Abstract
Background:
Studies evaluating the benefit of surgical reconstruction of the anterior cruciate ligament (ACL) in middle-aged patients have shown promising results, but study populations were limited primarily to patients who were 40 to 60 years old. Some authors have suggested that surgery may benefit these older patients.
Hypothesis:
Patients aged ≥60 years with functional instability after ACL injury would benefit from ACL reconstruction.
Study Design:
Case series; Level of evidence, 4.
Methods:
Medical records from 1984 through 2010 were searched for patients aged ≥60 years who had undergone primary arthroscopic ACL reconstruction at a single institution. Fifteen patients (15 knees) were identified as meeting the above criteria. All patients were contacted for a telephone interview, and they completed Short Form–36 and modified Cincinnati Knee Score forms. One patient was deceased, and 1 had undergone revision to total knee arthroplasty. Among the remaining 13 patients, the mean age at surgery was 63.5 years (range, 60-73 years), and the mean patient age at the time of follow-up was 73 years (range, 65-85 years). Preoperative radiographs showed no obvious evidence of arthritis in 10 (77%) of the 13 patients; small osteophytes without loss of joint space were seen in 3 (23%) patients. The mean length of follow up was 115.7 months (range, 53-193 months).
Results:
At their last clinic visits, all 13 patients had regained full range of motion and returned to sports or exercise, such as tennis, golf, gym exercise, and yoga. Twelve patients reported no joint laxity.
Conclusion:
Patients aged ≥60 years with symptomatic instability from ACL injury can have good to excellent subjective outcomes with surgical reconstruction.
Clinical Relevance:
Physicians who treat active patients older than 60 years should not exclude ACL reconstruction based on the patient’s age alone.
Keywords: knee, anterior cruciate ligament (ACL), aging athlete, arthroscopic ACL reconstruction
Recent data predict that the population of individuals older than 65 years will increase from 39 million in 2008 to a projected 80 million plus in the year 2050.12 Because many individuals remain physically active into their later years, the age of the sport-injured and ligament-deficient patient has increased. This trend has spawned several studies evaluating the benefit of surgical reconstruction of the anterior cruciate ligament (ACL) in so-called middle-aged or older patients.3,6,8,10,18,19,23 Investigators looked at the procedure in 40- to 60-year-old patients and reported results in patients 50 years and older in a few studies.6,14,19 These studies have shown promising results. Although some authors have suggested that surgery be withheld from older patients because of concerns of a higher rate of arthrofibrosis and decreased range of motion, no clinical studies have supported that hypothesis.7,10,15,17,22
In our review of the literature on ACL reconstruction in older patients, we did not find any studies of long-term outcomes of ACL reconstruction in patients older than 60 years. We hypothesized that these patients could benefit from the procedure. Our purpose was to determine outcomes after primary ACL reconstruction in our small series of patients 60 years and older.
Materials and Methods
Patient Selection
We searched medical records for patients aged 60 years and older who had undergone primary arthroscopic reconstruction of the ACL at our institution from 1984 through 2010 and who had at least 2 years of follow-up. Fifteen patients (15 knees) met the above criteria, and their charts were reviewed (Table 1). All patients had active lifestyles that included activities such as tennis, skiing, or running. At the time of our review, 1 patient was deceased and 1 had undergone revision to total knee arthroplasty, leaving 13 patients available for follow-up. All 13 (100%) patients were contacted and interviewed by telephone.
TABLE 1.
Patient Data
| Patient | Age, y | Sex | Mechanism of Injury | Surgical Indication | Injury to Surgery, mo | Length of Follow-up, y | Cincinnati Knee Score |
|---|---|---|---|---|---|---|---|
| 1 | 60 | Female | Fall | Instability | 0.27 | 8.81 | 86 |
| 2 | 62 | Female | Ice skating | Instability | 21.87 | 11.3 | 89 |
| 3 | 60 | Male | Four-wheeler injury | Weakness, decreased motion | 1.3 | 5.47 | 90 |
| 4 | 61 | Male | Unknown | Instability, pain | Unknown | 8.84 | 77 |
| 5 | 61 | Female | Skiing | Instability | 3.23 | 4.88 | 88 |
| 6 | 60 | Female | Fall | Instability | 4.73 | 12.53 | 90 |
| 7 | 60 | Male | Fall | Instability | 0.77 | 5.13 | 91 |
| 8a | 73 | Female | Fall | Instability | 11.9 | 4.35 | 72 |
| 9 | 63 | Female | Twist injury | Instability | 1.57 | 10.55 | 71 |
| 10 | 68 | Female | Twist injury | Instability | Unknown | 15.84 | 46 |
| 11 | 66 | Male | Twist injury | Instability | 3.87 | 14.87 | 59 |
| 12 | 67 | Female | Unknown | Instability | Unknown | 11.48 | 73 |
| 13 | 60 | Female | Twist injury | Instability, pain | 10.53 | 9.59 | 83 |
| 14b | 66 | Female | Unknown | Pain | 3.4 | NA | NA |
| 15c | 65 | Female | Skiing | Instability | Unknown | NA | NA |
aAfter a fall, patient had a revision anterior cruciate ligament reconstruction that was successful.
bPatient had a total knee arthroplasty.
cPatient deceased.
