Abstract
Background:
The number of children and adolescents with anterior cruciate ligament (ACL) reconstructions is increasing, and disturbing reports on high rerupture rates in this group have been noted.
Purpose:
To describe the outcome of ACL reconstruction in children and adolescents based on data from the Danish Knee Ligament Reconstruction Registry (DKRR).
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Data were retrieved from the DKRR, a national population-based registry. The analysis was based on a population of 14,806 ACL-reconstructed patients. The outcome was evaluated using risk of ACL revision, subjective outcome score (Knee injury and Osteoarthritis Outcome Score [KOOS]), Tegner function score, and objective knee laxity. Three age groups were defined (A, <13 years; B, 13-15 years; and C, 15-20 years) and compared with D, patients ≥20 years (adults). There were 95 patients in group A, 327 in B, 2888 in C, and 11,496 in D.
Results:
There was a significantly increased risk of revision surgery in the age groups B (6.7%) and C (4.9%) compared with the adults in group D (2.0%). Objective knee laxity did not differ between the 4 groups. Groups A, B, and C had a higher score on the combined KOOS symptoms, pain, sport, and quality of life subscales (KOOS4; 79.6, 76.6, and 73.1, respectively) compared with the adults (69.7). Group B had higher KOOS quality of life (76.6) and sports (71.1) scores than did group C (73.1 and 66.4, respectively). The Tegner activity score did not differ between the 4 groups. No impact of the use of extracortical graft fixation was detected in the youngest age group.
Conclusion:
Study results indicated an increased risk of graft failure in patients between 13 and 20 years of age. This is in contrast to the better subjective and equal objective knee score found in the same age groups.
Clinical Relevance:
The new knowledge about the high revision rate among ACL-reconstructed teenagers is important for evidence-based preoperative information of ACL patients and their parents.
Keywords: knee, ACL, reconstruction, adolescent, revision, national registry
A significant number of anterior cruciate ligament (ACL) injuries are seen in children and adolescents.2,7 Among youth soccer players, 7% of all injuries are midsubstance ACL tears.29 According to the Danish Knee Ligament Reconstruction Registry (DKRR), 6% of all ACL reconstructions are performed in patients younger than 15 years.18
Conservative treatment of ACL injuries in skeletally immature patients who continue to be active in competitive sports increases the risk of subsequent chondral and meniscal injury.3,13 Furthermore, Millett et al21 found a higher incidence of subsequent meniscal and cartilage injuries when ACL reconstruction was delayed in this group of patients. These findings have resulted in a general strategy to perform early ACL reconstruction in skeletally immature patients with ACL lesions.
Numerous reports exist on the outcomes of ACL reconstruction in children and adolescents.4,10,13,14,16,20,26 Most of the studies report satisfactory results in terms of subjective and objective outcomes. However, due to small sample sizes, these studies are unable to determine any changes in failure and revision rates.
The risk for revision of ACL reconstruction was found to be an alarming 13 times higher in a group of patients younger than 20 years compared with older patients.19 In comparison, another study found the revision rate to be 2.5 times higher in patients younger than 20 years.17
On the basis of literature review, Moksnes et al22 questioned whether there is sufficient evidence for surgical treatment of ACL lesions in children. The authors found that the methodological quality of the existing articles is too low for advocating surgical treatment of ACL reconstruction in children since the existing literature shows conflicting results.
Consequently, there is a need for more data elucidating the results after ACL reconstruction in children and adolescents. The aim of this study was to describe outcome and revisions rates in a large nationwide cohort of ACL-reconstructed children and adolescents.
Methods
Study Setting
Denmark has a population of 5.5 million people. Danish citizens are registered in different medical and administrative registers, and all Danish citizens are registered with a unique personal security number in the Danish Civil Registration System (CRS). This registration makes it possible to identify all citizens and to link data between several different registries at the level of the individual.
