Abstract
Background:
Presently, the treatment options available for patients with horizontal degenerative cleavage tears of the meniscus are limited. These tears are considered an indication for partial or subtotal meniscectomy because when the tear is located within an avascular area, it is difficult to induce healing. However, meniscectomy is not ideal because it disrupts the normal anatomical structure and function of the meniscus.
Purpose:
To examine the clinical and arthroscopic outcomes following meniscal repair of degenerative horizontal cleavage tears using fibrin clots.
Study Design:
Case series; Level of evidence, 4.
Methods:
Vertical sutures were placed in the meniscal tear, and the cleft was filled with fibrin clots before the sutures were tightened. We repaired 18 menisci in 18 consecutive eligible patients using a previously described technique. Three patients with anterior cruciate ligament (ACL) injury who underwent simultaneous ACL reconstruction and 5 patients who did not undergo follow-up arthroscopy within 12 months were excluded. The remaining 10 menisci in 10 patients were evaluated in this study. The mean age of the patients was 35.8 ± 16.5 years, and the mean postoperative follow-up time was 40.8 ± 5.4 months. Pre- and postoperative Lysholm scores, International Knee Documentation Committee (IKDC) subjective scores, and Tegner activity levels were compared. The arthroscopy findings were evaluated at a mean postoperative time of 6.7 ± 2.9 months.
Results:
The mean Lysholm score improved significantly from 69.3 ± 16.3 points preoperatively to 95.4 ± 3.6 points postoperatively (P < .005). The mean IKDC subjective score also improved significantly from 26.5% ± 19.0% preoperatively to 87.8% ± 7.5% postoperatively (P < .001). The Tegner activity level recovered to the preinjury level in 6 patients and to 1 level below the preinjury level in 4 patients. The follow-up arthroscopies showed complete healing in 7 patients (70%) and incomplete healing in 3 patients (30%).
Conclusion:
Meniscal repair of degenerative horizontal cleavage tears using fibrin clots resulted in improved Lysholm and IKDC subjective scores, but the complete healing rate on follow-up arthroscopy was only 70%.
Clinical Relevance:
If we are to prevent osteoarthritis, we should minimize resection and restore the contact area of the meniscus to preserve the original shape.
Keywords: meniscus, meniscal repair, horizontal cleavage tear, degenerative tear, fibrin clot
Horizontal cleavage tears of the meniscus are common in older patients, athletes, patients with parameniscal cysts, and patients with discoid menisci.5,7,8,20,22 Although they sometimes occur during the early stages of osteoarthritis, most tears are asymptomatic. The treatment of symptomatic tears is controversial.7 If the tear is associated with degenerative changes, conservative treatments, such as physical therapy or hyaluronic acid injection, may be used first. A horizontal cleavage tear of the meniscus is considered to be an indication for partial or subtotal meniscectomy because when the tear is located within a large avascular area, it is usually difficult to induce healing of the pathological changes associated with degeneration.5,7,8 A number of meniscectomy techniques for the treatment of horizontal cleavage tears have been described.18 However, preservation of the thickness and width of the meniscal rim in accordance with its original shape is desirable to retain meniscal function and reduce the risk of osteoarthritis. Meniscal repair is therefore preferable to meniscectomy, particularly in patients who wish to return to a high level of activity.2,3,8,11,20,26,33 The application of fibrin clots can augment repair and promote healing of the meniscus.1,27,31,32 Both animal models and human studies have shown that the platelets in fibrin clots contain growth factors, which promote cellular infiltration and healing.1,13,14,32
We hypothesized that fibrin clots promote the healing of horizontal cleavage tears that include widespread degenerative changes in the avascular zone. To test this, we performed meniscal repair of horizontal cleavage tears associated with degeneration of the meniscus using fibrin clots. The purpose of this study was to examine the clinical and arthroscopic outcomes of this technique.
