Abstract
Background:
Youth football programs across the United States represent an at-risk population of approximately 3.5 million athletes for sports-related concussions. The frequency of concussions in this population is not known.
Study Design:
Descriptive epidemiology study.
Methods:
Over an 11-year span from January 2002 to December 2012, the authors reviewed the concussions sustained by athletes aged 5 to 13 years while playing football, as evaluated in emergency departments (EDs) in the United States and captured by the National Electronic Injury Surveillance System (NEISS) database of the US Consumer Product Safety Commission.
Results:
There were 2028 (national estimate, 49,185) young football players evaluated in NEISS EDs with concussion from 2002 to 2012. There were 1987 (97.9%) males and 41 (2.1%) females, with a mean age of 11.2 years. The total number of concussions reported increased with age and by year. The majority of concussions were treated in the outpatient setting, with 1878 (91.7%) being treated and released. The total number of head-to-head injury mechanisms mirrored the total number of concussions by year, which increased throughout the 11-year span. The total number of players experiencing a loss of consciousness increased throughout the study period but did not match the total number of concussions over the 11-year time period. Fractures occurred in 11 (0.5%) patients, with 2 being severe (1 skull fracture and 1 thoracic compression fracture).
Conclusion:
Within the 5- to 13-year age range, there were a significant number of young athletes who presented to EDs with concussion as a result of playing organized football. Older children may be at greater risk for sustaining concussions, fractures, and catastrophic injuries while playing football when compared with younger children.
Clinical Relevance:
Younger children are more susceptible to long-term sequelae from head injuries, and thus, improved monitoring systems for these athletes are needed to assist in monitoring patterns of injury, identifying risk factors, and driving the development of evidence-based prevention programs.
Keywords: concussion, football, epidemiology, NEISS, pediatrics, head injuries
Concussions are generally self-limiting, mild traumatic brain injuries that induce transient disturbance of brain function.2,11 Linear and/or rotational forces transmitted to the brain, frequently caused by a blow to the head, produce concussions. Until normal cellular function is restored, the brain has an increased susceptibility to a second injury and progressively more significant metabolic and cognitive derangement.2,20,22 The concussed brain functions at a lower level and is less responsive to stimulation.20,22 Cognitive or physical exertion before complete recovery can potentiate metabolic and cognitive dysfunction.20,22
Concussion can occur in any sport but is more commonly seen in football, wrestling, soccer, basketball, baseball, and field hockey.19 The estimates of sports-related concussions range from 1.6 to 3.8 million per year.12 Powell and Barber-Foss19 found that the majority (63.4%) of mild traumatic brain injuries in high school athletes occurred in football players.
The monitoring of head injuries has increased more so for professional and college athletes compared with high school athletes.6,8,11,14,19,21 Recently, as the public has become more aware of the health implications associated with concussions, legislation has been passed in 42 states in the United States as well as the District of Columbia, setting guidelines for coaches and medical personnel with the goal of increasing the detection of concussions.15 These guidelines range from coaches receiving training on recognition of concussions to formal evaluation and clearance by a trained medical professional before allowing return to play.8,11,15 Guidelines may also help obtain more accurate estimates of concussion frequency in young athletes, and ultimately, result in rule changes that reduce the number of concussions.
Approximately 5 million athletes participate in organized football in the United States; 3.5 million of these are young football players,3 and therefore, they represent the largest group at risk for concussions. This group is also at risk for recurrent concussions with continued participation in collision sports. Historically, research on concussion has not been focused on this subgroup of athletes. The brains of young athletes are susceptible to the long-term sequelae of concussions in comparison with their older colleagues. It has been found that the young athlete’s developing brain is physiologically different from the adult and takes a longer time to recover from a concussion.9,22,23,25 The developing brain also has less cognitive reserve and less well-established engrams.7,22,23 Consequently, the prolonged recovery from concussion in the younger patients increases the risk for sequential/secondary injuries and may invalidate comparisons with more mature patients with concussion (high school, collegiate, and professional athletes).7,9,22,23,25
Bakhos et al1 utilized the National Electronic Injury Surveillance System (NEISS) database to identify sports-related concussion in adolescent and high school athletes aged 8 to 19 years from 2001 to 2005. These authors utilized the NEISS database to review the epidemiology of concussions and included all cases with a diagnosis of concussion that presented to the emergency departments (EDs) of hospitals that participated in the NEISS system. Bakhos et al1 divided subjects into 2 groups by age (pre–high school [8-13 years old] and high school [14-19 years old]) for further analysis and reported the sports in which concussions occurred: individual and leisure sports versus organized team sports (eg, football, basketball, baseball, ice hockey, and soccer). In their series, 50% (range, 35%-64% depending on sport) of all concussions occurred in sports-related activities. In athletes aged 8 to 13 years, 58% of concussions occurred during participation in sports, with football participation being the most common. They did not take into account the mechanism of injury, associated loss of consciousness, concurrent fractures, or athletes younger than 8 years.