The mean age of patients at the time of surgery was 63.5 years (range, 60-73 years). Eight (62%) patients were women. The main indication for surgical reconstruction was instability in 12 (92%) of 13 patients and weakness with loss of motion in the remaining patient (Table 1). Preoperative radiographs showed no obvious evidence of arthritis in 10 (77%) patients; small osteophytes without loss of joint space were seen in 3 (23%) patients. Three patients had an acute injury (surgery within 6 weeks of injury); the remaining patients had chronic injuries. Those with chronic injuries had recalcitrant symptoms after nonoperative treatment with rehabilitation and bracing for 1 to 6 months.
Surgical Procedure
Each patient had a single-incision arthroscopic ACL reconstruction procedure, as described by Arciero et al.1 Graft choices were as follows: 4 bone–patellar tendon–bone autografts, 6 hamstring autografts, and 3 tibialis tendon or Achilles tendon allografts. In addition to the ACL reconstruction, 6 patients had a partial medial meniscectomy, 2 had a partial lateral meniscectomy, 2 had a medial meniscectomy, 1 had a lateral meniscectomy, 1 had a medial and lateral meniscectomy, 4 had chondroplasty, and 1 had a repair of the medial collateral ligament. In the postoperative notes for these patients, some procedures were simply listed as “meniscectomy,” without qualifying them as partial or total, however it can be assumed they were partial because we only perform a partial meniscectomy or ACL reconstruction. Postoperative rehabilitation programs were standardized among patients. The protocol began with protected partial weightbearing and focused on early range of motion and quadriceps function.
When dismissed from rehabilitation, 12 of 13 knees were reported to be stable, with full range of motion. The remaining patient had an initial flexion contracture that improved over time, and her last documented note reported full motion.
Evaluation
All patients were contacted for a phone interview, and they completed the modified Cincinnati Knee Score forms and the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36). The mean patient age at follow-up was 73 years (range, 65-85 years). Mean length of follow-up was 116 months (range, 53-193 months).
The SF-36 is a questionnaire that is designed for self-administration. It measures overall health by 8 parameters to provide scores for a person’s functional status, well-being, and overall evaluation of health.9,26 These scores can be compared with those of the total population by predetermined averages and can be broken down by age range and sex for more specific comparisons.
The modified Cincinnati Knee Score is the subjective portion of the Cincinnati Knee Rating System.2,21 On a 0- to 100-point scale (<30, poor; 30-54, fair; 55-79, good; >80, excellent), it calculates a score using questions regarding a patient’s symptoms and functional variables. This system is a commonly used tool to measure outcomes of knee ligament reconstruction.
Results
All patient responses from the SF-36 form were scored, and individual totals for each of the 8 parameters were averaged. The group averages for each parameter are shown in Figure 1. The averaged scores exceeded the population averages in each scale. When evaluated on an individual basis, each patient had 8 calculated outcomes, and for 13 patients, that equaled 104 total outcomes. When each score was compared with age- and sex-matched means, our population had 88 outcomes (85%) that were greater than or equal to their age- and sex-matched means and 16 (15%) that were less than their age- and sex-matched means.
Figure 1.
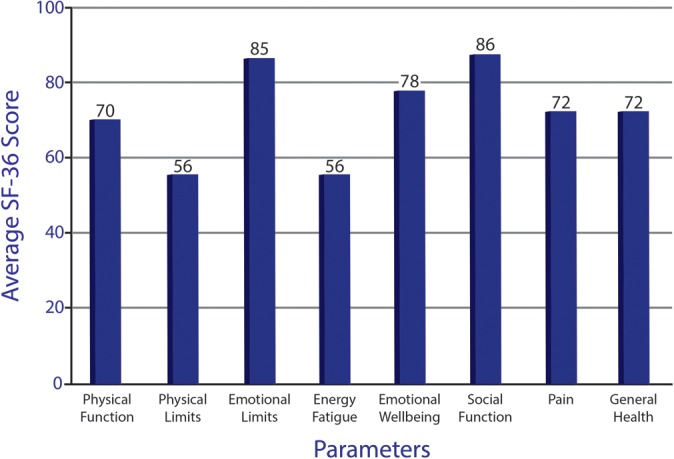
The 36-Item Short Form Health Survey (SF-36) includes 1 multi-item scale that assesses 8 health concepts: (1) physical functioning, (2) role limitations due to physical health, (3) role limitations due to emotional problems, (4) energy/fatigue, (5) emotional well-being, (6) social functioning, (7) pain, and (8) general health. All patient responses from the SF-36 form were scored, and individual totals for each of the 8 parameters were averaged. The group averages for each parameter are shown.
