Abstract
Background:
Since it was developed, hip arthroscopy has become the favored treatment for femoroacetabular impingement. Due to recent considerable improvements, the indications for this technique have been widely extended. Injuries of the rectus femoris tendon origin, after an acute phase, could result in a chronic tendinopathy with calcium hydroxyapatite crystal deposition, leading to pain and loss of function. Traditionally, this condition is addressed by local injection of anesthetic and corticosteroids or, when conservative measures fail, by open excision of the calcific lesion by an anterior approach.
Purpose:
To assess whether arthroscopic excision of calcification of the proximal rectus is a safe and effective treatment.
Study Design:
Case series; Level of evidence, 4.
Methods:
Outcomes were studied from 6 top amateur athletes (age range, 30-43 years; mean, 32.6 years) affected by calcification of the proximal rectus who underwent arthroscopic excision of the calcification. Patients were preoperatively assessed radiographically, and diagnosis was confirmed by a 3-dimensional computed tomography scan. To evaluate the outcome, standardized hip rating scores were used pre- and postoperatively (at 6 and 12 months): the Hip disability and Osteoarthritis Outcome Score, Oxford Hip Score, and Modified Harris Hip Score. Moreover, visual analog scales (VAS) for pain, sport activity level (SAL), and activities of daily living (ADL) were also used.
Results:
One year after surgery, all patients reported satisfactory outcomes, with 3 of 6 rating their return-to-sport level as high as preinjury level, and the remaining 3 with a percentage higher than 80%. Five patients ranked their ability to carry on daily activities at 100%. Statistical analysis showed significant improvement of the Oxford Hip Score, the Modified Harris Hip Score, and all 3 VAS subscales (pain, SAL, and ADL) from pre- to latest postoperative assessment (P < .05).
Conclusion:
Arthroscopic excision of rectus femoris tendon calcification yields satisfying results with few risks to the patient as well as rapid recovery.
Clinical Relevance:
The recent improvements in hip arthroscopy give the opportunity to address an increasing number of hip conditions effectively and safely, with rapid recovery for the patient. Arthroscopic excision of rectus femoris tendon calcification can be considered a feasible option, with few risks to the patient, rapid recovery, and satisfying outcomes.
Keywords: rectus femoris tendon calcification, hip arthroscopy, sport-related hip injury, hip pain
Heterotopic calcification (HC) could be an expression of chronic tendinopathy. Although this condition is mostly found in rotator cuff tendinopathy, it can occur in other joints, such as the elbow, wrist, knee, and foot.1,7,9,21 With regard to the hip, chronic tendinopathy of the trochanteric tendons is well described19 as causing an inflammatory reaction with tenderness, local swelling, and pain through the posterolateral aspect of the hip. Calcification of the proximal rectus femoris tendon has also been described, although rarely, following avulsion (with or without bony fragment) or tendon rupture (partial or complete) of the rectus femoris origin in young people, especially in kicking athletes and in football players.12 Ouellette et al23 found a 0.5% incidence of rectus femoris origin injuries on a retrospective revision of 3160 pelvis and hip magnetic resonance images, and it has been shown that after the acute phase, an injury of rectus femoris origin could lead to HC, resulting in pain and loss of function.3,12,18,26
A similar condition has been described after an avulsion of the anterior inferior iliac spine (AIIS). The healing process could lead to an extra bony mass extending inferiorly and resulting in a prominent AIIS that eventually will impinge on the femoral neck when the hip is flexed over 90°. This has been referred to as iliac spine impingement, AIIS impingement, or subspine impingement.20
Calcification of the rectus femoris tendon has been traditionally addressed by local injection of anesthetic and corticosteroids or by open excision of the lesion through an anterior (Smith-Petersen) approach.3 The same approach is used for subspine impingement. In recent years, hip arthroscopy has been proposed, with satisfactory outcomes, as a less invasive surgical alternative for both conditions.10,14,24 In this retrospective case-series study, we report on the outcomes of 6 consecutive patients who underwent arthroscopic excision of rectus femoris calcification.