The purpose of this study was to enhance this information by including athletes in a younger age group (aged 5-13 years) and describe the epidemiology of youth football–related concussions that presented to US EDs over an 11-year period from January 2002 to December 2012 using a nationally representative database.
Methods
National Electronic Injury Surveillance System
Data were collected from the NEISS, a database maintained by the US Consumer Product Safety Commission (CPSC) that collects information on injuries that present to US EDs at a network of 100 hospitals. NEISS hospitals are a stratified probability sample of hospitals in the United States and its territories. The participating hospitals have at least 6 beds and a 24-hour ED where trained coders review all ED records daily and enter demographic, injury, and treatment information into the NEISS database. Each case is assigned 1 or 2 CPSC-specific product codes that designate what products or activities were involved at the time of injury.24 National estimates can then be calculated by summing the number of cases that present to each NEISS ED after using a multiplier based on the size of the hospital and the number of hospitals similarly sized across the country.24 As the hospitals are a representative sample of all the hospitals nationwide, it is presumed that trauma centers of various levels are actively participating.
Utilization of NEISS
We queried the NEISS database for all football-related head injuries (football product code 1211, head body part location code 75, with a diagnosis of concussion) that presented to NEISS EDs from 2002 to 2012. The NEISS data set provides patient demographic information (age, race, and sex) on the injury sustained, diagnosis, disposition, location injury occurred (school, place of recreation, home, public property, or street or highway), and a brief narrative describing how the injury occurred. Narratives are a relatively new feature that were added to the NEISS database on January 1, 2002, but are highly variable as to their content and length. The variability in the narratives was minimized by targeting specific information. This included information on injury mechanisms, specifically: head-to-head collision, loss of consciousness (LoC), level of activity (competition or practice), or concurrently sustained fractures. There was overlap between our data set and that published by Bakhos et al.1 However, we focused specifically on football players and included an even younger demographic.
Exclusion Criteria
The narratives provided were also reviewed for each case, and those that mentioned “play with [a sibling/family member],” “play at home,” “gym class,” “PE [physical education]” or “pick-up game” were excluded. Narratives describing bystanders who were injured in the stands or individuals who were injured while helping at practice were excluded. Cases where the injury occurred from another event and the individual was only identified as a football player were excluded. Finally, all cases that had a location other than school, place of recreation or sports, or was not recorded were excluded.
Data Analysis
Descriptive statistical analysis was performed using Microsoft Excel (Microsoft, Redmond, Washington, USA). Subset analysis was performed on those who sustained a fracture as well as patients who required hospital admittance or were transferred to another hospital for further care. This subset also consisted of cases with a diagnosis of concussion with concomitant skull fracture in the NEISS database and was therefore included. National estimates of youth football concussions, loss of consciousness, and head-to-head contact as the mechanism of concussion were also calculated utilizing NEISS hospitals as a stratified national sampling.24 National estimates were calculated by multiplying the actual number of cases by an averaged conversion factor that was associated with each case. The Spearman correlation coefficient was used to quantify the relationship between the total number of concussions, total loss of consciousness, and head-to-head mechanism of injury over the 11-year period.
Results
There were 2028 football players who presented to NEISS EDs with concussions from January 2002 to December 2012 with a mean age of 11.2 years (median, 12 years). There were 1987 (97.9%) males and 41 (2.1%) females. National estimates were calculated to be 49,185 concussions occurring in youth football players 5 to 13 years of age over an 11-year time frame. A total of 374 cases were excluded as they did not fit the inclusion criteria.
The total number of concussions increased throughout this 11-year time frame. The number of concussions increased for each age group, and older players sustained more concussions than younger players (Figures 1 and 2). Figure 1 demonstrates a greater increase in the number of concussions from years 2008 to 2009 compared with previous years. The number of concussions increased 1.28 times in 2009 compared with 2008; however, the number of patients admitted to the hospital increased 4.67 times in 2009 compared with 2008.
Figure 1.
