Abstract
Background:
Acute patellar dislocation (APD) is a common knee injury in children. The pattern and frequency of injury to the medial patellofemoral ligament (MPFL) is different in pediatric compared with adult populations.
Purpose:
To report on injury patterns sustained to the MPFL after APD in children and to determine whether predisposing factors for APD cited in adults hold true in the pediatric population.
Study Design:
Case series; Level of evidence, 4.
Methods:
Magnetic resonance imaging (MRI) studies were reviewed for 36 children sustaining APD. Evidence of injury to the MPFL was documented, and when the MPFL was torn, the location of tear was determined. Presence of trochlear dysplasia, patella alta, tibial tubercle–trochlear groove (TTTG) distance, and thickness of the lateral patellofemoral retinaculum (LPR) were recorded and correlated with MPFL tear.
Results:
Of the 36 patients sustaining APD, only 16 tore the MPFL. The location of MPFL tear was equally divided between the origin, the insertion, or both, with no case of midsubstance tear. There was a significant correlation identified between MPFL rupture and both LPR thickness greater than 3 mm and TTTG distance greater than 19 mm.
Conclusion:
The MPFL does not always tear in children who sustain APD, and the tear location is variable. A thickened LPR and increased TTTG distance predispose to MPFL tear.
Keywords: medial patellofemoral ligament, lateral patellofemoral retinaculum, patella, dislocation
Acute patellar dislocation (APD) is a common injury in children, accounting for up to 16% of acute knee hemarthroses.30 Correctly diagnosing APD can be difficult as the displaced patella usually relocates spontaneously, with fewer than 10% of patients presenting with fixed lateral dislocation.7,14 While plain radiography is an important tool to diagnose APD, magnetic resonance imaging (MRI) is essential to identify the many injuries not seen on radiographs.3,13,20 APD may result in severe injury to bone, cartilage, and the supporting structures of the patella.22,25,30 The medial patellofemoral ligament (MPFL), a major static stabilizer of the patella in early flexion, is reported to be commonly injured as a result of APD.2,5,11,13,16,19,21,26–28 The site of MPFL injury has been variably reported to occur at the origin, the insertion, midsubstance, or a combination of these locations. In addition, several anatomic variables have been shown to predispose to APD and MPFL tear, including patella alta, trochlear dysplasia, and increased lateralization of the tibial tubercle.2,4,15,25,29,30 The purpose of this study was 2-fold: to report on the MPFL injury pattern found on MRI in a pediatric population sustaining APD and to determine if predisposing factors for MPFL tear reported in adults also are predictive in children.
Materials and Methods
After obtaining institutional review board approval, we retrospectively reviewed all cases of primary APD that presented to our pediatric orthopaedic department over a 6-year period from 2003 through 2009. All patients were initially identified through a query of available electronic medical records and hard-copy charts. Inclusion criteria were history and physical examination suggestive of first-time APD, children aged 5 to 18 years, and availability of an MRI performed at our institution. Patients were excluded from the study if there was a history of prior knee surgery, congenital knee problems, or prior patellar dislocation; lack of an MRI to review; or if patients were older than 18 years.
A fellowship-trained musculoskeletal radiologist and a senior radiology resident retrospectively reviewed all MRI studies by consensus. Thirty-five knee MRIs were performed on a 1.5-T magnet (GE Healthcare, Fairfield, Connecticut, USA), and 1 MRI was performed on a 1.0-T ONI extremity magnet (GE Healthcare). The following sequences were obtained using either a 4- or 8-channel knee coil: sagittal proton density fat-saturated (FSE) (repetition time [TR], 2100-2500 ms; echo time [TE], 42 ms); sagittal T2 fat-saturated (FSE) (TR, 3000-5000 ms; TE, 65 ms); coronal T1 (TR, 400-600 ms; TE, 14-25 ms); coronal T2 fat-saturated (TR, 3000-5000 ms; TE, 65 ms); and axial T2 fat-saturated (TR, 3000-5000 ms; TE, 60 ms). All slice thicknesses were 4 mm with a 1-mm gap. All images were 2-dimensional standard sequences, with no 3-dimensional isometric sequences performed.
