other studies where patients with anterior instability are predominately young males.6,11,21 In addition, although an intraoperative examination was completed for each patient, it did not take into account soft tissue restraints prior to surgical repair and was not repeated after repair to evaluate for a difference. Also, the examination was not standardized with regard to the amount of force applied or the degree of external rotation required to dislocate the shoulder. Finally, this study was a preliminary report that did not evaluate the glenoid track system in terms of outcomes. This study did not attempt to record the method of treatment or correlate group designation, with failure rates based on the surgical method. Further investigation will be required to determine the optimal treatment for these patients.
Conclusion
In this study, a radiographic review was performed of 140 patients with shoulder instability and associated Hill-Sachs lesions. The glenoid track was measured using MRA images, and large bipolar humeral and glenoid lesions were considered outside the glenoid track while smaller lesions were classified as inside the track. A total of 13.4% of the patients were determined to be outside the glenoid track, and a high percentage of these patients (84.5%) had functionally engaging lesions identified during examination under anesthesia.
These findings indicate that preoperative glenoid and humeral bone loss measurements can be effectively used to predict the risk for glenohumeral engagement and potentially be indicative of future instability. This may be helpful for surgical decision making, particularly when considering bony augmentation procedures.
The glenoid track is a new classification system that can be utilized to assess the risk of engagement of a Hill-Sachs lesion in a patient with anterior shoulder instability, and this article provides the first important data about how to apply the glenoid track concept clinically. Hill-Sachs injuries are common in shoulder instability, and one should look closely at the extent of glenoid bone loss in addition to the size of the Hill-Sachs lesion to more completely assess the potential for glenohumeral engagement, as this is a bipolar problem. Additional prospective data are necessary to determine the prognostic value of Hill-Sachs grading scores and the glenoid track concept.
Footnotes
One of more of the authors has declared the following potential conflict of interest or source of funding: Dr Solomon has received honoraria from Arthrex and Pacific Media for education presentations, and Dr Provencher is the deputy editor of Arthroscopy.
References
- 1. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS, De Beer JF, Barth JR, Cresswell T, Roberts C, Richards DP. Results of modified Latarjet reconstruction in patients with anteroinferior instability and significant bone loss. Arthroscopy. 2007;23:1033–1041. [DOI] [PubMed] [Google Scholar]
- 3. Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy. 1989;5:254–257. [DOI] [PubMed] [Google Scholar]
- 4. Chen AL, Hunt SA, Hawkins RJ, Zuckerman JD. Management of bone loss associated with recurrent anterior glenohumeral instability. Am J Sports Med. 2005;33:912–925. [DOI] [PubMed] [Google Scholar]
- 5. Danzig LA, Greenway G, Resnick D. The Hill-Sachs lesion. An experimental study. Am J Sports Med. 1980;8:328–332. [DOI] [PubMed] [Google Scholar]
- 6. Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19:732–739. [DOI] [PubMed] [Google Scholar]
- 7. Eve F. A case of subcoracoid dislocation of the humerus with the formation of an indentation on the posterior surface of the head. Medico-Chir Trans. 1880;63:317–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hill H. The groove defect of the humeral head. A frequently unrecognized complication of dislocations of the shoulder joint. Radiology. 1940;35:690–700. [Google Scholar]
- 9. Hintermann B, Gächter A. Arthroscopic findings after shoulder dislocation. Am J Sports Med. 1995;23:545–551. [DOI] [PubMed] [Google Scholar]
- 10. Hovelius L. Anterior dislocation of the shoulder in teen-agers and young adults. Five-year prognosis. J Bone Joint Surg Am. 1987;69:393–399. [PubMed] [Google Scholar]