The Danish Knee Ligament Reconstruction Register
The DKRR is a nationwide population-based clinical database established on July 1, 2005. The purpose of the database is to improve the monitoring and quality of primary and revision ACL surgery in Denmark.18 Both private (n = 27) and public (n = 24) hospitals report to the register, as registration is compulsory according to the Declaration Number 459 of June 2006.6 Completeness of registrations in the DKRR has been more than 85% for the past 3 years.25
Detailed preoperative, intraoperative, and 1-year follow-up data were recorded by the operating surgeon using a standardized form and a secure Internet portal.18 Furthermore, patients independently reported subjective scores on knee function using the Knee injury and Osteoarthritis Outcome Score (KOOS)27 and Tegner functional score.31 The KOOS and Tegner scores are validated subjective patient-related outcomes calculated according to published standards. Likewise, the KOOS4 is a validated patient-related outcome calculated from the 4 most responsive KOOS subscores: symptoms, pain, sport, and quality of life.9 KOOS scores range from 0 to 100, and Tegner scores range from 1 to 10, with higher scores representing better results. These data were web-recorded by the patient before surgery and 1 year after surgery.
The Danish Civil Registration System
All Danish citizens receive a unique 10-digit personal identification number at birth. The CRS records information on changes in vital status of all Danish citizens including changes in address, date of emigration, and the date of death since 1968.23 Precise individual-level linkage between public Danish registers is possible due to this personal identification number. In this study, the CRS was used to obtain complete follow-up data on all patients.
Study Population
In total, we identified 14,924 primary ACL procedures in 14,702 patients in the period from July 2005 to December 31, 2011. In 23 cases, the data entry was misleading, and the relevant patients were therefore excluded. During this period, 200 patients had emigrated. In 42 cases of operated knees, the patients had residence in Greenland, and in 53 cases, the patients had a nationality other than Danish. These 2 groups could not be properly followed up with, and consequently, they were excluded. In total, this left us with 14,806 primary ACL procedures included in our analysis. We divided these patients into 4 age groups: A, <13 years; B, 13-15 years; C, 15-20 years; and D, ≥20 years (adults). There were 95 patients in group A, 327 in B, 2888 in C, and 11,496 in D.
Outcomes
The primary outcome was revision ACL reconstruction. The follow-up period started from the day of the primary ACL surgery and ended on the day of revision of the primary ACL if revision occurred or at time of death or status date, which was the end of the study period (December 31, 2011), whichever came first. At the time of revision, the operating surgeon was prompted by the DKRR to enter data regarding his view on the course for the graft rupture. These data were based to the surgeon’s judgment.
The secondary outcomes were parameters of objective knee stability in terms of pivot-shift scores and instrumented side-to-side difference (eg, Rolimeter or KT1000) measured 1 year after primary ACL reconstruction. The pivot-shift test is a dynamic but passive test of the knee that measures the rotational stability of the ACL. The pivot-shift test is graded using a 4-point scale form normal (0), glide (1), clunk (2), and gross (3).15 The pivot-shift data were divided into 2 groups: negative results (n = 5094) and positive results (n = 1035). The instrumented side-to-side difference measures the variation in sagittal stability between the operated and healthy knee. Patients were categorized as having a difference of either ≤2 or >2 mm. Only patients with no previous ACL operation to their other knee were included in these analyses. Hence, 393 knees were excluded from these analyses.
Furthermore, we used patient-related outcomes (KOOS and Tegner score reported 1 year postoperatively) if reported. Pre- and postoperative KOOS and Tegner scores were available on 4865 of 14,806 patients (33%) and 3907 of 14,806 patients (26%), respectively. The distribution of revision surgery was estimated. We also compared poor outcome at 1-year follow-up with the risk of having a later revision surgery. As there is no consensus of how to define failure after ACL surgery, we defined failure as KOOS quality of life (QoL) score <44, Tegner score ≤2, positive pivot shift, or side-to-side difference of >2 mm.
Confounding Factors
We obtained data at the time of surgery from the DKRR on sex, cartilage injury (yes/no), operated meniscal injury (yes/no), prior surgery to the knee (yes/no), activity leading to primary ACL rupture (sport and other activities such as traffic, activity of daily living, and work), graft choice, and use of screw and washer as tibial fixation (yes/no).
Statistical Analysis
The median KOOS scores 1 year postoperative were calculated for the patients in each of the 4 age groups, and the difference was tested using the Kruskal-Wallis test and regression analysis. Normality was tested using qq-plots and histograms.
