Abstract
Background:
When to allow an athlete to return to unrestricted sporting activity after anterior cruciate ligament (ACL) reconstruction remains controversial.
Purpose:
To report the results of functional performance testing reported in the literature for individuals at differing time points following ACL reconstruction and to examine differences between graft types.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review of Medline, Scopus, and Cochrane Central Register of Controlled Trials was performed using PRISMA guidelines. Inclusion criteria were English-language studies that examined any functional rehabilitation test from 6 months to 2 years following ACL reconstruction. All patient-, limb-, and knee-specific demographics were extracted from included investigations. All functional rehabilitation tests were analyzed and compared when applicable.
Results:
The search term returned a total of 890 potential studies, with 88 meeting inclusion and exclusion criteria. A total of 4927 patients were included, of which 66% were male. The mean patient age was 26.5 ± 3.4 years. The predominant graft choices for reconstruction were bone–patellar tendon–bone (BPTB) autograft (59.8%) and hamstring autograft (37.9%). The most commonly reported functional tests were the hop tests. The results of these functional tests, as reported in the Limb Symmetry Index (LSI), improved with increasing time, with nearly all results greater than 90% at 1 year following primary ACL reconstruction. At 6 months postoperatively, a number of isokinetic strength measurements failed to reach 80% LSI, most commonly isokinetic knee extension testing in both BPTB and hamstring autograft groups. The knee flexion strength deficit was significantly less in the BPTB autograft group as compared with those having hamstring autograft at 1 year postoperatively, while no significant differences were found in isokinetic extension strength between the 2 groups.
Conclusion:
Hop testing was the most commonly reported functional test following ACL reconstruction. Increases in performance on functional tests were predictably seen as time increased following surgery. Those with hamstring autografts may experience increased strength deficits with knee flexion versus those having BPTB autograft. These data provide information that may assist providers in determining timing of return to unrestricted sporting activity.
Keywords: ACL, anterior, cruciate, ligament, functional test, hop, isokinetic
Anterior cruciate ligament (ACL) injuries are common in the young and athletically active population, with a reported incidence of 0.7 to 2.5 ACL tears per 1000 athletic-exposures.78 It has been estimated that between 100,000 and 200,000 reconstructions are performed in the United States each year.13,22 Reconstruction of the ACL using either bone–patellar tendon–bone (BPTB) autograft,69 hamstring autograft,97 or allograft tissue25 has become standard for treatment in patients who have functional knee instability and a desire to return to cutting and pivoting sports. Clinical follow-up has shown a high rate of return to previous level of activity using modern arthroscopically assisted reconstruction techniques.24,58,64,96
While the need for ACL reconstruction in athletically active individuals who desire a return to cutting and pivoting sports is generally accepted, there is a lack of consensus as to when an athlete may return to sport. In their review of 264 investigations, Barber-Westin and Noyes9 reported that criterion for return to play was not reported in 40% of studies, with an additional 32% of investigations using only postoperative time. Only 13% of the studies utilized objective criteria for determining when an athlete may return to sport.
Deficits in neuromuscular control of the lower extremity are known to be a risk factor for secondary (retear) ACL injury and are therefore often used in assessing return-to-play readiness.75,100 Quadriceps strength, in particular, has been associated with physical functioning of the leg following ACL reconstruction.16,57 Additionally, some authors have evaluated the presence of neuromuscular impairment following ACL reconstruction and its association with secondary reinjury.75 Hip and knee positions predicted a second injury,75 emphasizing the importance of addressing these parameters during rehabilitation.
To assist with returning a patient to sports, many groups have developed rehabilitation protocols, each with their own methods and return-to-play criteria.23,31,104 Areas of particular interest in determining return to play are functional tests (ie, hop testing), lower extremity isokinetic strength measurements, and movement and/or landing mechanics. Yabroudi and Irrgang104 recently outlined a detailed rehabilitation protocol and allowed full-effort sprinting, cutting, and plyometric activities once the patient reached a quadriceps index of 85% and has successfully completed the early postoperative, strengthening, and neuromuscular control phases. Heckmann et al31 defined return-to-play criteria through the use of a subjective evaluation, knee examination, and functional testing.
The goal of these rehabilitation programs is ultimately to allow return to play without additional injury to the knee. There has been no consensus as to which functional tests should be utilized to make this determination or what values should be achieved at different time points postoperatively. The goal of this investigation was to perform a systematic review of all available studies to provide normative data for functional tests utilized following primary ACL reconstruction to determine return to play. We also sought to detect any difference in the outcomes of functional testing between different graft types.
Methods
The first author performed a systematic review of multiple medical databases, including Medline and Scopus, using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.68 PRISMA guides authors in the appropriate design, conduct, and reporting of a systematic review and/or meta-analysis via appropriate identification, screening, and inclusion of relevant studies for review. The search term we usedi sought to find original research publications that investigated the results of functional testing following primary ACL reconstruction. Level 1, 2, 3, and 4 evidence clinical outcome studies were inclusive. Inclusion criteria were English-language studies that examined any lower extremity functional rehabilitation test from 6 months to 2 years following ACL reconstruction. This timeframe was chosen as the purpose of this investigation was to provide normative data for functional tests to help clinicians determine return to play criteria. This time frame captured data for patients who had undergone rehabilitation before returning to play at 6 months as well as those who had already returned to play and would presumably be maximally rehabilitated (2 years). Even if some patients had returned to play prior to the 6-month time point, their functional testing results would still provide adequate data from which to create normative data.
Exclusion criteria included studies reporting outcomes outside of the 6-month to 2-year postoperative timeframe, revision ACL reconstruction, non–English language, surgical technique, letters to the editor, systematic reviews, meta-analyses, duplicate subject populations, and multiligament knee injuries. Patients with concomitant ACL reconstruction with nonoperative treatment of a medial collateral ligament (MCL) injury were included, however. Studies that reported raw data or did not report results for single-leg testing as normalized data, such as through the use of the Limb Symmetry Index (LSI), were excluded even if results were compared with a healthy control subject. Exceptions to this included testing that required both legs, such as the shuttle run, in which case results were separately reported for males and females. When results were separately reported for 2 different cohorts within the same study, most commonly through the use of separate rehabilitation protocols, the results between groups for each time point were averaged.