Materials and Methods
Six consecutive male patients presented to Gvm Care and Research Hospital and Clinics (Ravenna, Italy) between September 2009 and July 2012 for chronic (>6 months) pain and impaired function of the hip, unresponsive to nonsteroidal anti-inflammatory drugs (NSAIDs). All patients were top amateur athletes (soccer players, 2-3 games per week). None had a history of previous hip issues or any other injury of note. Patients complained of pain at the anterolateral aspect of the hip, difficulty with weightbearing, and limited hip extension, preferring to hold the affected hip with 10° to 30° of flexion. A standard radiograph showed an HC close to the superior aspect of the acetabulum (Figures 1 and 2). To exclude other pathologies, sedimentation rates, C-reactive protein, rheumatoid latex test, serum uric acid level, white blood cell count, and blood chemistry were all investigated. A computed tomography scan was performed in all patients. Blood tests showed values within normal limits, except for C-reactive protein levels, which showed slightly higher values than normal (mean, 2.01 mg/dL; range, 0.85-2.56 mg/dL). Computed tomography scans confirmed the presence of a calcification of the direct head of the rectus femoris. Patients were therefore indicated for arthroscopic excision of the HC. Concomitant pathologies and relative treatment procedures are reported in Table 1.
Figure 1.

Anteroposterior radiographic view of a right hip. The tendon appears calcified in its proximal insertion.
Figure 2.

Axial radiographic view of a right hip. The tendon appears calcified in its proximal insertion.
TABLE 1.
Concomitant Pathologies and Relative Procedures
| Patient | Age, y | Comorbidity | Procedure |
|---|---|---|---|
| 1 | 30 | Labral tear | Debridement |
| 2 | 30 | Labral tear | Debridement |
| 3 | 31 | None | None |
| 4 | 30 | Cam-type impingement | Cam resection |
| 5 | 33 | None | None |
| 6 | 43 | Chondral defect | Debridement |
Outcome Evaluation
To evaluate the outcome, pre- and postoperative (6 and 12 months) standardized hip rating scores were used: the Hip disability and Osteoarthritis Outcome Score (HOOS),22 Oxford Hip Score (OHS),8 and modified Harris Hip Score (mHHS).5 Moreover, visual analog scales (VASs) were used for pain, sport activity level (SAL), and activities of daily living (ADL), expressed as a subjective value between 0 and 100 (100 = preinjury sport level, 0 = inability to play sport). The Wilcoxon test was used to compare the outcomes scores. Since the sample size was less than 10, the W value was used to assess whether differences between preoperative and postoperative scores were significant or not.
Surgical Technique
A standard fracture table was used with the patient in a supine position.4 The operative limb was placed with the hip in slight abduction and internal rotation. The contralateral limb was positioned in extension and neutral rotation, with the foot in a support applying a counterbalancing traction. Countertraction, lateralized toward the operative hip, was placed in the perineal region. Two standard portals were used. Using the 70° arthroscope, the anterolateral portal (ALP) was performed. The ALP provides a complete view of the central compartment for the treatment of possible associated intra-articular pathologies. Once inside the hip joint with the camera through the ALP, the midanterior portal was created via direct visualization. An arthroscopic knife (retractable cannulated knife; Arthrex) was introduced to perform an interportal capsulotomy parallel to the labrum. Coagulation of bleeding vessels was achieved with a radiofrequency device (EFLEX Electrothermal Ablator Probe; Smith & Nephew). The central compartment was addressed first. Concomitant lesions (labral tear, chondral lesion, impingement) were evaluated and eventually treated (Table 1). After central compartment examination and treatment was completed, the traction was removed and attention was focused to the calcification of the rectus femoris. A shaver was used to clear all soft tissue from the overhanging acetabulum and to better delimit the plane between the acetabular rim and the calcification. Using an extra-long, 5.5-mm full-radius shaver and a radiofrequency device, complete exposure of the calcification was achieved (Figures 3 –6). When possible, care was taken in detaching the minimum amount of fibers of the direct head of the rectus femoris from its insertion site. Using the image intensifier as a guide, the calcification was removed using a 5.5-mm bur (DYONICS Full Radius; Smith & Nephew) (Figure 9). During the entire procedure, both dynamic direct visualization and fluoroscopic evaluation of the amount of resection were performed (Figures 7 and 8). Patients were discharged the day after the procedure. Weightbearing was permitted as tolerated, but extension of the hip was forbidden for 3 weeks to avoid excessive elongation of the rectus femoris tendon. To avoid recurrence, a course of celecoxib was ordered (200 mg/d for 4 weeks).
