Abstract
Background:
Traumatic knee dislocation is becoming more prevalent because of improved recognition and increased exposure to high-energy trauma, but long-term results are lacking.
Purpose:
To present 2 cases with minimum 20-year follow-up and a review of the literature to illustrate some of the fundamental principles in the management of the dislocated knee.
Study Design:
Review and case reports.
Methods:
Two patients with knee dislocations who underwent multiligamentous knee reconstruction were reviewed, with a minimum 20-year follow-up. These patients were brought back for a clinical evaluation using both subjective and objective measures. Subjective measures include the following scales: Lysholm, Tegner activity, visual analog scale (VAS), Short Form–36 (SF-36), International Knee Documentation Committee (IKDC), and a psychosocial questionnaire. Objective measures included ligamentous examination, radiographic evaluation (including Telos stress radiographs), and physical therapy assessment of function and stability.
Results:
The mean follow-up was 22 years. One patient had a vascular injury requiring repair prior to ligament reconstruction. The average assessment scores were as follows: SF-36 physical health, 52; SF-36 mental health, 59; Lysholm, 92; IKDC, 86.5; VAS involved, 10.5 mm; and VAS uninvolved, 2.5 mm. Both patients had excellent stability and were functioning at high levels of activity for their age (eg, hiking, skydiving). Both patients had radiographic signs of arthritis, which lowered 1 subject’s IKDC score to “C.”
Conclusion:
Knee dislocations have rare long-term excellent results, and most intermediate-term studies show fair to good functional results. By following fundamental principles in the management of a dislocated knee, patients can be given the opportunity to function at high levels. Hopefully, continued advances in the evaluation and treatment of knee dislocations will improve the long-term outcomes for these patients in the future.
Keywords: knee dislocation, multiligamentous knee injury, ligament reconstruction, long-term clinical outcome
The past 2 decades have seen multiple advances in the understanding and treatment of the dislocated knee. Once seen as a rare occurrence, with most orthopaedic surgeons treating only 1 or 2 in a career, multiligamentous knee injuries are now more prevalent in part because of better recognition and increased exposure to high-energy trauma.32,63 Arom et al1 used a large national insurance database and identified 8050 knee dislocations over a 6-year period (2004-2009), with a mean patient age of 35 years. We present 2 cases with a minimum 20-year follow-up that illustrate some of the fundamental principles in the management of the dislocated knee. This article will provide a summary of the literature and focus on 6 concepts: (1) the importance of treating bicruciate injuries as knee dislocations, (2) the anatomic classification that describes the injury pattern based on what is torn, (3) the options for assessing the vascular status of the dislocated knee, (4) neurological injury and the role of surgery in the dislocated knee, (5) the role of external fixation, and (6) repair versus reconstruction of the injured ligaments and timing of surgical intervention.
Case 1
The patient was injured in the spring of 1991 at the age of 22 years when he was hit by a tractor trailer while stranded on a back road in South Texas. The patient recalls being thrown 100 feet by the truck and feeling as if “the truck driver tried to hit me.” He suffered a closed KD III-MC injury (Figure 1 and Table 1), upper arm soft tissue and humeral fracture, closed head injury, and multiple rib fractures. One of the senior authors (R.C.S.) was consulted while the trauma service was performing a reverse saphenous vein graft reconstruction of the arterial injury suffered at the time of knee dislocation (Figure 2). After completion of the arterial reconstruction, a peel-off lesion of the posterior cruciate ligament (PCL) and a tibial avulsion of the medial collateral ligament (MCL) were reattached utilizing locking nonabsorbable Krackow sutures. A large tibiofemoral Steinman pin was placed with the knee in full extension from the proximal medial tibia through the notch, avoiding the PCL and MCL repair, and exiting the distal-lateral femur to provide additional skeletal stability and protection of the vascular reconstruction. The pin was removed at 10 days with manipulation under anesthesia. Six weeks after revascularization, the patient underwent an ipsilateral semitendinosus/gracilis reconstruction of his anterior cruciate ligament (ACL). Six years after injury, the patient underwent arthroscopic debridement secondary to pain and concern for meniscal injury but with continuing excellent stability. Diagnostic arthroscopy noted intact ligamentous structures but findings of early medial compartment osteoarthritis (Figure 3, A and B).
Figure 1.

Lateral (and only) radiograph of injured knee for patient 1. Radiograph was not classifiable by position system and led the authors to classify by what is torn, or anatomically. Reprinted with permission from Muscat et al.36
TABLE 1.
Anatomic Classification of Knee Dislocationsa
| Classb | Injury |
|---|---|
| KD I | PCL or ACL intact knee dislocation |
| Variable collateral involvement | |
| KD II | Both cruciates torn, collaterals intact |
| KD III | Both cruciates torn, 1 collateral torn |
| Subset M (medial) or L (lateral) | |
| KD IV | All 4 ligaments torn |
| KD V | Knee fracture-dislocation |
aACL, anterior cruciate ligament; KD, knee dislocation; PCL, posterior cruciate ligament.
bSubtypes: C, arterial injury; N, neurologic injury.
Figure 2.
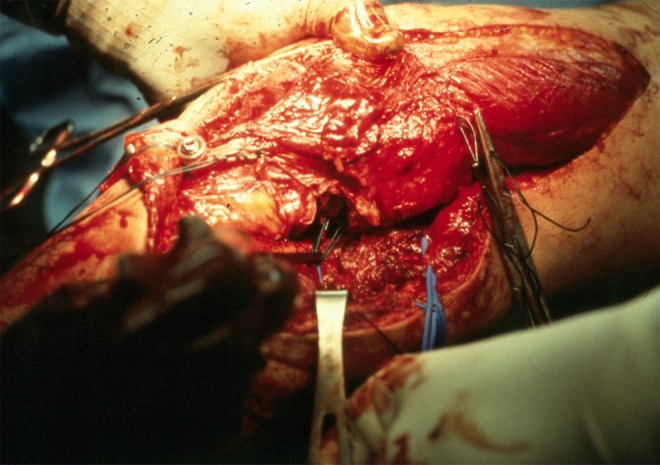
Open posteromedial approach for reverse saphenous vein grafting of a popliteal artery injury in patient 1. The sartorius, semimembranosus, semitendinosus, and gracilis tendons are incised approximately 2 cm proximal to their distal bony insertions and are reflected distally and proximally (stay sutures shown). The medial head of the gastrocnemius is incised along its proximal tendinous portion to expose the popliteal artery. Reprinted with permission from Muscat et al.36
Figure 3.