We conducted survival analysis using the Kaplan-Meier method to estimate the cumulative revision probability at different follow-up periods in the different age groups. We used Cox proportional regression analysis to compute the risk of revision surgery in groups A, B, and C, using group D (patients aged >20 years) as the reference group. Hence, we computed the hazard ratios as a measure for relative risk (RR) with 95% CI for patients in groups A, B, and C. We fit the model controlling for relevant confounders listed in Table 1. Multivariate analyses were used to adjust for relevant confounders. Baseline characteristics are presented as frequencies.
TABLE 1.
Patient Characteristics: Results From the DKRR (N = 14,806 Operated Knees Registered)a
| Group A (Patients Aged <13 y) | Group B (Patients Aged 13-15 y) | Group C (Patients Aged 15-20 y) | Group D (Patients Aged ≥20 y) | Total | |
|---|---|---|---|---|---|
| Total number | 95 | 327 | 2888 | 11,496 | 14,806 |
| Male patients | 53 (55.8) | 126 (38.5) | 1337 (46.3) | 7371 (64.1) | 8887 |
| Revision surgery | 3 (3.2) | 22 (6.7) | 140 (4.9) | 233 (2.0) | 398 |
| Hamstring graftb | 89 (93.7) | 280 (85.9) | 2355 (81.8) | 8952 (78.2) | 11,676 |
| Meniscal arthroscopic treatment performed (yes) | 19 (20) | 88 (26.9) | 1048 (36.3) | 4473 (38.9) | 5628 |
| Cartilage damage (yes/missing) | 8 (8.4) | 36 (11.0) | 333 (11.5) | 2685 (23.4) | 3062 |
| Tibial fixation, screw and washer (yes) | 46 (48.4) | 36 (11.0) | 11 (0.38) | 17 (0.15) | 110 |
| Patients with prior surgery to the kneec | 10 (10.6) | 45 (14.0) | 496 (17.3) | 3434 (30.1) | 3985 |
| Patients with sports activity leading to the ACL lesiond | 77 (81.1) | 294 (89.9) | 2598 (90.2) | 9038 (78.9) | 12,007 |
aValues are reported as n (%). ACL, anterior cruciate ligament; DKRR, Danish Knee Reconstruction Registry.
bSixty-three patients with missing data on graft registration in the DKRR.
cOne hundred thirteen missing variables in the DKRR.
dForty-five missing variables in the DKRR.
We used multiple imputations to examine the potential influence of missing values, generating 20 imputed data sets. The RRs were calculated as the average RRs of the 20 data sets, corrected for between- and within-imputation variation. The imputation model included all measured covariates in Table 1. In addition, we conducted a sensitivity analysis to examine the potential influence of missing values comparing results on RR estimates with and without multiple imputations. The assumption of the Cox regression model was assessed with use of log-log plots and Schoenfeld residuals and was found suitable.
All statistical analyses were computed using Stata, v 12 (Stata Corp). This study was approved by the Danish Data Protection agency.
Results
Patient characteristics in the 4 age groups are outlined in Table 1. Hamstring graft was used in 93.7% of the cases in group A, 85.9% in group B, and 81.8% in group C, compared with 78.2% of patients in group D. Bone–patellar tendon–bone graft was used in the remaining patients. No allograft was used as a primary graft. Females were predominant in group B (61.5%), and males in group D (64.1%). The frequency of associated cartilage damage seen at the time of ACL surgery increased with rising age, as well as with meniscal operation performed. Further, the fraction of patients having earlier knee surgery rose naturally with higher age.
Primary Outcomes
A statistically increased revision rate was seen in the younger age groups. Only a total of 3 revisions were registered in group A, which makes the statistics unreliable. However, in groups B and C, the revision rates were found to be 6.7 and 4.9, respectively, compared with 2.0 among patients in group D (Table 2). The adjusted RR risks of revision in the 3 age groups, using group D as reference, were 1.65 (95% CI, 0.47-5.79) for group A, 3.23 (95% CI, 2.05-5.08) for group B, and 2.50 (95% CI, 2.01-3.11) for group C (Table 2).
TABLE 2.