Figure 3.
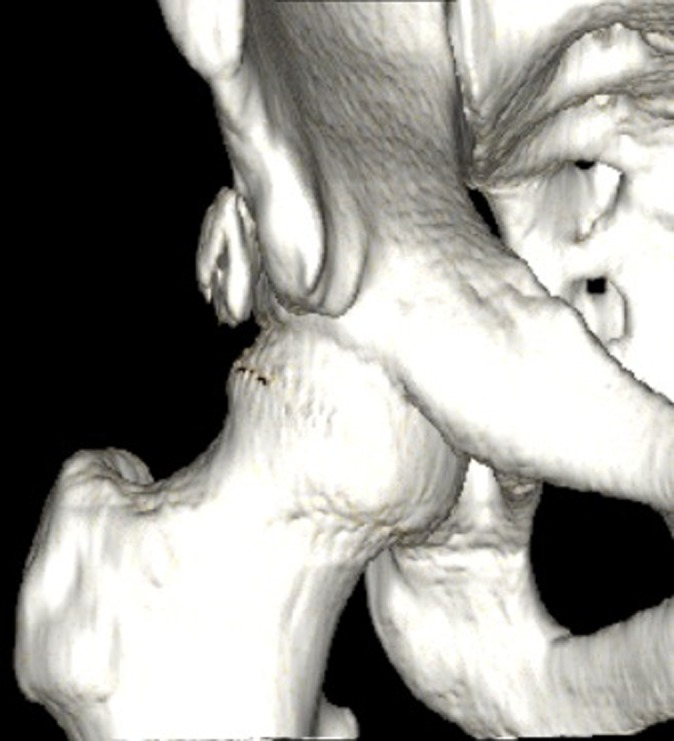
Three-dimensional computed tomography scan showing tendon calcification.
Figure 4.

Fluoroscopic view. The calcification has been reached by the radiofrequency ablator.
Figure 5.