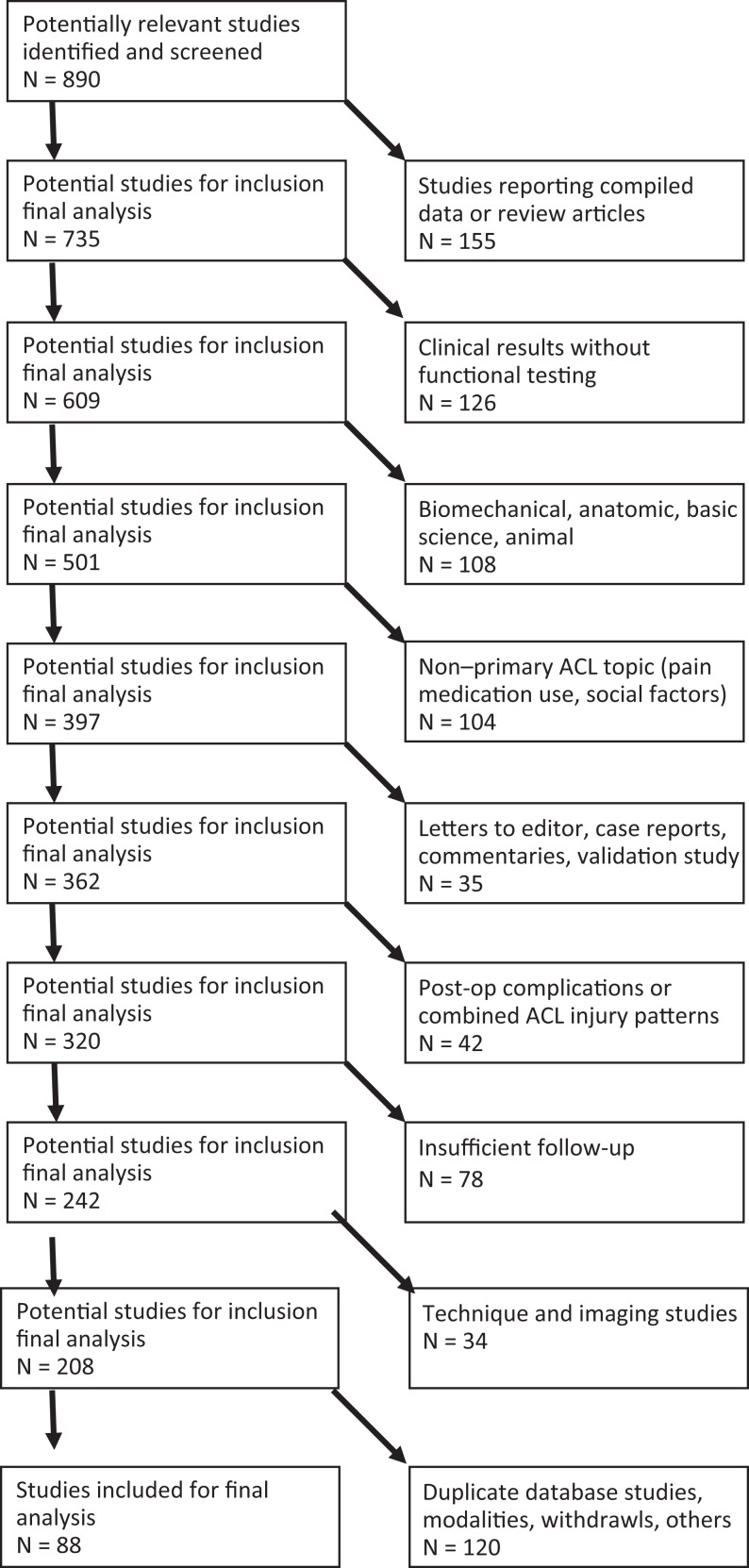
Both electronically and print published articles were accepted for inclusion, while meeting abstracts and proceedings were excluded. All references from the studies returned using the search term were cross-referenced for potential inclusion if initially omitted from the search results. If 2 or more separate studies existed that reported on identical patient populations, they were both included as long as they reported functional testing results for different time points between 6 months and 2 years. Figure 1 shows the search algorithm used to generate the final cohort of included investigations.
Figure 1.
Systematic review search algorithm within Medline database according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Descriptive statistics were used, with results reported as means ± standard deviations. Categorical data were reported as frequencies with percentages. Where applicable, results were compared using the Student t test and linear regression with an alpha value of .05 set as significant.
Results
The search term returned a total of 890 potential studies, with 88 meeting inclusion and exclusion criteria (Figure 1). A total of 4927 patients were included, of which 66% were male. The mean patient age was 26.5 ± 3.4 years. The predominant graft choices for reconstruction were BPTB autograft (59.8%) and hamstring autograft (37.9%). BPTB allograft was used in 1.6% of patients, hamstring allograft in 0.1%, and quadriceps autograft in 0.4%.
The most commonly reported functional tests were the hop tests. These included the single-leg, cross-over, triple, 6-m timed, and single-leg hop height tests (Table 1). In general, the results of these functional tests, as reported in LSI, improved with increasing time, with nearly all results greater than 90% at 1 year after primary ACL reconstruction. For example, single-leg hop LSI averaged 87%, 92%, and 94% at 6 months, 1 year, and 2 years, respectively. When examining the results of the 5 most common hop tests (single-leg hop, cross-over hop, triple hop, 6-m timed hop, and single-leg hop height), there were no significant differences at any time points in the results between those receiving BPTB and hamstring autograft (P > .265).
TABLE 1.
Studies Reporting the Results of Functional Performance Tests Involving Hopping, Jumping, or Squatting at Varying Time Points After ACLRa
| Functional Test | Follow-up, mo | ||||
|---|---|---|---|---|---|
| 6 | 9 | 12 | 18 | 24 | |
| Single-leg hopb | 87 ± 6 | 90 ± 2 | 92 ± 3 | 92 | 94 ± 4 |
| Cross-over hopc | 90 ± 4 | 91 ± 3 | 92 ± 3 | 96 | 93 |
| Triple hopd | 90 ± 4 | 92 | 95 ± 3 | 94 | 96 ± 2 |
| 6-meter timed hope | 90 ± 7 | 96 | 94 ± 5 | — | 99 ± 1 |
| Single-leg hop height1,8,11,36,39,47,70,76,99 | 80 ± 5 | 89 | 91 ± 2 | — | 95 ± 3 |
| Fatigue single-leg hop6 | — | — | 89 | — | — |
| Side hops in 30 seconds1,99 | 76 | — | 86 | — | 95 ± 4 |
| Stair hop1,39,84–86,99 | 84 ± 6 | — | 91 ± 5 | — | 92 ± 0 |
| Stair hopple7,83 | 87 | — | 88 | 90 | 95 |
| Vertical jump,72 cm | — | 50/36 f | — | — | — |
| Broad jump,72 cm | — | 213/160 f | — | — | — |
| 10-step stair climb,8 s | — | — | — | — | 5 g |
| Step-hop,8 s | — | — | — | — | 11.9 g |
| Step up and over62 | — | — | 85 | — | — |
aValues are expressed as Limb Symmetry Index values (in percentages; mean ± standard deviation) unless otherwise indicated. Where no error measurement is presented, not enough data were present to calculate a standard deviation. A dash indicates no data were available. ACLR, anterior cruciate ligament reconstruction.
bReferences 1, 4, 7, 8, 10, 11, 16, 19, 27, 30, 33, 36, 43–46, 52–56, 59, 60, 63, 72, 76, 79, 80, 84, 85, 89, 95, 98, 99, 107.
fValues reported as No. of males/No. of females (both legs).
gValues reported as No. of males.
