Abstract
Background:
Lateral ankle sprain (LAS) is one of the most common injuries in sports. Despite extensive research, intrinsic factors that predict initial and recurrent noncontact LAS remain undefined.
Purpose:
To identify the predictive factors of initial and recurrent noncontact LAS, focusing on ankle flexibility and/or alignment in collegiate athletes.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 191 athletes were assessed during the preseason for factors predictive of noncontact LAS. The baseline measurements included weightbearing dorsiflexion range of motion (ROM), leg-heel angle, foot internal rotation angle in plantar flexion, classification according to the mortise test, and navicular–medial malleolus (NMM) distance. Occurrence of noncontact LAS and participation in practice and games were prospectively recorded for 11 months.
Results:
Of the 191 athletes assessed, 169 (145 males, 24 females) completed the study; 125 athletes had a history of ankle sprain. During the observational period, 16 athletes suffered noncontact LAS (0.58 per 1000 athlete-exposures) consisting of 4 initial sprains and 12 recurrences. The hazard ratio estimated by a Cox regression analysis showed that athletes with an NMM distance ≥4.65 cm were 4.14 times more likely to suffer an initial noncontact LAS than were athletes with a shorter NMM distance (95% confidence interval, 1.12-14.30) and that athletes with a weightbearing dorsiflexion ROM >49.5° were 1.12 times as likely to suffer a recurrent noncontact LAS compared with athletes with a lower ROM (95% confidence interval, 1.05-1.20).
Conclusion:
NMM distance predicts initial noncontact LAS, and weightbearing dorsiflexion ROM predicts recurrent noncontact LAS.
Keywords: noncontact lateral ankle sprain, ankle dorsiflexion, navicular–medial malleolus distance, collegiate athlete
Lateral ankle sprain (LAS) is one of the most common injuries in competitive sports and recreational activities. Approximately 23,000 cases of LAS occur daily, and the annual indirect medical cost of treating LAS is $1.1 billion in the United States.17,20,23 The rate of recurrent ankle sprain is more than 40%. Predominant symptoms for the ankle are pain and crepitus, with 1 to 3 reinjuries, and unstable feeling, with 4 or more reinjuries.42 Thus, repeated ankle sprain leads to chronic ankle instability (CAI).11,33,42 Furthermore, the development of osteoarthritis in patients with long-standing CAI is thought to be about 80%, and some cases require surgical treatment.9,19,28 Therefore, the determination of factors that predict LAS and the development of an effective LAS prevention program are required.
Many studies have been performed to determine whether certain intrinsic factors can predict LAS. The predictive intrinsic factors of LAS proposed by these studies include anatomic characteristics,5,24 functional deficits in isokinetic strength,4,21 flexibility,2,12 joint position sense,37,40 muscle reaction time,4 balance-postural sway,41 gait mechanics,39 limb dominance,4,8 previous ankle sprains,2,21 weight, and body mass index (BMI).24,31 However, no consensus has been reached on the predictive intrinsic factors. Moreover, most previous studies have not distinguished between contact and noncontact injuries. Though injury mechanisms with different risk factors should be distinguished in prospective cohort studies of sports injuries,29,36 only a few studies have investigated factors specifically predictive of noncontact LAS.8,12,21,31 These studies suggested that previous ankle sprain12,21,31 or BMI21,31 can predict noncontact LAS, while Fousekis et al8 reported that previous ankle sprain and BMI do not predict noncontact LAS. Additionally, flexibility,8,12 ankle joint instability,8,12 generalized hypermobility,12 muscle strength,8,21 and static balance12 were not identified as predictive factors. Therefore, the intrinsic predictive factors in noncontact LAS are still undefined, and further research is needed.
Balance board training in a single-limb stance decreases the incidence of recurrent ankle sprain in athletes with a history of previous ankle sprain.1,20,23,30,32 In contrast, it does not prevent initial ankle sprain in athletes without previous ankle sprain.20,32 Because single-leg balance is disturbed in patients with CAI,22,25,38 balance training was speculated to improve proprioception, thereby protecting against recurrent injury.21 No effective training to prevent initial ankle sprain has been proposed at present, and potential predictive factors differentiating initial and recurrent LAS should be identified. Talocrural stability is supported by bony conformity, rear foot alignment, flexibility, and neuromuscular control,10,11 among which only the neuromuscular components have been studied in the literature. Therefore, the purpose of this case-control study was to identify the predictive factors of initial and recurrent noncontact LAS in collegiate athletes. We hypothesized that bony conformity and flexibility of the talocrural joint or rear foot alignment would predict initial LAS.
Methods
Subjects
This study protocol was approved by the local institutional review board. All subjects who met the specific selection criteria signed an institutional review board–approved informed consent form prior to participation. Intercollegiate athletes were recruited. Inclusion criteria were (1) intercollegiate athlete status and participation in jumping or cutting motions and (2) age 18 to 22 years. Both sexes were included. Exclusion criteria were (1) unavailability to participate in daily training or practice for personal reasons (eg, considering to quit the team); (2) injury, illness, or medical risk; (3) communication disability; or (4) mental disturbance diagnosed by psychiatrist.
