Abstract
Background:
Diagnosis of pectoralis major tears early in the acute phase is important for optimizing surgical repair and outcomes. However, physical examination of pectoralis major injuries can be misleading, often resulting in a potentially detrimental delay in surgical treatment.
Purpose:
To establish and validate a quantifiable clinical diagnostic test for structurally significant pectoralis major tears.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
A total of 50 healthy male participants (mean age, 43.3 ± 11.9 years) with normal uninjured pectoralis major anatomy were examined. Digital photographs of all participants were taken in the “military press” starting position (90° of shoulder abduction, 90° of shoulder external rotation). The length between the ipsilateral nipple and the apex of the pectoralis major muscle curvature along the anterior axillary fold, known as the pectoralis major distance, was measured bilaterally. Two orthopaedic surgeons measured all photographs on 2 separate occasions. The pectoralis major index (PMI) was calculated as a ratio of pectoralis major distance values to establish normal values. The PMI was also calculated in a cohort of 19 male patients (mean age, 33.8 ± 6.8 years) with a pectoralis major rupture to assess the diagnostic utility of this novel quantifiable physical examination technique.
Results:
Mean (± standard deviation) PMI for the uninjured group was 1.0 ± 0.07. A diagnostic threshold of a PMI <0.9 resulted in a sensitivity of 79%, specificity of 98%, and overall accuracy of 93% in identifying structurally significant pectoralis major ruptures. There was no correlation between PMI and age or activity level, including participation in sports and/or weight training. The PMI technique demonstrated good to excellent intrarater reliability (intraclass correlation coefficient [ICC] = 0.82, 0.74) and interrater reliability (ICC = 0.63, 0.76).
Conclusion:
The PMI technique is a simple, quantifiable, and accurate clinical diagnostic test for structurally significant pectoralis major tears. Routine application of the PMI technique by clinicians may improve accurate identification of structurally significant rupture and expedite referral to a surgical specialist for optimal treatment and outcome.
Keywords: diagnosis, pectoralis major, tendon rupture, shoulder
The pectoralis major (PM) is a broad multipennate muscle that functions as an adductor, flexor, and internal rotator of the humerus as well as a dynamic stabilizer of the shoulder. Indirect trauma is the main cause of PM injury.7 The PM muscle is most vulnerable when a force is applied during an eccentric contraction with the shoulder in a position of abduction and external rotation.3,19 Rupture of the PM occurs predominately in males, with the incidence of tears rising substantially in the past 20 years, which is in part because of the increase in indirect injuries associated with weight lifting, specifically the bench press maneuver.3,12,14,17 This trend is likely to continue as fitness and sports-related activities, including weight training, progressively increase in popularity.
Accurate and rapid diagnosis of structurally significant PM tears is important, especially in cases of structurally significant or total rupture, when surgical management is generally advised to prevent a functional loss of strength and to permit return to sports activities.1,9,12,14 Moreover, an untreated significant tear may permanently disrupt the contour of the anterior chest, resulting in poor cosmesis and potentially reduced patient satisfaction.1,14 Early referral and a prompt diagnosis are crucial, as surgical repair of chronic injuries may necessitate increased surgical exposure and dissection because of adhesions and muscle retraction. Delayed surgical treatment may compromise the length-tension relationship of a repair procedure, heighten the need for tissue grafts, and affect overall rates of healing and quality of overall clinical outcome.7,18
Despite the clinical urgency, and even with clinical suspicion, diagnosing PM tears in the clinical setting can be problematic, with physical examination results being difficult to interpret. With retraction of the PM muscle, a swollen, tender mass may be palpable medially and there may be a loss of the anterior axillary fold.6,12–14 However, the presence of a palpable or visible defect is not a reliable physical finding on its own. Hemorrhage may obscure the loss of the anterior axillary fold, and the fascial covering of the PM muscle may remain intact, masking the underlying tear.2,16 Further to these physical signs, tears of the PM are also associated with a subtle decrease in adduction strength,6 yet this can be difficult to identify in the acutely injured patient because of pain. A need currently exists for a simple accurate clinical test that can be used by clinicians to aid in the diagnosis of structurally significant PM tears.