Table 2 reports the results of agility testing at varying time points following primary ACL reconstruction. There was no significant difference between times in the co-contraction, shuttle run, or carioca tests over the 6-month to 2-year time period (P > .240). The times for long shuttle, modified agility, and pro shuttle tests were lower for men than women (Table 2).
TABLE 2.
Studies Reporting the Results of Agility Testing at Varying Time Points After ACLRa
| Functional Test | Follow-up, mo | ||||
|---|---|---|---|---|---|
| 6 | 9 | 12 | 18 | 24 | |
| Co-contraction,47,48,56 s | 14.9 | — | 15.8 | 16.0 | 15.8 |
| Shuttle run,46–48,56 s | 8.9 | — | 8.0 | 8.5 | 8.1 |
| Carioca test,8,46–48,56 s | 11.4 ± 2.9 | — | 9.5 | 11.0 | 9.4 ± 0.1 |
| Long shuttle—male/female,72 s | — | 8.7/9.3 | — | — | — |
| Modified agility test—male/female,72 s | — | 10.4/10.8 | — | — | — |
| Pro shuttle—male/female,72 s | — | 5.2/5.7 | — | — | — |
aAbsolute values are reported for males unless otherwise indicated. Where no error measurement is presented, not enough data were present to calculate a standard deviation. A dash indicates no data were available. ACLR, anterior cruciate ligament reconstruction.
Results of functional performance tests utilizing a motion analysis with or without a force plate are presented in Table 3. One-leg hop contact time and jump time returned to an average of 98% and 84% LSI, respectively, at 1 year postoperatively. Ground reaction force (GRF) during landing and takeoff were 89% and 73%, respectively, at 8 months. Proprioception was also assessed in a number of investigations (Table 3). In general, postural motion control, reproduction of passive motion of the knee, and overall joint position sense returned to values similar to the contralateral limb from 8 to 12 months following ACL reconstruction.
TABLE 3.
Results of Functional Performance Tests Utilizing a Force Plate and/or Motion Analysisa
| Functional Test | Follow-up, mo | ||||
|---|---|---|---|---|---|
| 6 | 8 | 9 | 12 | 24 | |
| One-leg hop contact time77 | — | — | — | 98 | — |
| One-leg hop jump time77 | — | — | — | 84 | — |
| One-leg hop eccentric knee angular velocity77 | — | — | — | 76 | — |
| One-leg hop concentric knee angular velocity77 | — | — | — | 81 | — |
| One-leg hop vertical jump off force (% body weight)88 | — | — | — | — | 190 |
| Lift off index62 | — | — | — | 85 | — |
| Lunge impact index62 | — | — | — | 81 | — |
| Jump GRF70,74 | 82 | — | 95 | — | — |
| Center of pressure motion with single-leg stance—AP/ML directions67 | — | 86/89 | — | — | — |
| Center of pressure velocity with single-leg stance—AP/ML directions67 | — | 94/95 | — | — | — |
| Center of pressure mean velocity with single-leg stance67 | — | 93 | — | — | — |
| Landing/take off peak vertical GRF67 | — | 89/73 | — | — | — |
| Take off vertical GRF loading rate67 | — | 90 | — | — | — |
| Reproduction of passive motion at 15°/30°/45° of flexion,54,81 deg | 5.7 (full extension) | — | — | 5.4/7.0/7.0 | — |
| Threshold to detection of passive motion at 15°/30°/45° of flexion,54,81,85 deg | 1.4 ± 0.3 | — | — | 1.7/2.0/1.8 | — |
| Squat jump GRF54 | — | — | — | — | 98 |
| Countermovement jump GRF54 | — | — | — | — | 98 |
| Drop jump GRF54 | — | — | — | — | 99 |
| Drop jump contact time,77 ms | — | — | — | 90 | — |
| Drop jump jumping time,77 ms | — | — | — | 86 | — |
| Drop jump eccentric/concentric knee angle speed,77 deg/s | — | — | — | 90/79 | — |
| Rebound jump GRF54 | — | — | — | 98 | — |
| Balance index85 | 96 | — | — | — | — |
| Stabilization angle when GRF equals body weight,88 deg | — | — | — | — | 21 |
| Angle of knee joint at landing,88 deg | — | — | — | — | 26 |
| Stance phase duration (% longer in operative leg)88 | — | — | — | — | 20 |
| Joint position sense difference in operative and nonoperative leg—flexion/extension weightbearing,38 deg | — | — | — | 1.2/0.8 | — |
| Joint position sense difference in operative and nonoperative leg—flexion/extension nonweightbearing,20,21,41 deg | 0.4 ± 0.2/0.8 ± 0.7 | — | — | —/1.2 | — |
| Postural sway dispersion index—eyes open/eyes closed29 | — | — | — | 100/92 | — |
| Coordination deficit—concentric/eccentric105 | 79/64 | — | 81/76 | — | — |
aData are expressed as Limb Symmetry Index values (in percentages) unless otherwise indicated. Where no error measurement is presented, not enough data were present to calculate a standard deviation. A dash indicates no data were available. GRF, ground reaction force; AP, anterior-posterior; ML, medial-lateral.
Functional testing involving strength assessment following ACL reconstruction was also extensively reported in the literature and is summarized in Table 4. At 6 months postoperatively, a number of strength measures had failed to reach 80% LSI as compared with the uninvolved contralateral leg (Table 4). This was most common for isokinetic knee extension testing in both BPTB and hamstring autograft groups. In comparing all patients, there were significantly greater deficits in isokinetic knee extension values at various angular velocities and multiple time points postoperatively (Table 5). Significant differences were seen for isokinetic knee flexion showing less deficit (versus extension) as compared with the contralateral limb. When comparing the results of the groups by graft type, knee flexor strength deficit at 60 and 180 deg/s was significantly less in the BPTB autograft group (97% and 99%) as compared with those having hamstring autograft (87% and 91%) at 1 year postoperatively (P = .002 and .015). No significant differences were found in isokinetic extension strength between the 2 groups at any time point or at any angular velocity.
TABLE 4.
