Abstract
Background:
Platelet-rich plasma (PRP) injections have been proposed to hasten soft tissue healing. There is a lack of evidence in the current literature to support their efficacy in elite athletes.
Purpose:
To investigate the effects of the addition of PRP to rehabilitation in the treatment of acute hamstring injuries in professional National Football League (NFL) players and to report the time to return to play.
Study Design:
Case control study.
Methods:
Ten NFL players with similar hamstring injury patterns were retrospectively divided into 2 groups. The treatment group (PRP; n = 5) was injected with PRP and the control group (non-PRP; n = 5) was not injected; both groups completed a rehabilitation program. The PRP injections were administered under ultrasound guidance with precise localization of the injury site, within 24 to 48 hours of injury. Age, muscle involved, extent of injury, grading, and time to return to play were noted. Descriptive statistics and the exact Wilcoxon rank-sum test were used for data analysis.
Results:
The mean age was 23 years (range, 22-27 years) for the PRP group and 26 years (range, 22-28 years) for the non-PRP group (P = .42). The median longitudinal extent of the injury was 14 cm (range, 9-18 cm) in the PRP group and 15 cm (range, 9-16 cm) in the non-PRP group (P = .77). The average transverse extent of the injury in the PRP and non-PRP groups was 4 cm (range, 1.6-6 cm) and 3.5 cm (range, 2-5 cm), respectively, and the respective average anteroposterior extent was 4 cm (range, 1.9-5 cm) and 2.9 cm (range, 1.5-4 cm). The long head of biceps femoris was most commonly involved (4 in each group), with a single tear of the semimembranosus in each group. The median injury classification was grade 2 in both groups. The median time to return to play was 20 days (range,16-30 days) in the PRP group and 17 days (range, 8-81 days) in the non-PRP group (P = .73).
Conclusion:
There were no significant differences in recovery from hamstring injury between treatment with PRP and routine rehabilitation. A larger, randomized controlled trial is warranted.
Keywords: hamstring injury, platelet-rich plasma, return to play, professional football
Hamstring injuries are prevalent in many sports that require high-speed running, acceleration, deceleration, and quick changes in direction.3,5,19 There is concern that significant time might be missed from play due to the occurrence of these injuries. In the United States, hamstring strain injuries accounted for 2.2 injuries/1000 athlete exposures (AEs) in training camps of the National Football League (NFL), from 1998 through 2007.9 It was the second most common injury seen during that time period and the most severe type of muscle strain.9 Authors have reported that 16% to 31% of all hamstring injuries are recurrent problems.1,2
Recently, platelet-rich plasma (PRP) has become a “hot topic” among clinicians who care for competitive athletes.20 As the excitement surrounding PRP has grown, so have the number of its proposed uses in the treatment of musculoskeletal disorders. It has been suggested as a primary or adjunctive treatment for acute tendon rupture,4,8,22 articular cartilage injury,11 ligament sprains,22 resistant fractures,12 osteoarthritis,23 muscle strains,13 and chronic tendinopathy.19
In 2006, Mishra and Pavelko18 published a seminal study on the use of PRP to promote healing in resistant tendinosis of the elbow. Sánchez et al22 reported the treatment of 6 athletes in whom a calcium chloride–activated platelet-rich fibrin matrix or plasma rich in growth factors (PRGFs) was used as an adjunct to Achilles tendon repair in comparison with a matched historical control group of 6 athletes who underwent Achilles repair alone. Although the study was not blinded, the PRGF group recovered more rapidly than did the comparison group, returning both to gentle running and subsequently to training, an average of 7 weeks sooner. However, there are no randomized controlled human studies regarding the use of PRP for muscle injuries.
Despite the rising attention given to PRP, the current literature still lacks evidence on its clinical effectiveness in the treatment of hamstring injuries, especially in professional athletes. This study aims to report the clinical effects of PRP and time to return to play following hamstring injuries in NFL players.
METHODS
This was a retrospective, case control study approved by our institutional review board (IRB). The data were collected from chart reviews, and documentation was done by the team physician during serial physical examinations over a single season. Ten professional football players from a single NFL team with grade 1 and 2 injuries were included. Players with a history of recurrent injury or previous injury within the last year were excluded from the study.
The players with hamstring injuries were divided into treatment and control groups, with 5 patients in each group. The treatment group received PRP injection along with routine rehabilitation for a hamstring injury, and the control group had rehabilitation alone. The 2 groups were matched for age, hamstring injury grade documented on magnetic resonance imaging (MRI), and medical comorbidities. All players underwent MRI within 24 to 48 hours of injury. The extent of the hamstring injury, grading of injury, muscle involved, age, position of the player, time to return to play (in days), and complications from PRP injection were documented. The grading of hamstring injury on the basis of MRI was done per the grading system described by Rettig et al.21 Both groups of patients followed the same rehabilitation protocol (Table 1) and were taken through a functional progression (Table 2) with a team athletic trainer prior to returning to play.