(A) Arthroscopic image of the medial compartment at 6 years after injury in patient 1. (B) Bilateral, standing, weightbearing images at 6 years after injury showing early medial compartment narrowing.
The patient was recently seen 22 years after injury (Table 2). He complained of mild knee pain, with a visual analog score (VAS) of 14 mm (uninvolved knee, 0 mm). To complete the VAS score, the patient was asked to place an “X” on a line measuring 100 mm in length to indicate his current level of pain (with 0 mm on the left side indicating no pain and 100 mm on the right side indicating the worst pain imaginable). The distance to the “X” is then measured (in mm) from the beginning of the line.
TABLE 2.
Patient Characteristics and Evaluation Resultsa
| Patient 1 | Patient 2 | |
|---|---|---|
| Age at time of injury, y | 22.4 | 49.9 |
| Sex | Male | Male |
| Follow-up, y | 22.1 | 22.7 |
| Mechanism | MVC vs pedestrian | Horse riding |
| Injury pattern | KD III-MC | KD III-L |
| Timing of reconstruction | Early PCL/MCL reattach, then staged ACL 8 wk later | Late, referred 1 y after injury |
| Graft | Reattach PCL/MCL, ACL hamstring autograft | ACL/PCL allograft, LCL autograft (biceps femoris) |
| Complications | None | None |
| Subjective assessment scores | ||
| SF-36 physical health (norm = 50) | 53.7 | 50.7 |
| SF-36 mental health (norm = 50) | 60.6 | 58.2 |
| Lysholm | 94 | 90 |
| IKDC subjective | 92 | 81 |
| VAS involved, mm (0-100) | 14 | 7 |
| VAS uninvolved, mm (0-100) | 0 | 5 |
| Tegner activity level (0-10) | Recreational sports = 6 | Moderate labor = 4 |
| Objective assessment scores | ||
| IKDC Objective | C | B |
| KT-1000 difference,b mm | ||
| 20° | 0.33 | 1.34 |
| 70° | 0.33 | 1.49 |
| Single hop distance, %b | 93.6 | 116.2 |
| 6-m timed hop, %b | 93.4 | 93.4 |
| Triple hop distance, %b | 88.9 | 115.7 |
| Cybex isokinetic quad strength, %b | 79 | 111 |
| Cybex isokinetic ham strength, %b | 98 | 82 |
| Imaging | ||
| Radiographs | Moderate-severe DJD | Mild medial DJD |
| Difference in PCL laxity on lateral stress radiograph, mmb | 5 | 8 |
| MRI | DJD, at least partial tearing of ACL | DJD, grafts intact |
aACL, anterior cruciate ligament; DJD, degenerative joint disease; IKDC, International Knee Documentation Committee; Involved, knee sustaining dislocation; KD, knee dislocation; LCL, lateral collateral ligament; MCL, medial collateral ligament; MRI, magnetic resonance imaging; MVC, motor vehicle collision; PCL, posterior cruciate ligament; SF-36, Short Form–36; VAS, visual analog scale.
bCompared with uninvolved side.
Otherwise, the patient noted continued excellent stability and continued to enjoy sporting activities such as skydiving. Knee range of motion was –2° to 130° on examination. Ligament examination showed a negative Lachman, negative posterior drawer, 1+ valgus laxity, and no varus laxity. KT-1000 measurements showed a side-to-side difference of 0.33 mm at both 20° and 70°. Stress radiographs performed with the Telos stress device (Telos, Marburg, Germany) at 90° showed similar findings.50 Radiographs revealed moderate tricompartmental arthritic changes (Figure 4, A-D). Average isokinetic strength testing performed at both 60 deg/s and 180 deg/s revealed quadriceps and hamstring strength 78.8% and 97.6% of the uninjured limb, respectively. A 6-m timed single-leg hop was 93.4% of the normal leg (average of 3 measurements). Outcomes scores showed a Short Form–36 (SF-36) score of 60.6, a Lysholm score of 94, and an International Knee Documentation Committee (IKDC) score of C (downgraded primarily because of radiographic changes).
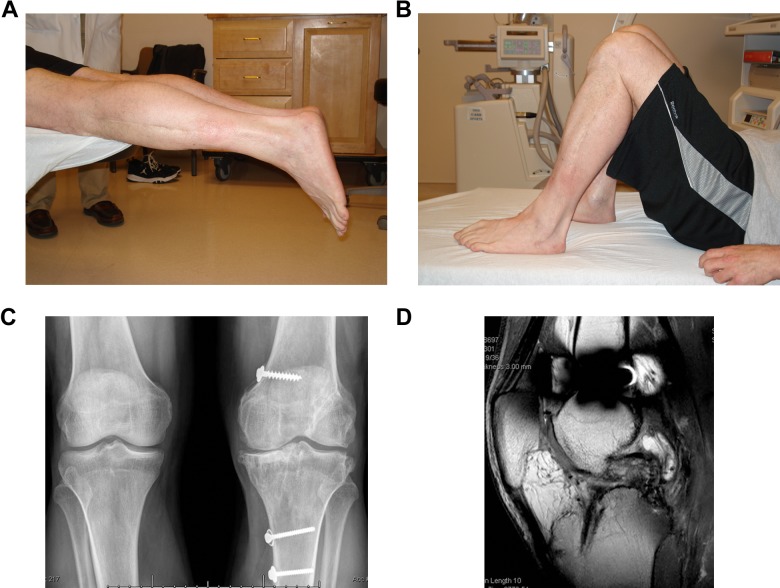
Figure 4.
