Abstract
Background:
Little knowledge exists on postoperative recovery of pain and shoulder function following arthroscopic removal of calcific deposits of the supraspinatus tendon (ACDSSP). Certain factors may influence outcome, including acromial morphology.
Purpose:
To examine postoperative recovery following ACDSSP without acromioplasty and to analyze influential outcome factors.
Study Design:
Case series; Level of evidence, 4.
Methods:
This prospective study evaluated 82 patients (105 shoulders) after ACDSSP without acromioplasty. Time periods for postoperative recovery of pain and subjective shoulder function were recorded. The absolute and normalized Constant scores (CSabs and CSnorm, respectively), Oxford Shoulder Score (OSS), DASH score (DS), and subjective shoulder value (SSV) were measured after a mean follow-up of 33.9 months. Analyzed outcome factors included localization of the calcific deposit (CD), acromial morphology, radiographic extent of CD removal, type of nonoperative treatment, and preoperative duration of symptoms.
Results:
Mean duration of postoperative pain was 2.2 weeks. Recovery of subjective shoulder function required 11.1 weeks on average. Mean ± standard deviation follow-up values were 91.1 ± 8.3 for CSabs, 104.2% ± 8.2% for CSnorm, 13.1 ± 2.6 for OSS, 1.81 ± 4.59 for DS, and 93.8% ± 10.7% for SSV. Abduction was significantly (P = .008) lower in patients with type III (170° ± 17.5°) compared with type I (174° ± 20.7°) and type II (179° ± 4.5°) acromions. Also, abduction was significantly (P = .001) lower in patients with long-standing symptoms (>72 months). Minor calcific remnants were found in 19 of 105 shoulders (18.1%), but affected neither postoperative recovery nor outcome.
Conclusion:
ACDSSP without acromioplasty yielded favorable outcomes and effected fast remission of pain regardless of acromial morphology. However, recovery of subjective shoulder function required almost 3 months on average. Minimal restriction of abduction occurred in patients with hook-shaped acromions and long-standing preoperative symptoms. The present data do not support routine performance of acromioplasty.
Keywords: calcific tendinitis, shoulder arthroscopy, acromioplasty, postoperative recovery, outcome factors
Calcific tendinitis of the shoulder (CTS) is regarded as a self-limiting condition following a pathogenetic cycle of precalcification (formation), calcification, and resorption.31,32 However, different stages and chronologies may coexist within a single calcific deposit (CD).28 Nonoperative treatment includes oral nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, ultrasound therapy, extracorporeal shock wave therapy (ESWT), subacromial corticoid injections, ultrasound-guided needling/barbotage, and many others.9,10,12,27,33 Surgery is indicated in chronic symptomatic cases unresponsive to nonoperative management. Previously, radiological prognostic factors for therapy-refractory courses of disease could be identified.24
Arthroscopy usually represents the surgical treatment of choice because of faster postoperative recovery and less invasiveness compared with open surgery.∥ However, methods of arthroscopic treatment differ substantially with regard to the technique and extent of CD removal as well as the performance of concomitant procedures, such as acromioplasty and/or coracoacromial ligament resection.13,16,20,26,30,34 Even though mid- and long-term clinical results can be expected to be good to excellent, there exists little knowledge on short-term postoperative evolution of remission of pain and recovery of shoulder function.20,28 Furthermore, it is largely unknown which factors influence postoperative recovery and outcome following arthroscopic treatment of CTS.
Therefore, this study focused on 2 main research questions. First, it examined evolution of postoperative remission of pain and recovery of subjective shoulder function following arthroscopic removal of calcific deposits of the supraspinatus tendon (ACDSSP). Concomitant procedures such as acromioplasty or coracoacromial ligament resection were not performed in any case. Second, it analyzed factors with potential influence on postoperative recovery and outcome (CD localization, acromial morphology, radiographic extent of CD removal, type of nonoperative treatment, and preoperative duration of symptoms).
Methods
This prospective study included a total of 90 patients (n = 115 shoulders) undergoing ACDSSP. Patients asked for surgical intervention because of refractory complaints after a minimum of 6 months of nonoperative management. All patients suffered from pain at rest and showed clinical signs of impingement. The mean period of preoperative nonoperative therapy was 41.3 months (range, 6-164 months). Nonoperative treatment consisted of oral analgesics (n = 67), supervised physical therapy (n = 44), up to 3 subacromial injections of low-dose corticosteroids (n = 52), and up to 2 sessions of high-energy ESWT (n = 37). Patients with concomitant shoulder pathologies, acute CD perforations, multifocal CTS, and prior or subsequent surgery of the affected shoulder were excluded from the study. Institutional review board approval for this study was obtained from the local ethics committee. All patients provided written informed consent prior to study inclusion.