T2 fat-suppressed axial images were used to identify injury to the MPFL. MPFL sprain was defined as increased signal in and around the MPFL without thickening and having intact fibers. MPFL tear was defined as absent or discontinuous ligament fibers. If the MPFL was torn, the site of injury was recorded as origin (patellar), insertion (femoral), midsubstance, or a combination. The lateral patellofemoral retinaculum (LPR) was evaluated for injury and thickness on the axial T2 fat-saturated images, with the area of maximal thickness measured. Axial, coronal, and sagittal images were reviewed for evidence of injury elsewhere in the knee, including collateral and cruciate ligament injury, meniscal injury, vastus medialis oblique muscle injury,11,30 bone edema, and osteochondral plate continuity.19 A thorough search of the joint was made for the low–signal intensity characteristics of osteochondral or chondral intra-articular loose bodies.
Several anatomic measurements were made using MRI. Trochlear dysplasia was assessed on axial images by measuring the subchondral sulcus angle (SSA). SSA measured by MRI has been shown to be equal to measurements made by radiographs.18 SSA was measured at the first craniocaudal image showing a complete cartilaginous trochlea and corresponding to the deepest depression of the intercondylar groove.4,9,12 Presence of patella alta was determined by measuring the patellar tendon–patella ratio using the method reported by Miller et al.17 The tibial tubercle–trochlear groove (TTTG) distance, a measure of tibial tubercle lateralization, was measured in all patients using the method described by Schoettle et al.23
An independent unpaired t test was computed to assess the relationship between MPFL tear and each of the following: LPR thickness, TTTG, SSA, and patella alta. Significance was set at P < .05.
Results
There were 40 patients initially identified as sustaining an acute patellar dislocation from the chart review. Three patients were ultimately excluded for not having an MRI, and 1 patient was excluded because of incorrect International Classification of Diseases, 9th Revision (ICD-9) code, leaving 36 patients available for study. The study population included 19 females with a mean age of 14.2 years (range, 8-17 years) and 17 males with a mean age of 14.8 years (range, 13-17 years). The average time from injury to MRI was 35 days (range, 5-135 days).
MRI revealed MPFL injury in only 21 patients (58%), with 16 identified as tears and 5 as sprains. Of those with MPFL tear, there was a balanced distribution for location of tear: 5 torn at origin (Figure 1), 6 torn at insertion (Figure 2), and 5 with tears at both origin and insertion. There were no intrasubstance tears identified.
Figure 1.
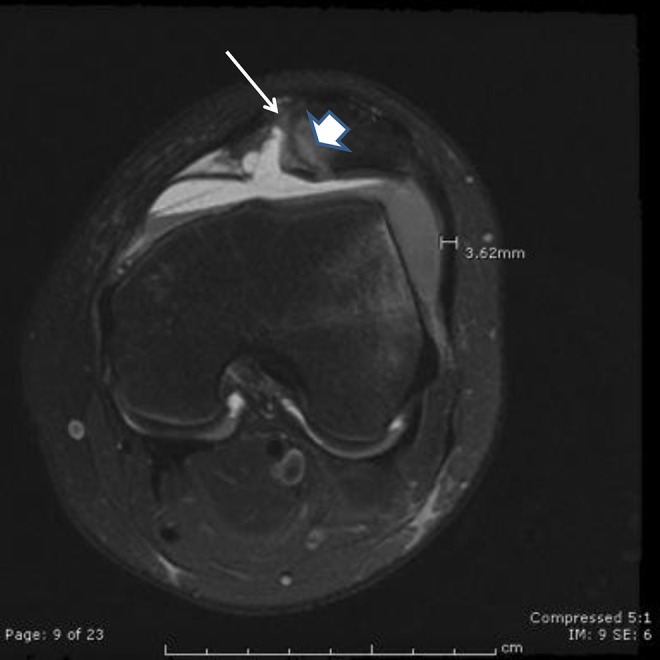
Axial T2-weighted image with fat saturation demonstrating a patellar-sided medial patellofemoral ligament tear (thin arrow) with thickening of the lateral patellofemoral retinaculum. A large osteochondral defect and bone contusion is present along the medial patella (thick arrow).