A total of 191 athletes aged 18 to 21 years participated in this study. The breakdown by sex and sport played was 13 males in basketball, 17 males and 16 females in badminton, 17 females in volleyball, 39 males in soccer, and 89 males in baseball.
Protocol
During the preseason period, all athletes underwent baseline measurements and completed a questionnaire regarding history of previous LAS. The athletes were followed for 11 months (48 weeks) to monitor the occurrence of ankle sprain and participation in practice or games. At the end of the follow-up period, analyses were performed to calculate the risk of injury and define the risk factors for both initial and recurrent noncontact LAS (Figure 1). All injured athletes reported their injury mechanisms (ie, contact/noncontact or inversion/eversion) and the severity of the sprain along with all necessary details. If necessary, they visited a medical institution to rule out fractures. Athletes who suffered contact ankle sprains, defined as an injury involving physical contact at any body part during the injurious action, were not included in the analyses. LAS was defined as an ankle injury with an inversion mechanism that caused the player to miss at least 1 game or practice. Hours participating in practice or games were recorded by a club manager and were reported to the researchers monthly.
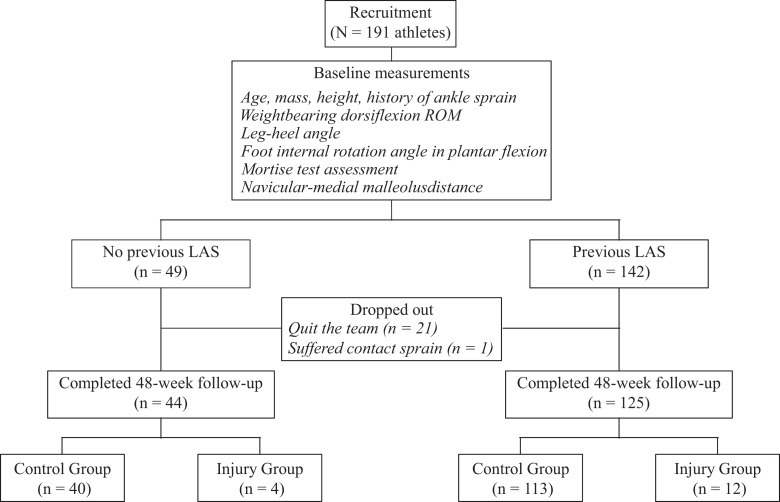
Figure 1.
Flowchart of the study protocol. LAS, lateral ankle sprain; ROM, range of motion.
Data Collection
Baseline measurements included weightbearing dorsiflexion range of motion (ROM), leg-heel angle (LHA), foot internal rotation angle in plantar flexion, mortise test assessment, and navicular–medial malleolus (NMM) distance (Figure 2). In addition, age, mass, height, history of ankle sprain, and sporting events were reported. The data for both sides of the body were collected, and the sequence in which measurements were taken was randomly decided. Each measurement was performed by trained examiners.
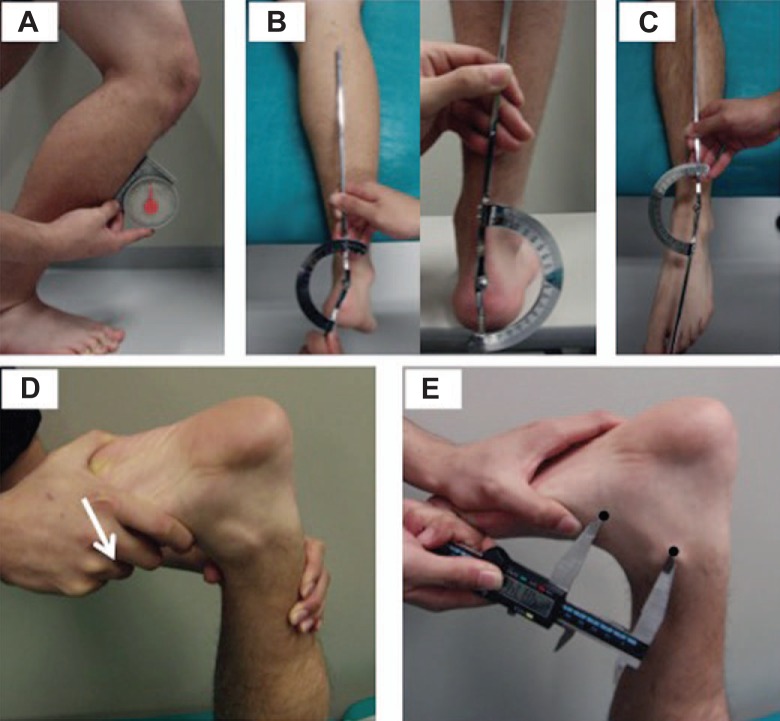
Figure 2.