Operative Technique
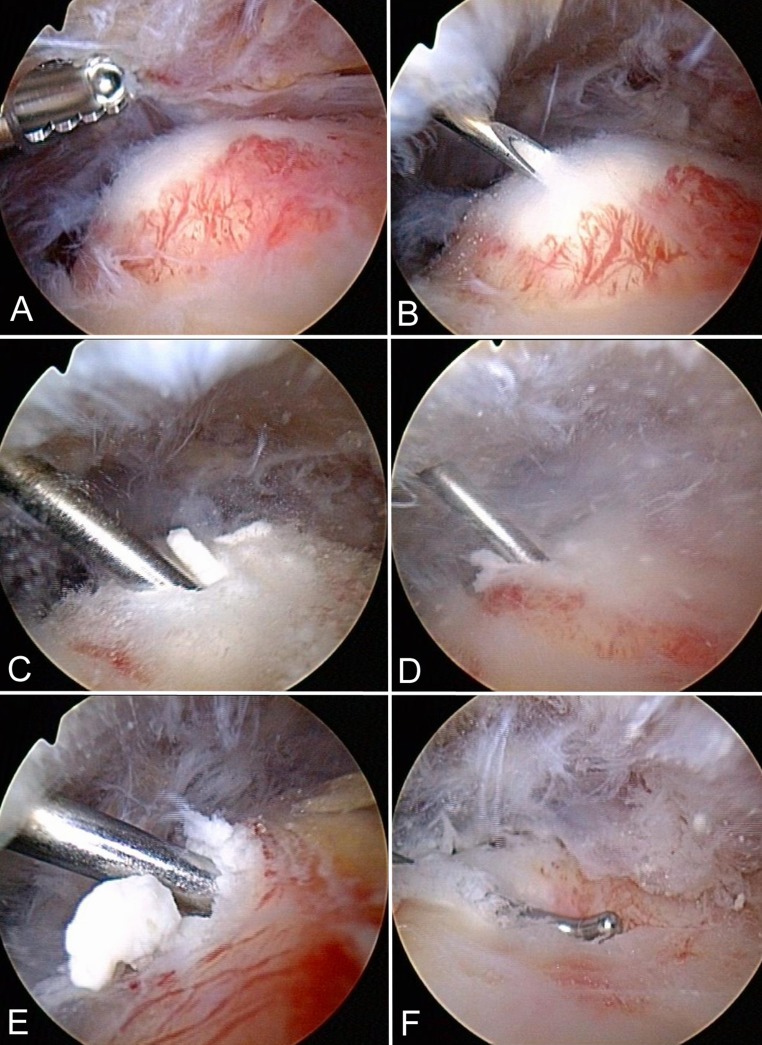
All surgeries were performed by the same surgeon (senior author, P.O.). Patients received general anesthesia and were positioned in lateral decubitus. A diagnostic glenohumeral arthroscopy was performed to exclude relevant intra-articular pathologies. The arthroscope was placed into the subacromial space, and a lateral portal was established within the affected quadrant. All CDs could be reliably detected by means of the quadrant technique.23 A shaver was used to perform partial bursectomy within the suspected area. The tendon was sparsely needled until the deposit was localized. Another needle was used to approximate the center of the CD. A blunt hook probe was inserted into the center of the CD without performing a tendon incision. The hook probe was used as a “stir” to eliminate the carbonate apatite out of the deposit. The CD was “squeezed out” by applying blunt pressure with the probe (Figure 1). This blunt technique (“squeeze and stir”) of CD removal preserved integrity of the supraspinatus tendon and avoided necessity of rotator cuff repair. No concomitant procedures, such as subacromial decompression or coracoacromial ligament resection, were performed in any case.
Figure 1.
Operative technique. (A) Partial subacromial bursectomy is performed in the suspected region of calcific deposit (CD) localization (left shoulder). The CD appears as a bump as a result of swelling of the affected supraspinatus tendon. (B) A needle is used to locate the center of the deposit. (C) A blunt hook probe is inserted into the center of the deposit without incising the tendon. (D) “Squeezing” and (E) “stirring” with the hook probe effectuates blunt elimination of carbonate apatite. (F) After CD removal, an indentation is noted at the site of the former bump.
Rehabilitation Protocol
Postoperative rehabilitation followed a standardized protocol under supervision of a physical therapist. The sling was removed on the first postoperative day. There were no restrictions of active range of motion. Particular focus was put on stretching of the posterior capsule, which was shortened frequently. However, patients were encouraged to refrain from excessive load exercises for about 6 postoperative weeks to promote tendon remodeling. Oral analgesics were taken only as needed. From week 7, patients intensified isometric and isokinetic training of the rotator cuff.