Studies Reporting the Results of Functional Performance Tests Involving Strength Testing at Varying Time Points After ACLRa
| Follow-up, mo | |||||
|---|---|---|---|---|---|
| 6 | 9 | 12 | 18 | 24 | |
| Single-leg press1,99 | 85 | — | 95 | — | 97 ± 1 |
| Single-leg press MVIC5,30,89 | 93 ± 6 | — | 98 ± 0 | — | — |
| Leg press rate of force development at 30%/50%/90% MVIC5 | 80/79/72 | — | 97/92/90 | — | — |
| Open chain knee flexion | 93 ± 1 | — | 98 ± 2 | — | 95 ± 5 |
| Hamstring autograft29 | — | — | 99 | — | — |
| Mixed graft1,50,99 | 93 ± 1 | — | 96 | — | 98 ± 0 |
| Isokinetic knee flexion peak torque at 60/120/180/240 deg/s | 89 ± 8/97 ± 14/92 ± 7/92 ± 1 | 95 ± 4/—/95/— | 92 ± 6/90 ± 14/96 ± 4/94 ± 3 | 95 ± 6/—/100/95 | 98 ± 3/100/96 ± 7/94 ± 5 |
| BPTB autograftb | 91 ± 6/87 ± 14/95 ± 7/92 ± 1 | — | 97 ± 2/80/99 ± 2/96 ± 0 | 95 ± 6/—/100/95 | 97 ± 3/—/100/98 |
| Hamstring autograftc | 84 ± 11/—/89 ± 8/— | 90/—/—/— | 87 ± 4/—/91 ± 1/— | — | 100/—/88/— |
| Allograft12 | 98/—/—/93 | — | — | — | — |
| Mixed graft2,7,8,11,16,26,32,33 | 91 ± 5/96/95/92 | 96/—/95/— | 97 ± 4/100/99 ± 1/91 | — | 98 ± 3/100/100/91 |
| Isokinetic knee extension peak torque at 60/120/180/240 deg/s | 75 ± 9/74 ± 4/84 ± 6/79 ± 3 | 73 ± 3/—/79/— | 86 ± 6/87 ± 8/88 ± 5/89 ± 2 | 89 ± 6/—/84/89 | 93 ± 5/100/96 ± 4/91 ± 2 |
| BPTB autograftd | 73 ± 6/74 ± 4/84 ± 6/79 ± 0 | —/—/79/— | 84 ± 3/81/86 ± 2/89 ± 3 | 86 ± 6/—/—/89 | 91 ± 3/—/93/89 |
| Hamstring autografte | 77 ± 14/—/86 ± 4/— | — | 87 ± 6/—/89 ± 4/— | — | —/—/96/— |
| Allograft12 | 65/—/—/73 | — | — | — | — |
| Mixed graftf | 78 ± 13/—/75/84 | 73 ± 3/—/—/— | 88 ± 7/93/91 ± 8/90 | 94/—/84/— | 95 ± 6/100/100/92 |
| Isokinetic knee internal rotation at 30/60/90/120 deg/s2,90 | — | — | 90 ± 1/95/95/90 | — | 97/97/96 |
| Isokinetic knee external rotation at 30/60/90/120 deg/s2,90 | — | — | 98 ± 0/97/98/99 | — | 98/98/97 |
| Time to peak torque flexion at 60/240 deg/s (BPTB autograft)103 | 100/100 | — | 95/94 | 95/100 | — |
| Time to peak torque extension at 60/240 deg/s (BPTB autograft)103 | 91/90 | — | 98/100 | 100/100 | — |
aAll data are expressed as Limb Symmetry Index values (in percentages; mean ± standard deviation). Where no error measurement is presented, not enough data were present to calculate a standard deviation. A dash indicates no data were available. ACLR, anterior cruciate ligament reconstruction. MVIC, maximal voluntary isometric contraction; BPTB, bone–patellar tendon–bone.
TABLE 5.
P Values Comparing Isokinetic Peak Knee Flexion and Extension Forces at Varying Time Points and Angular Velocitiesa
| Angular Velocity, deg/s | Follow-up, mo | ||||
|---|---|---|---|---|---|
| 6 | 9 | 12 | 18 | 24 | |
| 60 | <.001 | .008 | .008 | .372 | .021 |
| 120 | .211 | — | .841 | — | — |
| 180 | .018 | — | .002 | — | .944 |
| 240 | <.001 | — | .072 | — | .404 |
aAll significant values (P < .05, Student t test) represent increased strength in knee extension versus knee flexion. A dash indicates no data were available.
Discussion
The goal of this investigation was to provide normative data to assist both patients and physicians in determining return to play following ACL reconstruction. A secondary goal was to assess any subtle differences in the performance results of patients with differing graft types. Even with the large amount of published investigations regarding all aspects of ACL reconstruction, as well as functional testing following ACL reconstruction, few clinicians utilize objective data in determining return to play, and there is no evidence-based consensus on when it is appropriate for patients to return to unrestricted sports participation. A recent systematic review by Barber-Westin and Noyes9 examined 264 studies within the past 10 years describing return to play following primary ACL reconstruction. Of these included investigations, only 13% described objective criteria for return to play. Forty percent gave no criteria, 32% used only time from surgery, and 15% utilized time from surgery along with subjective functional assessment scores.
In this review, the most common functional tests reported in the literature following ACL reconstruction were the hop tests. The 4 standard hop tests (single-leg, cross-over, triple, and 6-m timed hop tests) all averaged greater than 90% LSI at 6 to 9 months postoperatively. Interestingly, when more demanding testing was carried out that required increased stamina in the operative leg, results declined. Although the number of studies reporting results of endurance hop tests is limited, the findings presented in this investigation demonstrated that the results of the fatigue single-leg hop and side hop in 30 seconds showed lower LSI values as compared with the standard hop testing regimen. This may indicate increased fatigability in the operative extremity that is still present at the 6- to 12-month time period. These deficiencies, however, appeared to normalize by the 24-month mark, with LSI values in the mid-90% range, comparable to the other hop testing results.
While an important objective measure, the results of hop testing have not been correlated with return to play. They have, however, been correlated with knee function as measured with self-reported questionnaires. Logerstedt et al60 examined the correlation between hop testing and the International Knee Documentation Committee 2000 subjective knee form (IKDC 2000) at 6 and 12 months after primary ACL reconstruction. To define “normal” knee function, they utilized published normative data for the top 85th percentile of age- and sex-matched control knees. While preoperative hop testing was not predictive of knee function at any time following ACL reconstruction, postoperative testing was predictive of self-reported knee function. Of the 4 common hop tests examined, the 6-m timed and cross-over hop tests were the best predictors of normal subjective knee function as measured by IKDC 2000. With a sensitivity of 88%, the cross-over hop test most accurately identified those with normal function. This is likely because of the fact that of all the tests, the cross-over hop is the most functionally demanding as it requires coordination and strength in the frontal, sagittal, and coronal planes. Near normal values in this test indicate improved neuromuscular control of the leg.
At 1 year, those with normal knee function had median LSI values of 93% for the single-leg, cross-over, and triple hop tests, while the median value was 96% for the 6-m timed hop. Reinke et al82 performed a similar investigation with a smaller cohort of patients and found that the triple hop test best correlated with the IKDC score as well as certain subsets of the Knee Injury and Osteoarthritis Outcomes Score (KOOS).