Demonstration of the methods used for the baseline measurements: (A) weightbearing dorsiflexion ROM, (B) LHA (prone/standing), (C) foot internal rotation angle in plantar flexion, (D) assessment by the mortise test (white arrow, internal rotation stress), and (E) NMM distance (black circle, most prominent points of the navicular tubercle and medial malleolus). LHA, leg-heel angle; NMM distance, navicular–medial malleolus distance; ROM, range of motion.
Measurement of Weightbearing Dorsiflexion ROM
Weightbearing dorsiflexion ROM was measured using a modified method of the technique reported by Bennell et al.3 An athlete was asked to place the foot perpendicular to a wall in a lunge position and bend the forward knee toward the wall, without lifting the heel, until the maximum range of ankle dorsiflexion was reached. During the testing, the athlete was instructed to align and maintain the orientation of the forward knee and toe. The examiner measured ankle dorsiflexion angle using an inclinometer tightly pressed against the anterior aspect of the tibia (Figure 2A). The reliability of this technique (intraclass correlation coefficient [ICC]) was excellent, with an intratester ICC(1, 1) of 0.987 and an intertester ICC(2, 2) of 0.984.
LHA Measurement
LHA was measured to assess rear foot alignment in both the prone and standing positions.18 An athlete was instructed to relax, and an examiner measured the angle formed by the long axis of the lower leg and the straight line bisecting the calcaneus using a goniometer (Figure 2B). The reliability of this measurement in the prone and standing positions was excellent, with an intratester ICC(1, 1) of 0.837 and 0.929 and an intertester ICC(2, 2) of 0.865 and 0.937, respectively.
Measurement of Foot Internal Rotation Angle in Plantar Flexion
Traditionally, LAS has been thought to occur in plantar flexion because the talocrural joint is less stable in plantar flexion, in which greater ankle inversion and internal rotation is thought to occur.35 Therefore, this study measured foot internal rotation angle in ankle plantar flexion. An athlete was instructed to maximally plantar flex in the supine position, while an examiner measured the angle formed between the long axis of the lower leg and the straight line connecting the midpoint of the lateral and medial malleolus to the second metatarsal bone using a goniometer (Figure 2C). The reliability of this measurement was good, with an intratester ICC(1, 1) of 0.774 and an intertester ICC(2, 2) of 0.795.
Mortise Test Assessment and NMM Distance Measurement
Recent case reports using 3-dimensional motion analysis techniques suggested that LAS occurs during ankle internal rotation in dorsiflexion.6,7,26 The data suggest that deficiency of talocrural stability due to bony conformity in dorsiflexion may be present, and the deficiency may be related to the occurrence of LAS. However, there is no standardized examination for the bony stability of the talocrural joint. Therefore, we used 2 novel tests, the mortise test and NMM distance measurement, to assess bony stability at maximum ankle dorsiflexion.
In the mortise test, an athlete was instructed to relax in the prone position and flex the knee at 90°. An examiner held and stabilized the lower leg with 1 hand, using the other hand to apply force at the ball of the foot that maintained maximum dorsiflexion of the ankle and to apply additional internal rotation torque (Figure 2D). The test result is considered “positive” if the ankle inverts and internally rotates without a bony end feel and with a yielding sensation, considered “questionable” if the ankle inverts with a slight bony end feel, and considered “negative” if no inversion occurs. The positive and questionable results were classified as unstable (+), while the negative result was classified as stable (–). The reliability of the mortise test was good, with an intertester reliability (κ) of 0.783.
To measure the NMM distance, an athlete was instructed to relax in the prone position and flex the knee at 90°. An examiner held the lower leg with 1 hand and applied a force on the plantar side of the forefoot until the ankle reached maximal dorsiflexion, without restricting the ankle’s horizontal plane motion. Once the maximal dorsiflexion of the ankle was established, the distance between the most prominent points of the navicular tubercle and the medial malleolus was measured with a digital caliper (Figure 2E). The reliability of this measurement was excellent, with an intratester ICC(1, 1) of 0.857 and an intertester ICC(2, 2) of 0.821.
Statistical Analysis
The measurements from all the athletes who completed this study, including mass, height, weightbearing dorsiflexion ROM, LHA (prone/standing), foot internal rotation angle in plantar flexion, mortise test assessment, and NMM distance, were used to create a predictive model using a forward stepwise Cox regression analysis. Because statistically significant differences were observed between the right and left ankles of the control group (P < .05), measurement data relevant to a sprained ankle in the injury group matched to measurements collected for a random ankle in the control group were used in the final model. The criterion to retain a variable in the model was P < .05, and the criterion for removal was P > .10. The incidence of injury was calculated as injuries per 1000 athlete-exposures. All data were analyzed with SPSS software (PASW Statistics 18; SPSS Inc, Chicago, Illinois, USA).