Methods
Informed consent was obtained from all patients, and the study protocol was approved by the local institutional review board. All surgical procedures were performed at a single surgical center by a single surgeon. The inclusion criterion of this study was symptomatic meniscal degeneration without instability. Patients were included if they had a horizontal cleavage tear associated with degeneration identified using magnetic resonance imaging (MRI) and arthroscopy; clinical findings limited to a positive McMurray test or pain during movement, especially in full flexion; tenderness of the femorotibial joint line; and no limitation of range of motion. The exclusion criteria of this study were advanced osteoarthritis and a history of additional surgical procedures augmenting the meniscal tear, such as microfracture surgery. We considered simultaneous anterior cruciate ligament (ACL) reconstruction as an augmentation because of the bone tunnel drilling. Patients were excluded if standing radiographs showed advanced osteoarthritis of the knee (Kellgren-Lawrence17 grade 3 or 4) and/or an associated ligament instability. We prospectively repaired 18 menisci in 18 consecutive eligible patients, using a previously described technique.16 Three patients with ACL injury who underwent simultaneous ACL reconstruction and 5 patients who did not undergo follow-up arthroscopy within 12 months were excluded. The remaining 10 menisci in 10 patients were evaluated in this study, which included 6 men and 4 women with a mean age of 35.8 ± 16.5 years (range, 15-63 years) at the time of surgery. We initially divided the 10 menisci into 3 groups according to the tear location. The torn menisci included 4 medial menisci (MM), 3 lateral menisci (LM), and 3 discoid lateral menisci (DLM) (Table 1). The mean time between injury and surgery was 5.6 ± 3.1 months. The mean femorotibial angle (FTA) was 176.7° ± 3.3° (range, 173°-183°) and the mean body mass index (BMI) was 25.5 ± 3.6 kg/m2 (range, 20.0-31.2 kg/m2) at the time of surgery. The mean postoperative follow-up time was 40.8 ± 5.4 months (range, 32.5-51.3 months).
TABLE 1.
Clinical Characteristics of Patients by Tear Locationa
| Medial Meniscus (n = 4) | Lateral Meniscus (n = 3) | Discoid Lateral Meniscus (n = 3) | |
|---|---|---|---|
| Age, y, mean ± SD (range) | 52.8 ± 6.2 (47-63) | 32.0 ± 10.0 (18-41) | 17.0 ± 2.8 (15–21) |
| Sex, n, male/female | 3/1 | 1/2 | 1/2 |
| Injury-to-surgery time, mo, mean ± SD (range) | 4.5 ± 1.5 (3-6) | 8.7 ± 3.4 (4-12) | 4.0 ± 0.8 (3-5) |
| Preoperative Lysholm score, points, mean ± SD (range) | 70.8 ± 8.6 (61-82) | 59.0 ± 30.5 (24-80) | 77.7 ± 5.5 (72-83) |
| Postoperative Lysholm score, points, mean ± SD (range) | 92.0 ± 2.3 (92-96) | 98.3 ± 2.4 (95-100) | 97.0 ± 2.2 (95-100) |
| Preoperative IKDC score, %, mean ± SD (range) | 16.1 ± 9.5 (9.2-29.9) | 38.3 ± 24.0 (5.7-63.2) | 28.7 ± 18.9 (17.2-50.6) |
| Postoperative IKDC score, %, mean ± SD (range) | 81.0 ± 4.0 (77-87.3) | 89.7 ± 3.5 (86.2-94.5) | 95.0 ± 6.2 (86.2-100.0) |
| Surrounding cartilage condition, Outerbridge classification (grade 0/1/2/3) | 0/2/1/1 | 0/1/2/0 | 0/3/0/0 |
aIKDC, International Knee Documentation Committee.