Primary Outcome Variables: Risk of Revision in Groups A-C Compared With Group D (Reference)a
| Group A (Patients Aged <13 y) | Group B (Patients Aged 13-15 y) | Group C (Patients Aged 15-20 y) | Group D (Patients Aged ≥20 y) | Total | |
|---|---|---|---|---|---|
| Total number | 95 | 327 | 2888 | 11,496 | 14,806 |
| Revision surgery, n (%) | 3 (3.2) | 22 (6.7) | 140 (4.9) | 233 (2.0) | 398 |
| Crude RR (95% CI) | 1.68 (0.54-5.25) | 3.48 (2.24-5.38) | 2.57 (2.09-3.18) | ||
| Adjusted RR (95% CI)b | 1.65 (0.47-5.79) | 3.23 (2.05-5.08) | 2.50 (2.01-3.11) |
aBolded values indicate statistical significance. RR, relative risk.
bAdjusted by sex, meniscal operation, cartilage damage, prior surgery to the injured knee, activity leading to anterior cruciate ligament lesion, graft choice, tibial fixation, and choice of placement of femoral tunnel.
The Kaplan-Meier cumulative revision rate after primary ACL reconstruction at 2 and 5 years for group A was 1.28% (95% CI, 0.18%-8.75%) and 7.42% (95% CI, 2.07%-2.48%), respectively; group B: 4.84% (95% CI, 2.84%-8.22%) and 10.36% (95% CI, 6.81%-15.59%), respectively; group C: 3.59% (95% CI, 2.89%-4.46%) and 8.39% (95% CI, 7.03%-10.00%), respectively; and group D: 1.58% (95% CI, 1.34%-1.86%) and 3.14% (95% CI, 2.74%-3.60%), respectively (Figure 1).
Figure 1.
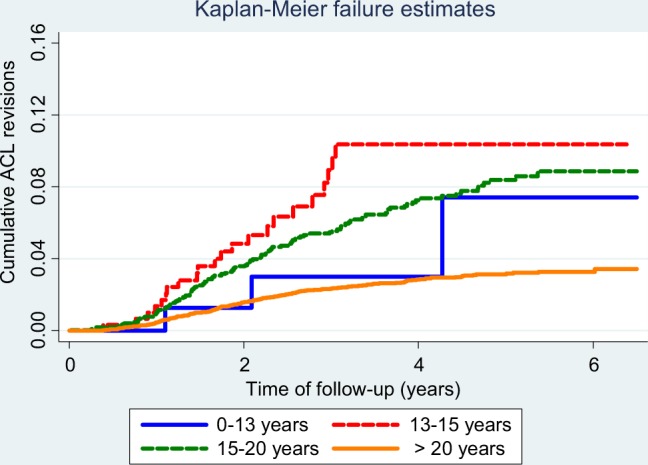
Kaplan-Meier cumulative revision curve of primary anterior cruciate ligament reconstructions in the 4 different age groups of the study.
Secondary Outcomes
No difference was found in positive pivot-shift test and side-to-side difference above 2 mm between the 4 groups (Table 3). The younger age groups showed significantly better KOOS and Tegner scores and had lower failure rates, defined as QoL ≤44 and Tegner ≤2 (Table 3). The older patients had a significantly worse KOOS4 score compared with the younger patients.
TABLE 3.
Secondary Outcome Variables: Data From 1-Year Follow-up (n = 6129 Operated Knees)
| Group A (Patients Aged <13 y) | Group B (Patients Aged 13-15 y) | Group C (Patients Aged 15-20 y) | Group D (Patients Aged ≥20 y) | Total | |
|---|---|---|---|---|---|
| KOOS QoL ≤44 | 6 (15.4) | 17 (20.2) | 166 (24.3) | 886 (28.6) | 1075 |
| Tegner ≤2 | 2 (5.1) | 3 (3.6) | 33 (4.8) | 296 (9.6) | 334 |
| Positive pivot-shift test | 6 (13.0) | 26 (16.6) | 228 (17.8) | 775 (16.7) | 1035 |
| Side-to-side difference >2 mm | 4 (8.7) | 20 (13.7) | 207 (17.5) | 665 (16.4) | 896 |
| KOOS4, mean (IQR) | 83.0 (68.8-93.1) | 80.0 (68.2-88.1) | 75.7 (64.2-85.0) | 72.0 (58.3-83.2) |
aValues are reported as n (%) unless otherwise indicated. IQR, interquartile range; KOOS QoL, Knee injury and Osteoarthritis Outcome Score quality of life subscore.