Modified Cincinnati Knee Scores calculated for each individual resulted in 7 excellent, 5 good, and 1 fair result (Table 1).
All patients reported that they were happy with their surgeries and, given the same injury, all would choose to have the surgery again.
Complications
One patient developed a superficial wound infection over the distal portion of his autograft site 2 weeks after surgery. It was successfully treated with superficial irrigation and debridement and oral antibiotics. He did not require any further intra-articular procedures. One patient treated with allograft fell on the operated knee 6 months after the index procedure. She was noted to have increased laxity after the fall that did not improve with therapy and time. She underwent a revision reconstruction with allograft 14 months after the index procedure and has done well since.
Discussion
Surgical reconstruction of the ACL-deficient knee, regardless of the patient’s age, has been solidly endorsed in the scientific and clinical literature,4,5,11,13,18,20,24,25 although some authors advocate conservative treatment.7,10,16,17,22 In a 2003 prospective study, Blyth et al6 followed 30 patients who had undergone ACL reconstruction at greater than 50 years of age. Their preoperative Lysholm scores increased from 63 (range, 32-95) to 93 (range, 76-100) postoperatively, and Cincinnati scores improved from 49 (range, 18-73) to 89 (range, 73-100). International Knee Documentation Committee scores all improved by at least 1 grade.
The patient population in our study was similar to those in previous studies measuring outcomes of ACL reconstruction with respect to mechanism of injury, time to surgery, reason for surgery, and concomitant injuries. The patient satisfaction rate of 100% matched or surpassed that previously reported.6,8,23
The Cincinnati Knee Scores in our patients indicated all but 1 patient in our series had good or excellent results. The patient who had the fair result was our oldest patient and was 83.8 years old at the time of follow-up. She was also assessed at 15.8 years of follow-up, and she attributed her results more to her age and the multiple falls she had sustained in the previous 2 to 3 years.
Any of the lesser or negative responses given on the SF-36 questionnaire were attributed by the patients to other comorbidities or even to age itself. Several of the patients studied stated they had chronic back pain or other medical issues that affected their scores. No patient attributed any low score or answer to their operative knee. Average SF-36 scores for our patients were greater than those of the general population; however, this fact should not be misconstrued. We do not believe that having an ACL reconstruction will improve a person’s overall functionality over that of the rest of the population, injured or uninjured. It is most likely that our population’s scores are higher because of their active lifestyle and motivation to maintain such a lifestyle, thus making them appropriate candidates for surgery in the first place.
Only 1 patient (6%) suffered reinjury that required revision surgery. Blyth et al6 reported 1 (3%) reinjury in 30 patients without any mention of revision surgery. Plancher et al23 reported a 7% reinjury rate in their population of ACL reconstruction in 40- to 60-year-old patients.
Our study does have limitations. First, the patient population is very small. Second, there was no control group of age-matched patients undergoing nonoperative treatment for ACL deficiency. However, given the reasons that our patient population chose surgery, there would be an inherent selection bias, including age-matched patients choosing not to undergo surgery. Another potential weakness of the study is the lack of recent objective patient data, such as physical examination findings and radiographs. However, for this population, we believe the most important outcomes were a patient’s perceived knee performance, satisfaction, and daily functioning. Coupled with the modified Cincinnati Knee Scores, this information gives us a good representation of outcome success.