Radiological Evaluation
A single orthopaedic surgeon (P.O.) performed standardized preoperative sonography for determination of CD localization within the supraspinatus tendon according to the quadrant technique.23 The quadrant technique divides the acromion from anterior to posterior into 4 equal quadrants (1-4). True anterior-posterior and outlet radiographs were obtained preoperatively, postoperatively, and at follow-up. One experienced orthopaedic resident analyzed all outlet views and classified acromial morphologies according to Bigliani et al5 (type I = flat, type II = curved, and type III = hooked). In addition, postoperative radiographs were evaluated with regard to the accomplished extent of CD removal.
Outcome Measures
Postoperative Recovery
Postoperatively, we recorded time periods (weeks) required for full remission of pain and recovery of subjective shoulder function. In this context, we calculated the proportions of patients having achieved full recovery.
Shoulder Scores
One independent investigator (experienced orthopaedic resident) examined both shoulder joints after a minimum follow-up period of 24 months. The absolute and normalized Constant scores (CSabs and CSnorm), Oxford Shoulder Score (OSS), DASH score (DS), and subjective shoulder value (SSV) served as functional outcome measures.8,14,17 The adjusted CSnorm, as described by Katolik et al,17 represents the sex- and age-matched function of the shoulder.
Outcome Factors
Outcome factors analyzed included CD localization within the supraspinatus tendon (quadrants 1-4), acromial morphology (types I-III), radiographic extent of CD removal, type of nonoperative treatment (preoperative ESWT or subacromial corticoid injection), and preoperative duration of symptoms (group 1, 0-24 months; group 2, 25-48 months; group 3, 49-72 months; group 4, 73-96 months; group 5, 97-120 months). Statistical analysis evaluated whether stated outcome factors significantly influenced postoperative recovery (remission of pain, recovery subjective shoulder function) and outcome.
Statistical Analysis
The software SPSS version 17 (SPSS Inc, Chicago, Illinois, USA) was used for statistical analysis. Unless stated otherwise, results are given as mean values including their standard deviations (SDs). All data were tested for normal distribution using the Kolmogorov-Smirnov test. Analysis of variance or nonparametric tests (Mann-Whitney U or Kruskal-Wallis test) were used to compare group data. Kaplan-Meier plots displayed postoperative remission of pain and recovery of subjective shoulder function. The level of significance was set at α = .05. P values <.05 indicated statistical significance. Calculations relied on 95% confidence intervals.
Results
Follow-up examinations were completed in 82 (51 females, 31 males) patients, corresponding to a follow-up rate of 91%. Fourteen female and 9 male patients underwent bilateral surgery. Thus, a total of 105 shoulders were reviewed. Eight patients dropped out because of one of the following reasons: address unknown (n = 4), refusal of study participation (n = 3), or death (n = 1). The mean age was 50.0 years (range, 32-68 years) at the time of surgery. The mean follow-up period was 33.9 months (range, 24-108 months).
Radiological Findings
Sonographically, 64 of 105 (61.0%) CDs were localized in quadrant 1 (most anterior portion of the supraspinatus tendon), 19 (18.1%) in quadrant 2 (anterior middle portion of the supraspinatus tendon), 14 (13.3%) in quadrant 3 (posterior middle portion of the supraspinatus tendon), and 8 (7.6%) in quadrant 4 (most posterior portion of the supraspinatus tendon) of the acromion. Radiographically, type I (flat) acromions were found in 32 of 105 (30.5%) shoulders, type II (curved) acromions in 57 (54.3%), and type III (hooked) acromions in 16 (15.2%). Age between acromion type patient groups did not differ (P = .651). Complete radiographic CD elimination was achieved in 86 of 105 (81.9%) shoulders. Minor calcific remnants (CRs) were found in 19 of 105 (18.1%) cases, presenting as radiolucent residues of the former CDs. CRs did not appear more frequently in patients with previous ESWT (n = 31) compared with patients without previous ESWT (n = 74) (82.4% vs 80.6%; P = .829).
Operative Findings
Mean operative time was 41 minutes (SD, 11.2 minutes; range, 11-75 minutes). All CDs were detected by means of the quadrant technique without use of intraoperative radiography.23 Sonographically, 11 of 105 (10.5%) CDs were located adjacent to the long head of the biceps tendon. Mild to moderate inflammation (tenosynovitis) of the anterior aspects of the tendon was found in these cases. No calcification primarily originated from the long head of the biceps tendon. Focal subacromial bursitis and swelling of the affected supraspinatus tendon were found in all cases.
Postoperative Recovery
Remission of Pain
Postoperatively, pain fully subsided in 103 of 105 (98.1%) shoulders. Overall, the average period of postoperative pain was 2.24 weeks (SD, 2.23 weeks; range, 0-16 weeks). None of the analyzed outcome factors significantly influenced postoperative remission of pain. Table 1 displays the chronology of postoperative evolution of pain, indicating time periods as well as related numbers and proportions of patients having achieved complete remission of pain. We performed Kaplan-Meier (survival) analysis based on the event “remission of pain.” Figure 2 shows the linear interpolation curve for the 103 cases with full remission of pain.