Results
During the follow-up period, 22 (8 badminton players, 8 soccer players, and 6 baseball players) of the 191 initial participants dropped out of the study, and the remaining 169 athletes (145 males, 24 females) completed the study. Of the athletes who did not complete the study, 21 quit the team because of unrelated reasons and 1 suffered a contact ankle sprain. Of those who completed the study, 125 athletes (74.0%) had a history of ankle sprain prior to participation in this study. During the observational period, 16 athletes (9.47%) suffered noncontact LAS, including 4 initial cases of LAS and 12 recurrences (Figure 1). The injury incidence of noncontact LAS was 0.58 per 1000 athlete-exposures. That amount correlated to: male basketball, 1.04; male badminton, 0.60; female badminton, 0.80; female volleyball, 0.45; male soccer, 0.90; and male baseball, 0.37 per 1000 athlete-exposures.
The measurements gathered from the 44 athletes without previous ankle sprain were used in a Cox regression analysis of the injury and control groups, which demonstrated the NMM distance was predictive of an initial noncontact LAS (Table 1). The hazard ratio estimate indicated that athletes with an NMM distance greater than 4.65 cm were 4.14 times as likely to suffer an initial noncontact LAS as athletes with a shorter NMM distance (95% confidence interval [CI], 1.12-14.30) (Table 2). Figure 3 shows the survival curves based on the NMM distance. Because the cutoff value of NMM distance was 4.65 cm (sensitivity, 0.75; specificity, 0.88) by a receiver operating characteristic curve (Figure 4), the athletes were categorized into 2 groups: (1) NMM <4.65 cm (35 athletes) and (2) NMM ≥4.65 cm (9 athletes). Group 1 exhibited a 97.1% survival rate at the end of the follow-up, while group 2 exhibited a 66.7% survival rate, where “survival” is defined as free from ankle sprain.
TABLE 1.
Intrinsic Factors Analyzed in Athletes Without Previous Ankle Spraina
| Variable | Control Group (n = 40) | Injury Group (n = 4) | P Value |
|---|---|---|---|
| Mass, kg | 68.3 ± 10.0 | 73.2 ± 6.1 | .175 |
| Height, cm | 171.5 ± 7.6 | 175.3 ± 3.4 | .122 |
| Dorsiflexion ROM, deg | 43.7 ± 6.3 | 42.0 ± 8.8 | .961 |
| LHA prone, deg | –5.8 ± 2.6 | –4.3 ± 1.0 | .368 |
| LHA standing, deg | 3.0 ± 1.6 | 2.5 ± 1.7 | .408 |
| Foot internal rotation angle, deg | 8.4 ± 3.4 | 6.0 ± 2.4 | .199 |
| Mortise test, positive % | 86.3 | 75.0 | .611 |
| NMM distance, cm | 3.8 ± 0.7 | 4.7 ± 0.5b | .025 |
aData are presented as mean ± standard deviation. The control group included athletes who suffered no ankle sprain during the study period; the injury group included athletes who suffered lateral ankle sprain. LHA, leg-heel angle; NMM distance, navicular–medial malleolus distance; ROM, range of motion.
bP < .05.
TABLE 2.
Cox Regression Analysis (Forward Stepwise Method) of Athletes Without Previous Ankle Sprain
| Variable | Coefficient | Hazard Ratio (95% Confidence Interval) | P Value |
|---|---|---|---|
| Navicular–medial malleolus distance | 1.419 | 4.14 (1.12-14.30) | .025 |
Figure 3.
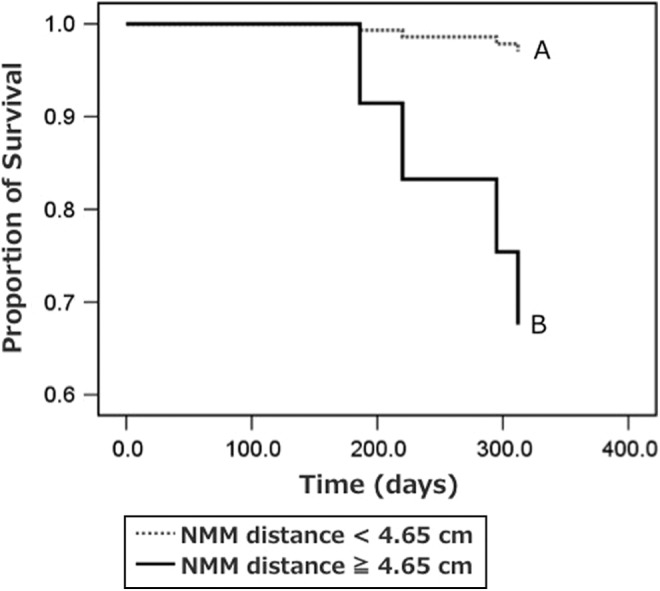
Survival curves for athletes sorted by navicular–medial malleolus (NMM) distance based on the Cox regression model. The gray dotted line represents athletes with NMM distance <4.65 cm (group 1); the black line represents athletes with NMM distance ≥4.65 cm (group 2).
Figure 4.