Another common functional test reported in the literature is knee flexion and extension strength testing. In examining the results presented in Table 4, 6 months following ACL reconstruction, mean LSI values for isokinetic knee flexion were in the range of 80% to 90%, with correction to near normal values by 1 year. This trend was not seen in the results for isokinetic knee extension, with values commonly in the 70% range at 6 months and remaining below 90% in almost all categories at the 1-year mark postoperatively. These observations are supported by the data presented in Table 5, with significant knee extension deficits (compared with knee flexion LSI) at a number of time points postoperatively. These results compare with other investigations that have looked at isokinetic strength between BPTB and hamstring autograft reconstruction techniques. Wipfler et al102 reported isokinetic knee flexion to be 99% and 91% in the BPTB and hamstring autograft groups at 1-year follow-up, while extension was 87% and 92%, respectively. Aglietti et al2 also reported significantly increased isokinetic extension strength deficits at 1 year follow-up for BPTB versus hamstring autograft patients without concomitant decreased flexion strength in the hamstring graft group.
While the results of functional testing have not been shown to predict return to sport, Hewett et al35 proposed that strength training with correction of faulty movement biomechanics and balance training are the most effective methods for preventing ACL injuries. Many of these factors can be tested using the motion analysis and force plate data described in Table 3. The effectiveness of these programs in the prevention of initial ACL injury as well as other lower extremity injuries has been demonstrated.49,61,94,101 Mandelbaum et al61 investigated whether the use of a neuromuscular and proprioceptive performance program was effective at decreasing the incidence of ACL injury in an elite population of female soccer players. In their cohort study, they found that the program decreased the incidence of ACL injury by 88% and 74% in years 1 and 2, respectively, after initiation of the program.
While normative values as well as values that correlate with perceived “normal” knee function can be provided for functional testing following ACL reconstruction, objective evidence is lacking for determining return to play criteria based on an exact result of a functional test. Many authors have advocated using multiple tests to determine full return to play status.60,82 Barber-Westin and Noyes9 report that their protocol includes a less than 10% deficit in strength of the quadriceps and hamstring on isokinetic testing at 180 deg/s; less than 15% deficit in lower limb symmetry for single-hop, triple hop, cross-over hop, and timed hop; greater than 60% normalized knee separation distance on a video drop-jump test; as well as a normal physical examination. For even beginning a return-to-sport rehabilitation regimen, Myer et al71 recommend a minimum IKDC score of 70, no postsurgical history of giving way or a negative pivot shift, and a minimum baseline strength knee extension peak torque/body mass of 40% and 30% at 300 deg/s and 60% and 50% at 180 deg/s for males and females, respectively. The last stage the athlete must pass before slow reintegration into full athletic activity includes drop vertical jump landing force within 15% LSI, modified agility test (MAT) time within 10%, single limb average peak power test for 10 seconds within 15%, and a perfect score on the tuck jump or improvement of 20 percentage points from the initial score.71
Limitations of this investigation are based in the weaknesses of the studies included. One potential is that the time frame for functional testing was slightly different than that reported. For example, testing of a patient at 5 or 7 months following surgery, versus at the 6-month time point, may slightly affect results because of the increased or decreased time that the patient has had for rehabilitation. It is possible that some studies reporting on functional testing following ACL reconstruction that met our inclusion and exclusion criteria were not captured. This is minimized, however, with the use of 3 separate databases and cross-referencing of reference sections for investigations that the search algorithm may have missed.
Conclusion
This investigation provides data on all published functional testing following primary ACL reconstruction. The most commonly reported tests were the hop tests as well as isokinetic knee flexion and extension strength. Knee extension strength lagged behind that of knee flexion strength in all graft types, underlining the importance of quadriceps rehabilitation postoperatively. Those with hamstring autografts were found to have decreased isokinetic knee flexion strength versus BPTB autograft patients, while there were no differences in isokinetic knee extension strength between groups at any time point. The values summarized in this investigation should serve as guidance to aid in decision-making when deciding when to return the athlete to unrestricted play following ACL reconstruction.
NOTE
i. Online search term: (((((((((((((((((((((((anterior[Title/Abstract]) AND cruciate[Title/Abstract]) AND ligament[Title/Abstract])) OR acl[Title/Abstract])) AND reconstruction[Title/Abstract] AND (English[lang]))) AND (((((functional[Title/Abstract]) AND test[Title/Abstract] AND (English[lang]))) OR rehab[Title/Abstract]) OR rehabilitation[Title/Abstract] AND (English[lang])) AND (English[lang]))) NOT shoulder[Title/Abstract]) NOT elbow[Title/Abstract]) NOT wrist[Title/Abstract]) NOT hand[Title/Abstract]) NOT finger[Title/Abstract]) NOT pelvis[Title/Abstract]) NOT spine[Title/Abstract]) NOT hip[Title/Abstract]) NOT foot[Title/Abstract]) NOT ankle[Title/Abstract]) NOT cadaver[Title/Abstract]) NOT cadaveric[Title/Abstract]) NOT pcl[Title/Abstract]) NOT posterior[Title/Abstract] AND (English[lang])).
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: C.A.B. is an unpaid consultant for The Foundry and is on the editorial board of the American Journal of Sports Medicine. N.N.V. receives royalties from Smith & Nephew; is a paid speaker for Arthrosurface; is a consultant for Smith & Nephew and Arthrex; owns stock options in Omeros; receives research support from Arthrex, Smith & Nephew, Athletico, ConMed Linvatec, Miomed, Mitek, and Arthrosurface; receives royalties/publisher support from Vindico Medical-Orthopedics Hyperguide and Arthroscopy; and is a board member of the Journal of Knee Surgery, Arthroscopy, SLACK Inc, and the Arthroscopy Association Learning Center committee. B.J.C. is a board member of the Arthroscopy Association of North America; is a consultant for Genzyme, Arthrex, Zimmer, Carticept, Regentis, DJO, and Johnson & Johnson; receives research support from Major League Baseball, MTF, OREF, NIH/MIMAS, Arthrex, Zimmer, Arthrosurface, Medipost, and Johnson & Johnson; and receives royalties from Arthrex and DJO. B.R.B. receives research support from Arthrex, ConMed Linvatec, DJ Orthopaedics, Ossur, Smith & Nephew, and Tornier; receives publisher compensation from SLACK Inc; and is a board member of the American Orthopaedic Society for Sports Medicine and Orthopaedics Today.