Figure 2.
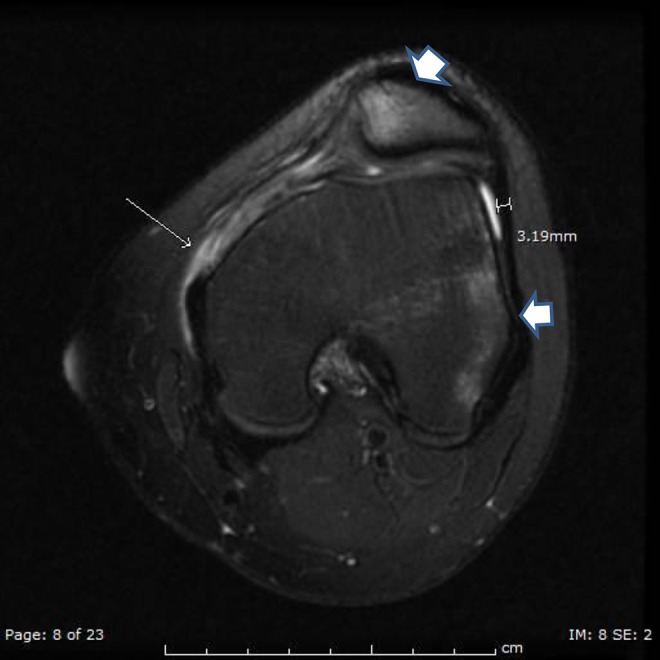
Axial T2-weighted image with fat saturation demonstrating a femoral-sided medial patellofemoral ligament tear (thin arrow) with thickening of the lateral patellofemoral retinaculum. Classic bone edema pattern is present involving the inferomedial patella and the lateral femoral condyle (thick arrows).
The thickness of the LPR was measured in all cases (Figures 1 and 2). The mean LPR thickness in patients sustaining an MPFL tear was 3.09 mm (standard deviation [SD], 1.22 mm), while that of patients sustaining sprain or no injury to the MPFL measured 2.33 mm (SD, 0.39 mm). The relationship between increasing LPR thickness and MPFL tear reached statistical significance (P = .012).
SSAs averaged 149° (range, 117° to 180°) for all patients, with normal considered to be 142° (±9°).18 The mean SSA for patients with MPFL tear was not statistically different from knees without MPFL tear (P = .078). Patella alta was identified on sagittal MRI by a patellar tendon–patella ratio >1.3.9 The mean tendon-patella ratio for our cases was 1.26 (range, 0.99-1.63), with no difference in patella height between patients with and without MPFL tear (P = .99). The mean TTTG distance for patients with MPFL tear was 18.9 mm (SD, 5 mm), while those without MPFL tear averaged 14.9 mm (SD, 4.6 mm). Increased TTTG was found to be statistically correlated with tear of the MPFL (P = .02).
There were numerous other injuries noted on MRI (Table 1), with 50% of patients having additional injury. These are reported to demonstrate the destructive force sustained by the knee during APD.
Table 1.