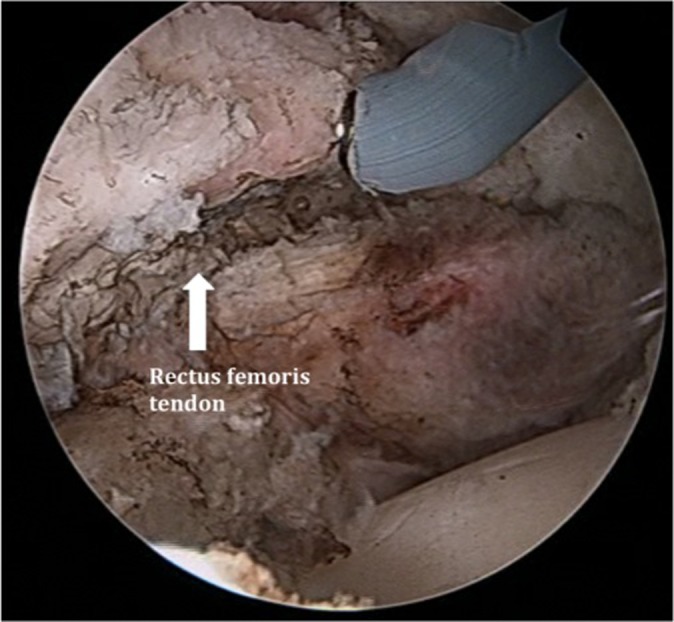
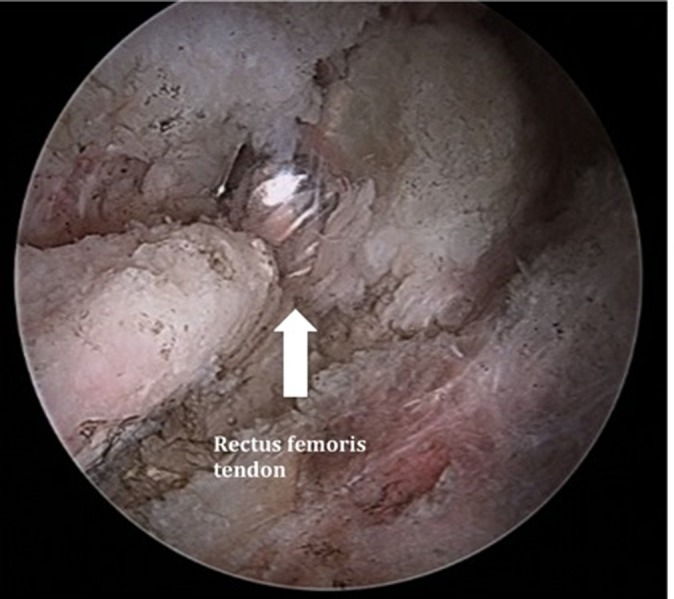
Arthroscopic view. The calcification has been isolated.
Figure 6.
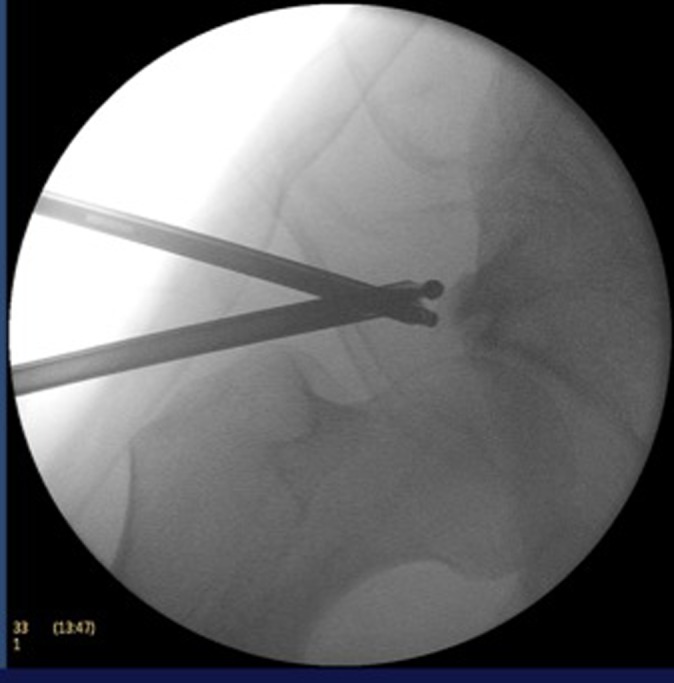
Fluoroscopic view showing the decompression process.
Figure 9.
