Abstract
Background:
Medial patellofemoral ligament (MPFL) reconstruction in adults often utilizes screw fixation in the distal femur. The aim was to define the safety of similar fixation in young patients, with respect to their open physis.
Purpose:
To define the age-related relationship between the femoral insertion of the MPFL and the medial aspect of the distal femoral physis on magnetic resonance imaging (MRI) scans. The study investigates whether screw fixation at this point is safe with respect to patient age and screw inclination.
Study Design:
Cross-sectional study.
Methods:
Retrospective review of the MRI scans of 159 skeletally immature patients. The femoral insertion of the MPFL was defined with respect to the distal femoral physis. The predicted paths of 2-cm screw fixation were simulated both parallel to the joint line and 45° distally oblique; physeal and joint penetration were noted when present. Results are plotted against age and compared as quartile ranges.
Results:
The femoral insertion of the MPFL was found to be distal to the distal femoral physis in all patients by an average of 10 mm (range, 2-16 mm). The mean distance increases slightly with age in a nonlinear relationship (r = 0.51, P < .001) from 9 mm at age 10 years to 12 mm by age 16 years. For the classic, parallel screw, the risk of physeal breach is high for all age groups (mean, 64%). For the novel, oblique screw, joint penetration and physeal breach were less prevalent (mean, 13%), and importantly, the vast majority of these breaches were in younger children (age <9 years 9 months). With oblique screws, older children were at significantly lower risk than younger children (<3% vs 48%; P < .001).
Conclusion:
This study accurately defines the relationship between the femoral insertion of the MPFL and the distal femoral physis in children and adolescents. A high risk of potentially poor outcomes was found during anatomic reconstruction of the MPFL in children utilizing classic (parallel) screw fixation, irrespective of age. However, in children older than 10 years, a 20-mm screw, from the anatomic MPFL insertion and directed 45° distally oblique, should be safe in 98% of patients.
Keywords: MPFL, MRI, adolescent, children, physis, reconstruction
Patellar dislocation is relatively common, accounting for up to 16% of acute knee trauma in young athletes with hemarthrosis.12 The medial patellofemoral ligament (MPFL) is the primary medial soft tissue restraint preventing lateral displacement of the patella in the normal knee.3 Following patellar dislocation, injury to the MPFL may predispose to recurrent instability; hence, current surgical management of these patients often includes reconstruction of the incompetent MPFL.4
Adult MPFL reconstructions often utilize screw fixation in the distal femur. In the skeletally immature patient, consideration must be given to the proximity of this screw to the distal femoral physis. Concern regarding physeal injury in children has led to reconstructions using soft tissue fixation at nonanatomic sites.4 Although not yet confirmed in a pediatric population, authors in the adult reconstruction literature stress that replication of the anatomic insertion site of the MPFL is important for successful clinical outcomes.1
The purpose of this study was to define the relationship between the femoral insertion of the MPFL and the medial aspect of the distal femoral physis with respect to age. We then determined whether proposed femoral screw fixation at the anatomic site of MPFL insertion would be safe with respect to physeal and joint penetration. Finally, we wanted to evaluate the safety of a novel screw inclination 45° distally oblique to the plane of the joint.
Materials and Methods
This was an observational cross-sectional study based on a retrospective review of magnetic resonance imaging (MRI) scans. The electronic Picture Archiving and Communication System (PACS; Carestream, Rochester, NY, USA) was used to identify patients who underwent knee MRI at the Mater Children’s Hospital, Brisbane, Australia. The inclusion criteria were an available MRI of the knee with the patient being younger than 16 years. Exclusion criteria included documented injury to the medial retinaculum or medial femoral condyle, previous surgical treatment, or significant congenital structural abnormality. Further exclusion criteria included the lack of both axial and coronal plane imaging or imaging not adequate to confidently define the femoral insertion of the MPFL. Only 1 study per patient was included. A total of 159 patients were included, of which 93 were male (mean age, 11 years; range, 3-16 years). MRIs were obtained in 0° degrees of knee extension, using standardized knee protocols.