MRI Findings After Acute Patellar Dislocation
| Finding | Frequency (n = 36) | Percentage of Patients |
|---|---|---|
| Joint effusion | 23 | 63.9 |
| Bone bruise | 28 | 77.8 |
| Cartilage injury | 16 | 44.4 |
| Osseous fragments | 6 | 16.7 |
| Other injury site | ||
| Vastus medialis obliquus | 8 | 22.2 |
| Medial collateral ligament | 1 | 2.8 |
| Anterior cruciate ligament | 1 | 2.8 |
| Menisci | 1 | 2.8 |
| Hoffa fat pad edema | 6 | 16.7 |
| Popliteus | 1 | 2.8 |
| Total | 18 | 50.0 |
Discussion
MRI has proven an excellent adjunct in confirming the diagnosis of APD in the setting of an acute posttraumatic knee hemarthrosis. MRI is also invaluable for demonstrating additional injury sustained to supporting structures throughout the knee not identified on radiographs. We sought to better define the injury pattern sustained to the MPFL as a result of patellar dislocation in a pediatric population and determine which anatomic measurements might be predictive of MPFL tear.
The MPFL is the major static stabilizer of the patella during early knee flexion. MPFL tear has been considered the “essential lesion” of APD by some.1 In a series of 73 adults with APD, Balcarek et al2 reported that more than 98% sustained MPFL complete or partial tears. Sillanpaa et al26 reported on 40 adult patients with APD, all but 1 of whom sustained a complete MPFL tear. Weber-Spickschen et al29 reported on 59 patients, mostly adults, all but 1 of whom sustained an MPFL tear. The consistent correlation of APD to MPFL tear in adults does not seem to hold true for a pediatric population. Zaidi et al30 reported on 26 children with suspected APD and none had complete MPFL tears, though all showed MPFL sprain. Seeley et al25 reported on 111 adolescents and found MPFL injury in 78%, with complete tears in 68%. We too report a much lower rate of MPFL tear (44%) and overall injury rate (58%) than is reported in adult populations after APD. It remains unclear why pediatric populations have a lower incidence of MPFL tear after APD compared with adult counterparts.
The site of MPFL tear is important to discern when considering surgical repair, as tears can occur at the origin, the insertion, midsubstance, or a combination. Authors of studies including mostly adult patients (age >18 years) report a higher incidence of MPFL tear at the femoral insertion,2,20,27,29 though 1 large study of 195 patents by Guerrero et al13 found the majority of tears occur at the patellar origin. Studies reviewing APD in children seem split. Some authors report a higher incidence of MPFL tear at the patellar origin,15,30 while others found more tears at the femoral insertion.4,21 We found a nearly equal distribution for MPFL tear location, with one third involving the origin, one third the insertion, and one third involving both. If surgical repair of a torn MPFL is planned, preoperative MRI is essential to determine location of tear, as the tear pattern cannot be assumed to occur only at 1 location in children.
Several anatomic variables have been implicated as predisposing to MPFL tear: patella alta, trochlear dysplasia, and tibial tubercle lateralization to name a few. While we found no correlation of patella alta or trochlear dysplasia to MPFL tear, we did find that a TTTG greater than 19 mm increased the risk of MPFL tear. To our knowledge, only 1 other article has identified this correlation with TTTG.4
In all our cases, we chose to measure the thickness of the lateral patellofemoral retinaculum. In an anatomic selective cutting study evaluating soft tissue restraints to lateral patellar translation, Desio et al10 found that the LPR somewhat paradoxically contributed 10% of the restraining force to lateral translation. The authors concluded that lateral release alone for treatment of recurrent patellar dislocation is not indicated and may explain the high failure rates reported by others when done as a stand-alone procedure.6,8,24 We postulated we might find injury to this structure in children with APD. While we found no injury to the LPR, we do report a new finding that LPR thickness greater than 3 mm was predictive of MPFL tear after APD. Perhaps this information suggests that the thickened LPR may be part of the pathology leading to MPFL tear and that lateral release may be beneficial when performing comprehensive surgery to prevent recurrent patellar dislocation.