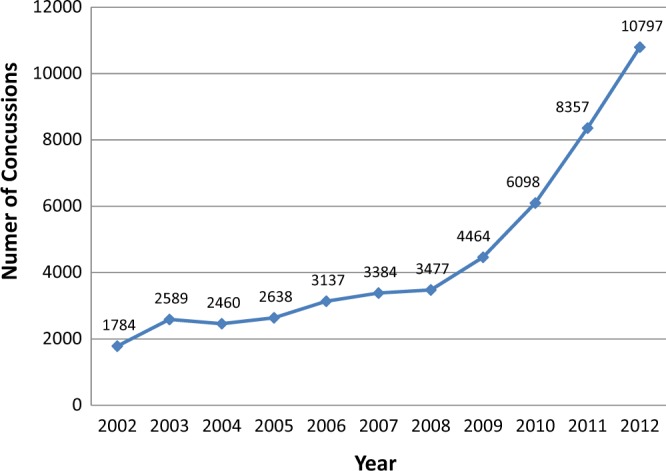
National estimates of concussions per year. Calculated national estimates are based on NEISS database probability samples, demonstrating increasing prevalence of concussions.
Figure 2.
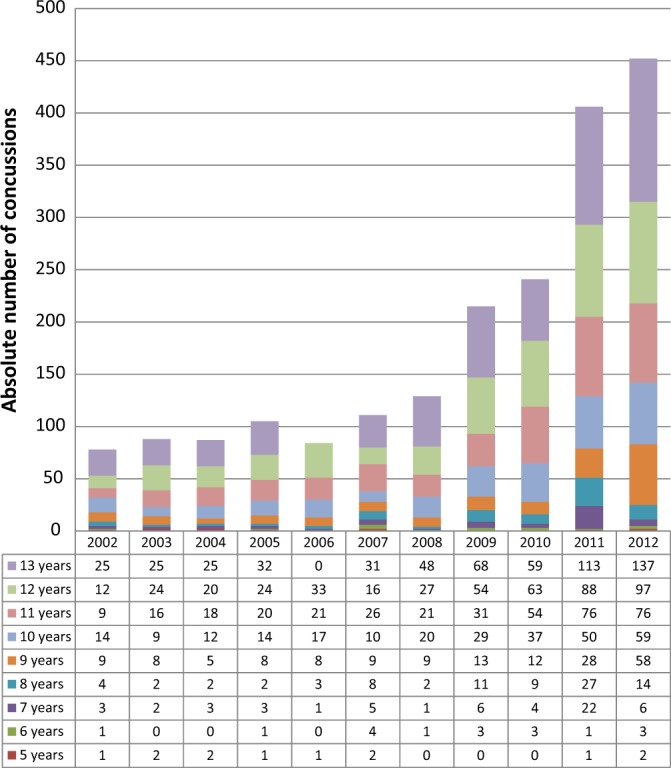
Total number of concussions by age. Concussion prevalence increased with age within each individual year as well as over the 11-year time frame studied.
The majority of concussions were treated in the outpatient setting after their initial evaluation. The vast majority (91.7%) were examined and released. There were 168 patients (8.3%) who were admitted and held for observation or transferred to another hospital for further treatment; 1 left against medical advice. The national estimate for those youth football players hospitalized for additional care was 2020 over this 11-year period.
The most common location for concussion to occur was at a place of recreation or sports (58%, n = 1180). Other locations were school (26.2%, n = 535), not recorded (15.3%, n = 310), and other (0.2%, n = 4).
Review of the narrative information on the mechanism and circumstances of injury revealed information on head-to-head injury mechanism (25.0%, n = 507), LoC (10.2%, n = 207), and concurrent fractures (0.5%, n = 11). Fractures of the skull (9.1%, n = 1), nasal bones (18%, n = 2), forearm (9.1%, n = 1), wrist (9.1%, n = 1), clavicle (9.1%, n = 1), thoracic spine (9.1%, n = 1), oral cavity (18%, n = 2), toe (9.1%, n = 1), and tibia/fibula (9.1%, n = 1) were recorded.
The total number of head-to-head injury mechanisms increased throughout the 11-year evaluation period (Figure 3). There was a correlation of r = 0.97 between the total number of concussions compared with the total number of head-to-head injuries over the 11-year time frame (Figure 4). The total number of players experiencing a concussion compared with the total number of players experiencing LoC over the 11-year time period had a correlation coefficient of r = 0.82. The total number of head-to-head injuries compared with the total number of players with LoC over this same time period demonstrated a correlation of r = 0.78 (Figure 4). At an alpha of 0.05, r > 0.618, which is considered to be statistically significant.