The primary reasons for graft failure in patients aged 13 to 15 years (group B) were new trauma (59%) and suboptimal graft placement in the femur (27%). In comparison, 36% of the patients were registered with new trauma, and 16% registered as suboptimal graft placement in the femur as reason for graft failure in patients older than 20 years (group D) (Table 4). Moreover, infections were registered as cause of graft failure in only 4.8% of revision cases in group D. In contrast, no patients younger than 15 years had infections registered as the reason for revision surgery.
TABLE 4.
Causes for Revision ACL Surgery in the 4 Age Groupsa
| Group A (Patients Aged <13 y) | Group B (Patients Aged 13-15 y) | Group C (Patients Aged 15-20 y) | Group D (Patients Aged ≥20 y) | Total | |
|---|---|---|---|---|---|
| New trauma | 0 (0) | 13 (59) | 65 (48) | 80 (36) | 160 (41) |
| Tunnel widening | 0 (0) | 0 (0) | 2 (1.5) | 6 (2.6) | 8 (2) |
| Suboptimal graft placement in tibia | 1 (50) | 0 (0) | 12 (8.9) | 19 (8.3) | 32 (8.2) |
| Suboptimal graft placement in femur | 0 (0) | 6 (27) | 16 (12) | 37 (16) | 59 (15.3) |
| Infection | 0 (0) | 0 (0) | 3 (2.2) | 11 (4.8) | 14 (3.6) |
| Unknown reason for instability | 0 (0) | 3 (14) | 24 (18) | 55 (24) | 82 (21) |
| Other ligament instability | 1 (50) | 0 (0) | 7 (5.2) | 11 (4.8) | 19 (4.9) |
| Other reason | 0 (0) | 0 (0) | 6 (4.4) | 7 (3.1) | 13 (3.4) |
| Total | 2 | 22 | 135 | 228 | 387 |
aValues are reported as n (%). ACL, anterior cruciate ligament.
Use of extracortical fixation or other fixation types or graft type was not found to be an indicator of more laxity or increased risk for revision surgery in the younger age groups.
Discussion
This is the first nationwide population-based cohort study describing a population of children and adolescents and their risk of ACL revision surgery as well as patient-reported outcome scores. A low revision rate is important not only because the patient is facing the risk associated with a troublesome revision surgery, but it has been shown that the subjective outcome score after revision ACL surgery is considerably lower than after primary reconstruction despite acceptable objective findings.13
We found an overall 5-year revision rate of 2.7%, which is comparable to other studies.1,18,24 Our study demonstrates that the ACL-reconstructed teenager is at higher risk for a subsequent revision ACL reconstruction.
We did not find an overall significant difference in revision rate between sexes, which is in accordance with the findings of Shelbourne et al,30 but in the 13- to 15-year age group, girls (61.5%) were more prone to have revision surgery compared with boys. This is in accordance with the results from the Swedish ACL registry, where a revision rate of 22% was found among teenage female soccer players.1
Due to small sample size (95 patients), the risk for revision estimated in patients younger than 13 years was uncertain. Thus, a larger cohort and longer follow-up are needed to evaluate this younger age group.
In a study of 98 ACL-reconstructed patients, Kamien et al12 found a failure rate of 15%. The true rate of graft failure is not detectable in this study as the register only includes performed operations and revision reconstructions. One must assume that the true incidence of failed grafts is somewhat higher than the revision rate seen in this study. However, comparing studies that have graft failure as their endpoint is difficult since there is no consensus of how to detect graft failure.
Extracortical graft fixation in the tibia (see Table 1) was used more frequently in the youngest age group. This fixation technique is chosen for younger patients to keep the epiphysis undisturbed by fixation devices. Using extracortical graft fixation in the tibia could result in more knee laxity in this group since extracortical fixation can result in more laxity compared with closer to joint fixations.8 However, we did not see increased objective knee laxity in the youngest age groups, despite the use of extracortical tibial fixation.