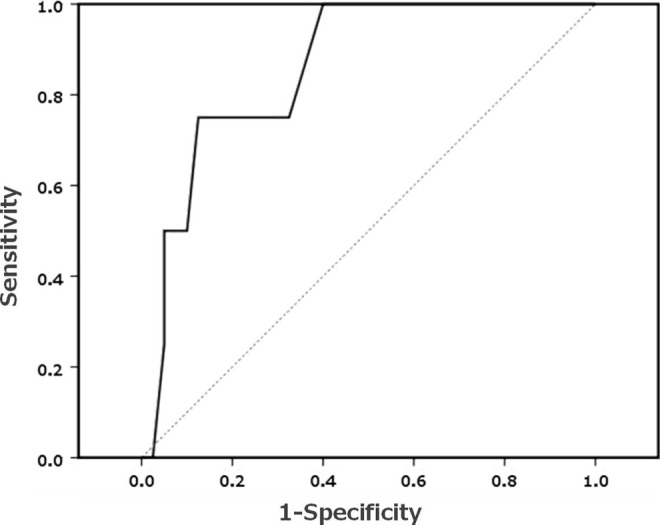
Receiver operating characteristic curves for athletes sorted by navicular–medial malleolus (NMM) distance. The cutoff value was 4.65 cm (sensitivity, 0.75; specificity, 0.88).
The measurements taken from the 125 athletes with a previous ankle sprain were used in a Cox regression analysis of the injury and control groups, which demonstrated that weightbearing dorsiflexion ROM was predictive of a recurrent noncontact LAS (Table 3). The hazard ratio estimate indicated that athletes with a weightbearing dorsiflexion ROM greater than 49.5° were 1.12 times as likely to suffer a recurrent noncontact LAS as athletes with a lower ROM (95% CI, 1.05-1.20) (Table 4). Figure 5 shows the survival curve based on the weightbearing dorsiflexion ROM. Because the cut-off value of weightbearing dorsiflexion ROM was 49.5° (sensitivity, 0.75; specificity, 0.86) by a receiver operating characteristic curve (Figure 6), and the average weightbearing dorsiflexion ROM in this study and the previous large prospective study was 45° ± 4°,27 the athletes’ outcomes were categorized into 3 groups according to their weightbearing dorsiflexion ROM: group 1, <41° (50 athletes); group 2, 41° to 49.5° (50 athletes); and group 3, >49.5° (25 athletes). Group 2 exhibited the highest survival rate (100.0%), followed by group 1 (94.0%) and group 3 (64.0%), where “survival” is defined as free from ankle sprain.
TABLE 3.
Intrinsic Factors Analyzed in Athletes With Previous Ankle Spraina
| Variable | Control Group (n = 113) | Injury Group (n = 12) | P Value |
|---|---|---|---|
| Mass, kg | 68.0 ± 9.2 | 62.8 ± 12.0 | .080 |
| Height, cm | 172.2 ± 7.0 | 169.1 ± 6.1 | .144 |
| Dorsiflexion ROM, deg | 42.3 ± 6.1 | 49.3 ± 9.3b | .000 |
| LHA prone, deg | −6.3 ± 2.7 | –6.8 ± 2.7 | .934 |
| LHA standing, deg | 3.2 ± 1.9 | 4.5 ± 1.9 | .207 |
| Foot internal rotation angle, deg | 9.3 ± 4.0 | 9.4 ± 5.3 | .640 |
| Mortise test, positive % | 72.3 | 58.3 | .547 |
| NMM distance, cm | 3.9 ± 0.7 | 3.5 ± 0.7 | .324 |
aData are presented as mean ± standard deviation. The control group included athletes who suffered no ankle sprain during the study period; the injury group included athletes who suffered lateral ankle sprain. LHA, leg-heel angle; NMM distance, navicular–medial malleolus distance; ROM, range of motion.
bP < .05.
TABLE 4.
Cox Regression Analysis (Forward Stepwise Method) of Athletes With Previous Ankle Sprain
| Variable | Coefficient | Hazard Ratio (95% Confidence Interval) | P Value |
|---|---|---|---|
| Dorsiflexion range of motion | 0.115 | 1.12 (1.05-1.20) | .000 |
Figure 5.