Figure 3.
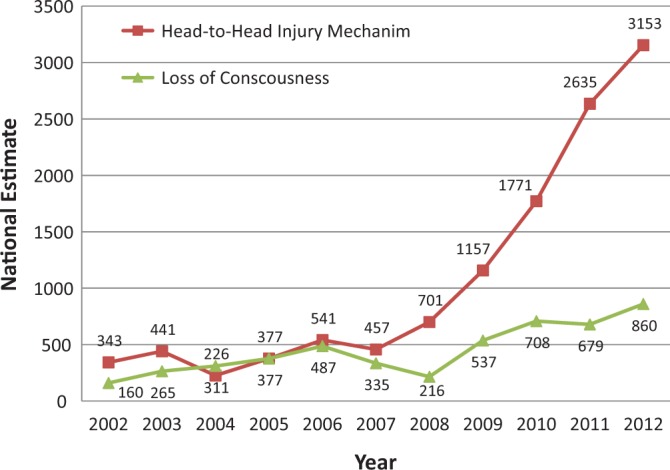
Head injury mechanism and loss of consciousness by year. Head-to-head collision injury mechanism increased over the 11-year time frame studied. Concurrent loss of consciousness with concussion increased only slightly over the 11-year time frame studied.
Figure 4.
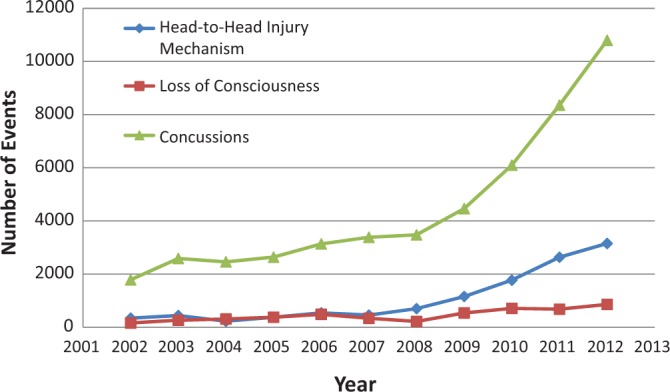
Number of concussions, loss of consciousness, and head-to-head mechanism of injury by year. Calculated national estimates of cases are displayed with Spearman correlation coefficients. Statistically significant correlations (r > 0.618 at α = 0.05) between all 3 groups were observed: concussion vs head-to-head mechanism of injury, r = 0.97; rate of concussion vs loss of consciousness, r = 0.82; and rate of head-to-head injury vs loss of consciousness, r = 0.78.
Subgroup analysis of the 8.3% of young football players admitted or transferred to another hospital (national estimate, 2020) demonstrated 44 (26.2%) of these concussions resulted from a head-to-head collision, 28 (16.7%) had an associated LoC, 18 (10.7%) occurred at practice, and 11 (6.5%) were tackled. There was 1 concomitant skull fracture. This subgroup of players, who were admitted or transferred, had a mean age of 11.6 years (median, 12 years; standard deviation [SD], 1.6 years).
Subgroup analysis of the 11 (national estimate, 313) players who sustained a concurrent fracture demonstrated 2 severe injuries, including of the skull and a thoracic spine compression fracture. This subgroup had a mean age of 10.9 years (median, 12 years; SD, 2.0 years). In this subgroup, 1 (9.1%) of these concussions resulted from a head-to-head collision, 4 (36.4%) had an associated LoC, and 2 (18.2%) occurred while being tackled.
Discussion
It has been estimated that 3.5 million young athletes participate in football each year in the United States prior to attending high school.3,10,19 This represents the largest population of football players at risk for concussion and the least studied. We queried the NEISS database for football-related concussions for a total of 11 years in youth football players aged 5 to 13 years in an attempt to evaluate this large but poorly understood cohort.
Our data includes the football-related concussions presented in the series by Bakhos et al1 and substantially increases both the number of years and pre–high school level athletes evaluated. Youth football athletes are as young as 5 years in the United States,18 leaving 3 years of concussion data out of the study by Bakhos et al.1 Additionally, we focused on a single sport, football, which has been highlighted recently for the risk of concussion and long-term sequelae of head injuries.4,5,13,17 The information on concussions sustained in this age group while playing football is not already available.