(A) Prone extension of the affected knee with 2° of flexion contracture compared with normal side in patient 1 at 22-year follow-up. (B) Supine knee flexion with 10° of flexion loss compared with normal. (C) Bilateral, standing, weightbearing images with tricompartmental degenerative changes. (D) Magnetic resonance image of anterior cruciate ligament graft demonstrating some graft attenuation.
Case 2
The patient was a 50-year-old male injured in 1990 while riding a horse that fell, suffering a varus stress to the knee resulting in a knee dislocation. He presented to an outside facility with a reduced knee and a normal neurovascular examination. He was initially treated nonoperatively but underwent arthroscopy 6 months later with attempted posterolateral corner repair because of persistent instability with activities of daily living. The patient was eventually referred to one of the senior authors (D.C.W.). He underwent simultaneous PCL and ACL reconstruction with allograft patellar tendon grafts and a biceps tenodesis to reconstruct the posterolateral corner given the failed attempt at primary repair performed elsewhere.
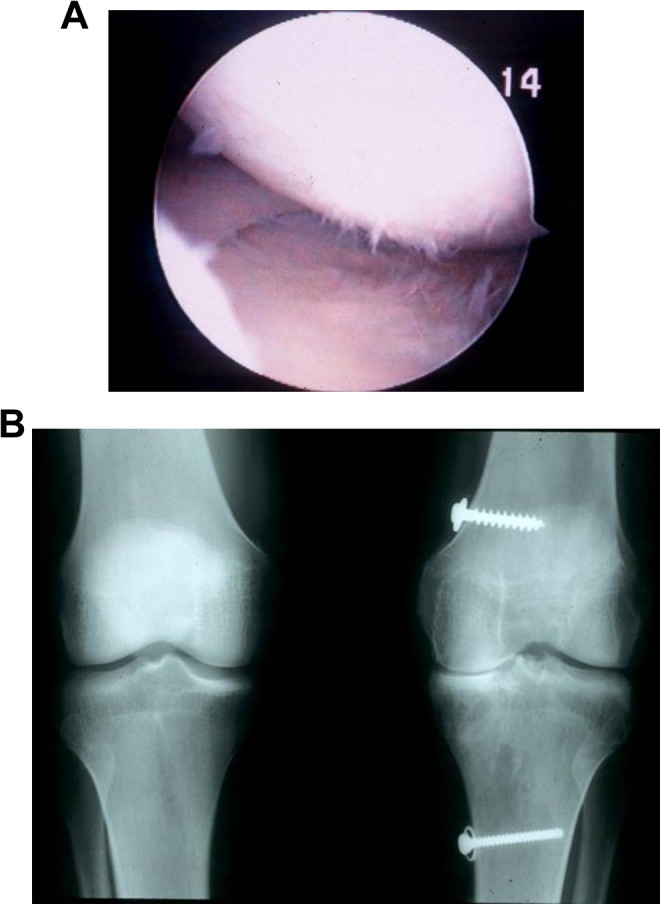
This patient was also recently seen 22 years after injury (Table 2). He complained of mild knee pain with hiking. His VAS was 7 mm versus 5 mm on his uninjured knee. On physical examination, he had knee range of motion from 0° to 130°, equal to the other knee. Ligament examination showed a negative Lachman, 1+ posterior drawer, no valgus laxity, and 1+ varus laxity. KT-1000 arthrometer measurements showed a side-to-side difference of 1.34 mm at 20° and 1.49 mm at 70°. Stress radiographs performed with the Telos stress device at 90° showed approximately 8 mm of posterior displacement of the tibia on the femur compared with the uninjured knee. Radiographs revealed mild medial joint space narrowing (Figure 5). Average isokinetic strength testing performed at both 60 deg/s and 180 deg/s revealed quadriceps and hamstring strength 111% and 82% of the uninjured limb, respectively. A 6-m timed single-leg hop was 93.4% of the normal leg. Outcomes scores showed an SF-36 of 50.7, a Lysholm score of 90, and an IKDC score of B. At most recent follow-up, the patient was 72 years of age. He enjoyed recreational hiking and had recently completed a descent and ascent of the Grand Canyon (Figure 6).
Figure 5.

Bilateral, standing, weightbearing images with mild medial joint space narrowing in patient 2 at 22-year follow-up. The broken drill bit below the Gerdy tubercle and surgical staple in the tibia are from a previous failed attempt of posterolateral corner repair at an outside hospital. The anterior cruciate ligament was repaired using a bone–patellar tendon–bone allograft with interference screw fixation (femur and tibia) and back up sutures around a screw/washer on the tibia. The posterior cruciate ligament was repaired using Achilles allograft with press fit of the bone block on the femur and sutures around a screw/washer on the tibia. The soft tissue screw and spiked washer represents the biceps tenodesis for the posterolateral corner reconstruction.
Figure 6.

Photograph of patient 2 after completing a hike of the Grand Canyon.
Bicruciate Knee Injuries
Knee dislocations are simply defined as ligamentous disruptions with loss of continuity of tibiofemoral articulation. However, several authors have recognized the existence of “spontaneously reduced” knee dislocations.11,61,63 Spontaneously reduced knee dislocations are those with plain radiographic tibiofemoral alignment but have multiple injured ligaments and gross instability on stress testing. These injuries have been identified in our previous work on knee dislocations, demonstrating that bicruciate ligament injuries are equivalent to knee dislocations with regard to mechanism of injury, severity of ligamentous injury, and frequency of major arterial injuries.63 More than 50% of dislocated knees presenting to our institution were noted to be spontaneously reduced. A combination of tears of the ACL, PCL, MCL, lateral collateral ligament (LCL), tendinous structures (patellar tendon, biceps femoris, etc), and other stabilizing structures are typical of knee dislocations. Critical to recognizing spontaneously reduced knee dislocations is the equivalent risk of injury to the popliteal artery as compared with dislocations presenting with radiographic evidence of a dislocated tibiofemoral joint. Both patients in this series illustrate the bicruciate injury pattern, although 1 patient presented dislocated and the other presented reduced. Steele and Singh58 present a case report in which a spontaneously reduced knee dislocation with popliteal artery disruption was incorrectly attributed to a compartment syndrome with absent distal pulses. The correct diagnosis was made after operative release of lower extremity compartments, when it was noted that distal vascular flow remained absent and subsequent computed tomography (CT) angiogram demonstrated complete rupture of the popliteal artery.