New trauma as a cause of graft failure was reported with a higher incidence in groups B (59%) and C (48%) compared with group D (36%). This is in accordance with prior studies reporting that an increased failure rate in younger patients is associated with postoperative return to sports.5,28,30
In our study, the revisions took place from 1 to 5 years after primary reconstruction in all age groups.18 Of note, the 2 teenage groups showed many revisions several years after primary surgery (Figure 1). This is in contrast to the theory that the high incidence of ACL graft rerupture among teenagers is caused by too early return to sports activities after surgery.
The primary cause for ACL revision was new trauma, but a secondary cause of malposition of the tunnels in either the femur or tibia was found in 1 of 4 revision cases, which is comparable to the findings of a recent French study.32
Our study does not explain the reason for the significantly greater reoperation rates seen in the 2 teenage groups. A possible explanation to the high rerupture rate could be the urging of teenage athletes to return as fast as possible to contact sports, but in our study the Kaplan-Meier curve reveals that a large proportion of the revisions took place much later than the first year (Figure 1).
Consequently, it is imperative that young patients eligible for primary ACL reconstruction receive proper counseling in terms of outcome expectancies. Counseling the young athlete and their family about this increased risk for rerupture is imperative.
Strengths and Limitations
Our study is based on data from a national clinical registry, and it therefore has several strengths and limitations. The fact that the DKRR is a large national database is an obvious strength from a data quality perspective. Moreover, owing to the unrestricted and free access to health care in Denmark, the DKRR provides an unselected study population. Also, the population-based design with a tax-supported health care system principally limits some aspects concerning selection bias, such as preference for surgical treatments.
However, data based on national clinical registries encounter several limitations. One problem is the completeness of the data and patients’ compliance with online subjective patient registrations. The completeness of operation registration in the database is higher than 85% for the past 3 years, which we consider as acceptable.25 Using ACL revision surgery as a failure outcome also has limitations. Some patients are not willing to undergo revision surgery and instead accept reduction in activity level and chronic knee instability. In other cases, surgeons do not find patients suitable for surgery despite a poor outcome. Thus, the revision surgery rate is a conservative measure for clinical failure after ACL reconstruction. Data completeness for the pre- and postoperative patient-related outcome scores could be a concern, which could lead to information bias if missing data on patient-related outcomes are related to both graft choices and later revision. Since the data collection is prospective and registration of primary ACL is independent of registration of later revision, the risk of information bias is very limited. A recent validity study has demonstrated no difference in patient-related outcome scores between responders and nonresponders in the DKRR.25 We included important confounders in the multivariate analysis, which have previously been associated with the risk of revision surgery. Although we adjusted for a number of potential confounding factors, our study, like all observational studies, may suffer from unmeasured and residual confounding such as missing data on sports activity level, smoking habits, and alcohol consumption, which are not available in the DKRR. There has been concern over whether transphyseal drilling in skeletal immature patients might cause growth disturbancy.11 This possible complication was not registered in this register study.
Conclusion
We have found that the revision rate in the 13- to 20-year-old ACL-reconstructed patient is up to 3.5 times greater than that of adult ACL-reconstructed patients. However, subjective outcome is better in the teenage group, and objective knee stability is comparable to adult patients. There is a need for further studies that elucidate causes for and prevention of ACL graft rerupture in children and adolescents.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register. A report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40:2230–2235. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF, Dome DC, Gautam S, Awh MH, Rennirt GW. Correlation of anthropometric measurements, strength, anterior cruciate ligament size and intercondylar notch characteristics to sex differences in anterior cruciate ligament tear rates. Am J Sports Med. 2001;29:58–66. [DOI] [PubMed] [Google Scholar]