In our data set, there was an exponential increase in concussions sustained by youth football players when grouped by age and year (Figure 2). This correlates with increased musculoskeletal maturity of the athletes and greater forces transmitted during collisions between players. Additionally, the increased awareness of concussion and the number of young athletes participating in football can also contribute to the increasing frequency of concussions. However, even better education and a more uniform definition for concussion may provide a more accurate representation of the true number of concussions. Accurate records of concussions may lead to evaluation of the effectiveness of specific rule changes designed to minimize the incidence of concussions. The significant increase in concussions from 2008 to 2009 might reflect increased participation in sports, increased incidence of traumatic brain injury among participants, and/or increased awareness of the importance of early diagnosis of traumatic brain injury. Also, the disproportional increase in the number of hospital admissions compared with the increased number of concussions in 2008 to 2009 may suggest an increase in the level of aggressive play over these 2 years.
The correlation between the frequencies of concussions, head-to-head mechanism of injury, and loss of consciousness were statistically significant. The correlations (r > 0.618 at α = 0.05) between all 3 groups over the 11-year time period were r = 0.97 (concussion frequency vs head-to-head mechanism of injury), r = 0.82 (concussion frequency vs LoC), and r = 0.78 (head-to-head injury frequency vs LoC). The correlation was the strongest between total number of concussions and total number of head-to-head mechanism of injury (r = 0.97). This suggests that the rate of concussions may be limited if the prevalence of head-to-head impact is reduced. Changes in rules regarding head-to-head contact and/or helmets/equipment designed to limit head-to-head contact may result in a lower prevalence of concussion.
Of all football players, 91.7% were examined and released for outpatient follow-up while 8.3% required hospital admission. However, subgroup analysis on the cohort that was admitted demonstrated an equivocal ratio of head-to-head injury mechanisms (discharged group, 25.0%; admitted group, 26.2%) and a slightly increased ratio of LoC (discharged group, 10.2%; admitted group, 16.7%). This group did include a skull fracture (1 of the 2 severe injuries).
Fractures occurred in 11 players (national estimate, 313) concurrently with concussion. The fractures were reported in the narratives, which were brief. The narrative did not specifically say that the fractures occurred during the same collision that caused the head injury but it was assumed this was the case. The majority of these fractures involved the head (nasal bones, oral cavity, skull), demonstrating additional significant injuries to the head other than concussion. The fractures occurred in children with a mean age of 10.9 years, and closely coincided with our overall data set. Younger children may be at less risk for sustaining a fracture due to their having more elastic bones.
There were 2 serious injuries, defined as “no permanent functional disability but severe injury” by the National Catastrophic Injury project at the University of North Carolina,16 identified in the data set. The first was a 10-year-old Caucasian male who was tackled resulting in LoC, concussion, and skull fracture, for which he was admitted to the hospital. The second was a 12-year-old Caucasian male who was involved in a head-to-head collision resulting in LoC, concussion, and thoracic spine compression fracture. This patient was treated and discharged without being admitted or held for observation. Unfortunately, no additional information could be obtained from the NEISS database about the treatment or outcomes of these injuries. The 2 catastrophic injuries occurred in older children. National estimates calculated for the number of skull fractures and spinal fractures were 15.3 and 6, respectively. Older children may be at greater risk for catastrophic injury, but increased numbers would be needed before definitively making this conclusion.
The NEISS data set provides valuable epidemiologic information allowing analysis of the changes in prevalence of concussion in young football players. The narratives provide some additional information, but because of the heterogeneity of the information, their value is greatly diminished. Obtaining a large data set that can focus on these injuries could be invaluable in identifying risk factors and implementing safety measures such as innovative protective equipment (helmets, mouth guards, pads, etc), rule changes, and player and coaching education programs focusing on proper technique. These changes, designed to reduce the incidence of concussion, may subsequently be monitored to determine if they are effective in reducing the incidence of concussion in younger players at the national level.
One limitation of this study is that only athletes who presented to the ED with concussion were analyzed. It is possible that these patients are a minority of the total number of patients with concussion. It is also possible that the patients with concussions that presented to the ED were more severe (higher incidence of LoC, fractures, spine injury, etc). The external validity of this study is believed to be strong. However, it is possible that the less severe concussion cases did not present to EDs or had failed to be diagnosed, therefore possibly decreasing the generalizability of the results of this study to the general youth athlete population. This may be addressed in future studies by differentiating between athletes who suffer from a concussion and then go home versus those who present to the ED with more severe symptomatology (eg, vomiting, LoC, and deteriorating symptoms).