Knee Dislocation Classification Systems
Classification of knee dislocations has been varied and not without limitations. Position classification was the standard for decades, but as noted, in the 1990s, it was discovered that 50% of patients were spontaneously reduced and hence, unclassifiable.63 However, even when able to be classified, the position classification system gave little information about the severity of injury and was not helpful in planning treatment. One exception is the posterolateral (PL) knee dislocation. The PL dislocation implies a complex dislocation (unable to reduce the joint under closed means) that occurs with tears of the ACL, PCL, and MCL, with the MCL invaginated into the knee joint. Clinical examination reveals medial furrowing of the skin—a sine qua non of irreducibility of the dislocation. Radiographs reveal subtle tibiofemoral subluxation. These injuries require urgent open reduction to prevent skin necrosis.
Other authors have classified knee dislocations by velocity, with low velocity most commonly used in describing sporting injuries.53 Recently, the term ultra–low velocity knee dislocations has been used to describe dislocations occurring in morbidly obese patients with minimal trauma or falls.2,14
In contrast, trauma surgeons discuss fractures by levels of energy. The discrepancy in velocity versus energy when describing knee dislocations often requires a combination of both descriptive terms: energy and velocity. Regardless, in sports medicine literature, velocity is most commonly utilized. Finally, classifying knee dislocations as open or closed can help in planning the urgency of treatment. However, the vast majority of dislocations are closed injuries.
The injury seen in patient 1 helped one of the senior authors (R.C.S.) to realize the limitation of the position classification (appears perched on lateral radiograph; additionally, no anteroposterior radiograph was obtained) and led him to the concept of classifying knee dislocations based on what is torn, the “anatomic classification.”61 This system has proven to be useful in discussing knee dislocation injuries between surgeons and in the literature.11 More important, the system allows for directing the surgeon in what needs to be treated.
Anatomic Classification of Knee Dislocations
There are 5 major injury patterns that can occur in a dislocated knee (Table 1). Injuries are classified by roman numerals; in general, higher number injuries have sustained greater trauma than lower number injuries (higher energy). A KD I is a knee dislocation with injury to 1 of the cruciate ligaments, and includes both PCL intact and ACL intact dislocation injuries.8,54 KD I injuries are usually seen in sporting injuries and would be described as low-velocity or lower energy injuries. A KD II is a bicruciate injury with functionally intact collateral ligaments. Although rare, the KD II occurs in straight extreme knee hyperextension without varus or valgus forces to disrupt an associated corner. In contrast, KD III, the most common injury pattern, involves tears of both cruciate ligaments and 1 of the collateral ligaments. These injuries are subdivided into medial-sided (KD III-M) or lateral-sided (KD III-L) injuries. It is important to note that the designation of injury is best made by physical examination. For example, a KD III-M will have complete tearing of the medial side (both MCL and posteromedial corner [PMC]) on examination but a stable posterolateral corner (PLC) on varus and dial tests. Although magnetic resonance imaging (MRI) may show fluid or partial injury of the PLC, the functionally intact PLC makes this a KD III-M. A KD IV involves complete disruption of all 4 major knee ligaments and is usually only seen in high-energy motor vehicle trauma (the senior authors prefer the terminology of high energy rather than velocity). Finally, the KD V group is a knee dislocation with the presence of a major periarticular fracture and is best described and classified as a fracture-dislocation of the knee.35,47,49,63 The final component of the anatomic classification is the use of additional labels to identify associated neurovascular injuries. A subtype “C” indicates a popliteal arterial injury, and subtype “N” indicates a peripheral nerve injury, either to the tibial nerve or, more commonly, the peroneal nerve. This “N” subtype is used for any neurological deficit (neuropraxia, neurotmesis, or axonotmesis). Tendinous injuries, avulsions of the biceps femoris, tibial tubercle, and quadriceps tendon tears are important and added as descriptive terminology. Injury to the medial patellofemoral ligament (MPFL) is often seen in grossly injured KD III-M or KD IV knees and, in contrast to the examination under anesthesia (EUA), is often accurately determined by MRI. The posterolateral knee dislocation is usually a KD III-MN injury. Interestingly, the senior author (R.C.S.) first published this system in 1994,61 but it was not until a presentation by Bill Clancy at the American Orthopaedic Society of Sports Medicine Annual Meeting in 1997 that the concept was routinely recognized and utilized by sports surgeons worldwide.10,25
Vascular Examination in the Dislocated Knee
The evaluation and treatment of arterial injuries in knee dislocations has evolved over the past 25 years. Initial recommendations by Jones et al23 in 1979 discussed the need for arteriography in all patients with a knee dislocation. The authors advocated for routine arteriography because of the “unreliability of clinical examination.” In that study, the presence of postreduction pulses did not rule out an arterial injury, as 27% of their patients had palpable pulses present at the time of diagnosis of an arterial injury. Arteriography was the standard of care, with a quoted incidence of arterial injuries in a knee dislocation of 33%, as described by the Piedmont Orthopaedic Group.16,30
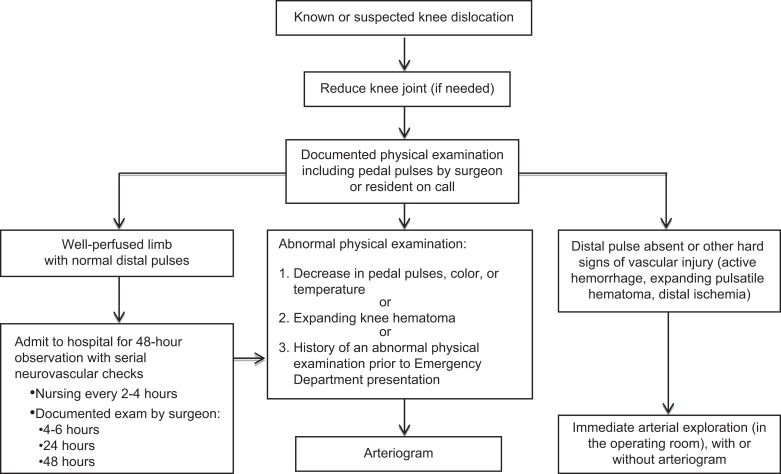