Kepler et al7 demonstrated that the MPFL originates at the superomedial aspect of the patella and inserts on the femur distal and anterior to the adductor tubercle. Dirim et al5 confirmed on both radiology and histology that the femoral insertion of the MPFL blends with the origin on the medial collateral ligament in the second medial layer of the knee. We used this knowledge to accurately identify the MPFL insertion on sequential axial MRI scans (Figure 1). We then cross-referenced this axial postion with the coronal images using the PACS software. A line was drawn through the cortical margins of the distal femoral physis, and the perpendicular distance from this line to the MPFL insertion was measured (Figure 1).
Figure 1.
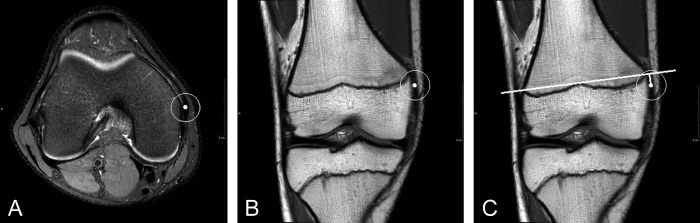
Measuring the MPFL-to-physis distance. (A) The femoral insertion of the MPFL is identified on axial T2 images as it merges with MCL origin. (B) The position is then cross-referenced onto coronal T1 images. (C) The perpendicular distance between a line through the cortical margins of the distal femoral physis and the MPFL insertion is then measured. MPFL, medial patellofemoral ligament; MCL, medial collateral ligament.
A line was drawn through the most distal aspect of the medial and lateral femoral condyles, and a second line was drawn parallel to this but through the MPFL insertion point (Figure 2). The projected path of a fixation screw (20 mm in length) was then drawn from the MPFL insertion point. The classic screw path was drawn along a parallel line. Our novel screw path was then drawn 45° distally oblique to the parallel line (Figure 2). If the projected screw crossed the physis, a physeal breach was recorded. Similarly, if the projected screw crossed the bony cortex of the medial femoral condyle or the intercondylar notch, joint penetration was recorded.
Figure 2.
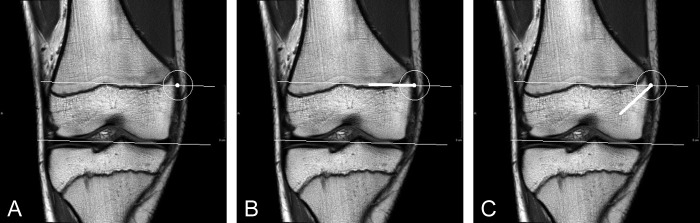
Projected screw paths. (A) The distal aspect of the femoral condyle is marked, and a parallel line was drawn through the medial patellofemoral ligament (MPFL) insertion point. (B) The classic screw path is drawn along the parallel line, while (C) the novel screw path is drawn 45° distally oblique.
Statistical Analysis
All measurements were performed by a single radiologist; reliability was confirmed by parallel analysis of a randomly selected subgroup by a second independent radiologist. The data set was divided into equal-numbered quartiles to allow valid comparisons to be drawn. The maximum age cutoffs for each quartile were 9 years 9 months, 12 years 1 month, 13 years 5 months, and 16 years. Statistical analysis used the McNemar test for nonparametric binomial data (χ2) and Pearson correlation coeffecients (r). Nonlinear regression analysis was used when needed, and probability values (P) were calculated with P < .05 used to determine significance.
Results
The femoral insertion of the MPFL was found to be distal to the distal femoral physis in all patients by a mean distance of 10 mm (range, 2-16 mm). The mean distance between the femoral insertion of the MPFL and the distal femoral physis increased slightly with age from 9 mm at 10 years to 12 mm at 16 years (Figure 3). It follows a nonlinear relationship (r = 0.51, P < .001), which approximates to 0.6 mm per year in older children. There was no significant effect for sex other than the expected earlier physeal closure in girls.
Figure 3.
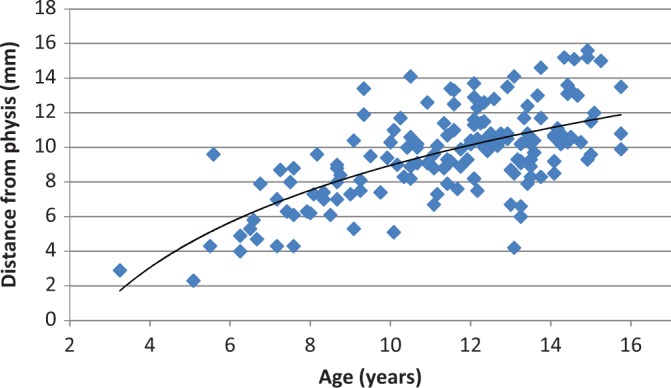
Age-related increase. Plot of age versus distance from the femoral insertion of the medial patellofemoral ligament (MPFL) to the distal femoral physis.