- 3. Angel KR, Hall DJ. Anterior cruciate ligament injury in children and adolescents. Arthroscopy. 1989;5:197–200. [DOI] [PubMed] [Google Scholar]
- 4. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds have not returned by 12 months after surgery. Am J Sports Med. 2011;39:538–543. [DOI] [PubMed] [Google Scholar]
- 5. Borchers JR, Pedroza A, Kaeding C. Activity level and graft type as risk factors for anterior cruciate ligament graft failure: a case-control study. Am J Sports Med. 2009;37:2362–2367. [DOI] [PubMed] [Google Scholar]
- 6. Danish Health and Medicines Authority. Declaration on Approval of Nationwide and Regional Clinical Quality Databases [in Danish] Statutory Order 459. June 2006. [Google Scholar]
- 7. Dorizas JA, Stanitski CL. Anterior cruciate ligament injury in the skeletally immature. Orthop Clin North Am. 2003;34:355–363. [DOI] [PubMed] [Google Scholar]
- 8. Faunø P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005:21:1337–1341. [DOI] [PubMed] [Google Scholar]
- 9. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363:331–342. [DOI] [PubMed] [Google Scholar]
- 10. Gaulrapp HM, Haus J. Intraarticular stabilization after anterior cruciate ligament tear in children and adolescents: results 6 years after surgery. Knee Surg Sports Traumatol Arthrosc. 2006;14:417–424. [DOI] [PubMed] [Google Scholar]
- 11. Janarv PM, Wikstrom B, Hirsch G. The influence of transphyseal drilling and tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop. 1998;18:149–154. [PubMed] [Google Scholar]
- 12. Kamien PM, Hydrick JM, Replogle WH. Age, graft size and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41:1808–1812. [DOI] [PubMed] [Google Scholar]
- 13. Kannus P, Järvinen MJ. Knee ligament injuries in adolescents. Eight year follow-up of conservative management. J Bone Joint Surg Br. 1988;70:772–776. [DOI] [PubMed] [Google Scholar]
- 14. Kocher MS, Smith JT, Zoric BJ, Lee B, Michell LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89:2632–2639. [DOI] [PubMed] [Google Scholar]
- 15. Kopf S, Kauert R, Halfpaap J, Jung T, Becker R. A new quantitative method for pivot shift grading. Knee Surg Sports Traumatol Arthrosc. 2012;20:718–723. [DOI] [PubMed] [Google Scholar]
- 16. Kumar S, Ahearne D, Hunt DM. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature. J Bone Joint Surg Am. 2013;95:e1 (1-6). [DOI] [PubMed] [Google Scholar]
- 17. Lind M, Lund B, Faunø P, Said S, Miller LL, Christiansen SE. Medium to long-term follow-up after ACL revision. Knee Surg Sports Traumatol Arthrosc. 2012;20:166–172. [DOI] [PubMed] [Google Scholar]
- 18. Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epimediological follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17:117–124. [DOI] [PubMed] [Google Scholar]
- 19. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. [DOI] [PubMed] [Google Scholar]
- 20. Marx A, Siebold R, Sobau C, Saxler G, Ellermann A. ACL reconstruction in skeletally immature patients [in German]. Sportverletz Sportschaden. 2009;23:47–51. [DOI] [PubMed] [Google Scholar]
- 21. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18:955–959. [DOI] [PubMed] [Google Scholar]
- 22. Moksnes H, Engebretsen L, Risberg MA. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg Am. 2012;94:1112–1119. [DOI] [PubMed] [Google Scholar]
- 23. Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39 (suppl):22–25. [DOI] [PubMed] [Google Scholar]
- 24. Persson A, Fjeldsgaard K, Gjertsen JE, et al. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. [DOI] [PubMed] [Google Scholar]
- 25. Rahr-Wagner L, Thillemann TM, Lind MC, Pedersen AB. Validation of 14,500 operated knees registered in the Danish Knee Ligament Reconstruction Register: registration completeness and validity of key variables. Clin Epidemiol. 2013;22:219–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Redler LH, Brafman RT, Trentacosta N, Ahmad CS. Anterior cruciate ligament reconstruction in skeletally immature patients with transphyseal tunnels. Arthroscopy. 2012;28:1710–1717. [DOI] [PubMed] [Google Scholar]
- 27. Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:948–957. [DOI] [PubMed] [Google Scholar]
- 29. Shea KG, Pfeiffer R, Wang JH, Curtin M, Apel PJ. Anterior cruciate ligament injury in pediatric and adolescent soccer players: an analysis of insurance data. J Pediatr Orthop. 2004;24:623–628. [DOI] [PubMed] [Google Scholar]
- 30. Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after ACL reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251. [DOI] [PubMed] [Google Scholar]
- 31. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 32. Trojani C, Sbihi A, Djian P, et al. Causes for failure of ACL reconstruction and influence of mensicectomies after revision. Knee Surg Sports Traumatol Arthrosc. 2011;19:196–201. [DOI] [PubMed] [Google Scholar]