In 1993, Kendall et al24 published their study of a small cohort of 35 patients where clinical examination was reliable and the presence of a normal vascular examination (normal and symmetrical pulses, capillary refill, neurological examination) proved to be reliable to screen patients with knee dislocations for “selective” arteriography. Stannard et al56 then developed a prospective protocol where clinical examination was utilized to safely follow knee dislocation patients with a normal vascular examination without utilizing arteriography. It is critical that the orthopaedic surgeon follow the protocol by Stannard et al56 carefully when utilizing selective arteriography (Figure 7). Importantly, the clinical neurovascular examination must be normal without any evidence of neurologic injury or extremity asymmetry in the vascular examination throughout the prehospital course (ie, time of injury and triage) and at initial evaluation in the emergency department. The protocol requires both nursing evaluations every 2 to 4 hours and physician examinations at time zero, at 4 to 6 hours, 24 hours, and 48 hours after presentation. On a busy trauma service or at a community hospital where the orthopaedic surgeon has multiple call responsibilities, these repeated clinical examinations by the physician can be difficult to properly follow. We cannot emphasize enough that if utilizing the selective arteriography approach, subtle changes in serial examinations must prompt urgent vascular imaging. We have seen cases where failure to act on mild abnormalities (eg, mottling, present but unequal pulses, discrepancies between nursing and physician examination, etc) has led to a delayed diagnosis of complete popliteal artery disruption and loss of limb. We feel that it is critical to have a treatment algorithm at each institution for the dislocated knee centered around the vascular examination. This can be based on the protocol by Stannard et al,56 as described above, or institution specific, such as that described at the University of Pittsburgh by Seroyer et al.52
Figure 7.
Standard protocol for selective arteriography.
In our experience, many patients with high-energy knee dislocations have associated injuries that are evaluated by CT scanning. In these patients, it is relatively easy to simultaneously perform a CT angiogram to evaluate the popliteal artery. Use of other objective noninvasive studies such as an ankle-brachial index (ABI ≥0.9) or an arterial Doppler can be extremely useful as an adjunct to physical examination.33,59 In those patients presenting late, the senior authors recommend a thorough vascular examination and an additional objective study such as ABI or noninvasive vascular studies. It is the authors’ preference to perform an arterial and venous Doppler to rule out arterial injury or deep venous thrombosis in patients who are referred several days after imaging without arteriography.
Failure to restore arterial flow within 8 hours of injury usually results in amputation.20,38 As seen with patient 1, prompt arterial repair can salvage an extremity with normal vascular function at 22-year follow-up. He presented with a dysvascular, pulseless leg, and the patient underwent immediate arterial exploration without arteriography utilizing a posteromedial approach.36 This highlights that obtaining an arteriogram should not delay the emergent treatment of an obvious vascular injury. Furthermore, the effect of vascular insufficiency on the development of knee osteoarthritis has been discussed predominantly in the rheumatology literature.13 Disruption of blood flow in subchondral bone may reduce nutrient diffusion to articular cartilage. Ischemia in subchondral bone may produce osteocyte death, bone resorption, and articular damage. It is unclear if patient 1’s time in the field (vascular insufficiency) contributed to the degree of osteoarthritis at long-term follow-up.
Neurological Evaluation and Treatment in the Dislocated Knee
The incidence of neurologic injury with knee dislocation is estimated to be between 10% and 40%, with the common peroneal nerve being the most frequently injured.4,17 While vascular injuries can be limb threatening, neurologic injuries affect function, can cause neuropathic pain, and negatively affect overall quality of life.5,7 Patients with multiligamentous knee injuries and common peroneal nerve palsy have the worst functional outcomes.42,51 Peroneal nerve palsy is a debilitating problem that can affect timing of surgical reconstruction and overall knee and lower extremity function.
Peskun et al40 reviewed a series of 26 patients with peroneal nerve palsy secondary to knee dislocation. Peroneal nerve injury was defined as lack of sensation over the dorsum of the foot and 0/5 motor function on examination. KD III-L was the most common ligamentous injury pattern in their series. Sex, body mass index, and fibular head fractures were found to be associated with peroneal nerve injury. The rate of peroneal nerve recovery in this study was 31%, with younger patient age being a favorable factor for nerve recovery.
Conservative management with stretching, splinting, and physical therapy to avoid contracture can be appropriate in the early phase of treatment. Electromyography and nerve conduction velocity testing are commonly used tools to help determine the site and severity of peripheral nerve injuries. However, findings that indicate nerve injury (positive sharp waves, fibrillations) are generally not present until 2 to 3 weeks after injury, which limits their usefulness in the acute postinjury phase. For persistent nerve damage, surgery is the treatment of choice as it results in better functional outcomes.9,15 Neurolysis, primary nerve repair, nerve grafting, and posterior tibialis tendon transfer have all been used by surgeons as viable surgical treatment options. Our preference is for exploration and neurolysis of the peroneal nerve at the time of planned ligament reconstruction. The patient is then closely followed with serial examinations and electromyographic studies. Additional procedures such as posterior tibialis tendon transfer may be necessary if nerve function does not recover.34,37
Role of External Fixation in Knee Dislocations
In 1991, the senior author (R.C.S.) utilized a tibiofemoral Steinmann pin and ligamentous repair to protect the arterial reconstruction. Today, we utilize a spanning external fixator to protect the vessels, with delayed ligamentous reconstruction after 6 weeks. The use of external fixation has been recommended for the treatment of knee dislocation in a variety of algorithms in which immediate stabilization is required with or without ligamentous repair or reconstruction.3,44,46,48,57 Mercer et al31 highlighted the interest in this topic when they examined the stiffness of various external fixator (ex-fix) constructs for the treatment of traumatic knee dislocations. Ex-fix devices provide stability to the knee and maintain reduction, allowing soft tissue healing. In addition to protecting a vascular repair, we believe that external fixators are also indicated for various presentations: open knee dislocations, in the multitrauma patient or one with a closed head injury, and inability to maintain reduction by closed means. Furthermore, external fixation in obese patients with ultra–low velocity dislocations has recently been described by Azar et al2 as a reliable joint stabilization adjunct to brace (knee immobilizer) stabilization in a conically shaped leg due to morbid obesity.