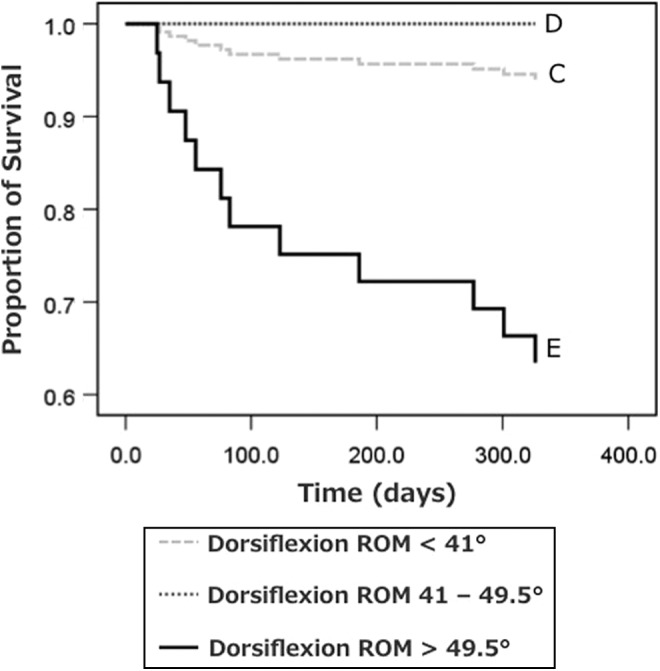
Survival curves for athletes sorted by weightbearing dorsiflexion range of motion (ROM) based on the Cox regression model. The light gray dotted line represents athletes with dorsiflexion ROM <41° (group 1), the dark gray dotted line represents athletes with dorsiflexion ROM 41° to 49.5° (group 1), and the black line represents athletes with dorsiflexion ROM >49.5° (group 3).
Figure 6.
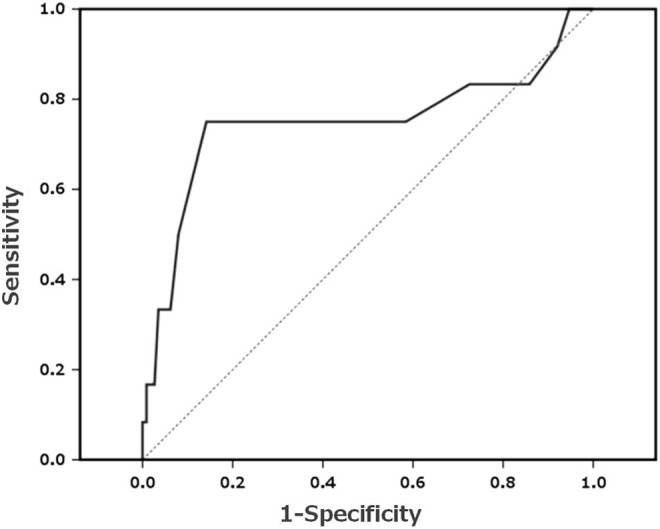
Receiver operating characteristic curves for athletes sorted by weightbearing dorsiflexion range of motion. The cutoff value is 49.5° (sensitivity, 0.75; specificity, 0.86).
Discussion
The purpose of this study was to identify predictive factors of initial and recurrent noncontact LAS in collegiate athletes. The incidence of noncontact LAS during the 48-week monitoring period of 169 collegiate athletes in this study was 0.58 per 1000 athlete-exposures. An NMM distance greater than 4.65 cm predicted initial noncontact LAS, and a greater weightbearing dorsiflexion ROM (>49.5°) predicted recurrent noncontact LAS.
We observed an incidence of noncontact LAS of 0.58 per 1000 athlete-exposures. This incidence was much lower than the incidences of 1.13 and 1.08 per 1000 athlete-exposures reported by McHugh et al21 and Tyler et al,31 respectively. A reason for this discrepancy may include the differences in sports played by the athletes in each study. According to a large epidemiological study, the incidence of ankle sprain is high in soccer and basketball and low in baseball.16 Previous studies have focused on high-risk sports, including high school soccer31 and high school soccer and basketball.21 In contrast, nearly half of athletes in this study participated in low-risk sports such as baseball (0.37 per 1000 athlete-exposures). Similarly, a study of adolescent ballet dancers has shown that the incidence of noncontact LAS was 0.21 per 1000 athlete-exposures.12 Therefore, the type of sport may affect the incidence of noncontact LAS.
Athletes with an NMM distance >4.65 cm at maximum ankle dorsiflexion were at higher risk of an initial noncontact LAS. The location of the navicular tubercle was used as a substitute landmark to assess the location of the head of the talus in the sagittal plane. Greater NMM distance indicates that the medial aspect of the talus shifts anteriorly during dorsiflexion compared with an ankle with a smaller NMM distance. An ankle with greater NMM distance typically demonstrates external rotation of the talus near the maximal dorsiflexion, suggesting the gliding motion of the talocrural joint is limited medially, but not laterally, near the maximal dorsiflexion. This limit in motion may reduce bony conformity at maximal talocrural dorsiflexion, resulting in the higher incidence of initial LAS. Because manual posterior gliding is reportedly effective for functional recovery of joints involving CAI,13–15,34 normalizing talar posterior glide during ankle dorsiflexion may decrease the incidence of noncontact LAS. An association between the NMM distance and talar posterior glide should be investigated in the future. Although a standardized method of assessing the bony conformity of the talocrural joint at maximal dorsiflexion has not been established, the NMM distance may provide information on talocrural abnormal kinematics predicting initial LAS. All subjects in this study were Japanese, and the average height was 171.9 ± 7.1 cm. Therefore, the cutoff value used in this study needs to be adjusted for taller or shorter populations.