Table 1.
Rehabilitation Protocol for Grade 2 Hamstring Injuries
| Days 1-4 | |
| HIVAMAT (Physiomed Elektromedizin AG, Germany) | |
| Light soft tissue massage | |
| Active hamstring stretch in a supine 90/90 position | |
| Standing leg curls | |
| Prone hip extension | |
| Clam shell | |
| Ice and electrical stimulation | |
| Days 4-7 | |
| Pulsed ultrasound | |
| Soft tissue massage/trigger point release | |
| Check hip alignment | |
| Active/light passive hamstring stretch | |
| Stool scoots | |
| Tubing hamstring curls focusing on the negative | |
| Tubing hip extension | |
| Double-leg bridge with core focus | |
| Bike | |
| HIVAMAT (Physiomed Elektromedizin AG) | |
| Ice | |
| Days 7-14 | |
| Ultrasound/jacuzzi | |
| Soft tissue massage/foam roller | |
| Check hip alignment | |
| Passive stretch | |
| Weighted leg curls still focusing on the negatives | |
| Slide board lunges | |
| Single-leg Romanian dead lifts | |
| Swiss ball bridges with progression to curls | |
| Elliptical/stairstepper progression to treadmill (follow progression guidelines) | |
| Contrast bath/HIVAMAT (Physiomed Elektromedizin AG) | |
| Days 14-21 | |
| Continue with week 3 progression of strength | |
| Return to field program | |
| Post-exercise recovery |
Table 2.
Functional Progression for Hamstring Injuries
| Phase 1 | |
| Stairstepper/elliptical progression | |
| a) Stairstepper/elliptical 20-30 min | |
| b) 2 consecutive days without setbacks, progress to phase 2 | |
| Phase 2 | |
| Treadmill progression (15-30 min) | |
| a) Treadmill warm-up (3-6 mph) | |
| b) Progressive speed intervals (7-14 mph), increase in 0.5-mph increments 20 s run/20 s rest (7-10 mph), 10 s run/15 s rest (10-14 mph) | |
| c) If a player has apprehension or pain before 14 mph, work on a 1 min walking/1 min jogging program. Choose a comfortable speed between 7-10 mph and have the player jog 1 min and walk 1 min at 3.5 mph. | |
| d) If player completes 14 mph without hesitation and jog/run for an additional 15 min with 1 min/1 min then progress to phase 3. | |
| Phase 3 | |
| Field functional progression | |
| a) Jog 50 yards × 4 | |
| b) Dynamics/stretching | |
| c) High knees 10 yards × 4 | |
| d) Butt kicks 10 yards × 4 | |
| e) A skips 10 yards × 4 | |
| f) B skips 10 yards × 4 | |
| g) Back pedal 5 yards × 4 | |
| h) Lateral shuffle 10 yards both directions × 2 | |
| i) Cariocas both directions × 2 | |
| j) 50 yards accelerations (50%-75%) × 3 | |
| k) 30 yards arc left 10, arc right 10, sprint straight (50%-75%) 10 × 2 | |
| l) 5-yard zigzags 25 yards × 2 | |
| m) W drill, both directions | |
| n) Triangle drill both directions | |
| o) Combine short shuttle × 2 | |
| p) Individual period specific to position | |
| q) If player can complete all aspects of progression without hesitation and pain progress to phase 4 | |
| Phase 4 | |
| Position-specific conditioning and progressive return to practice |
The Biomet Gravitational Platelet Separation System (GPS III; Biomet, Warsaw, Indiana) was used for blood centrifugation to obtain PRP. An 18-gauge needle was attached to a 60-cc syringe and approximately 54 cc of blood was collected from the patient using an aseptic technique; 6 cc of citrate anticoagulant (ACD-A) was added to the collected blood. The blood sample was then centrifuged for 15 minutes at 3200 rpm. Approximately 6 cc of platelet concentrate was obtained at the end of the process. To neutralize the acidotic environment and minimize pain around the injury site, 0.5 cc of sodium bicarbonate per 1 cc of PRP was added to the platelet concentrate before it was injected into the patient. The injury site was accurately identified by an experienced board-certified radiologist using ultrasound, and the PRP injection was administered at the site of the injury under ultrasound guidance, within 24 to 48 hours of injury. A P value of <.05 was considered to be statistically significant.