The purpose of this study was to develop an accurate quantifiable clinical diagnostic test for structurally significant PM tears to enhance patient referral to the orthopaedic surgeon for optimal surgical management in a timely fashion. We refer to this newly described surface anatomy parameter as the pectoralis major distance, which, when known for both sides, can be used to calculate the pectoralis major index (PMI). The primary objectives of this study were to determine the PMI values that constitute normal PM anatomy, to establish an effective cutoff value diagnostic of structurally significant rupture, and to evaluate the diagnostic utility of this measure by determining sensitivity, specificity, positive predictive value, negative predictive value, and overall accuracy. We hypothesized that there would be a quantifiable difference in the PM anatomy of patients with a structurally significant PM rupture.
Materials and Methods
Fifty-one healthy male participants were recruited for the normal uninjured PM group (control) following institutional research ethics board approval. A testing station was established, and participants were screened for eligibility. To be included in the uninjured PM group, participants had to be male and older than 18 years. Females were not included since the clinical entity of PM rupture has been exclusively described in males. Participants were excluded from the uninjured group if they sustained a previous PM injury or were unable to assume the standardized testing position for PM examination. One participant was excluded from this group on suspicion of previous PM injury, resulting in a total of 50 participants in the uninjured PM group.
Participants completed a short questionnaire containing demographics, activity level, and history of PM injury or surgery. A high-definition digital photograph of each participant was obtained in a standardized position (subject standing 6 feet away, with the camera at chest level). Participants were asked to maintain a standardized testing position, referred to as the “military press” starting position: 90° of shoulder abduction and 90° of shoulder external rotation for both upper extremities (Figure 1). The choice of this testing position is seen by us as critically important to the utility of the test, since we are attempting to maximize the distance between the origin and insertion of the PM to passively reveal a significant structural disconnect. We feel the medial surface anatomy location should be low and medial, if not central (and could just as easily have been the xiphoid process), since not only are the lower sternal head segments (that contribute to the posterior tendon layer of the PM) most commonly torn, they also contribute the most to the normally bulky and curved prominence of the anterior axillary fold contour of the PM, which is enhanced in the “military press” starting position. Numerous reports of PM diagnosis and treatment show clinical images of the chest with the arm adducted if not internally rotated. This position hides any scars, closes up and covers the anterior axillary fold, and allows the origin to be much closer to the insertion of the PM muscle, thereby masking any traumatic deformity and/or quality of its postoperative restoration.
Figure 1.

Preoperative photograph of a chronic right pectoralis major rupture 84 days after injury. Alteration due to a structurally significant rupture is apparent in the visual appearance of the anterior axillary fold on the injured side (arrow).
Patients who were referred to the principal investigator (A.W.E.) between July 2010 and August 2012 for clinical assessment of a PM injury were identified from a prospectively gathered database. The database contained demographic and clinical information as well as digital photographs of the PM injury in the “military press” starting position. To have been included in the injured PM group, participants had to be male, older than 18 years, and had a structurally significant tear of the PM (determined definitively at the time of surgical exploration). The extent of each structural injury was described based on the classification system by ElMaraghy and Devereaux.7 Participants were excluded from the injured PM group if they were unable to assume the standardized testing position, if the occurrence of a structurally significant PM tear could not be determined definitively at the time of surgical exploration, or if the surface landmarks to determine the PMI were obscured from either previous injury or surgery. We identified 24 patients who were referred for PM injury, and of these, 19 patients consented to surgical exploration and had sufficient information to be utilized for this study and were designated the injured PM group.
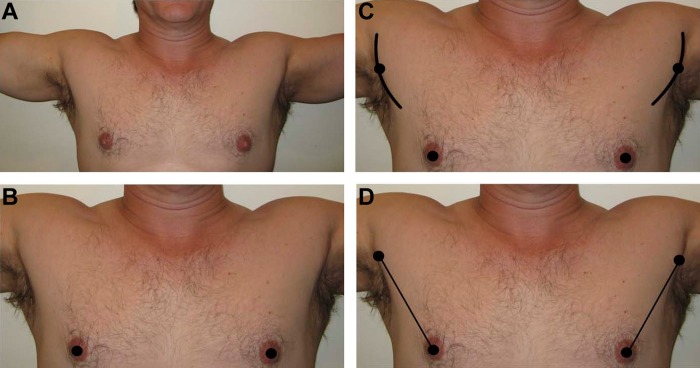
Digital photographs from both groups, uninjured PM and injured PM, were de-identified and randomly ordered using a computer-generated random number table. Two raters measured each photograph on 2 separate occasions that were at least 2 weeks apart. Rater 1 was an orthopaedic surgeon with more than 12 years of experience, and rater 2 was an orthopaedic surgeon who was in the process of completing fellowship training. The length (in centimeters, to 1 decimal place) of a straight line from the nipple to the apex of the PM contour along the anterior axillary fold, known as the pectoralis major distance (PMD), was recorded bilaterally for each participant (Figure 2). The PMI was expressed as the value (to 1 decimal place) of a calculated ratio of the 2 PMD measurements on the digital photograph (dominant arm over nondominant arm in uninjured participants and injured side over uninjured side in patients with a PM injury).