Repair Versus Reconstruction
Comparing ligamentous treatment approaches to our patients’ injuries is also instructive. Historically, primary repair of all injured ligaments frequently led to recurrent laxity if early mobilization was accomplished.55 This led many authors to advocate for reconstruction of the cruciate ligaments and associated collateral ligaments, as was done in patient 2. The use of allografts and autografts with simultaneous reconstruction of the cruciates and corner with a delayed presentation is a commonly utilized technique.‡ Chhabra et al6 reviewed a series of 31 patients operatively treated with multiple ligament reconstruction for knee dislocations. Nineteen patients were treated acutely (<3 weeks from injury) and trended toward higher subjective scores and objective knee stability. Average loss of flexion was 12°, with 4 patients requiring manipulation because of stiffness. Nearly all patients were able to perform daily activities with few problems; however, return to high-demand sports and manual labor was less predictable. Multiple reviews in the literature increasingly show a consensus that surgical intervention should be performed early (within 2-3 weeks), leading to improved outcome measures.21,27
Levy et al26 noted a significant failure rate (40%) with repair of the LCL and posterolateral corner. Of note, these authors showed that if a repair does fail, then revision reconstruction will produce similar results to the patient undergoing an initial reconstruction. As seen in patient 1, secure repair of ligament avulsions can provide successful long-term stability. Currently, we perform primary repair of ligament avulsions (ie, PCL peel off or tibial eminence avulsion) as we believe a successful repair more accurately restores anatomy and functional stability compared with a reconstruction.
Over the past 30 years, many synthetic devices have been used for ligament reconstruction, such as the Carbon (Integraft, AMS Research Corp, Minnetonka, Minnesota, USA), Gore-Tex (W.L. Gore & Associates, Elkton, Maryland, USA), Dacron (Invista, Wichita, Kansas, USA), the Leeds-Keio artificial ligament (Xiros, Leeds, UK), and the Kennedy ligament augmentation device (Minnesota Mining and Manufacturing Co, St Paul, Minnesota, USA). After an initial wave of enthusiasm, disadvantages appeared including poor long-term stability, synovitis, and knee effusions. The Ligament Advanced Reinforcement System (LARS; LARS Surgical Implants and Devices, Arc-sur-Tille, France) has recently been described in the literature with early promising results in ligament reconstruction as an alternative to allografts, but long-term results, safety, and efficacy compared with the current standard of care are needed.22,43
Conclusion
It is critical to treat each patient individually (based on anatomic structures injured, age, ability to participate in postoperative rehabilitation, comorbidities, etc) while adhering to some fundamental principles in the management of the dislocated knee. The senior authors regularly treat multiligamentous injuries as the primary surgeon as well as participate in discussions with other treating surgeons at outside facilities or at their own level I trauma center. The critical questions are always: associated injuries, vascular tree, soft tissue envelope, and ability to participate in a postoperative rehabilitation program. Temporary external fixation and liberal use of arteriography (CT angiography most commonly) in the multiple-trauma patient with a dislocated knee are recommended as commonly as is early range of motion and simultaneous reconstruction of all torn structures in the competitive contact athlete with an isolated knee dislocation. The orthopaedic surgeon treating patients with knee dislocations must keep in mind the surrounding factors before managing the ligamentous reconstructions. With an isolated injury in the sporting population, a management tree is often simple, and surgical timing depends on motion and personal preferences for cruciate and corner reconstructions. However, in more than half of patients, such treatment decisions require attention first to other potentially life-threatening injuries, and the ligamentous injury takes secondary importance to treating the patient as a whole.
Finally, the evaluation of these 2 patients with long-term follow-up underlines the lack of a disease-specific outcome measure for knee dislocations. At over 20-year follow-up, both patients had good stability and were functioning at high levels of activity for their ages. This is reflected in their high Lysholm and Tegner activity scores. However, both patients had radiographic signs of arthritis, which for patient 1 lowered his IKDC score to C. Given these findings, we feel that measures of stability and function are more important to an active patient population than are arthritic changes on radiograph. In our experience, lower outcome scores are seen in high-energy dislocations with associated trauma. Most reassuring were the findings that in both patients, mental and physical health, as evaluated by the SF-36, were well maintained despite the significant knee injuries (as well as multitrauma seen in patient 1). Knee dislocations have rare long-term excellent results, and most intermediate-term studies show fair to good functional results. Hopefully, continued advances in the evaluation and treatment of knee dislocations will improve the long-term outcomes for these patients in the future.
Acknowledgment
The authors thank the University of New Mexico Knee Dislocation research team, including Kim Fields, research coordinator; Burke Gurney, PT, PhD; James Dexter, PT, MA; Lindsey Dietrich, MD; Ron Andrews, PT, PhD; and Sandra Schreyer.
‡References 12, 18, 19, 27-29, 39, 41, 45, 60, 62, 64.
Footnotes
One or more of the authors declared the following potential conflict of interest or source of funding: Institutional and fellowship support was received from Arthrex and Smith & Nephew.