TABLE 1.
Chronology of Remission of Pain
| Interval, wk | No. of Cases per Interval | Cumulative No. of Cases | Proportional Percentagea | Cumulative Percentagea |
|---|---|---|---|---|
| 0.0-1.0 | 38 | 38 | 36.2 | 36.2 |
| 1.0-2.0 | 30 | 68 | 28.6 | 64.8 |
| 2.0-3.0 | 20 | 88 | 19.0 | 83.8 |
| 3.0-4.0 | 4 | 92 | 3.8 | 87.6 |
| 4.0-5.0 | 2 | 94 | 1.9 | 89.5 |
| 5.0-6.0 | 2 | 96 | 1.9 | 91.4 |
| 6.0-7.0 | 4 | 100 | 3.8 | 95.2 |
| 7.0-8.0 | 2 | 102 | 1.9 | 97.1 |
| 8.0-16.0 | 1 | 103 | 1.0 | 98.1 |
| Pain at follow-up | 2 | 105 | 1.9 | 100.0 |
aValues were rounded to 1 decimal point.
Figure 2.
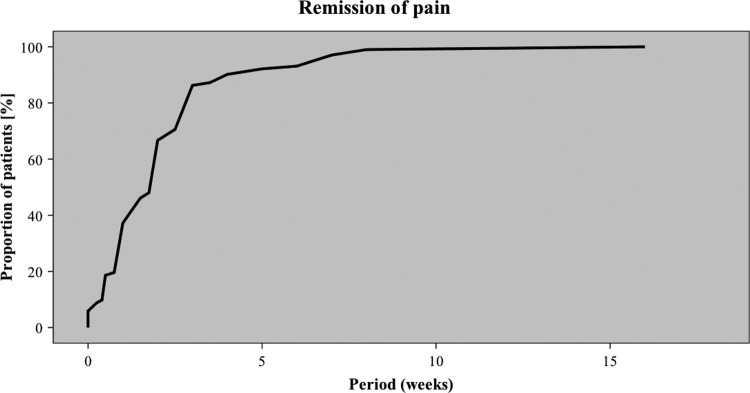
Complete remission of pain occurred in 103 of 105 (98.1%) cases. The linear interpolation curve illustrates the chronology of remission of pain.
Subjective Shoulder Function
Postoperatively, 93 of 105 (88.6%) cases regained full subjective shoulder function. Overall, the average period required for recovery of subjective shoulder function was 11.1 weeks (SD, 9.8 weeks; range, 2-54 weeks). None of the analyzed outcome factors significantly influenced subjective functional recovery. Table 2 displays the chronology of recovery of subjective shoulder function, indicating time periods as well as related numbers and proportions of patients having regained full subjective shoulder function. We performed Kaplan-Meier (survival) analysis based on the event “recovery of subjective shoulder function.” Figure 3 shows the linear interpolation curve for the 93 cases with full recovery of subjective shoulder function. The 12 patients who did not achieve full functional recovery did not have significantly longer preoperative symptomatic courses on average (33.8 vs 36.0 months; P = .578).
TABLE 2.
Chronology of Recovery of Subjective Shoulder Function
| Interval, wk | No. of Cases per Interval | Cumulative No. of Cases | Proportional Percentagea | Cumulative Percentagea |
|---|---|---|---|---|
| 0.0-1.0 | 0 | 0 | 0.0 | 0.0 |
| 1.0-2.0 | 3 | 3 | 2.9 | 2.9 |
| 2.0-3.0 | 3 | 6 | 2.9 | 5.8 |
| 3.0-4.0 | 7 | 13 | 6.7 | 12.5 |
| 4.0-5.0 | 4 | 17 | 3.8 | 16.3 |
| 5.0-6.0 | 12 | 29 | 11.4 | 27.7 |
| 6.0-7.0 | 16 | 45 | 15.2 | 42.9 |
| 7.0-8.0 | 10 | 55 | 9.5 | 52.4 |
| 8.0-12.0 | 20 | 75 | 19.0 | 71.4 |
| 12.0-16.0 | 5 | 80 | 4.7 | 76.1 |
| 16.0-20.0 | 3 | 83 | 2.9 | 79.0 |
| 20.0-24.0 | 3 | 86 | 2.9 | 81.9 |
| 24.0-34.0 | 3 | 89 | 2.9 | 84.8 |
| 34.0-44.0 | 2 | 91 | 1.9 | 86.7 |
| 44.0-54.0 | 2 | 93 | 1.9 | 88.6 |
| Restricted subjective shoulder function at follow-up | 12 | 105 | 11.4 | 100.0 |
aValues were rounded to 1 decimal point.