Figure 2.
Description of the technique to determine the pectoralis major index (PMI). (A) The patient positions both arms in the “military press” starting position (shoulders in 90° abduction, 90° external rotation). (B) Both nipples are marked. (C) The pectoralis major contour is followed along the anterior axillary fold and the most laterally prominent apex is marked on both sides. (D) The distance along a straight line between the nipple and the apex (the pectoralis major distance [PMD]) is measured to 1 decimal place, and the PMI is calculated as the injured-side PMD over the uninjured-side PMD.
Descriptive statistics (mean, standard deviation, frequency) were used to describe the demographics of both groups. Inter- and intrarater reliabilities were measured using intraclass correlation coefficients (ICCs) with associated 95% confidence intervals. A 2-way mixed, absolute agreement, single measure ICC was used. Values of ICC were interpreted as ICC ≥0.75 (excellent); 0.40 ≥ ICC > 0.75 (fair to good), and ICC <0.40 (poor).8 With an ICC value meeting the threshold of 0.75, the 2 sets of measurements made by the experienced orthopaedic surgeon were averaged to obtain an overall mean PMI value for each photograph. A diagnostic threshold was set at a PMI value 2 standard deviations below the established mean of the uninjured PM group. To assess the diagnostic utility of this physical examination technique, the diagnostic threshold was used to categorize the injured and uninjured PM groups as PMI positive for a structurally significant PM tear or PMI negative for no tear. PMI measurements of injured and uninjured participants were compared with the definitive tear status to determine diagnostic values of specificity, sensitivity, positive predictive value, negative predictive value, and overall accuracy. Normality was assessed using the Shapiro-Wilk test. The Mann-Whitney U test was used to identify differences among means of continuous variables. Pearson r and point-biserial correlation coefficients were used to indicate correlations between PMI and age, arm dominance, and activity level. Statistical analyses were performed using IBM SPSS Statistics for Windows version 21.0 (IBM Corp, Armonk, New York, USA) and Excel 2013 (Microsoft Corp, Redmond, Washington, USA). A P value less than .05 was statistically significant.
Results
Fifty participants met the inclusion criteria in the uninjured PM group (mean age, 43.3 ± 11.9 years) (Table 1). All participants were male. Mean (± standard deviation) PMI for the uninjured PM group was 1.0 ± 0.07. There was no correlation between PMI and age or activity level, including participation in sports and/or weight training. However, there was a correlation between PMI and hand dominance, with left hand–dominant participants displaying lower PMI values (P = .01).
TABLE 1.
Patient Demographics of the Participants in the Uninjured and Injured Groupsa
| Uninjured PM | Injured PM | |
|---|---|---|
| Subjects, n | 50 | 19 |
| Age, mean ± SD, y | 43.3 ± 11.9 | 33.8 ± 6.8 |
| Smoker, n | 8 | 3 |
| Steroids, n | 2 | 1 |
| Arm dominance, n (INJb) | ||
| Right | 44 (n/a) | 16 (6) |
| Left | 6 (n/a) | 3 (1) |
aINJ, injured; n/a, not applicable; PM, pectoralis major; SD, standard deviation.
bDominant side injured.
Nineteen patients were included in the injured PM group (mean age, 33.8 ± 6.8 years). All 19 patients underwent surgical exploration and were found to have structurally significant tears that required repair. Classification of tears was made according to timing, location, and extent in terms of both thickness and width (Table 2).7 The mean (± standard deviation) PMI for the injured PM group was 0.7 ± 0.17. There was a significant difference in PMI (P < .001) between uninjured and injured groups. There was not a significant difference in PMI values between any of the tear classification categories (timing/location/extent) determined at the time of surgical repair.
TABLE 2.