RESULTS
There were 5 patients in each of the treatment and control groups. The median age was 23 years (range, 22-27 years) in the treatment group versus 26 years (range, 23-28 years) in the control group (P = .42) (Table 3). Each group had 2 grade 1 and 3 grade 2 hamstring injuries. The long head of biceps femoris (LHB) was the most commonly involved hamstring muscle, with 4 in each group; we observed 1 semimembranosus (SM) injury in each group. There were no significant differences between groups regarding the extent of the injuries in the longitudinal, transverse, or anteroposterior planes as read on MRI (Table 4).
Table 3.
Patient Age, Injury Grade and Size, and Time to Return to Play in Treatment and Control Groups
| Treatment | Control | P Value | |
|---|---|---|---|
| Age, y | 23 (22-27) | 26 (23-28) | .42 |
| Injury grade | Grade 2 (2 grade 1; 3 grade 2) | Grade 2 (2 grade 1; 3 grade 2) | >.99 |
| Hamstring strain dimensions, cm | 14 (9-18) | 15 (9-16) | .77 |
| Return to play, d | 20 (16-30) | 17 (8-81) | .73 |
Table 4.
Extent of Hamstring Injury in Longitudinal, Transverse, and Anteroposterior Planes on MRIa
| Extent of Injury, cm | |||
|---|---|---|---|
| MRI Plane | Treatment Group | Control Group | P Value |
| Longitudinal | 14 (9-18) | 15 (9-16) | .77 |
| Transverse | 4 (1.6-6) | 3.5 (2-5) | .45 |
| Anteroposterior | 4 (1.9-5) | 2.9 (1.5-4) | .3 |
aMRI, magnetic resonance imaging.
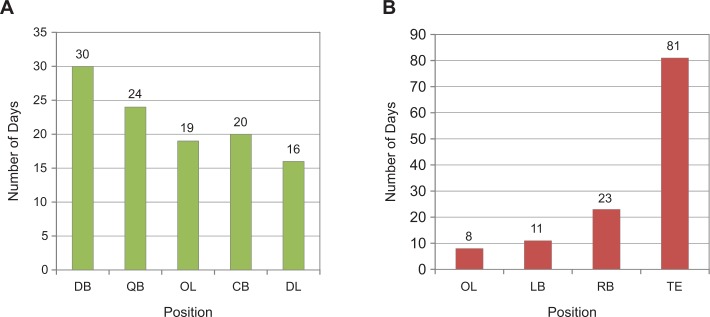
The median time to return to play was 20 days in the treatment group and 17 days in the control group (Table 3). The difference in recovery time was not statistically significant (P = .73) (Figure 1). The details of the dimension of the hamstring injuries in both groups are summarized in Table 3. In the treatment group, the follow-up at 6 months after injury did not reveal scarring, persistent pain, injection-related complications, infection, or bruising. None of the patients from either group reported recurrence at follow-up.
Figure 1.
Time to return to play (days) and different position of the player in the field in (A) the treatment (PRP) group and (B) the control group. DB, defensive back; QB, quarterback; OL, offensive line; CB, cornerback; DL, defensive line; LB, linebacker; RB, running back; TE, tight end; PRP, platelet-rich plasma.
DISCUSSION
Platelet-rich plasma is a general term for new technologies that are focused on enhancing the healing response after injury of different tissue types. The first descriptions of the development and use of PRP were in the 1990s, when science was focused on developing new “biologic glues.” The PRP preparations were considered potent glues because of their high proportion of fibrin, and they were primarily used in maxillofacial surgery.1,17
Sports medicine is an evolving field in which patients desire and require rapid recovery after injuries. Since the article that appeared on page 1 of the New York Times on February 17, 2009, concerning the treatment of a professional football player with PRP prior to his playing in the Superbowl,24 the excitement surrounding PRP has grown and the number of proposed uses has elevated it to the level of a platelet-rich panacea in the treatment of musculoskeletal disorders. To date, there is no published literature on the clinical outcome of PRP application over routine rehabilitation for hamstring injuries in professional athletes such as NFL players. This study was aimed to report comparative recovery time (return to play) with PRP injection versus rehabilitation only for hamstring injuries in elite athletes. Although no complications were noted with PRP injection, we could not find any significant difference in time to return to play between the players treated with PRP injection and rehabilitation only for hamstring injuries.