References
- 1. Ageberg E, Thomee R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two- to five-year followup. Arthritis Rheum. 2008;59:1773–1779. [DOI] [PubMed] [Google Scholar]
- 2. Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86-A:2143–2155. [PubMed] [Google Scholar]
- 3. Ahlden M, Sernert N, Karlsson J, Kartus J. Outcome of anterior cruciate ligament reconstruction with emphasis on sex-related differences. Scand J Med Sci Sports. 2012;22:618–626. [DOI] [PubMed] [Google Scholar]
- 4. Allen AD, Sitler MR, Marchetto P, Kelly JD, Mattacola CG. Assessment of the endoscopic semitendinosus/gracilis autograft procedure with interference screw fixation for reconstruction of the anterior cruciate ligament. Orthopedics. 2001;24:347–353. [DOI] [PubMed] [Google Scholar]
- 5. Angelozzi M, Madama M, Corsica C, et al. Rate of force development as an adjunctive outcome measure for return-to-sport decisions after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:772–780. [DOI] [PubMed] [Google Scholar]
- 6. Augustsson J, Thomee R, Karlsson J. Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2004;12:350–356. [DOI] [PubMed] [Google Scholar]
- 7. Aune AK, Holm I, Risberg MA, Jensen HK, Steen H. Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. Am J Sports Med. 2001;29:722–728. [DOI] [PubMed] [Google Scholar]
- 8. Baltaci G, Yilmaz G, Atay AO. The outcomes of anterior cruciate ligament reconstructed and rehabilitated knees versus healthy knees: a functional comparison. Acta Orthop Traumatol Turc. 2012;46:186–195. [DOI] [PubMed] [Google Scholar]
- 9. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1697–1705. [DOI] [PubMed] [Google Scholar]
- 10. Birmingham TB, Bryant DM, Giffin JR, et al. A randomized controlled trial comparing the effectiveness of functional knee brace and neoprene sleeve use after anterior cruciate ligament reconstruction. Am J Sports Med. 2008;36:648–655. [DOI] [PubMed] [Google Scholar]
- 11. Brosky JA, Jr, Nitz AJ, Malone TR, Caborn DN, Rayens MK. Intrarater reliability of selected clinical outcome measures following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:39–48. [DOI] [PubMed] [Google Scholar]
- 12. Cameron SE, Wilson W, St Pierre P. A prospective, randomized comparison of open vs arthroscopically assisted ACL reconstruction. Orthopedics. 1995;18:249–252. [DOI] [PubMed] [Google Scholar]
- 13. Cuellar JM, Scuderi GJ, Cuellar VG, Golish SR, Yeomans DC. Diagnostic utility of cytokine biomarkers in the evaluation of acute knee pain. J Bone Joint Surg Am. 2009;91:2313–2320. [DOI] [PubMed] [Google Scholar]
- 14. Czamara A, Tomaszewski W, Bober T, Lubarski B. The effect of physiotherapy on knee joint extensor and flexor muscle strength after anterior cruciate ligament reconstruction using hamstring tendon. Med Sci Monit. 2011;17:CR35–CR41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. De Carlo MS, Sell KE. The effects of the number and frequency of physical therapy treatments on selected outcomes of treatment in patients with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1997;26:332–339. [DOI] [PubMed] [Google Scholar]
- 16. de Jong SN, van Caspel DR, van Haeff MJ, Saris DB. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23:21–28, 28.e21–28.e23. [DOI] [PubMed] [Google Scholar]
- 17. Fabbriciani C, Milano G, Mulas PD, Ziranu F, Severini G. Anterior cruciate ligament reconstruction with doubled semitendinosus and gracilis tendon graft in rugby players. Knee Surg Sports Traumatol Arthrosc. 2005;13:2–7. [DOI] [PubMed] [Google Scholar]
- 18. Fabis J. The impact of a isokinetic training program on the peak torque of the quadriceps and knee flexors after anterior cruciate ligament reconstruction with hamstrings. Ortop Traumatol Rehabil. 2007;9:527–531. [PubMed] [Google Scholar]
- 19. Flanagan EP, Galvin L, Harrison AJ. Force production and reactive strength capabilities after anterior cruciate ligament reconstruction. J Athl Train. 2008;43:249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fremerey R, Lobenhoffer P, Skutek M, Gerich T, Bosch U. Proprioception in anterior cruciate ligament reconstruction. Endoscopic versus open two-tunnel technique. A prospective study. Int J Sports Med. 2001;22:144–148. [DOI] [PubMed] [Google Scholar]
- 21. Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br. 2000;82:801–806. [DOI] [PubMed] [Google Scholar]
- 22. Fu FH, West R, Musahl V, Vyas D. Anatomic single- and double-bundle anterior cruciate ligament (ACL) reconstruction. http://www.orthonet.pitt.edu/content/DoubleBundle.htm. Accessed January 13, 2013.
- 23. Garrison JC, Shanley E, Thigpen C, Geary R, Osler M, Delgiorno J. The reliability of the vail sport test as a measure of physical performance following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2012;7:20–30. [PMC free article] [PubMed] [Google Scholar]
- 24. Gerhard P, Bolt R, Duck K, Mayer R, Friederich NF, Hirschmann MT. Long-term results of arthroscopically assisted anatomical single-bundle anterior cruciate ligament reconstruction using patellar tendon autograft: are there any predictors for the development of osteoarthritis? Knee Surg Sports Traumatol Arthrosc. 2013;21:957–964. [DOI] [PubMed] [Google Scholar]
- 25. Ghodadra NS, Mall NA, Grumet R, et al. Interval arthrometric comparison of anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft versus allograft: do grafts attenuate within the first year postoperatively? Am J Sports Med. 2012;40:1347–1354. [DOI] [PubMed] [Google Scholar]
- 26. Grant JA, Mohtadi NG. Two- to 4-year follow-up to a comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38:1389–1394. [DOI] [PubMed] [Google Scholar]
- 27. Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39:2347–2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Harilainen A, Sandelin J, Vanhanen I, Kivinen A. Knee brace after bone-tendon-bone anterior cruciate ligament reconstruction. Randomized, prospective study with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1997;5:10–13. [DOI] [PubMed] [Google Scholar]
- 29. Harrison EL, Duenkel N, Dunlop R, Russell G. Evaluation of single-leg standing following anterior cruciate ligament surgery and rehabilitation. Phys Ther. 1994;74:245–252. [DOI] [PubMed] [Google Scholar]
- 30. Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Oorthop Sports Phys Ther. 2010;40:141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Heckmann TP, Noyes FR, Barber-Westin SD. Rehabilitation after ACL reconstruction In: FR Noyes, SD Barber-Westin, eds. ACL Injuries in the Female Athlete: Causes, Impacts, and Conditioning Programs. New York, NY: Springer; 2012:427–454. [Google Scholar]
- 32. Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15:402–414. [DOI] [PubMed] [Google Scholar]
- 33. Heijne A, Werner S. A 2-year follow-up of rehabilitation after ACL reconstruction using patellar tendon or hamstring tendon grafts: a prospective randomised outcome study. Knee Surg Sports Traumatol Arthrosc. 2010;18:805–813. [DOI] [PubMed] [Google Scholar]