Tear Classification of Participants in the Injured Groupa
| Tear Classification | No. of Patients |
|---|---|
| A-2-Pp-I | 1 |
| A-2-Pp-C | 3 |
| A-2-F-C | 3 |
| C-2-Pp-I | 4 |
| C-2-Pp-C | 4 |
| C-2-F-I | 1 |
| C-2-F-C | 3 |
aA, acute; C, chronic; 2, at or between the musculotendinous junction and tendinous insertion; Pp, partial posterior; F, full-thickness; I, incomplete; C, complete.
The diagnostic threshold was set at 0.9, a value that was 2 standard deviations below the mean determined for the uninjured patients. Fifteen of 19 patients in the injured group had a positive PMI prediction for a structurally significant PM tear (Table 3). Using PMI as a diagnostic indicator of a structurally significant PM tear resulted in sensitivity of 79%, specificity of 98%, positive predictive value of 94%, negative predictive value of 92%, and overall accuracy of 93% (Table 4).
TABLE 3.
Diagnostic Results of PMI (Threshold PMI <0.9)
| Actual | |||
|---|---|---|---|
| No Tear | Tear | ||
| PMI prediction | ≥0.9, no tear | 49 | 4 |
| (true negative) | (false negative) | ||
| <0.9, tear | 1 | 15 | |
| (false positive) | (true positive) | ||
TABLE 4.
Utility of PMI as a Diagnostic Testa
| Value, % | Formula | |
|---|---|---|
| Sensitivity | 79 | TP/(TP + FN) |
| Specificity | 98 | TN/(FP + TN) |
| Positive predictive value | 94 | TP/(TP + FP) |
| Negative predictive value | 92 | TN/(TN + FN) |
| Overall accuracy | 93 | (TP + TN)/(TP + FP + FN + TN) |
aFN, false negative; FP, false positive; PMI, pectoralis major index; TN, true negative; TP, true positive.
The intrarater reliability was good to excellent for both raters, with the more experienced orthopaedic surgeon demonstrating a higher ICC of 0.82 (Table 5). The interrater reliability was also good to excellent, with a higher ICC of 0.76 for the second set of measurements (Table 5).
TABLE 5.
Reliability of Pectoralis Major Index Measurementsa
| Examiner | ICC | 95% CI | |
|---|---|---|---|
| Lower Bound | Upper Bound | ||
| Intrarater reliability | |||
| Rater 1 | 0.82 | 0.72 | 0.88 |
| Rater 2 | 0.74 | 0.61 | 0.83 |
| Interrater reliability | |||
| Rater 1 vs rater 2 (first measurement) | 0.63 | 0.47 | 0.76 |
| Rater 1 vs rater 2 (second measurement) | 0.76 | 0.63 | 0.84 |
aCI, confidence interval; ICC, intraclass correlation coefficient.
Discussion
The accurate and rapid diagnosis of structurally significant PM ruptures is vital to patient care, yet a quantifiable and validated clinical diagnostic test does not currently exist. With the use of this newly described PMI test, clinicians can accurately and confidently identify a structurally significant PM rupture, thereby hopefully expediting referral to a surgical specialist and minimizing treatment complexity and improving outcomes.
The mechanism of injury for PM rupture is most commonly indirect with the shoulder abducted and externally rotated, such as in the bench press position.3 In this position, the inferior sternal head fibers are under particular tensile stress and are more prone to rupture.19 The inferior muscular segments have a mechanical disadvantage at the end of the eccentric phase when their fibers are maximally stretched and respond disproportionately, causing them to be susceptible to rupture under high loads.19 Propagation of the tear to become complete can occur with ongoing or excessive load. These PM segments also contribute most to the readily identifiable curved muscle bulk of the anterior axillary contour.
None of the previously described physical examination features reported with PM injury are quantifiable, nor are they always reliable. Pochini et al14 described the “S” sign to characterize this defect in the appearance of the axillary fold. Chronic tears may also present with “webbing,” an accentuation of the inferior border of the deltoid.19 Hematoma may fill the gap in the anterior axillary fold, allowing the defect to be visible only when the arm is fully abducted or adducted.2,16 In acute tears, hematoma and edema can also contribute to the so-called “dropped nipple,” where the ipsilateral nipple sits and points more downward than the contralateral nipple. Magnetic resonance imaging may be useful in identifying PM rupture5,6,20 but may be unable to accurately identify partial-thickness PM tears and may not be overly helpful in preoperative planning.2–4,15 Because of the rarity of this condition, without a definitive test for PM rupture, an inexperienced clinician may underestimate the severity of the injury or miss the diagnosis completely.