Surgical Technique
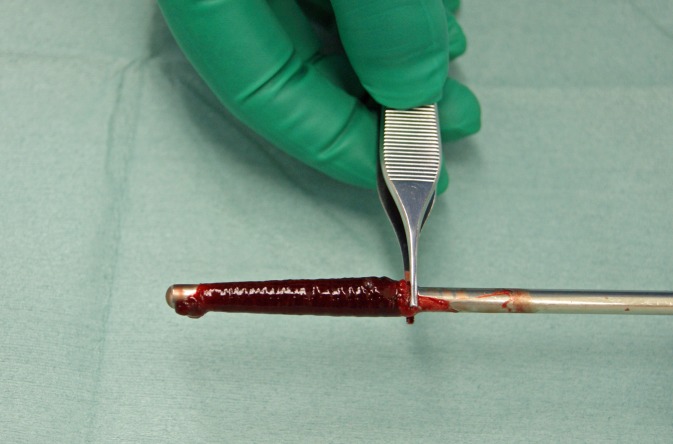
We collected 25 to 30 mL of blood from the patient in a sterile glass syringe and stirred it for 10 minutes with a stainless steel swizzle stick. Elastic fibrin clots precipitated on the stick in a tubular fashion (Figure 1) and were cut into lengths of approximately 5 mm.
Figure 1.
Preparation of fibrin clots. A swizzle stick was stirred in blood collected from the patient, and elastic fibrin clots precipitated on the stick in a tubular fashion.
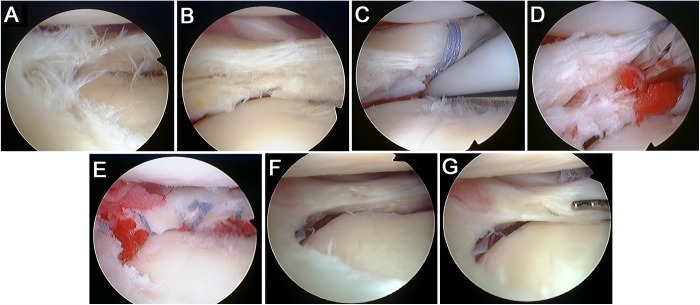
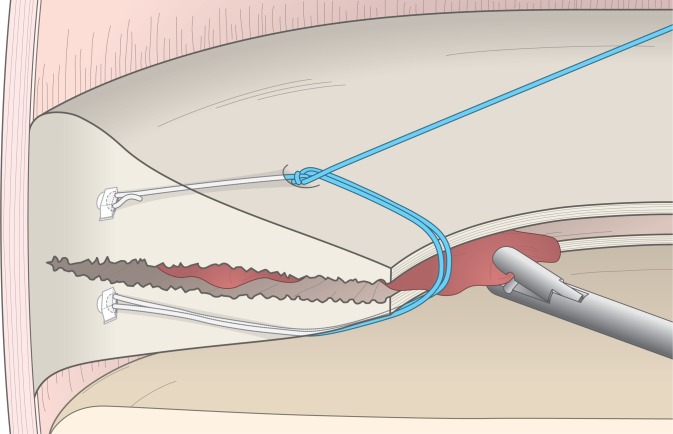
Diagnostic arthroscopy was performed before surgery. The meniscus was abraded with a basket punch and shaver to expose the margins of the tear (Figure 2, A and B). In the 3 patients with a discoid lateral meniscus, we first performed meniscectomy and saucerization and then repaired the horizontal cleavage tear in the remaining meniscus. We used an all-inside device to repair the posterior horn and place vertical sutures that closed the cleft of the tear (FAST-FIX; Smith & Nephew Endoscopy). Tears extending from the posterior to anterior horn were repaired using FAST-FIX combined with an inside-out or outside-in technique with 2-0 braided nylon sutures because FAST-FIX is designed for easy repair of the posterior segment. The all-inside device needle was inserted from the proximal side with the first anchor, and the second anchor was placed in the distal side across the horizontal cleavage tear (Figure 2C). We inserted fibrin clots into the cleft using a rongeur or grasper, placing the clots between the suture strands to ensure that they were secured within the cleft. We then tightened the sutures and completed the repair in a sandwich fashion (Figures 2, D and E, and 3).
Figure 2.