- 34. Henriksson M, Rockborn P, Good L. Range of motion training in brace vs. plaster immobilization after anterior cruciate ligament reconstruction: a prospective randomized comparison with a 2-year follow-up. Scand J Med Sci Sports. 2002;12:73–80. [DOI] [PubMed] [Google Scholar]
- 35. Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34:490–498. [DOI] [PubMed] [Google Scholar]
- 36. Hohmann E, Tetsworth K, Bryant A. Physiotherapy-guided versus home-based, unsupervised rehabilitation in isolated anterior cruciate injuries following surgical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1158–1167. [DOI] [PubMed] [Google Scholar]
- 37. Holm I, Hammer S, Larsen S, Nordsletten L, Steen H. Can a regular leg extension bench be used in testing deficits of the quadriceps muscle during rehabilitation? Scand J Med Sci Sports. 1995;5:29–35. [DOI] [PubMed] [Google Scholar]
- 38. Hopper DM, Creagh MJ, Formby PA, Goh SC, Boyle JJ, Strauss GR. Functional measurement of knee joint position sense after anterior cruciate ligament reconstruction. Arch Phys Med Rehabil. 2003;84:868–872. [DOI] [PubMed] [Google Scholar]
- 39. Hopper DM, Strauss GR, Boyle JJ, Bell J. Functional recovery after anterior cruciate ligament reconstruction: a longitudinal perspective. Arch Phys Med Rehabil. 2008;89:1535–1541. [DOI] [PubMed] [Google Scholar]
- 40. Iriuchishima T, Horaguchi T, Morimoto Y, et al. Intensity of physiotherapy after anterior cruciate ligament reconstruction: a comparison of two rehabilitation regimen. Arch Orthop Trauma Surg. 2010;130:1053–1058. [DOI] [PubMed] [Google Scholar]
- 41. Ito Y, Deie M, Adachi N, et al. A prospective study of 3-day versus 2-week immobilization period after anterior cruciate ligament reconstruction. Knee. 2007;14:34–38. [DOI] [PubMed] [Google Scholar]
- 42. Jansson KA, Linko E, Sandelin J, Harilainen A. A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:12–18. [DOI] [PubMed] [Google Scholar]
- 43. Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop Scand. 2004;75:594–599. [DOI] [PubMed] [Google Scholar]
- 44. Karasel S, Akpinar B, Gulbahar S, et al. Clinical and functional outcomes and proprioception after a modified accelerated rehabilitation program following anterior cruciate ligament reconstruction with patellar tendon autograft. Acta Orthop Traumatol Turc. 2010;44:220–228. [DOI] [PubMed] [Google Scholar]
- 45. Kartus J, Stener S, Kohler K, Sernert N, Eriksson BI, Karlsson J. Is bracing after anterior cruciate ligament reconstruction necessary? A 2-year follow-up of 78 consecutive patients rehabilitated with or without a brace. Knee Surg Sports Traumatol Arthrosc. 1997;5:157–161. [DOI] [PubMed] [Google Scholar]
- 46. Keays SL, Bullock-Saxton J, Keays AC. Strength and function before and after anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2000;(373):174–183. [DOI] [PubMed] [Google Scholar]
- 47. Ko MS, Yang SJ, Ha JK, Choi JY, Kim JG. Correlation between hamstring flexor power restoration and functional performance test: 2-year follow-up after ACL reconstruction using hamstring autograft. Knee Surg Relat Res. 2012;24:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kong DH, Yang SJ, Ha JK, Jang SH, Seo JG, Kim JG. Validation of functional performance tests after anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2012;24:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2011;165:1033–1040. [DOI] [PubMed] [Google Scholar]
- 50. Landes S, Nyland J, Elmlinger B, Tillett E, Caborn D. Knee flexor strength after ACL reconstruction: comparison between hamstring autograft, tibialis anterior allograft, and non-injured controls. Knee Surg Sports Traumatol Arthrosc. 2010;18:317–324. [DOI] [PubMed] [Google Scholar]
- 51. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377–381. [DOI] [PubMed] [Google Scholar]
- 52. Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:34–42. [DOI] [PubMed] [Google Scholar]
- 53. Laxdal G, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and hamstring tendon grafts for anterior cruciate ligament reconstruction in male patients. Knee Surg Sports Traumatol Arthrosc. 2007;15:115–125. [DOI] [PubMed] [Google Scholar]
- 54. Lee BI, Kwon SW, Kim JB, Choi HS, Min KD. Comparison of clinical results according to amount of preserved remnant in arthroscopic anterior cruciate ligament reconstruction using quadrupled hamstring graft. Arthroscopy. 2008;24:560–568. [DOI] [PubMed] [Google Scholar]
- 55. Lentz TA, Tillman SM, Indelicato PA, Moser MW, George SZ, Chmielewski TL. Factors associated with function after anterior cruciate ligament reconstruction. Sports Health. 2009;1:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Lephart SM, Kocher MS, Harner CD, Fu FH. Quadriceps strength and functional capacity after anterior cruciate ligament reconstruction. Patellar tendon autograft versus allograft. Am J Sports Med. 1993;21:738–743. [DOI] [PubMed] [Google Scholar]
- 57. Lewek M, Rudolph K, Axe M, Snyder-Mackler L. The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002;17:56–63. [DOI] [PubMed] [Google Scholar]
- 58. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35:740–748. [DOI] [PubMed] [Google Scholar]
- 59. Lindstrom M, Strandberg S, Wredmark T, Fellander-Tsai L, Henriksson M. Functional and muscle morphometric effects of ACL reconstruction. A prospective CT study with 1 year follow-up. Scand J Med Sci Sports. 2013;23:431–442. [DOI] [PubMed] [Google Scholar]
- 60. Logerstedt D, Grindem H, Lynch A, et al. Single-legged hop tests as predictors of self-reported knee function after anterior cruciate ligament reconstruction: the Delaware-Oslo ACL cohort study. Am J Sports Med. 2012;40:2348–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–1010. [DOI] [PubMed] [Google Scholar]
- 62. Mattacola CG, Jacobs CA, Rund MA, Johnson DL. Functional assessment using the step-up-and-over test and forward lunge following ACL reconstruction. Orthopedics. 2004;27:602–608. [DOI] [PubMed] [Google Scholar]
- 63. McDevitt ER, Taylor DC, Miller MD, et al. Functional bracing after anterior cruciate ligament reconstruction: a prospective, randomized, multicenter study. Am J Sports Med. 2004;32:1887–1892. [DOI] [PubMed] [Google Scholar]
- 64. Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17-20 years. Int Orthop. 2011;35:1093–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. 2000;8:337–342. [DOI] [PubMed] [Google Scholar]
- 66. Mittlmeier T, Weiler A, Söhn T, et al. Novel Award Second Prize Paper. Functional monitoring during rehabilitation following anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 1999;14:576–584. [DOI] [PubMed] [Google Scholar]
- 67. Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Khorrami M, Negahban H. Static and dynamic postural control in competitive athletes after anterior cruciate ligament reconstruction and controls. Knee Surg Sports Traumatol Arthrosc. 2012;20:1603–1610. [DOI] [PubMed] [Google Scholar]