Confident, timely diagnosis of structurally significant PM ruptures without the time delay and associated expense of “confirmatory” imaging is important in the management of PM injuries. Despite the importance of early diagnosis and referral, 63% of patients with PM ruptures in this study were delayed in referral, and despite expedited care, underwent surgical exploration more than 6 weeks after the initial injury, which is similar to rates of missed or late diagnosis reported by other studies.1,3,11 The PMI technique has the potential to reduce the number of late diagnoses, as 79% of patients with a PM rupture in this study had a true positive result. Although few studies have suggested otherwise,9,17 it is generally accepted that repair of acute PM ruptures results in better outcomes than repair of chronic injuries.1,3,4,10,12,15 A timely diagnosis can expedite surgical treatment, avoiding muscle retraction, adhesions, and atrophy that can occur even 6 weeks after injury.13,19 Residual cosmetic defects and strength deficits may not be acceptable to active individuals, emphasizing the importance of treating PM injuries in the acute stage through urgent referral to a specialist.
This study introduces the concept of quantifying the alteration in the anterior axillary fold contour of the PM, which is revealed by positioning the PM insertion maximally away from its origin. The study demonstrates the diagnostic utility of the PMI test to accurately identify patients with a structurally significant PM tear. The PMI technique is intended to be used as a diagnostic indicator for confident evaluation and urgent triage to a surgical specialist. With a specificity of 98%, the risk of misdiagnosis is very low using PMI as the initial indicator of suspected PM rupture. With a sensitivity of 79%, the risk of missed diagnosis is also relatively low, which is of extreme importance in identifying PM ruptures in the acute stage.
Although the PMI test can be used to identify patients with structurally significant injury to the PM, it could not distinguish between the various tear classification categories of location and extent. This is not surprising, given that in our experience, the detailed structurally pathologic information necessary to correctly classify the location and extent category of a particular tear cannot even be visualized on MRI and can only be determined accurately at the time of surgical exploration and repair. Although there was a correlation between hand dominance and PMI, the reason for this relationship is unknown. Compared with other muscular ruptures that occur more frequently in the dominant arm, such as a distal biceps tendon rupture, PM ruptures occur more in the nondominant arm; we are unsure as to the reason for this, but it is interesting to note. Identification of anatomic landmarks used in the PMI technique may be simpler in the injured population. As the bench press maneuver used in weight lifting is the main cause of PM rupture, this population tends to be more physically fit with better muscle definition. This is actually a positive attribute of the technique, as these are the patients that will likely present to the clinician with suspected PM injury.
Identification of the apex of the curved anterior axillary fold may present a challenge initially, and the examiner should take care in identifying the appropriate location to increase accuracy of the test results. Like all physical examination techniques, the ability to visually and palpably identify physical landmarks may improve with practice, which is demonstrated by the higher ICC value for interrater reliability in the second set of measurements made by both testers. In addition, the more experienced orthopaedic surgeon demonstrated more reliable measurements, suggesting that with more clinical experience, the ease and accuracy of identifying physical landmarks may also improve.
The main limitation of this study was the use of digital photographs to measure the PMI. Palpation is important in the identification of anatomic landmarks, with the use of 2-dimensional images there was a lack of tactile feedback. Patient positioning was also problematic with the use of photographs as the arm may be slightly rotated and lighting may not be ideal. While the use of photographs presents some pitfalls, we believe that it was the most appropriate way to establish normal PMI values and to compare normal with injured participants in a standardized manner while keeping the assessor blinded. Another potential limitation is the selection of the nipple as the medial anatomic landmark, which may introduce some variability into the PMD measurements as there is the potential for a difference in nipple position between sides. Any consistent low midline anatomic landmark, such as the xiphoid process, could have been selected and would likely provide a similar diagnostic difference in surface anatomy; however, this was not specifically tested. Also, all participants in the study were male, as PM rupture is a male-dominant injury, and thus it is difficult to generalize the results to the population as a whole.