A 37-year-old female patient presented with a 1-month history of pain and repeated effusion in her right knee. Her preoperative Lysholm score was 24 points and International Knee Documentation Committee (IKDC) subjective score was 5.7%. Her Tegner activity level was 4 before injury and 0 before surgery. (A) Arthroscopy revealed a frayed lateral meniscus with degenerative changes. (B) There was an extensive horizontal cleavage tear at the posterior third of the meniscus, which reached the peripheral margins after the fibrillation had been abraded. (C) FAST-FIX was used to place vertical sutures to close the cleft of the tear. (D, E) Fibrin clots were inserted into the cleft before tightening the sutures and completed the repair in a sandwich fashion. (F) Follow-up arthroscopy at 6 months postoperatively. The cleft of the horizontal cleavage tear had closed and healed, and there was regenerated tissue on the lateral meniscus. (G) Probing confirmed that the suture knots had migrated into the regenerated scar tissue and that the repaired horizontal cleavage tear was well healed. The Lysholm score was 100 points, IKDC subjective score was 94.5%, and Tegner activity level was 4 at the time of follow-up arthroscopy. These improved scores were maintained at the final follow-up at 42 months postoperatively. This case was part of the complete healing group.
Figure 3.
Schematic diagram of the repair technique. The exogenous fibrin clot was inserted via the same portal as the FAST-FIX and placed in the cleft of the tear using a hand instrument such as a rongeur or a grasper. The cleft was then closed by tightening the sutures.
We applied an extension brace or cast to the knee and restricted patients to limited flexion with no weightbearing for 4 weeks postoperatively. We then permitted weightbearing as tolerated and began physical therapy. We permitted a return to moderate activities such as jogging at 4 to 5 months postoperatively. Follow-up arthroscopy was performed in all patients at approximately 6 months postoperatively, and higher levels of activity, including playing sports, were permitted after the follow-up arthroscopy.
Clinical Evaluation
We performed clinical evaluation using the Lysholm score,30 International Knee Documentation Committee (IKDC) subjective score,12 and Tegner activity scale30 before surgery and at the final follow-up, and we analyzed differences between these 2 time points using Student t tests. We also compared the arthroscopy findings at approximately 6 months postoperatively, as the outcome measure of the repair, with the results of clinical evaluations at the time of the final follow-up.
Follow-up Arthroscopy
Arthroscopic findings were divided into 2 groups by the second author according to their pattern of healing: a complete healing group with closure of the cleft and a layer of vascular synovial tissue extending over the proximal and/or distal surface of the meniscus (Figure 2, F and G) and an incomplete healing group with only partial closure of the cleft (Figure 4).
Figure 4.
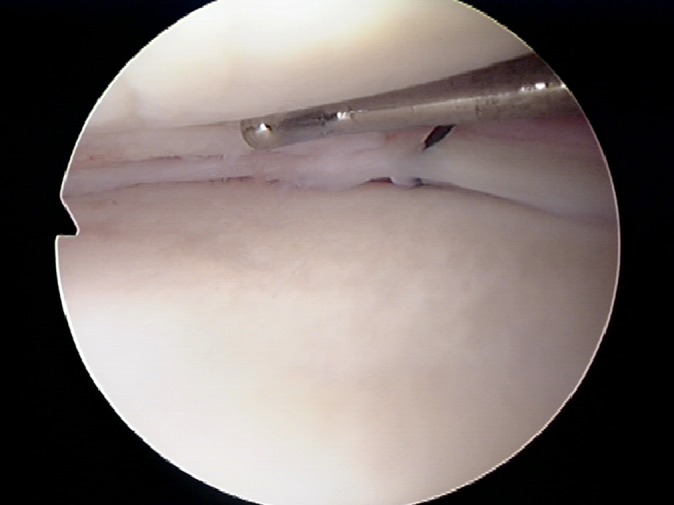
Follow-up arthroscopy findings of the incomplete healing group.
Statistical Analysis
Differences between the pre- and postoperative results were assessed using the Student t test, with P values <.05 considered to be statistically significant.
Results
The Lysholm and IKDC subjective scores improved in all patients postoperatively. The mean Lysholm score improved significantly from 69.3 ± 16.3 points (range, 24-83 points) preoperatively to 95.4 ± 3.6 points (range, 90-100 points) postoperatively (P < .005), and the mean IKDC subjective score improved significantly from 26.5% ± 19.0% (range, 5.7%-63.2%) preoperatively to 87.8% ± 7.5% (range, 77%-100%) postoperatively (P < .001). The postoperative Tegner activity level recovered to the preinjury level in 6 patients and to 1 level below the preinjury level in 4 patients.