Figure 3.

Full recovery of subjective function occurred in 93 of 105 (88.6%) shoulders. The linear interpolation curve illustrates the chronology of recovery of subjective shoulder function.
Outcome Analysis
Ninety-three (88.6%) patients presented without relevant functional restrictions at follow-up. A distinct limitation of at least 1 range of motion (<8 points in CS) was found in 12 patients. Internal rotation was found to be restricted in all cases. Two of these 12 patients still complained about shoulder pain being present at a lower level than preoperatively.
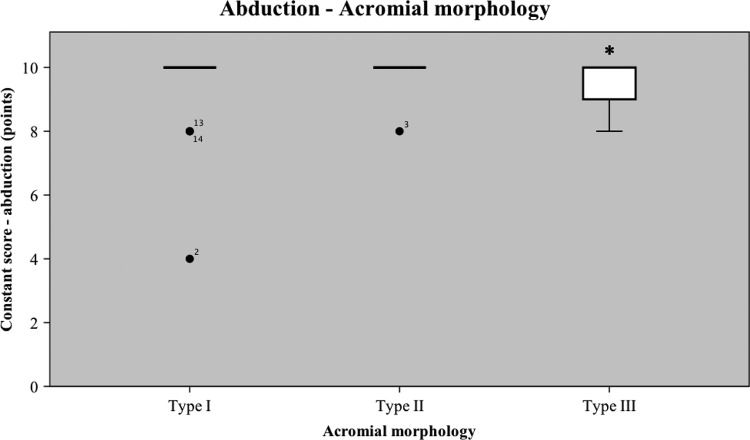
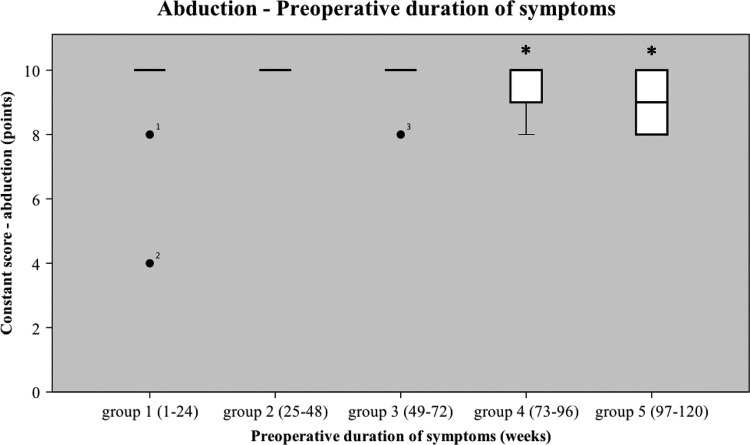
Mean follow-up values were 91.1 points (±8.3) for CSabs and 104.2% (±8.2%) for CSnorm. Analysis of outcome factors did not show significant differences for total scores of CSabs and CSnorm. However, abduction was significantly (P = .008) lower in patients with type III (9.43 ± 1.0 points, 169.7° ± 17.5°) compared with type I (9.69 ± 1.2 points, 174.4° ± 20.7°) and type II (9.97 ± 0.3 points, 179.5° ± 4.5°) acromions (Figure 4). Also, abduction was significantly (P = .001) lower in patients who had suffered from long-standing preoperative symptoms (>72 months; groups 4 and 5). Mean abduction was 9.84 ± 0.9 points (177.1° ± 16.0°) in group 1, 10.00 ± 0.0 points (180.0° ± 0.0°) in group 2, 9.85 ± 0.56 points (177.3° ± 10.1°) in group 3, 9.50 ± 1.00 points (171.0° ± 18.0°) in group 4, and 9.00 ± 1.16 points (162.0° ± 20.9°) in group 5 (Figure 5).
Figure 4.
Outcome analysis related to acromial morphology shows significantly (P = .008) lower abduction in patients with type III acromions. *Statistical significance; black dots with case numbers are outliers.
Figure 5.
Outcome analysis related to acromial morphology shows significantly (P = .001) lower abduction in patients with long-standing preoperative symptoms (groups 4 and 5). *Statistical significance; black dots with case numbers are outliers.
Further mean follow-up values were 13.1 points (±2.6) for OSS, 1.81 points (±4.6) for DS, and 93.8% (±10.7%) for SSV. Analysis of outcome factors did not show significant differences for the OSS, DS, and SSV.
Complications
There were no surgical complications. Postoperative stiffness appeared in 3 of 105 (2.9%) shoulders. Of these, 1 patient presented with a notably restricted range of motion at follow-up.