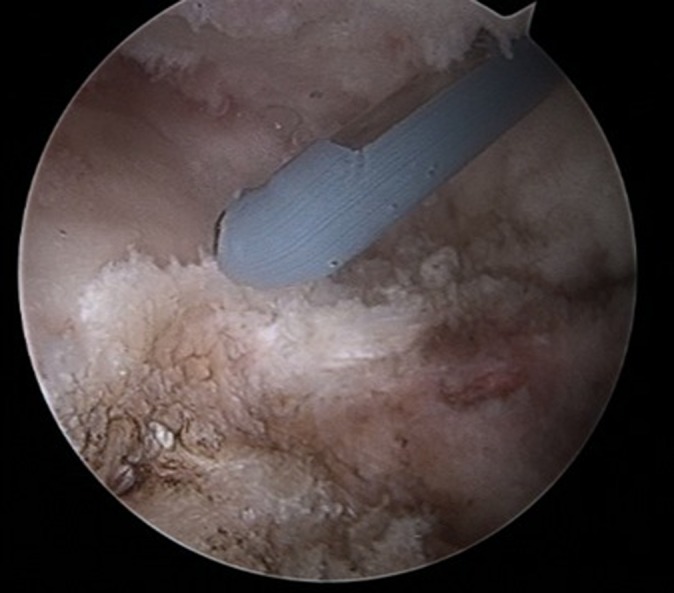
Arthroscopic view. The calcification has been completely removed.
Figure 7.
Arthroscopic view showing the decompression.
Figure 8.

Fluoroscopic view showing complete removal of the calcified tendon.
Results
The average age of the patients was 32.6 years (range, 30-43 years). The mean time from symptoms to surgery was 13.7 months. After surgery, all patients reported satisfactory outcomes, with 3 of 6 patients rating their return to sport level as high as preinjury (P < .05), and the remaining 3 returned at a percentage above 80% according to the SAL score at a mean of 8 weeks (range, 4-9 weeks) from surgery. Five of 6 patients ranked their ability to carry on daily activities as 100%. Comparing pre- with postoperative values at 1 year from surgery, the statistical analysis showed significant improvement for HOOS (mean, 91.1 ± 8), OHS (mean, 46.5 ± 0.8), mHHS (mean, 96.9 ± 4.4), and the VAS for pain (mean, 0.2 ± 0.4), ADL (mean, 98.3 ± 3.7), and SAL (mean, 91.6 ± 8.9) from pre- to postoperative (P < .05) (Table 2).
TABLE 2.
Pre- and Postoperative Pain and Function Scoresa
| Measure | Preoperative (Mean ± SD) | Postoperative | P Value | |||
|---|---|---|---|---|---|---|
| 6 Months (Mean ± SD) | 12 Months (Mean ± SD) | Preoperative vs 6 Months | 6 Months vs 12 Months | Preoperative vs 12 Months | ||
| HOOS | 44.4 ± 24.0 | 77.7 ± 7.2 | 91.1 ± 8.0 | <.05 | <.05 | <.05 |
| mHHS | 70.8 ± 6.0 | 86.9 ± 9.3 | 96.9 ± 4.4 | <.05 | <.05 | <.05 |
| OHS | 37.5 ± 5.0 | 40.2 ± 2.1 | 46.5 ± 0.8 | NS | <.05 | <.05 |
| VAS | ||||||
| Pain | 4.3 ± 1.1 | 2.3 ± 1.1 | 0.2 ± 0.4 | <.05 | <.05 | <.05 |
| ADL | 71.6 ± 14.6 | 80 | 98.3 ± 3.7 | <.05 | NS | <.05 |
| SAL | 18.3 ± 26.0 | 71.6 ± 6 | 91.6 ± 8.9 | <.05 | NS | <.05 |
aADL, activities of daily living; HOOS, Hip disability and Osteoarthritis Outcome Score; mHHS, modified Harris Hip Score; NS, not significant; OHS, Oxford Hip Score; SAL, sport activity level; VAS, visual analog scale.