For the classic, parallel screw, the risk of physeal breach was high (50% to 77%) in all groups (mean, 64%) and significantly increased with increasing age (χ2 = 9.8, P < .05) (Figure 4). For the novel 45° distally oblique screw, either joint penetration or physeal breach occurred in 13% of patients. Quartile ranges revealed children in the first quartile (<9 years 9 months of age) were at a much higher risk than older children (48% vs <3%; χ2 = 55, P < .001).
Figure 4.
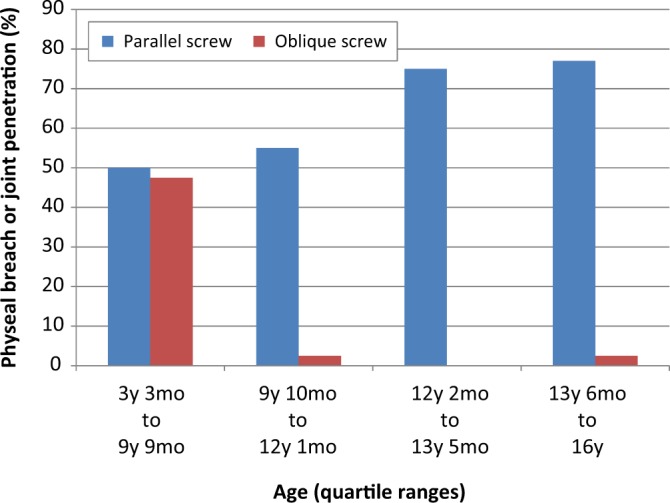
Risk of physeal breach or joint penetration by age quartiles and screw direction. Note that parallel screws pose significant risk at all ages, while oblique screws appear significantly safer in all but the youngest children.
While similar risks occur in younger children, a dramatic difference between parallel screws (46%) and oblique screws (2%) in children older than 10 years is evident (Figure 5).
Figure 5.
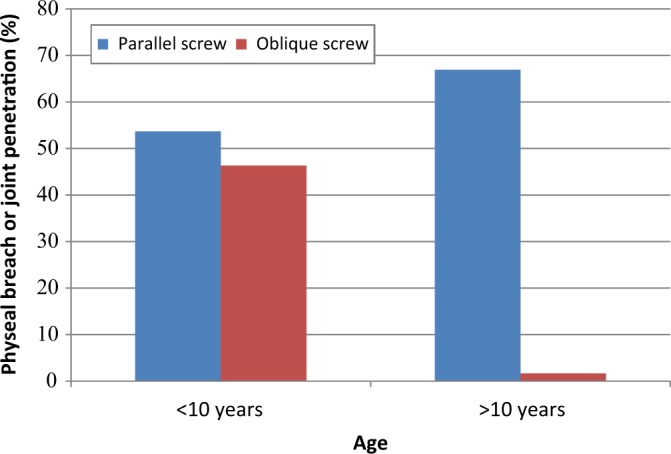
Risk of physeal breach or joint penetration by age and screw direction. All ages are at risk from parallel screws. Distally oblique screws are safe in children older than 10 years (<2%) but still carry significant risk in children younger than 10 years (46%).
Discussion
Several recent studies have attempted to characterize the relationship between the MPFL insertion and the distal femoral physis. Schoettle et al11 and Redfern et al10 described adult radiographic landmarks used to determine the position of the MPFL insertion intraoperatively. Nelitz et al9 defined the MPFL to physis relationship using those same radiological landmarks in children and adolescents. They recognized that the physis sweeps proximally (by an average of 9 mm) at the medial cortex. While the MPFL insertion appeared 3 mm proximal to the physis on lateral radiographs, the medial physeal sweep resulted in the true MPFL insertion being 6 mm distal to the physis. Kepler et al7 found the MPFL insertion to be distal to the physis in 86% of cases by an average of 5 mm based on their MRI study of 43 adolescents.