Conclusion
The pectoralis major index is a simple, quantifiable, and accurate clinical diagnostic test that can be used by clinicians to accurately diagnose structurally significant PM ruptures. It is hoped that accurate diagnosis in the acute stage can expedite referral to a surgical specialist and hasten definitive management, allowing for a technically simpler procedure and improved outcomes.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Aarimaa V, Rantanen J, Heikkila J, Helttula I, Orava S. Rupture of the pectoralis major muscle. Am J Sports Med. 2004;32:1256–1262. [DOI] [PubMed] [Google Scholar]
- 2. Alho A. Ruptured pectoralis major tendon. A case report on delayed repair with muscle advancement. Acta Orthop Scand. 1994;65:652–653. [DOI] [PubMed] [Google Scholar]
- 3. Bak K, Cameron EA, Henderson IJP. Rupture of the pectoralis major: a meta-analysis of 112 cases. Knee Surg Sports Traumatol Arthrosc. 2000;8:113–119. [DOI] [PubMed] [Google Scholar]
- 4. Bal GK, Basamania CJ. Pectoralis major tendon ruptures: diagnosis and treatment. Tech Shoulder Elbow Surg. 2005;6:128–134. [Google Scholar]
- 5. Carrino JA, Chandnanni VP, Mitchell DB, Choi-Chinn K, DeBerardino TM, Miller MD. Pectoralis major muscle and tendon tears: diagnosis and grading using magnetic resonance imaging. Skeletal Radiol. 2000;29:305–313. [DOI] [PubMed] [Google Scholar]
- 6. Connell DA, Potter HG, Sherman MF, Wickiewicz TL. Injuries of the pectoralis major muscle: evaluation with MR imaging. Radiology. 1999;210:785–791. [DOI] [PubMed] [Google Scholar]
- 7. ElMaraghy AW, Devereaux MW. A systematic review and comprehensive classification of pectoralis major tears. J Shoulder Elbow Surg. 2011;21:412–422. [DOI] [PubMed] [Google Scholar]
- 8. Fleiss JL. The Design and Analysis of Clinical Experiments. New York: Wiley; 1986. [Google Scholar]
- 9. Hanna CM, Glenny AB, Stanley SN, Caughey MA. Pectoralis major tears: comparison of surgical and conservative treatment. Br J Sports Med. 2001;35:202–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hasegawa K, Schofer JM. Rupture of the pectoralis major: a case report and review. J Emerg Med. 2010;38:196–200. [DOI] [PubMed] [Google Scholar]
- 11. Jones MW, Matthews JP. Rupture of pectoralis major in weight lifters: a case report and review of the literature. Injury. 1988;19:219. [DOI] [PubMed] [Google Scholar]
- 12. Kakwani G, Matthews JJ, Kumar KM, Pimpalnerkar A, Mohtadi N. Rupture of the pectoralis major muscle: surgical treatment in athletes. Int Orthop. 2007;31:159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McEntire JE, Hess WE, Coleman SS. Rupture of the pectoralis major muscle: a report of eleven injuries and review of fifty-six. J Bone Joint Surg Am. 1972;54:1040–1046. [PubMed] [Google Scholar]
- 14. Pochini A, Ejnisman B, Andreoli CV, et al. Pectoralis major muscle rupture in athletes: a prospective study. Am J Sports Med. 2010;38:92–98. [DOI] [PubMed] [Google Scholar]
- 15. Provencher MT, Handfield K, Boniquit NT, Reiff SN, Sekiya JK, Romeo AA. Injuries to the pectoralis major muscle: diagnosis and management. Am J Sports Med. 2010;38:1693–1705. [DOI] [PubMed] [Google Scholar]
- 16. Rijnberg WJ, van Linge B. Rupture of the pectoralis major muscle in body-builders. Arch Orthop Trauma Surg. 1993;112:104–105. [DOI] [PubMed] [Google Scholar]
- 17. Schepsis AA, Grafe MW, Jones HP, Lemos MJ. Rupture of the pectoralis major muscle. Outcome after repair of acute and chronic injuries. Am J Sports Med. 2000;28:9–15. [DOI] [PubMed] [Google Scholar]
- 18. Shubin Stein BE, Potter HG, Wickiewicz TL. Repair of chronic pectoralis major ruptures. Tech Shoulder Elbow Surg. 2002;3:174–179. [Google Scholar]
- 19. Wolfe SW, Wickiewicz TL, Cavanaugh JT. Ruptures of the pectoralis major muscle. An anatomic and clinical analysis. Am J Sports Med. 1992;20:587–593. [DOI] [PubMed] [Google Scholar]
- 20. Zvijac JE, Schurhoff MR, Hechtman KS, Uribe JW. Pectoralis major tears: correlation of magnetic resonance imaging and treatment strategies. Am J Sports Med. 2006;34:289–294. [DOI] [PubMed] [Google Scholar]