References
- 1. Arom GA, Yeranosian MG, Petrigliano FA, Terrell RD, McAllister DR. The changing demographics of knee dislocation: a retrospective database review [published online November 9, 2013]. Clin Orthop Relat Res. doi:10.1007/s11999-013-3373-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Azar FM, Brandt JC, Miller RH, 3rd, Phillips B. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39:2170–2174. [DOI] [PubMed] [Google Scholar]
- 3. Bin SI, Nam T. Surgical outcome of 2-stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy. 2007;23:1066–1072. [DOI] [PubMed] [Google Scholar]
- 4. Bonnevialle P, Dubrana F, Galau B, et al. Common peroneal nerve palsy complicating knee dislocation and bicruciate ligaments tears. Orthop Traumatol Surg Res. 2010;96:64–69. [DOI] [PubMed] [Google Scholar]
- 5. Bruijn IL, Geertzen JH, Dijkstra PU. Functional outcome after peroneal nerve injury. Int J Rehabil Res. 2007;30:333–337. [DOI] [PubMed] [Google Scholar]
- 6. Chhabra A, Cha PS, Rihn JA, et al. Surgical management of knee dislocations: surgical technique. J Bone Joint Surg Am. 2005;87 (suppl 1):1–21. [DOI] [PubMed] [Google Scholar]
- 7. Ciaramitaro P, Mondelli M, Logullo F, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010;15:120–127. [DOI] [PubMed] [Google Scholar]
- 8. Cooper DE, Speer KP, Wickiewicz TL, Warren RF. Complete knee dislocation without posterior cruciate ligament disruption. A report of four cases and review of the literature. Clin Orthop Relat Res. 1992;(284):228–233. [PubMed] [Google Scholar]
- 9. Cush G, Irgit K. Drop foot after knee dislocation: evaluation and treatment. Sports Med Arthrosc. 2011;19:139–146. [DOI] [PubMed] [Google Scholar]
- 10. Darabos N, Gusic N, Vlahovic T, Darabos A, Popovic I, Vlahovic I. Staged management of knee dislocation in polytrauma injured patients. Injury. 2013;44 (suppl 3):S40–S45. [DOI] [PubMed] [Google Scholar]
- 11. Eastlack RK, Schenck RC, Jr, Guarducci C. The dislocated knee: classification, treatment, and outcome. US Army Med Department J. 1997;11 (12):2–9. [Google Scholar]
- 12. Fanelli GC, Edson CJ. Arthroscopically combined anterior and posterior cruciate ligament reconstruction in the multiple ligament injured knee: 2- to 10-year follow-up. Arthroscopy. 2002;18:703–714. [DOI] [PubMed] [Google Scholar]
- 13. Findlay DM. Review: vascular pathology and osteoarthritis. Rheumatology. 2007;46:1763–1768. [DOI] [PubMed] [Google Scholar]
- 14. Georgiadis AG, Mohammad FH, Mizerik KT, Nypaver TJ, Shepard AD. Changing presentation of knee dislocation and vascular injury from high-energy trauma to low-energy falls in the morbidly obese. J Vasc Surg. 2013;57:1196–1203. [DOI] [PubMed] [Google Scholar]
- 15. Giuseffi SA, Bishop AT, Shin AY, Dahm DL, Stuart MJ, Levy BA. Surgical treatment of peroneal nerve palsy after knee dislocation. Knee Surg Sports Traumatol Arthrosc. 2010;18:1583–1586. [DOI] [PubMed] [Google Scholar]
- 16. Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59:236–239. [PubMed] [Google Scholar]
- 17. Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86–A: 262–273. [DOI] [PubMed] [Google Scholar]
- 18. Hirschmann MT, Iranpour F, Muller W, Friederich NF. Surgical treatment of complex bicruciate knee ligament injuries in elite athletes: what long-term outcome can we expect? Am J Sports Med. 2010;38:1103–1109. [DOI] [PubMed] [Google Scholar]
- 19. Hirschmann MT, Meier MD, Amsler F, Friederich NF. Long-term outcome of patients treated surgically for traumatic knee dislocations: does the injury pattern matter? Phys Sportsmed. 2010;38:82–89. [DOI] [PubMed] [Google Scholar]
- 20. Hoover NW. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin North Am. 1961;41:1099–1112. [DOI] [PubMed] [Google Scholar]
- 21. Howells NR, Brunton LR, Robinson J, Porteus AJ, Eldridge JD, Murray JR. Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury. 2011;42:1198–1204. [DOI] [PubMed] [Google Scholar]
- 22. Ibrahim SA, Ahmad FH, Salah M, Al Misfer AR, Ghaffer SA, Khirat S. Surgical management of traumatic knee dislocation. Arthroscopy. 2008;24:178–187. [DOI] [PubMed] [Google Scholar]
- 23. Jones RE, Smith EC, Bone GE. Vascular and orthopedic complications of knee dislocation. Surg Gynecol Obstet. 1979;149:554–558. [PubMed] [Google Scholar]
- 24. Kendall RW, Taylor DC, Salvian AJ, O’Brien PJ. The role of arteriography in assessing vascular injuries associated with dislocations of the knee. J Trauma. 1993;35:875–878. [DOI] [PubMed] [Google Scholar]
- 25. Krych AJ, Giuseffi SA, Kuzma SA, Stuart MJ, Levy BA. Is peroneal nerve injury associated with worse function after knee dislocation [published online February 27, 2014]? Clin Orthop Relat Res. doi:10.1007/s11999-014-3542-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. [DOI] [PubMed] [Google Scholar]
- 27. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25:430–438. [DOI] [PubMed] [Google Scholar]
- 28. Levy BA, Krych AJ, Shah JP, Morgan JA, Stuart MJ. Staged protocol for initial management of the dislocated knee. Knee Surg Sports Traumatol Arthrosc. 2010;18:1630–1637. [DOI] [PubMed] [Google Scholar]
- 29. Linko E, Harilainen A, Malmivaara A, Seitsalo S. Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. Cochrane Database Syst Rev. 2005;(2):CD001356. [DOI] [PubMed] [Google Scholar]
- 30. McDonough EB, Jr, Wojtys EM. Multiligamentous injuries of the knee and associated vascular injuries. Am J Sports Med. 2009;37:156–159. [DOI] [PubMed] [Google Scholar]
- 31. Mercer D, Firoozbakhsh K, Prevost M, Mulkey P, DeCoster TA, Schenck R. Stiffness of knee-spanning external fixation systems for traumatic knee dislocations: a biomechanical study. J Orthop Trauma. 2010;24:693–696. [DOI] [PubMed] [Google Scholar]