There are several weaknesses to this study, especially with regard to our reporting that LPR thickness predisposes to MPFL tear during acute patellar dislocation. One can argue that the LPR is not truly thick; rather, the LPR only appears thick because of subtle lateral patellar subluxation as a result of MPFL tear. The only way to know for certain is to obtain MRI of the knee both before and after injury, which clearly cannot be done. One could obtain MRI of both the injured and uninjured knee at the same time, assuming the anatomy is the same, and compare LPR thickness of both knees; however, the authors feel the added time and expense of imaging an uninjured knee may not be justified. The authors believe the measurement of the LPR reported is representative as the LPR does not appear to be lax on the axial images.
Another weakness of the study is the delay between injury and MRI. While the average of 35 days would certainly still demonstrate acute MPFL injury, one could argue that an MRI obtained at 3 and 4 months from injury (latest MRI was at 135 days) might show no MPFL injury if it had healed. The authors believe that this range of injury to MRI represents what often happens in a general practice with usual delays of referral to an orthopaedic surgeon, so we decided to keep the patient population together for analysis.
In summary, APD in children can result in significant injuries to the knee. For children presenting with acute knee hemarthrosis, a high index of suspicion for APD must be maintained so as not to miss these associated injuries. The effect APD has on the MPFL seems distinct between adult and pediatric populations: Whereas the MPFL is usually torn in adults, it is not as commonly torn in children. In addition, when the MPFL is torn, the location of injury is variable and cannot always be assumed to occur at 1 location. As such, MRI is a necessary imaging modality to evaluate these injured knees to help guide treatment. In addition, we report that increased TTTG and thickened LPR are predictive of MPFL tear during patellar dislocation.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the US Government.
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215–220. [DOI] [PubMed] [Google Scholar]
- 2. Balcarek P, Ammon J, Frosch S, et al. Magnetic resonance imaging characteristics of the medial patellofemoral ligament lesion in acute lateral patellar dislocations considering trochlear dysplasia, patella alta, and tibial tuberosity-trochlear groove distance. Arthroscopy. 2010;26:926–935. [DOI] [PubMed] [Google Scholar]
- 3. Balcarek P, Walde TA, Frosch S, Schuttrumpf JP, Wachowski MM, Sturmer KM. MRI but not arthroscopy accurately diagnoses femoral MPFL injury in first-time patellar dislocations. Knee Surg Sports Traumatol Arthrosc. 2012;20:1575–1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Balcarek P, Walde TA, Frosch S, et al. Patellar dislocations in children, adolescents and adults: a comparative MRI study of medial patellofemoral ligament injury patterns and trochlear groove anatomy. Eur J Radiol. 2011;79:415–420. [DOI] [PubMed] [Google Scholar]
- 5. Beasley LS, Vidal AF. Traumatic patellar dislocation in children and adolescents: treatment update and literature review. Curr Opin Pediatr. 2004;16:29–36. [DOI] [PubMed] [Google Scholar]
- 6. Betz RR, Magill JT, 3rd, Lonergan RP. The percutaneous lateral retinacular release. Am J Sports Med. 1987;15:477–482. [DOI] [PubMed] [Google Scholar]
- 7. Boden BP, Pearsall AW, Garrett WE, Jr, Feagin JA., Jr Patellofemoral instability: evaluation and management. J Am Acad Orthop Surg. 1997;5:47–57. [DOI] [PubMed] [Google Scholar]
- 8. Chen SC, Ramanathan EB. The treatment of patellar instability by lateral release. J Bone Joint Surg Br. 1984;66:344–348. [DOI] [PubMed] [Google Scholar]