Discussion
Calcification of the rectus femoris tendon is a rare condition, mostly affecting athletes, that can cause hip pain and impairment.12 Other possible causes of hip pain coming from rectus femoris origin include os acetabuli, avulsion fractures, and myositis ossificans.15,26 Generally, a calcific deposit within the tendon of the rectus femoris can be visualized on radiograph as a formation usually parallel to the long axis of the femur (see Figure 1). The exact etiopathogenesis is still unknown. Various hypotheses have been proposed, such as consequence of a previous injury.27 Local stress necrosis6 has been suggested as the first step for the deposition of calcium salts, either directly or through fatty acid and soap intermediaries. A more recent theory proposed the role of local hypoxia as a cause secondary to either mechanical or vascular factors.26 In this series, 2 cases presented the tendon calcification together with a labral tear. A relatively recent paper described a new pathological entity, the hip anterosuperior labral tear with avulsion of rectus femoris (HALTAR).17 This entity combines the labral tear with an injury of the rectus femoris, similarly to what happens in superior labral anterior-posterior (SLAP) lesions of the shoulder. Since the insertion of the rectus femoris tendon is close to the acetabular labrum, a sudden and powerful eccentric contraction of the rectus femoris muscle or a sudden knee flexion may cause an avulsion injury of the rectus femoris as well as a concomitant labral tear.17
Traditional treatment for calcific tendinitis of rectus femoris included oral NSAIDs,16,25 and previously, radiotherapy.19 All the treatment options give the possibility of recovery from symptoms. In refractory cases or when a large bone formation occurs after traumatic injuries (ie, avulsion), a surgical excision of the calcification may be necessary, traditionally performed through an anterior approach.3 The recent improvements in hip arthroscopy give the opportunity to treat this pathology with rapid recovery. In addition, it allows concomitant intra- and extra-articular disorders such us a femoroacetabular impingement to be addressed.
This is the largest published series of rectus femoris tendon calcification in top amateur athletes (soccer players) to date, although other authors have reported on the arthroscopic treatment of this injury.10,24 El-Husseiny et al10 reported 1 case of arthroscopic excision of HC in a chronic rectus femoris origin injury. The patient was pain free and able to return to full training within 8 weeks. Peng et al24 reported on 3 patients (age range, 38-55 years) affected by a calcific tendinitis of the rectus femoris tendon addressed using arthroscopic excision. At 9-month follow-up, all 3 patients were pain free and had recovered full function.
Limitations of the study include the small number of patients and the short follow-up. A longer follow-up would be preferable to assess possible recurrences of HC.
No complications were reported during the follow-up period, and patients needed a short hospitalization (1 night) and immediately started rehabilitation. A recent systematic review of 92 studies and more than 6000 patients reported major and minor complication rates of hip arthroscopy as 0.58% and 7.5%, respectively.13 As a minimally invasive surgery, the main advantages of hip arthroscopy are minimal damage of the soft tissues surrounding the hip area and rapid recovery.11 In addition, it provides the opportunity to address concomitant lesions, such as labral tear, femoroacetabular impingement, and cartilage lesions.2,11
Conclusion
Calcification of the rectus femoris tendon origin is associated with sports involving powerful and repetitive hip movement through full the range of motion. It is usually a self-limiting condition, or it responds well to conservative measures. Surgical excision is necessary in cases of persistent pain. Arthroscopic excision of rectus femoris tendon calcification can be considered a feasible and effective option, with few risks for the patients, rapid recovery, and satisfying outcomes.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Benanti JC, Gramling P, Bulat PI, Chen P, Lundstrom G. Retropharyngeal calcific tendinitis: report of five cases and review of the literature. J Emerg Med. 1986;4:15–24. [DOI] [PubMed] [Google Scholar]