- 68. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 69. Murray JR, Lindh AM, Hogan NA, et al. Does anterior cruciate ligament reconstruction lead to degenerative disease? Thirteen-year results after bone-patellar tendon-bone autograft. Am J Sports Med. 2012;40:404–413. [DOI] [PubMed] [Google Scholar]
- 70. Myer GD, Martin L, Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40:2256–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36:385–402. [DOI] [PubMed] [Google Scholar]
- 72. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41:377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Nakayama Y, Shirai Y, Narita T, Mori A, Kobayashi K. Knee functions and a return to sports activity in competitive athletes following anterior cruciate ligament reconstruction. J Nippon Med Sch. 2000;67:172–176. [DOI] [PubMed] [Google Scholar]
- 74. Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011;41:553–559. [DOI] [PubMed] [Google Scholar]
- 75. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38:1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Petschnig R, Baron R, Albrecht M. The relationship between isokinetic quadriceps strength test and hop tests for distance and one-legged vertical jump test following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1998;28:23–31. [DOI] [PubMed] [Google Scholar]
- 77. Pfeifer K, Banzer W. Motor performance in different dynamic tests in knee rehabilitation. Scand J Med Sci Sports. 1999;9:19–27. [DOI] [PubMed] [Google Scholar]
- 78. Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23:1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 79. Reat JF, Lintner DM. One- versus two-incision ACL reconstruction. A prospective, randomized study. Am J Knee Surg. 1997;10:198–208. [PubMed] [Google Scholar]
- 80. Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87:337–349. [DOI] [PubMed] [Google Scholar]
- 81. Reider B, Arcand MA, Diehl LH, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy. 2003;19:2–12. [DOI] [PubMed] [Google Scholar]
- 82. Reinke EK, Spindler KP, Lorring D, et al. Hop tests correlate with IKDC and KOOS at minimum of 2 years after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1806–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Risberg MA, Ekeland A. Assessment of functional tests after anterior cruciate ligament surgery. J Orthop Sports Phys Ther. 1994;19:212–217. [DOI] [PubMed] [Google Scholar]
- 84. Risberg MA, Holm I. The long-term effect of 2 postoperative rehabilitation programs after anterior cruciate ligament reconstruction: a randomized controlled clinical trial with 2 years of follow-up. Am J Sports Med. 2009;37:1958–1966. [DOI] [PubMed] [Google Scholar]
- 85. Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87:737–750. [DOI] [PubMed] [Google Scholar]
- 86. Risberg MA, Holm I, Steen H, Beynnon BD. Sensitivity to changes over time for the IKDC form, the Lysholm score, and the Cincinnati knee score. A prospective study of 120 ACL reconstructed patients with a 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1999;7:152–159. [DOI] [PubMed] [Google Scholar]
- 87. Rosenberg TD, Franklin JL, Baldwin GN, Nelson KA. Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:519–525. [DOI] [PubMed] [Google Scholar]
- 88. Rudroff T. Functional capability is enhanced with semitendinosus than patellar tendon ACL repair. Med Sci Sports Exerc. 2003;35:1486–1492. [DOI] [PubMed] [Google Scholar]
- 89. Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Segawa H, Omori G, Koga Y, Kameo T, Iida S, Tanaka M. Rotational muscle strength of the limb after anterior cruciate ligament reconstruction using semitendinosus and gracilis tendon. Arthroscopy. 2002;18:177–182. [DOI] [PubMed] [Google Scholar]
- 91. Shelbourne KD, Foulk DA. Timing of surgery in acute anterior cruciate ligament tears on the return of quadriceps muscle strength after reconstruction using an autogenous patellar tendon graft. Am J Sports Med. 1995;23:686–689. [DOI] [PubMed] [Google Scholar]
- 92. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992;15:256–264. [DOI] [PubMed] [Google Scholar]
- 93. Shelbourne KD, Rubinstein RA, Jr, VanMeter CD, McCarroll JR, Rettig AC. Correlation of remaining patellar tendon width with quadriceps strength after autogenous bone-patellar tendon-bone anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:774–777. [DOI] [PubMed] [Google Scholar]
- 94. Soligard T, Myklebust G, Steffen K, et al. Comprehensive warm-up programme to prevent injuries in young female footballers: cluster randomised controlled trial. BMJ. 2008;337:a2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Souissi S, Wong DP, Dellal A, Croisier JL, Ellouze Z, Chamari K. Improving functional performance and muscle power 4-to-6 months after anterior cruciate ligament reconstruction. J Sports Sci Med. 2011;10:655–664. [PMC free article] [PubMed] [Google Scholar]
- 96. Struewer J, Frangen TM, Ishaque B, et al. Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop. 2012;36:171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Suomalainen P, Jarvela T, Paakkala A, Kannus P, Jarvinen M. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med. 2012;40:1511–1518. [DOI] [PubMed] [Google Scholar]
- 98. Svensson M, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction in female patients. Knee Surg Sports Traumatol Arthrosc. 2006;14:278–286. [DOI] [PubMed] [Google Scholar]
- 99. Thomee R, Neeter C, Gustavsson A, et al. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1143–1151. [DOI] [PubMed] [Google Scholar]
- 100. Timoney JM, Inman WS, Quesada PM, et al. Return of normal gait patterns after anterior cruciate ligament reconstruction. Am J Sports Med. 1993;21:887–889. [DOI] [PubMed] [Google Scholar]
- 101. Walden M, Atroshi I, Magnusson H, Wagner P, Hagglund M. Prevention of acute knee injuries in adolescent female football players: cluster randomised controlled trial. BMJ. 2012;344:e3042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy. 2011;27:653–665. [DOI] [PubMed] [Google Scholar]
- 103. Wojtys EM, Huston LJ. Longitudinal effects of anterior cruciate ligament injury and patellar tendon autograft reconstruction on neuromuscular performance. Am J Sports Med. 2000;28:336–344. [DOI] [PubMed] [Google Scholar]
- 104. Yabroudi MA, Irrgang JJ. Rehabilitation and return to play after anatomic anterior cruciate ligament reconstruction. Clin Sports Med. 2013;32:165–175. [DOI] [PubMed] [Google Scholar]
- 105. Yosmaoglu HB, Baltaci G, Kaya D, Ozer H. Tracking ability, motor coordination, and functional determinants after anterior cruciate ligament reconstruction. J Sport Rehabil. 2011;20:207–218. [DOI] [PubMed] [Google Scholar]
- 106. Yosmaoglu HB, Baltaci G, Ozer H, Atay A. Effects of additional gracilis tendon harvest on muscle torque, motor coordination, and knee laxity in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1287–1292. [DOI] [PubMed] [Google Scholar]
- 107. Yosmaoglua HB, Baltaci G, Kaya D, Ozer H, Atay A. Comparison of functional outcomes of two anterior cruciate ligament reconstruction methods with hamstring tendon graft. Acta Orthop Traumatol Turc. 2011;45:240–247. [DOI] [PubMed] [Google Scholar]