- 9. Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45–54. [PubMed] [Google Scholar]
- 10. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translatoin in the human knee. Am J Sports Med. 1998;26:59–65. [DOI] [PubMed] [Google Scholar]
- 11. Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225:736–743. [DOI] [PubMed] [Google Scholar]
- 12. Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schottle PB. The patellar morphology in trochlear dysplasia—a comparative MRI study. Knee. 2006;13:145–150. [DOI] [PubMed] [Google Scholar]
- 13. Guerrero P, Li X, Patel K, Brown M, Busconi B. Medial patellofemoral ligament injury patterns and associated pathology in lateral patella dislocation: an MRI study. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34:385–396. [DOI] [PubMed] [Google Scholar]
- 15. Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39:1444–1449. [DOI] [PubMed] [Google Scholar]
- 16. Mashoof AA, Scholl MD, Lahav A, Greis PE, Burks RT. Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patella dislocation. Arthroscopy. 2005;21:228–232. [DOI] [PubMed] [Google Scholar]
- 17. Miller TT, Staron RB, Feldman F. Patellar height on sagittal MR imaging of the knee. AJR Am J Roentgenol. 1996;167:339–341. [DOI] [PubMed] [Google Scholar]
- 18. Murshed KA, Cicekcibasi AE, Ziylan T, Karabacakoglu A. Femoral sulcus angle measurements: an anatomical study of magnetic resonance images and dry bones. Turk J Med Sci. 2004;34:165–169. [Google Scholar]
- 19. Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19:717–721. [DOI] [PubMed] [Google Scholar]
- 20. Nomura E, Horiuchi Y, Inoue M. Correlation of MR imaging findings and open exploration of medial patellofemoral ligament injuries in acute patellar dislocations. Knee. 2002;9:139–143. [DOI] [PubMed] [Google Scholar]
- 21. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90:463–470. [DOI] [PubMed] [Google Scholar]
- 22. Sanders TG, Paruchuri NB, Zlatkin MB. MRI of osteochondral defects of the lateral femoral condyle: incidence and pattern of injury after transient lateral dislocation of the patella. AJR Am J Roentgenol. 2006;187:1332–1337. [DOI] [PubMed] [Google Scholar]
- 23. Schoettle PB, Zanetti M, Seifert B, Pfirrmann CW, Fucentese SF, Romero J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee. 2006;13:26–31. [DOI] [PubMed] [Google Scholar]
- 24. Schonholtz GJ, Zahn MG, Magee CM. Lateral retinacular release of the patella. Arthroscopy. 1987;3:269–272. [DOI] [PubMed] [Google Scholar]
- 25. Seeley M, Bowman KF, Walsh C, Sabb BJ, Vanderhave KL. Magnetic resonance imaging of acute patellar dislocation in children: patterns of injury and risk factors for recurrence. J Pediatr Orthop. 2012;32:145–155. [DOI] [PubMed] [Google Scholar]
- 26. Sillanpaa PJ, Mattila VM, Maenpaa H, Kiuru M, Visuri T, Pihlajamaki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am. 2009;91:263–273. [DOI] [PubMed] [Google Scholar]
- 27. Sillanpaa PJ, Peltola E, Mattila VM, Kiuru M, Visuri T, Pihlajamaki H. Femoral avulsion of the medial patellofemoral ligament after primary traumatic patellar dislocation predicts subsequent instability in men: a mean 7-year nonoperative follow-up study. Am J Sports Med. 2009;37:1513–1521. [DOI] [PubMed] [Google Scholar]
- 28. Stanitski CL, Paletta GA., Jr Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med. 1998;26:52–55. [DOI] [PubMed] [Google Scholar]
- 29. Weber-Spickschen TS, Spang J, Kohn L, Imhoff AB, Schottle PB. The relationship between trochlear dysplasia and medial patellofemoral ligament rupture location after patellar dislocation: an MRI evaluation. Knee. 2011;18:185–188. [DOI] [PubMed] [Google Scholar]
- 30. Zaidi A, Babyn P, Astori I, White L, Doria A, Cole W. MRI of traumatic patellar dislocation in children. Pediatr Radiol. 2006;36:1163–1170. [DOI] [PubMed] [Google Scholar]