Discussion
Only very few studies evaluated the chronology of postoperative recovery following arthroscopic treatment of CTS.21,28 Molé et al21 reported an average period of recovery of 4 to 6 months. Seil et al28 noted a rather irregular evolution of postoperative pain. Eighteen of 58 (31%) patients were free of pain or had reached their minimum pain level after 3 months, 48% after 6 months, 68% after 9 months, and 96% after 12 months. Postoperative recovery lasted for several months in the majority of patients. The authors assumed that prolongation of recovery might have been caused by remodeling and healing processes within the tendon and subacromial bursa. In our series, 71% of patients recovered within a period of 3 months, 82% within 6 months, and almost 90% within 13.5 months. Patients were free of pain after 2.2 weeks on average and recovered shoulder function within a mean period of almost 3 months. Thus, we observed faster postoperative recovery compared with other studies.1,15,21,28,34 This finding could be well explained by use of the tendon-preserving technique of blunt arthroscopic CD removal (squeeze-and-stir).20 Other techniques involve incision and/or debridement of the affected rotator cuff tendon with or without subsequent repair.¶ This additional surgical impact possibly impairs tendon remodeling and healing.
Interestingly, none of the analyzed factors exerted significant influence on evolution of postoperative recovery. Neither CD localization within the most anterior portion of the supraspinatus tendon (quadrant 1) nor hook-shaped (type III) acromial morphology delayed postoperative recovery. Thus, pain and functional restrictions seem to be directly related to the pathologic changes inside (CD) and around (bursitis) the affected tendon. These results indicate that additional acromioplasty in ACDSSP does not seem to be advantageous. In a previous study,20 postoperative continuance of minor CRs did not impair clinical mid- and long-term outcomes and showed spontaneous resolution. In addition, this study demonstrated that minor postoperative CRs did not delay short-term remission of pain and recovery of shoulder function. These findings support our recommendation not to aim for full CD removal at the expense of tendon defects. On the other hand, focal bursitis should be removed, as it most likely represents a principal correlate of pain in CTS. Corticoids are known to negatively affect metabolism and mechanical properties of rotator cuff tendons.29 Thus, we examined the possible influence of previous subacromial corticoid injection on outcome following ACDSSP. We did not observe a significant impact of up to 3 subacromial injections on postoperative recovery or outcome. However, cortisone was not injected directly into the deposit, and only rather low dosages of maximum 10 mg triamcinolone were used. Related to preoperative ESWT treatment, this study confirmed the findings of Lorbach et al,19 which showed no significant impact on postoperative mid- and long-term outcomes. In addition, we found, that previous ESWT affected neither short-term postoperative recovery nor the extent of CD removal. Furthermore, postoperative recovery was not related to preoperative duration of symptoms. However, analysis of postoperative recovery only included the 93 patients who had fully recovered. Outcome analysis of all patients showed significantly lower abduction in cases with long-standing preoperative symptoms (>72 months). Abduction was restricted by 9° (group 4) and 18° (group 5). A proportion of 11.4% of patients showed limitation of internal rotation and abduction as the most common functional deficits at follow-up. This finding was most likely attributed to remaining pathological capsular and muscular patterns (shortening, dysbalance) in long-term symptomatic CTS.
While total scores of CSabs, CSnorm, OSS, DS, and SSV did not differ, mean abduction at follow-up was slightly lower in patients with type III acromions (169.7°). Presumably, the minor restriction of abduction derived from a mild form of mechanical outlet impingement. However, clinical relevance of this finding appears debatable, since only 1 patient presented with symptoms of outlet impingement (painful arc, positive Neer sign) at follow-up. Distribution of acromial morphology matches those reported in previous studies.3,18 Loew et al18 found a proportion of 16% of type III acromions in 75 patients with CTS and found no radiological correlation with typical findings of outlet impingement. Balke et al3 examined acromial morphology in patients with CTS. Only 16% of patients with CTS had a type III acromion compared with 20% of patients with symptomatic outlet impingement. In conclusion, patient populations suffering from symptomatic outlet impingement syndrome and/or rotator cuff tear differ from patients with CTS and exhibit a considerably higher prevalence of type III acromions (20%-40%).3,5 The role of acromioplasty in arthroscopic treatment of CTS is still a matter of debate. Several authors generally propose subacromial decompression (SAD) with or without CD removal.3,13,21,30 Hofstee et al13 compared open subacromial decompression with and without CD removal for treatment of CTS and found no differences in outcome after a minimum follow-up of 3 years. However, the authors did not match acromial morphology and did not perform postoperative and follow-up radiograph controls. Balke et al2 noticed less postoperative pain after a mean follow-up period of 6 years if concomitant SAD was performed. Some surgeons perform additional SAD in selective cases only15,25,28; others do not recommend its routine performance.16,20 Jerosch et al16 found that acromioplasty did not improve, even in the presence of radiologic or intraoperative subacromial stenosis. Clinical outcome, rather, was related to the extent of CD removal. The present data confirm this study. Arthroscopic CD removal without acromioplasty yielded excellent outcomes in almost 90% of patients regardless of acromial morphology. Postoperative recovery was not delayed in patients with type III acromions. We found a very slight limitation of abduction (10°) in the 15% of patients with type III acromions. Even though the finding was most likely attributed to mechanical outlet impingement, it appeared to be of little clinical relevance. Only 1 patient (1%) showed clinical signs of impingement at follow-up.