Several studies have reported that a deficit in ankle dorsiflexion ROM is a significant predictor of LAS.27,40 In a study of army recruits, Pope et al27 showed that the least flexible ankle (34° of dorsiflexion ROM) has 5 times the risk of LAS compared with ankles of average flexibility (45° ± 4° of dorsiflexion ROM). Willems et al41 showed that decreased ankle dorsiflexion ROM during knee extension increases the risk of LAS in male collegiate students. However, many studies have failed to demonstrate an association between a deficit in ankle dorsiflexion ROM and the occurrence of LAS.2,4,5,41 Also, a few studies have failed to show that a deficit in ankle dorsiflexion ROM or a difference in the right and left ankle dorsiflexion ROM are predicting factors for noncontact LAS.8,12 Interestingly, we observed that ankles with mediocre weightbearing dorsiflexion ROM (41°-49.5°) are at low risk of recurrent LAS. Recent kinematic studies have suggested that LAS occurs during slight plantar flexion to slight dorsiflexion,6,26 indicating that LAS can occur during dorsiflexion. No explanation for this result exists in the literature, and greater attention should be directed to the injury mechanism of LAS occurring during dorsiflexion.
This study is a case-control study utilizing highly reliable measurement techniques. Athlete-exposures and injury data were collected on campus by a physical therapist, which further improves data reliability. However, this study involved only collegiate athletes in a limited number of sports; thus, these results may neither be applicable to adolescent or older athletes nor to athletes participating in other sports. This study was also methodologically limited by an insufficient number of subjects, especially athletes without previous ankle sprain. Accordingly, we adopted the forward stepwise analysis to prevent a reduced goodness of fit of the predictive model; the final events-to-predictors ratio was 4.0 (initial LAS) and 12.0 (recurrent LAS). These ratios are not low compared with the ratios of previous noncontact LAS studies, 4.8 and 3 in the study by Tyler et al,31 2.2 in the study by McHugh et al,21 and 3.4 in the study by Fousekis et al.8 Therefore, our study was methodologically comparable to previous relevant studies.
During the 48-week follow-up of 169 collegiate athletes, the incidence of noncontact LAS was 0.58 per 1000 athlete-exposures. The NMM distance predicted the occurrence of initial noncontact LAS, and a mediocre weightbearing dorsiflexion ROM lowered the risk of recurrent noncontact LAS. This study, to our knowledge, is the first to distinguish predictive factors for initial LAS from those for recurrent noncontact LAS. We feel that the NMM distance can be reduced by improving the flexibility of surrounding tissues such as the skin, Achilles tendon, and/or the flexor retinaculum. A future randomized control study may focus on the effects of an intervention to improve bony conformity at maximal dorsiflexion on preventing LAS.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bahr R, Lian O, Bahr IA. A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study. Scand J Med Sci Sports. 1997;7:172–177. [DOI] [PubMed] [Google Scholar]
- 2. Baumhauer JF, Alosa DM, Renstrom AF, Trevino S, Beynnon B. A prospective study of ankle injury risk factors. Am J Sports Med. 1995;23:564–570. [DOI] [PubMed] [Google Scholar]
- 3. Bennell KL, Talbot RC, Wajswelner H, Techovanich W, Kelly DH, Hall AJ. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44:175–180. [DOI] [PubMed] [Google Scholar]
- 4. Beynnon BD, Renström PA, Alosa DM, Baumhauer JF, Vacek PM. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19:213–220. [DOI] [PubMed] [Google Scholar]
- 5. de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: a prospective study. Scand J Med Sci Sports. 2013;23:541–547. [DOI] [PubMed] [Google Scholar]
- 6. Fong DT, Ha SC, Mok KM, Chan CW, Chan KM. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: five cases from televised tennis competitions. Am J Sports Med. 2012;40:2627–2632. [DOI] [PubMed] [Google Scholar]
- 7. Fong DT, Hong Y, Shima Y, Krosshaug T, Yung PS, Chan KM. Biomechanics of supination ankle sprain: a case report of an accidental injury event in the laboratory. Am J Sports Med. 2009;37:822–827. [DOI] [PubMed] [Google Scholar]
- 8. Fousekis K, Tsepis E, Vagenas G. Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players. Am J Sports Med. 2012;40:1842–1850. [DOI] [PubMed] [Google Scholar]
- 9. Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61:354–361. [PubMed] [Google Scholar]
- 10. Hayes A, Tochigi Y, Saltzman CL. Ankle morphometry on 3D-CT images. Iowa Orthop J. 2006;26:1–4. [PMC free article] [PubMed] [Google Scholar]
- 11. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37:364–375. [PMC free article] [PubMed] [Google Scholar]