Zarins presented the results of a 10-year (1989-1998) epidemiological study of hamstring muscle strains in the NFL players (Zarins B. “Epidemiology of Hamstring Injuries in the NFL.” Presented at the NFL Combine Scientific Meeting, 2002). The authors noted that 16% of hamstring injuries were recurrent injuries. Orchard et al19 reported that 30% of Australian rules football players could be expected to sustain a recurrent injury. Rettig et al21 reported an incidence of 31% for recurrent hamstring injuries in NFL players. Koulouris and Connelly15 concluded that the cross-sectional area, size, and grade of the injury on MRI were the significant predictors of recovery time as well as recurrence. The authors stated that 90% of Australian football players sustaining a repeat injury had an initial injury length >60 mm or >10% on cross section. In our series, the follow-up at 6 months did not reveal recurrent injuries noted among the players in the treatment or control groups. One player in the control group with a grade 2 hamstring injury affecting the LHB took longer (81 days) than average to return to play. The background history for this player was significant for a grade 1 hamstring injury that occurred 18 months previously, but a follow-up MRI did not show any sign of residual injury prior to his second hamstring injury.
It has been documented in the literature7 that the LHB is the most commonly involved muscle, followed by the SM and semitendinosus (ST) (Bradley J, Cohen S. “Hamstring Injuries in NFL Players: MRI Correlation With Return to Play.” Presented at the AAOS Annual Meeting, 2009). The findings of this series are also comparable, with 4 (80%) LHB and 1 (20%) SM injury in each group.
Bradley and Cohen reported the correlation between MRI findings and time to return to play after hamstring injuries in NFL players (Bradley J, Cohen S. “Hamstring Injuries in NFL Players: MRI Correlation With Return to Play ”; 2009.). The authors noted that rapid (1 week or less) return to play was observed if the injury involved isolated LHB, less than 50% of the cross section, and minimal perimuscular edema. Intermediate return (1-2 weeks) was observed when there was multiple muscle or short head of biceps involvement with circumferential edema. Delayed return (>3 weeks) was seen in cases of hamstring injuries with muscle retraction or involvement of over 75% of the cross-section area. Rettig et al21 reported the time to return to play for grade 1, 2, and 3 hamstring injuries as 16, 21.5, and 28.5 days, respectively. In our series, the median time to return to play in the treatment and control groups was 20 and 17 days, respectively. Although the recovery time in both groups was consistent with published data, the difference between the 2 groups was not statistically significant.
Muscle healing follows the stages of inflammation, proliferation, and remodeling that are coordinated by cellular interactions. The usual recommendation for recovery from a muscular injury is rest, ice, compressive dressings, and elevation of the affected extremity. Several techniques have been employed in an effort to shorten return-to-play intervals. One in vitro study suggests that growth factors may influence muscle regeneration after injury.14 However, there are no randomized controlled human studies regarding the use of PRP to treat muscle injuries. Bradley presented an unpublished report at the NFL combined meeting in 2010 (Bradley J. “Hamstring Injuries in NFL: Does ACP Affect Return to Play?” Presented at the NFL Combine Meeting, 2010.) and demonstrated a difference in return to practice of 3 days in grade 1 and 5 days in grade 2 hamstring injuries in NFL players when they were treated with repeated autologous conditioned plasma (ACP). Although we used a different commercial system to prepare the platelet concentrate, with single PRP injection for acute hamstring injuries, we did not notice any difference in time to return to play over routine rehabilitation only.
It is not surprising that the encouraging results of PRP use in the treatment of different musculoskeletal disorders2,10,14,18,20,22,23 make the addition of PRP to other forms of treatment a very tempting option. With the limited information available, the risk of PRP has been described as minimal,4,22 although excessive scarring and delay in remodeling of healing tissues have been mentioned as theoretical side effects of growth factor application.6,8,16 Sanchez et al found no fibrosis in 20 athletes treated with a preparation rich in growth factors at long-term follow-up, and no reinjuries occurred (Sanchez M, Anitua E, Andia I. “Application of Autologous Growth Factors on Skeletal Muscle Healing.” Presented at the 2nd International Conference on Regenerative Medicine, 2005). In the current series, there was no scarring, no injection site infection, and no recurrence of injury.
There are some limitations with this study. This study was a retrospective, case control study in design, and the number of patients treated was small. A larger study is warranted to assess the safety and efficacy of the use of PRP as a treatment of hamstring injuries. The potential impact of widespread PRP use on impecunious health care budgets also requires careful consideration. The positions of players in the 2 groups were not matched. As different positions of the players in the field demand different levels of activity, the effect of playing position on time to return to play has to be taken into account. At the same time, we should remember that it is not easy to conduct a randomized controlled study of elite athletes such as NFL players who can be matched completely, including the position they play.