Our study confirmed this relationship and found a statistically significant increase in the MPFL-to-physis distance (approximately 0.6 mm per year) with advancing age. These findings were consistent with Ladd et al,8 who postulated that the change in distance likely reflects the nominal growth of the proximal portion of the femoral epiphysis during development.
Our study has also revealed that a standard surgical technique6 carries with it a high risk of physeal breach (64%) in both children and adolescents. While the 2-cm screw safely begins distal to the MPFL, the distally convex nature of the physis leads to a high probability of physeal breach deep to the surface.
Failure to restore the anatomic femoral insertion is a main risk factor for failure of MPFL reconstruction.2 This, in conjunction with the high variability in the convexity of the distal femoral physis, means that simply adjusting the entry point of the parallel screw more distally is not an adequate solution to the risk of physeal injury. Our alternative recommendation is to direct the screw 45° distally oblique. Our study shows that this technique represents a significantly safer alternative, with the risk of physeal breach all but mitigated. Although oblique screws carry a risk of joint penetration, we found this was very unlikely in older children (<2% of patients older than 10 years).
As this is an observational cross-sectional study and not a longitudinal study, we were not able monitor the change in MPFL-to-physis distance over time within individuals. Also, we did not take into account the skeletal age of the patient, only their chronological age. Further limitations of this study include not allowing for the width of the fixation screw; however, similar joint penetration and physeal breach risks would be expected from a more complex model. Typical fixation screws in adolescents are 6 mm wide (3 mm radius), which leaves 7 to 9 mm between the screw entry point and physis. Careful surgical dissection around the superficial border of the physis is unlikely to cause significant physeal injury, so the 7- to 9-mm distance provides for an adequate “safe zone” for screw insertion. Finally, we acknowledge that we did not investigate the effect of oblique screw placement on graft fixation, as this was not a biomechanical study. Experience gained from anterior cruciate ligament reconstruction would suggest that screws can be almost parallel to their reconstructed ligaments without compromising interference screw fixation clinically.
Conclusion
We believe our study has helped confirm that the MPFL-to-physis distance does change during skeletal development and has helped to quantify this change. More important, our study demonstrates that there is a significant risk of physeal breach (64%) during MPFL reconstruction, if using the classic method of screw fixation in the distal femur parallel to the knee joint. We feel directing the screw 45° distally oblique is a safer alternative in children older than 10 years (<2%). As no single method is completely safe in all cases, assessment of routine preoperative MRI imaging and confirmation with intraoperative fluoroscopy is recommended.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bollier M, Fulkerson J, Cosgarea A, Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy. 2011;8:1153–1159. [DOI] [PubMed] [Google Scholar]
- 2. Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38:2248–2254. [DOI] [PubMed] [Google Scholar]
- 3. Conlan T, Garth WP, Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682–693. [DOI] [PubMed] [Google Scholar]
- 4. Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstructions of the medial patellofemoral ligament of the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85:887–890. [PubMed] [Google Scholar]
- 5. Dirim B, Haghighi P, Trudell D, Portes G, Resnick D. Medial patellofemoral ligament: cadaveric investigation of anatomy with MRI, MR arthrography, and histologic correlation. AJR Am J Roentgenol. 2008;191:490–498. [DOI] [PubMed] [Google Scholar]
- 6. Fithian D, Khan N. Medial patellofemoral ligament reconstruction. Oper Tech Sports Med. 2010;18:93–97. [DOI] [PubMed] [Google Scholar]
- 7. Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW. Zone of injury of the medial patello-femoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444–1449. [DOI] [PubMed] [Google Scholar]
- 8. Ladd PE, Laor T, Emery KH, Salisbury SR, Parikh SN. Medial collateral ligament of the knee on magnetic resonance imaging: does the site of the femoral origin change at different patient ages in children and young adults? J Pediatr Orthop. 2010;30:224–230. [DOI] [PubMed] [Google Scholar]
- 9. Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19:2067–2071. [DOI] [PubMed] [Google Scholar]
- 10. Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38:293–297. [DOI] [PubMed] [Google Scholar]
- 11. Schoettle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. [DOI] [PubMed] [Google Scholar]
- 12. Zaidi A, Babyn P, Astori I, White L, Doria A, Cole W. MRI of traumatic patellar dislocation in children. Pediatr Radiol. 2006;36:1163–1170. [DOI] [PubMed] [Google Scholar]