- 12. Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Intrinsic predictors of lateral ankle sprain in adolescent dancers: a prospective cohort study. Clin J Sport Med. 2008;18:44–48. [DOI] [PubMed] [Google Scholar]
- 13. Hoch MC, Andreatta RD, Mullineaux DR, et al. Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability. J Orthop Res. 2012;30:1798–1804. [DOI] [PubMed] [Google Scholar]
- 14. Hoch MC, McKeon PO. The effectiveness of mobilization with movement at improving dorsiflexion after ankle sprain. J Sport Rehabil. 2010;19:226–232. [DOI] [PubMed] [Google Scholar]
- 15. Hoch MC, McKeon PO. Joint mobilization improves spatiotemporal postural control and range of motion in those with chronic ankle instability. J Orthop Res. 2011;29:326–332. [DOI] [PubMed] [Google Scholar]
- 16. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 17. Kannus P, Renstrom P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305–312. [PubMed] [Google Scholar]
- 18. Lang LM, Volpe RG, Wernick J. Static biomechanical evaluation of the foot and lower limb: the podiatrist’s perspective. Man Ther. 1997;2:58–66. [DOI] [PubMed] [Google Scholar]
- 19. Lofvenberg R, Karrholm J, Lund B. The outcome of nonoperated patients with chronic lateral instability of the ankle: a 20-year follow-up study. Foot Ankle Int. 1994;15:165–169. [DOI] [PubMed] [Google Scholar]
- 20. McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34:1103–1111. [DOI] [PubMed] [Google Scholar]
- 21. McHugh MP, Tyler TF, Tetro DT, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school athletes: the role of hip strength and balance ability. Am J Sports Med. 2006;34:464–470. [DOI] [PubMed] [Google Scholar]
- 22. McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McKeon PO, Mattacola CG. Interventions for the prevention of first time and recurrent ankle sprains. Clin Sports Med. 2008;27:371–382. [DOI] [PubMed] [Google Scholar]
- 24. Milgrom C, Shlamkovitch N, Finestone A, et al. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991;12:26–30. [DOI] [PubMed] [Google Scholar]
- 25. Mitchell A, Dyson R, Hale T, Abraham C. Biomechanics of ankle instability. Part 2: postural sway-reaction time relationship. Med Sci Sports Exerc. 2008;40:1522–1528. [DOI] [PubMed] [Google Scholar]
- 26. Mok KM, Fong DT, Krosshaug T, et al. Kinematics analysis of ankle inversion ligamentous sprain injuries in sports: 2 cases during the 2008 Beijing Olympics. Am J Sports Med. 2011;39:1548–1552. [DOI] [PubMed] [Google Scholar]
- 27. Pope R, Herbert R, Kirwan J. Effects of ankle dorsiflexion range and pre-exercise calf muscle stretching on injury risk in army recruits. Aust J Physiother. 1998;44:165–172. [DOI] [PubMed] [Google Scholar]
- 28. Povacz P, Unger SF, Miller WK, Tockner R, Resch H. A randomized, prospective study of operative and non-operative treatment of injuries of the fibular collateral ligaments of the ankle. J Bone Joint Surg Am. 1998;80:345–351. [DOI] [PubMed] [Google Scholar]
- 29. Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94:769–776. [DOI] [PubMed] [Google Scholar]
- 30. Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–262. [DOI] [PubMed] [Google Scholar]
- 31. Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34:471–475. [DOI] [PubMed] [Google Scholar]
- 32. Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385–1393. [DOI] [PubMed] [Google Scholar]
- 33. Verhagen RA, de Keizer G, van Dijk CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114:92–96. [DOI] [PubMed] [Google Scholar]
- 34. Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36:464–471. [DOI] [PubMed] [Google Scholar]
- 35. Vitale TD, Fallat LM. Lateral ankle sprains: evaluation and treatment. J Foot Surg. 1988;27:248–258. [PubMed] [Google Scholar]
- 36. Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Watson AW. Ankle sprains in players of the field-games Gaelic football and hurling. J Sports Med Phys Fitness. 1999;39:66–70. [PubMed] [Google Scholar]
- 38. Wikstrom EA, Tillman MD, Chmielewski TL, Cauraugh JH, Borsa PA. Dynamic postural stability deficits in subjects with self-reported ankle instability. Med Sci Sports Exerc. 2007;39:397–402. [DOI] [PubMed] [Google Scholar]
- 39. Willems T, Witvrouw E, Delbaere K, De Cock A, De Clercq D. Relationship between gait biomechanics and inversion sprains: a prospective study of risk factors. Gait Posture. 2005;21:379–387. [DOI] [PubMed] [Google Scholar]
- 40. Willems TM, Witvrouw E, Delbaere K, Mahieu N, De Bourdeaudhuij I, De Clercq D. Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study. Am J Sports Med. 2005;33:415–423. [DOI] [PubMed] [Google Scholar]
- 41. Willems TM, Witvrouw E, Delbaere K, Philippaerts R, De Bourdeaudhuij I, De Clercq D. Intrinsic risk factors for inversion ankle sprains in females—a prospective study. Scand J Med Sci Sports. 2005;15:336–345. [DOI] [PubMed] [Google Scholar]
- 42. Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]