CONCLUSION
This preliminary study involving the use of PRP and rehabilitation program for the treatment of acute hamstring injuries in NFL players did not show any significant difference in time to return to play. Although some promising results have been shown in different musculoskeletal disorders, further research needs to be aimed at delineating correct dosage, timing, and quantification as well as ideal techniques of PRP application. Future randomized controlled studies with a larger group of patients are warranted.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
REFERENCES
- 1. Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14:529–535. [PubMed] [Google Scholar]
- 2. Arnoczky SP, Anderson L, Fanelli G, Ho S, Mishra A, Sgaglione N. The role of platelet-rich plasma in connective tissue repair. Orthopedics Today. 2009;26:29. [Google Scholar]
- 3. Askling CM, Tengvar M, Saartok T, Thorstensson A. Acute first-time hamstring strains during high-speed running: a longitudinal study including clinical and magnetic resonance imaging findings. Am J Sports Med. 2007;35:197–206. [DOI] [PubMed] [Google Scholar]
- 4. Aspenberg P, Virchenko O. Platelet concentrate injection improves Achilles tendon repair in rats. Acta Orthop Scand. 2004;75:93–99. [DOI] [PubMed] [Google Scholar]
- 5. Brooks JH, Fuller CW, Kemp SP, Redding DB. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34:1297–1306. [DOI] [PubMed] [Google Scholar]
- 6. Chan YS, Li Y, Foster W, Fu FH, Huard J. The use of suramin, an antifibrotic agent, to improve muscle recovery after strain injury. Am J Sports Med. 2005;33:43–51. [DOI] [PubMed] [Google Scholar]
- 7. Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975–984. [DOI] [PubMed] [Google Scholar]
- 8. de Mos M, van der Windt AE, Jahr H, et al. Can platelet-rich plasma enhance tendon repair? A cell culture study. Am J Sports Med. 2008;36:1171–1178. [DOI] [PubMed] [Google Scholar]
- 9. Feeley BT, Kennelly S, Barnes RP, et al. Epidemiology of national football league training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36:1597–1603. [DOI] [PubMed] [Google Scholar]
- 10. Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari PM, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop. 2010;34:909–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Plasma-rich protein: from basic science to clinical applications. Am J Sports Med. 2009;37:2259–2272. [DOI] [PubMed] [Google Scholar]
- 12. Gandhi A, Bibbo C, Pinzur M, Lin SS. The role of platelet-rich plasma in foot and ankle surgery. Foot Ankle Clin. 2005;10:621–637. [DOI] [PubMed] [Google Scholar]
- 13. Hammond JW, Hinton RY, Curl LA, Muriel JM, Lovering RM. Use of autologous platelet-rich plasma to treat muscle strain injuries. Am J Sports Med. 2009;37:1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kasemkijwattana C, Menetrey J, Bosch P, et al. Use of growth factors to improve muscle healing after strain injury. Clin Orthop Relat Res. 2000;370:272–285. [DOI] [PubMed] [Google Scholar]
- 15. Koulouris G, Connelly D. Imaging of hamstring injuries: therapeutic implications. Eur Radiol. 2006;16:1478–1487. [DOI] [PubMed] [Google Scholar]
- 16. Majewski M, Ochsner PE, Liu F, Flückiger R, Evans CH. Accelerated healing of the rat Achilles tendon in response to autologous conditioned serum. Am J Sports Med. 2009;37:2117–2125. [DOI] [PubMed] [Google Scholar]
- 17. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638–646. [DOI] [PubMed] [Google Scholar]
- 18. Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;34:1774–1778. [DOI] [PubMed] [Google Scholar]
- 19. Orchard J, Best TM, Verrall GM. Return to play following muscle strains. Clin J Sports Med. 2005;15:436–441. [DOI] [PubMed] [Google Scholar]
- 20. Reider B. Proceed with caution. Am J Sports Med. 2009;37:2099–2101. [DOI] [PubMed] [Google Scholar]
- 21. Rettig AC, Myers S, Kersey PA, et al. Categorization of hamstring strain injuries by MRI and playing time lost in professional football players. NATA News. July 2000;29–32. [Google Scholar]
- 22. Sánchez M, Anitua E, Azofra J, Andía I, Padilla S, Mujika I. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med. 2007;35:245–251. [DOI] [PubMed] [Google Scholar]
- 23. Sánchez M, Anitua E, Azofra J, Aguirre JJ, Andia I. Intra-articular injection of an autologous preparation rich in growth factors for the treatment of knee OA: a retrospective cohort study. Clin Exp Rheumatol. 2008;26:910–913. [PubMed] [Google Scholar]
- 24. Schwartz A. A promising treatment for athletes, in blood. The New York Times. February 17, 2009. [Google Scholar]