- 2. Bozic KJ, Chan V, Valone FH, 3rd, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28 (8 suppl):140–143. [DOI] [PubMed] [Google Scholar]
- 3. Braun-Moscovici Y, Schapira D, Nahir AM. Calcific tendinitis of the rectus femoris. J Clin Rheumatol. 2006;12:298–300. [DOI] [PubMed] [Google Scholar]
- 4. Byrd JW. Hip arthroscopy utilizing the supine position. Arthroscopy. 1994;10:275–280. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. [DOI] [PubMed] [Google Scholar]
- 6. Carroll RE, Seitz WH, Jr, Putnam MD. Acute calcium deposit in the hand of an 11-year-old girl. J Pediatr Orthop. 1985;5:468–470. [DOI] [PubMed] [Google Scholar]
- 7. Cox D, Paterson FW. Acute calcific tendinitis of peroneus longus. J Bone Joint Surg Br. 1991;73:342. [DOI] [PubMed] [Google Scholar]
- 8. Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 9. Dilley DF, Tonkin MA. Acute calcific tendinitis in the hand and wrist. J Hand Surg Br. 1991;16:215–216. [DOI] [PubMed] [Google Scholar]
- 10. El-Husseiny M, Sukeik M, Haddad FS. Arthroscopic excision of heterotopic calcification in a chronic rectus femoris origin injury: a case report. Ann R Coll Surg Engl. 2012;94 (3):e129–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Enseki KR, Martin RL, Draovitch P, Kelly BT, Philippon MJ, Schenker ML. The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36:516–525. [DOI] [PubMed] [Google Scholar]
- 12. Gamradt SC, Brophy RH, Barnes R, Warren RF, Thomas Byrd JW, Kelly BT. Nonoperative treatment for proximal avulsion of the rectus femoris in professional American football. Am J Sports Med. 2009;37:1370–1374. [DOI] [PubMed] [Google Scholar]
- 13. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. [DOI] [PubMed] [Google Scholar]
- 14. Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644–1653. [DOI] [PubMed] [Google Scholar]
- 15. Hodge JC, Schneider R, Freiberger RH, Magid SK. Calcific tendinitis in the proximal thigh. Arthritis Rheum. 1993;36:1476–1482. [DOI] [PubMed] [Google Scholar]
- 16. Holt PD, Keats TE. Calcific tendinitis: a review of the usual and unusual. Skeletal Radiol. 1993;22:1–9. [DOI] [PubMed] [Google Scholar]
- 17. Hosalkar HS, Pennock AT, Zaps D, Schmitz MR, Bomar JD, Bittersohl B. The hip antero-superior labral tear with avulsion of rectus femoris (HALTAR) lesion: does the SLAP equivalent in the hip exist? Hip Int. 2012;22:391–396. [DOI] [PubMed] [Google Scholar]
- 18. Kim YS, Lee HM, Kim JP. Acute calcific tendinitis of the rectus femoris associated with intraosseous involvement: a case report with serial CT and MRI findings. Eur J Orthop Surg Traumatol. 2013;23 (suppl 2):S233–S239. [DOI] [PubMed] [Google Scholar]
- 19. King JW, Vanderpool DW. Calcific tendonitis of the rectus femoris. Am J Orthop. 1967;9:110–111. [PubMed] [Google Scholar]
- 20. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27:1732–1737. [DOI] [PubMed] [Google Scholar]
- 21. Neviaser RJ. Painful conditions affecting the shoulder. Clin Orthop Relat Res. 1983;(173):63–69. [PubMed] [Google Scholar]
- 22. Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)—validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol. 2006;35:665–672. [DOI] [PubMed] [Google Scholar]
- 24. Peng X, Feng Y, Chen G, Yang L. Arthroscopic treatment of chronically painful calcific tendinitis of the rectus femoris. Eur J Med Res. 2013;18:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pope TL, Jr, Keats TE. Case report 733. Calcific tendinitis of the origin of the medial and lateral heads of the rectus femoris muscle and the anterior iliac spin (AIIS). Skeletal Radiol. 1992;21:271–272. [DOI] [PubMed] [Google Scholar]
- 26. Sarkar JS, Haddad FS, Crean SV, Brooks P. Acute calcific tendinitis of the rectus femoris. J Bone Joint Surg Br. 1996;78:814–816. [PubMed] [Google Scholar]
- 27. Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res. 1976;(118):164–168. [PubMed] [Google Scholar]