The design of this study entails some methodological deficiencies. We did not evaluate other morphological criteria, for example, lateral acromion angle and acromion index.4,22 Intraobserver reliability and repeatability of radiographic evaluation of acromial morphology according to the Bigliani criteria5 are limited. However, experienced observers proved to obtain good to excellent kappa values.7 We were unable to consistently assess preoperative outcome scores. The question of whether acromioplasty yields superior or inferior clinical results in addition to arthroscopic CD removal is beyond the scope of this investigation. Therefore, randomized controlled clinical trials should conclusively evaluate the role of additional acromioplasty in ACDSSP.
Conclusion
ACDSSP without acromioplasty yielded favorable outcomes and effected fast remission of pain regardless of acromial morphology. However, recovery of subjective shoulder function required almost 3 months on average. Minimal restriction of abduction occurred in patients with hook-shaped acromions and long-standing preoperative symptoms. The present data do not support routine performance of acromioplasty in ACDSSP.
∥References 1, 2, 6, 11, 15, 16, 20, 21, 25, 28, 34.
¶References 1, 2, 11, 15, 16, 21, 25, 28, 34.
Footnotes
The authors declared that they have no conflicts of interest in the authorship or publication of this contribution.
References
- 1. Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy. 1992;8:183–188. [DOI] [PubMed] [Google Scholar]
- 2. Balke M, Bielefeld R, Schmidt C, Dedy N, Liem D. Calcifying tendinitis of the shoulder: midterm results after arthroscopic treatment. Am J Sports Med. 2012;40:657–661. [DOI] [PubMed] [Google Scholar]
- 3. Balke M, Schmidt C, Dedy N, Banerjee M, Bouillon B, Liem D. Correlation of acromial morphology with impingement syndrome and rotator cuff tears. Acta Orthop. 2013;84:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Banas MP, Miller RJ, Totterman S. Relationship between the lateral acromion angle and rotator cuff disease. J Shoulder Elbow Surg. 1995;4:454–461. [DOI] [PubMed] [Google Scholar]
- 5. Bigliani LU, Morrison DS, April EW. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:216–228. [Google Scholar]
- 6. Boyer T. Arthroscopic treatment of calcifying tendinitis of the rotator cuff [in French]. Chir Main. 2006;25(suppl 1):S29–S35. [PubMed] [Google Scholar]
- 7. Bright AS, Torpey B, Magid D, Codd T, McFarland EG. Reliability of radiographic evaluation for acromial morphology. Skeletal Radiol. 1997;26:718–721. [DOI] [PubMed] [Google Scholar]
- 8. Constant CR. Assessment of shoulder function [in German]. Orthopade. 1991;20:289–294. [PubMed] [Google Scholar]
- 9. de Witte PB, Selten JW, Navas A, et al. Calcific tendinitis of the rotator cuff: a randomized controlled trial of ultrasound-guided needling and lavage versus subacromial corticosteroids. Am J Sports Med. 2013;41:1665–1673. [DOI] [PubMed] [Google Scholar]
- 10. Ebenbichler GR, Erdogmus CB, Resch KL, et al. Ultrasound therapy for calcific tendinitis of the shoulder. N Engl J Med. 1999;340:1533–1538. [DOI] [PubMed] [Google Scholar]
- 11. El Shewy MT. Arthroscopic removal of calcium deposits of the rotator cuff: a 7-year follow-up. Am J Sports Med. 2011;39:1302–1305. [DOI] [PubMed] [Google Scholar]
- 12. Green S, Buchbinder R, Hetrick S. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev. 2003;(2):CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hofstee DJ, Gosens T, Bonnet M, De Waal Malefijt J. Calcifications in the cuff: take it or leave it? Br J Sports Med. 2007;41:832–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Huber W, Hofstaetter JG, Hanslik-Schnabel B, Posch M, Wurnig C. The German version of the Oxford Shoulder Score—cross-cultural adaptation and validation. Arch Orthop Trauma Surg. 2004;124:531–536. [DOI] [PubMed] [Google Scholar]
- 15. Jacobs R, Debeer P. Calcifying tendinitis of the rotator cuff: functional outcome after arthroscopic treatment. Acta Orthop Belg. 2006;72:276–281. [PubMed] [Google Scholar]