- 11. Hovelius L, Sandström B, Sundgren K, Saebö M. One hundred eighteen Bristow-Latarjet repairs for recurrent anterior dislocation of the shoulder prospectively followed for fifteen years: study I—clinical results. J Shoulder Elbow Surg. 2004;13:509–516. [DOI] [PubMed] [Google Scholar]
- 12. Huijsmans PE, Haen PS, Kidd M, Dhert WJ, van der Hulst VP, Willems WJ. Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: a cadaveric study. J Shoulder Elbow Surg. 2007;16:803–809. [DOI] [PubMed] [Google Scholar]
- 13. Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW. The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg. 2006;15:759–763. [DOI] [PubMed] [Google Scholar]
- 14. Ito H, Takayama A, Shirai Y. Radiographic evaluation of the Hill-Sachs lesion in patients with recurrent anterior shoulder instability. J Shoulder Elbow Surg. 2000;9:495–497. [DOI] [PubMed] [Google Scholar]
- 15. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. [DOI] [PubMed] [Google Scholar]
- 16. Lynch JR, Clinton JM, Dewing CB, Warme WJ, Matsen FA., 3rd Treatment of osseous defects associated with anterior shoulder instability. J Shoulder Elbow Surg. 2009;18:317–328. [DOI] [PubMed] [Google Scholar]
- 17. Osmond-Clarke H. Habitual dislocation of the shoulder; the Putti-Platt operation. J Bone Joint Surg Am. 1948;30B:19–25. [PubMed] [Google Scholar]
- 18. Pagnani MJ. Open capsular repair without bone block for recurrent anterior shoulder instability in patients with and without bony defects of the glenoid and/or humeral head. Am J Sports Med. 2008;36:1805–1812. [DOI] [PubMed] [Google Scholar]
- 19. Palmer I, Widen A. The bone block method for recurrent dislocation of the shoulder joint. J Bone Joint Surg Am. 1948;30B:53–58. [PubMed] [Google Scholar]
- 20. Pavlov H, Warren RF, Weiss CB, Jr, Dines DM. The roentgenographic evaluation of anterior shoulder instability. Clin Orthop Relat Res. 1985;(194):153–158. [PubMed] [Google Scholar]
- 21. Porcellini G, Paladini P, Campi F, Paganelli M. Long-term outcome of acute versus chronic bony Bankart lesions managed arthroscopically. Am J Sports Med. 2007;35:2067–2072. [DOI] [PubMed] [Google Scholar]
- 22. Provencher MT, Romeo AA. Shoulder Instability: A Comprehensive Approach. Philadelphia, PA: Saunders; 2012. [Google Scholar]
- 23. Richards RD, Sartoris DJ, Pathria MN, Resnick D. Hill-Sachs lesion and normal humeral groove: MR imaging features allowing their differentiation. Radiology. 1994;190:665–668. [DOI] [PubMed] [Google Scholar]
- 24. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 25. Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63:863–872. [PubMed] [Google Scholar]
- 26. Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am. 1984;66:159–168. [PubMed] [Google Scholar]
- 27. Saito H, Itoi E, Minagawa H, Yamamoto N, Tuoheti Y, Seki N. Location of the Hill-Sachs lesion in shoulders with recurrent anterior dislocation. Arch Orthop Trauma Surg. 2009;129:1327–1334. [DOI] [PubMed] [Google Scholar]
- 28. Soslowsky LJ, Flatow EL, Bigliani LU, Pawluk RJ, Ateshian GA, Mow VC. Quantitation of in situ contact areas at the glenohumeral joint: a biomechanical study. J Orthop Res. 1992;10:524–534. [DOI] [PubMed] [Google Scholar]
- 29. Ungersböck A, Michel M, Hertel R. Factors influencing the results of a modified Bankart procedure. J Shoulder Elbow Surg. 1995;4:365–369. [DOI] [PubMed] [Google Scholar]
- 30. Weber BG, Simpson LA, Hardegger F. Rotational humeral osteotomy for recurrent anterior dislocation of the shoulder associated with a large Hill-Sachs lesion. J Bone Joint Surg Am. 1984;66:1443–1450. [PubMed] [Google Scholar]
- 31. Workman TL, Burkhard TK, Resnick D, et al. Hill-Sachs lesion: comparison of detection with MR imaging, radiography, and arthroscopy. Radiology. 1992;185:847–852. [DOI] [PubMed] [Google Scholar]
- 32. Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16:649–656. [DOI] [PubMed] [Google Scholar]
- 33. Yiannakopoulos CK, Mataragas E, Antonogiannakis E. A comparison of the spectrum of intra-articular lesions in acute and chronic anterior shoulder instability. Arthroscopy. 2007;23:985–990. [DOI] [PubMed] [Google Scholar]