Conclusion
Our results suggest that individuals 60 years and older who have symptomatic instability from an absent or insufficient ACL can have good to excellent subjective outcomes with surgical reconstruction. We believe that patients of any age who are active and desire to maintain their level of activity can be successfully treated with ACL reconstruction if there are no contraindications.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Arciero RA, Scoville CR, Snyder RJ, Uhorchak JM, Taylor DC, Huggard DJ. Single- versus two-incision arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1996;12:462–469. [DOI] [PubMed] [Google Scholar]
- 2. Barber-Westin SD, Noyes FR, McCloskey JW. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament-reconstructed knees. Am J Sports Med. 1999;27:402–416. [DOI] [PubMed] [Google Scholar]
- 3. Barrett G, Stokes D, White M. Anterior cruciate ligament reconstruction in patients older than 40 years. Am J Sports Med. 2005;33:1505–1512. [DOI] [PubMed] [Google Scholar]
- 4. Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols NE. Treatment of anterior cruciate ligament injuries. Part I. Am J Sports Med. 2005;33:1579–1602. [DOI] [PubMed] [Google Scholar]
- 5. Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols NE. Treatment of anterior cruciate ligament injuries. Part II. Am J Sports Med. 2005;33:1751–1767. [DOI] [PubMed] [Google Scholar]
- 6. Blyth MJ, Gosal HS, Peake WM, Bartlett RJ. Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2-8 year follow-up. Knee Surg Sports Traumatol Arthrosc. 2003;11:204–211. [DOI] [PubMed] [Google Scholar]
- 7. Bonamo JJ, Fay C, Fierstone T. The conservative treatment of the anterior cruciate deficient knee. Am J Sports Med. 1990;18:618–623. [DOI] [PubMed] [Google Scholar]
- 8. Brandsson S, Kartus J, Larsson J, Eriksson BI, Karlsson J. A comparison of results in middle-aged and young patients after anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:178–182. [DOI] [PubMed] [Google Scholar]
- 9. Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients: results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315–1321. [DOI] [PubMed] [Google Scholar]
- 11. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of ACL injured patient: a prospective outcome study. Am J Sports Med. 1994;22:632–644. [DOI] [PubMed] [Google Scholar]
- 12. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: key indicators of well-being. http://www.agingstats.gov/Main_Site/Data/2012_Documents/docs/EntireChartbook.pdf. Accessed June 6. 2012.
- 13. Ferrari JD, Bach BR., Jr Isolated anterior cruciate ligament injury, In: Chapman MW, ed. Chapman’s Orthopaedic Surgery. 3rd ed Philadelphia, PA: Lippincott Williams & Wilkins; 2001:2347–2359. [Google Scholar]
- 14. Gee AO, Kinsella S, Huffman GR, Sennett BJ, Tjoumakaris FP. Anterior ligament reconstruction in patients >40 years: a case-control study. Phys Sportsmed. 2013;41:30–34. [DOI] [PubMed] [Google Scholar]
- 15. Goel MK, Khanna P, Kishore J. Understanding survival analysis: Kaplan-Meier estimate. Int J Ayurveda Res. 2010;1:274–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hawkins RJ, Misamore GW, Merritt TR. Follow-up of the acute non-operative isolated anterior cruciate ligament tear. Am J Sports Med. 1986;14:205–210. [DOI] [PubMed] [Google Scholar]
- 17. Kannus P, Jarvinen M. Conservatively treated tears of the anterior cruciate ligament: long-term results. J Bone Joint Surg Am. 1987;69:1007–1012. [PubMed] [Google Scholar]
- 18. Kuechle DK, Pearson SE, Beach WR, et al. Allograft anterior cruciate ligament reconstruction in patients over 40 years of age. Arthroscopy. 2002;18:845–853. [DOI] [PubMed] [Google Scholar]
- 19. Miller MD, Sullivan RT. Anterior cruciate ligament reconstruction in an 84-year-old man. Arthroscopy. 2001;17:70–72. [DOI] [PubMed] [Google Scholar]
- 20. Muneta T, Sekiya I, Yagashita K, Ogiuchi T, Yamanoto H, Shinomiya K. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy. 1999;15:618–624. [DOI] [PubMed] [Google Scholar]
- 21. Noyes FR, McGinniss GH, Mooar LA. Functional disability in the anterior cruciate insufficient knee syndrome: review of knee rating systems and projected risk factors in determining treatment. Sports Med. 1984;1:278–302. [DOI] [PubMed] [Google Scholar]
- 22. Noyes FR, Mooar PA, Mathews DS, Butler DL. The symptomatic anterior cruciate-deficient knee. Part I: the long-term functional disability in athletically active individuals. J Bone Joint Surg Am. 1983;65:154–162. [DOI] [PubMed] [Google Scholar]
- 23. Plancher KD, Steadman JR, Briggs KK, Hutton KS. Reconstruction of the anterior cruciate ligament in patients who are at least forty years old. A long-term follow-up and outcome study. J Bone Joint Surg Am. 1998;80:184–197. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Stube KC. Anterior cruciate ligament (ACL)-deficient knee with degenerative arthrosis: treatment with an isolated autogenous patellar tendon ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 1997;5:150–156. [DOI] [PubMed] [Google Scholar]
- 25. Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ware JE, Jr, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]