Despite these limitations, this data set is the only nationally representative stratified probability sample of concussion in youth football players in the United States. The stability of the data set allows changes over time to be monitored. Thus, these study results provide important information about risk of injury among the youth football population. The utility of these data, in the absence of ongoing community-level surveillance systems, is important for monitoring patterns of injury, identifying risk factors, and driving the development of evidence-based prevention programs. The development of a more comprehensive concussion database that contains specific injury descriptions and classifications could be even more valuable in the effort to prevent concussion.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–e556. [DOI] [PubMed] [Google Scholar]
- 2. Barkhoudarian G, Hovda DA, Giza CC. The molecular pathophysiology of concussive brain injury. Clin Sports Med. 2011;30:33–48. [DOI] [PubMed] [Google Scholar]
- 3. Daniel RW, Rowson S, Duma SM. Head impact exposure in youth football. Ann Biomed Eng. 2012;40:976–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fox M. Head injuries clearly linked to brain damage. NBC News. 2013. http://www.nbcnews.com/health/head-injuries-clearly-linked-brain-damage-8C11034117. Accessed October 25, 2013.
- 5. Gavett BE, Stern RA, McKee AC. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin Sports Med. 2011;30:179–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42:495–503. [PMC free article] [PubMed] [Google Scholar]
- 7. Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36:228–235. [PMC free article] [PubMed] [Google Scholar]
- 8. Guskiewicz KM, Bruce SL, Cantu RC. National Athletic Trainers’ Association position statement: management of sport-related concussion. J Athl Train. 2004;39:280–297. [PMC free article] [PubMed] [Google Scholar]
- 9. Guskiewicz KM, Valovich McLeod TC. Pediatric sports-related concussion. PM R. 2011;3:353–364. [DOI] [PubMed] [Google Scholar]
- 10. Guskiewicz KM, Weaver NL, Padua DA, Garrett WE ., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. [DOI] [PubMed] [Google Scholar]
- 11. Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47:15–26. [DOI] [PubMed] [Google Scholar]
- 12. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375–378. [DOI] [PubMed] [Google Scholar]
- 13. Lau BC, Collins MW, Lovell MR. Sensitivity and specificity of subacute computerized neurocognitive testing and symptom evaluation in predicting outcomes after sports-related concussion. Am J Sports Med. 2011;39:1209–1216. [DOI] [PubMed] [Google Scholar]
- 14. Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39:958–963. [DOI] [PubMed] [Google Scholar]
- 15. Lowrey KM. Summary Matrix of State Laws Addressing Concussions in Youth Sports. St Paul, MN: The Network for Public Health Law; 2012. [Google Scholar]
- 16. Mueller FO, Cantu RC. Catastrophic Sports Injury Research, 28th Annual Report. Chapel Hill, NC: University of North Carolina; 2010. [Google Scholar]
- 17. Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery. 2005;57:128–134. [DOI] [PubMed] [Google Scholar]
- 18. Pop Warner Little Scholars. 2013 Season age/weight matrix. http://www.popwarner.com/Assets/01-assets/admin/2013Forms/2013+Age-Weight.pdf. Accessed September 24, 2013.
- 19. Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282:958–963. [DOI] [PubMed] [Google Scholar]
- 20. Prins ML, Hales A, Reger M, Giza CC, Hovda DA. Repeat traumatic brain injury in the juvenile rat is associated with increased axonal injury and cognitive impairments. Dev Neurosci. 2010;32:510–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160:937–944. [DOI] [PubMed] [Google Scholar]
- 22. Shrey DW, Griesbach GS, Giza CC. The pathophysiology of concussions in youth. Phys Med Rehabil Clin N Am. 2011;22:577–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sim A, Terryberry-Spohr L, Wilson KR. Prolonged recovery of memory functioning after mild traumatic brain injury in adolescent athletes. J Neurosurg. 2008;108:511–516. [DOI] [PubMed] [Google Scholar]
- 24. Schroeder T, Ault K. The NEISS Sample (Design and Implementation) 1997 to Present. Bethesda, MD: Division of Hazard and Injury Data Systems, US Consumer Product Safety Commission; 2001. http://www.cpsc.gov/PageFiles/106617/2001d011-6b6.pdf. Accessed October 22, 2013. [Google Scholar]
- 25. Zuckerman SL, Lee YM, Odom MJ, Solomon GS, Forbes JA, Sills AK. Recovery from sports-related concussion: days to return to neurocognitive baseline in adolescents versus young adults. Surg Neurol Int. 2012;3:130. [DOI] [PMC free article] [PubMed] [Google Scholar]