- 16. Jerosch J, Strauss JM, Schmiel S. Arthroscopic treatment of calcific tendinitis of the shoulder. J Shoulder Elbow Surg. 1998;7:30–37. [DOI] [PubMed] [Google Scholar]
- 17. Katolik LI, Romeo AA, Cole BJ, Verma NN, Hayden JK, Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14:279–285. [DOI] [PubMed] [Google Scholar]
- 18. Loew M, Sabo D, Wehrle M, Mau H. Relationship between calcifying tendinitis and subacromial impingement: a prospective radiography and magnetic resonance imaging study. J Shoulder Elbow Surg. 1996;5:314–319. [DOI] [PubMed] [Google Scholar]
- 19. Lorbach O, Kusma M, Pape D, Kohn D, Dienst M. Influence of deposit stage and failed ESWT on the surgical results of arthroscopic treatment of calcifying tendonitis of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2008;16:516–521. [DOI] [PubMed] [Google Scholar]
- 20. Maier D, Jaeger M, Izadpanah K, Bornebusch L, Suedkamp NP, Ogon P. Rotator cuff preservation in arthroscopic treatment of calcific tendinitis. Arthroscopy. 2013;29:824–831. [DOI] [PubMed] [Google Scholar]
- 21. Molé D, Kempf JF, Gleyze P, Rio B, Bonnomet F, Walch G. Results of endoscopic treatment of non-broken tendinopathies of the rotator cuff. 2. Calcifications of the rotator cuff [in French]. Rev Chir Orthop Reparatrice Appar Mot. 1993;79:532–541. [PubMed] [Google Scholar]
- 22. Nyffeler RW, Werner CM, Sukthankar A, Schmid MR, Gerber C. Association of a large lateral extension of the acromion with rotator cuff tears. J Bone Joint Surg Am. 2006;88:800–805. [DOI] [PubMed] [Google Scholar]
- 23. Ogon P, Ogon M, Jager A. Technical note: the quadrant technique for arthroscopic treatment of rotator cuff calcifications. Arthroscopy. 2001;17(3):E13. [DOI] [PubMed] [Google Scholar]
- 24. Ogon P, Suedkamp NP, Jaeger M, Izadpanah K, Koestler W, Maier D. Prognostic factors in nonoperative therapy for chronic symptomatic calcific tendinitis of the shoulder. Arthritis Rheum. 2009;60:2978–2984. [DOI] [PubMed] [Google Scholar]
- 25. Porcellini G, Paladini P, Campi F, Paganelli M. Arthroscopic treatment of calcifying tendinitis of the shoulder: clinical and ultrasonographic follow-up findings at two to five years. J Shoulder Elbow Surg. 2004;13:503–508. [DOI] [PubMed] [Google Scholar]
- 26. Rizzello G, Franceschi F, Longo UG, et al. Arthroscopic management of calcific tendinopathy of the shoulder—do we need to remove all the deposit? Bull NYU Hosp Jt Dis. 2009;67:330–333. [PubMed] [Google Scholar]
- 27. Rompe JD, Zoellner J, Nafe B. Shock wave therapy versus conventional surgery in the treatment of calcifying tendinitis of the shoulder. Clin Orthop Relat Res. 2001;(387):72–82. [DOI] [PubMed] [Google Scholar]
- 28. Seil R, Litzenburger H, Kohn D, Rupp S. Arthroscopic treatment of chronically painful calcifying tendinitis of the supraspinatus tendon. Arthroscopy. 2006;22:521–527. [DOI] [PubMed] [Google Scholar]
- 29. Tempfer H, Gehwolf R, Lehner C, et al. Effects of crystalline glucocorticoid triamcinolone acetonide on cultered human supraspinatus tendon cells. Acta Orthop. 2009;80:357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tillander BM, Norlin RO. Change of calcifications after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 1998;7:213–217. [DOI] [PubMed] [Google Scholar]
- 31. Uhthoff HK. Calcifying tendinitis, an active cell-mediated calcification. Virchows Arch A Pathol Anat Histol. 1975;366:51–58. [DOI] [PubMed] [Google Scholar]
- 32. Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat Res. 1976;(118):164–168. [PubMed] [Google Scholar]
- 33. Wittenberg RH, Rubenthaler F, Wolk T, Ludwig J, Willburger RE, Steffen R. Surgical or conservative treatment for chronic rotator cuff calcifying tendinitis—a matched-pair analysis of 100 patients. Arch Orthop Trauma Surg. 2001;121:56–59. [DOI] [PubMed] [Google Scholar]
- 34. Yoo JC, Park WH, Koh KH, Kim SM. Arthroscopic treatment of chronic calcific tendinitis with complete removal and rotator cuff tendon repair. Knee Surg Sports Traumatol Arthrosc. 2010;18:1694–1699. [DOI] [PubMed] [Google Scholar]