- 32. Meyers M, Harvey JP. Traumatic dislocation of the knee joint. J Bone Joint Surg Am. 1971;53:16–29. [PubMed] [Google Scholar]
- 33. Mills WJ, Barei DP, McNair P. The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study. J Trauma. 2004;56:1261–1265. [DOI] [PubMed] [Google Scholar]
- 34. Molund M, Engebretsen L, Hvaal K, Hellesnes J, Ellingsen Husebye E. Posterior tibial tendon transfer improves function for foot drop after knee dislocation [published online February 25, 2014]. Clin Orthop Relat Res. doi:10.1007/s11999-014-3533-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Moore TM. Fracture-dislocation of the knee. Clin Orthop. 1981;156:128–140. [PubMed] [Google Scholar]
- 36. Muscat JO, Roger W, Cruz AB, Schenck RC ., Jr The posteromedial approach for vascular control about the knee. J Orthop Trauma. 1996;10:476–480. [DOI] [PubMed] [Google Scholar]
- 37. Ozkan T, Tucner S, Ozturk K, Aydin A, Ozkan S. Tibialis posterior tendon transfer for persistent drop foot after peroneal nerve repair. J Reconstr Microsurg. 2009;25:157–164. [DOI] [PubMed] [Google Scholar]
- 38. Patterson BM, Agel J, Swiontkowski MF, Mackenzie EJ, Bosse MJ; LEAP Study Group. Knee dislocations with vascular injury: outcomes in the Lower Extremity Assessment Project (LEAP) Study. J Trauma. 2007;63:855–858. [DOI] [PubMed] [Google Scholar]
- 39. Peccin MS, Almeida GJM, Amaro J, Cohen M, Soares BG, Atallah AN. Interventions for treating posterior cruciate ligament injuries of the knee in adults. Cochrane Database Syst Rev. 2005;(2):CD002939. [DOI] [PubMed] [Google Scholar]
- 40. Peskun CJ, Chahal J, Steinfeld ZY, Whelan DB. Risk factors for peroneal nerve injury and recovery in knee dislocation. Clin Orthop Relat Res. 2012;470:774–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Peskun CJ, Whelan DB. Outcomes of operative and nonoperative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc. 2011;19:167–173. [DOI] [PubMed] [Google Scholar]
- 42. Plancher KD, Siliski J. Long-term functional results and complications in patients with knee dislocations. J Knee Surg. 2008;21:261–268. [DOI] [PubMed] [Google Scholar]
- 43. Ranger P, Renaud A, Phan P, Dahan P, De Oliveira E, Jr, Delisle J. Evaluation of reconstructive surgery using artificial ligaments in 71 acute knee dislocations. Int Orthop. 2011;35:1477–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12:334–346. [DOI] [PubMed] [Google Scholar]
- 45. Rios A, Villa A, Fahandezh H, de Jose C, Vaguero J. Results after treatment of traumatic knee dislocations: a report of 26 cases. J Trauma. 2003;55:489–494. [DOI] [PubMed] [Google Scholar]
- 46. Robertson A, Nutton RW, Keating JF. Dislocation of the knee. J Bone Joint Surg Br. 2006;88:706–711. [DOI] [PubMed] [Google Scholar]
- 47. Schenck RC., Jr The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 48. Schenck RC., Jr Multiple Ligamentous Injuries in the Athlete. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2003. [Google Scholar]
- 49. Schenck RC, McGanity PLJ, Heckman JD. Femoral-sided fracture-dislocations of the knee. J Orthop Trauma. 1997;11:416–421. [DOI] [PubMed] [Google Scholar]
- 50. Schulz MS, Steenlage ES, Russe K, Strobel MJ. Distribution of posterior tibial displacement in knees with posterior cruciate ligament tears. J Bone Joint Surg Am. 2007;89:332–338. [DOI] [PubMed] [Google Scholar]
- 51. Seebacher JR, Inglis AE, Marshall JL, Warren RF. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64:536–541. [PubMed] [Google Scholar]
- 52. Seroyer ST, Musahl V, Harner CD. Management of the acute knee dislocation: the Pittsburgh experience. Injury. 2008;39:710–718. [DOI] [PubMed] [Google Scholar]
- 53. Shelbourne KD, Porter DA, Clingman JA, McCarroll JR, Rettig AC. Low-velocity knee dislocation. Orthop Rev. 1991;20:995–1004. [PubMed] [Google Scholar]
- 54. Shelbourne KD, Pritchard J, Rettig AC, McCarroll JR, Vanmeter CD. Knee dislocations with intact PCL. Orthop Rev. 1992;21:610–611. [PubMed] [Google Scholar]
- 55. Sisto DJ, Warren RF. Complete knee dislocation: a follow-up study of operative treatment. Clin Orthop. 1985;198:94–101. [PubMed] [Google Scholar]
- 56. Stannard JP, Sheils TM, Lopez-Ben RR, McGwin G, Jr, Robinson JR, Volgas DA. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86–A: 910–915. [PubMed] [Google Scholar]
- 57. Stannard JP, Sheils TM, McGwin G, Volgas DA, Alonso JE. Use of a hinged external knee fixator after surgery for knee dislocation. Arthroscopy. 2003;19:626–631. [DOI] [PubMed] [Google Scholar]
- 58. Steele HL, Singh A. Vascular injury after occult knee dislocation presenting as compartment syndrome. J Emerg Med. 2012;42:271–274. [DOI] [PubMed] [Google Scholar]
- 59. Tocci SL, Heard WM, Fadale PD, Brody JM, Born C. Magnetic resonance angiography for the evaluation of vascular injury in knee dislocations. J Knee Surg. 2010;23:201–207. [DOI] [PubMed] [Google Scholar]
- 60. Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:739–749. [DOI] [PubMed] [Google Scholar]
- 61. Walker DN, Hardison RR, Schenck RC., Jr A baker's dozen of knee dislocations. Am J Knee Surg. 1994;7:117–124. [Google Scholar]
- 62. Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen nonirradiated allografts. Am J Sports Med. 1999;27:189–196. [DOI] [PubMed] [Google Scholar]
- 63. Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–529. [DOI] [PubMed] [Google Scholar]
- 64. Wong C, Tan J, Chang HC, Khin LW, Low CO. Knee dislocations – a retrospective study comparing operative versus closed immobilization treatment outcomes. Knee Surg Sports Traumatol Arthrosc. 2004;12:540–544. [DOI] [PubMed] [Google Scholar]