The clinical characteristics of the patients, including tear location, are shown in Table 1. The mean FTA was 179.0° ± 4.1° (range, 175°-182°) in the MM group, 174. 0° ± 1.7° (range, 173°-176°) in the LM group, and 176.3° ± 2.3° (range, 175°-179°) in the DLM group. The mean BMI was 25.3 ± 3.7 kg/m2 (range, 21.5-30.3 kg/m2) in the MM group, 25.5 ± 5.4 kg/m2 (range, 20.4-31.2 kg/m2) in the LM group, and 25.9 ± 5.3 kg/m2 (range, 20.0-30.0 kg/m2) in the DLM group.
The mean age and FTA were highest in the MM group, and the mean age and time between injury and surgery were lowest in the DLM group. The preoperative Lysholm score was lowest and the postoperative score was highest in the LM group. The preoperative IKDC score was lowest in the MM group, and the postoperative score was highest in the DLM group.
The condition of the surrounding cartilage in the involved compartment at the time of surgery was evaluated with the Outerbridge classification.23 No cases with grade 0 or 4 were found. Six cases were grade 1, 3 cases were grade 2, and 1 case was grade 3. The MM group included 2 cases of grade 1, 1 case of grade 2, and 1 case of grade 3. The LM group included 1 case of grade 1 and 2 cases of grade 2. All cases in the DLM group were grade 1.
To summarize the tendency among these 3 groups, the order of groups by increasing age and decreasing postoperative IKDC scores was DLM, LM, and MM. Additionally, the cartilage condition in all cases in the DLM group was grade 1. However, the time between injury and surgery and the preoperative Lysholm scores were lowest in the LM group.
Follow-up arthroscopy was performed at 6.7 ± 2.9 months (range, 5.3-7.5 months) postoperatively. We did not observe failure of healing or advanced degeneration in any patients. The follow-up arthroscopy showed that complete healing had occurred in 7 patients (70%) and incomplete healing had occurred in 3 patients (30%). The characteristics of these groups are shown in Table 2. The complete healing group included 2 MM tears, 2 LM tears, and 3 DLM tears. In this group, the mean age of the patients was 29.6 ± 16.2 years (range, 15-52 years), mean FTA was 176.7° ± 3.0° (range, 173°-182°), and mean preoperative BMI was 25.2 ± 4.3 kg/m2 (range, 20.0-31.2 kg/m2). The Lysholm score improved from 66.9 ± 20.3 points (range, 24-83 points) preoperatively to 96 ± 4.3 points (range, 90-100 points) postoperatively, and the IKDC subjective score improved from 25.4% ± 17.4% (range, 5.7%-50.6%) preoperatively to 91.0% ± 6.9% (range, 81.6%-100.0%) postoperatively. The surrounding cartilage condition at the time of surgery was grade 1 in 6 cases and grade 3 in 1 case.
TABLE 2.
Clinical Characteristics of Patients With Complete and Incomplete Healinga
| Complete Healing (n = 7) | Incomplete Healing (n = 3) | P Value | |
|---|---|---|---|
| Age, y, mean ± SD (range) | 29.6 ± 16.2 (15-52) | 50.3 ± 11.4 (41-63) | .03 |
| Sex, n, male/female | 3/4 | 3/0 | |
| Tear location, MM/LM/DLM | 2/2/3 | 2/1/0 | |
| Postoperative Lysholm score, points, mean ± SD (range) | 96 ± 4.3 (90-100) | 94 ± 2.2 (91-96) | .20 |
| Postoperative IKDC score, %, mean ± SD (range) | 91.0 ± 6.9 (81.6-100.0) | 80.5 ± 5.0 (77-86.2) | .02 |
| Surrounding cartilage condition, Outerbridge classification (grade 0/1/2/3) | 0/6/0/1 | 0/1/2/0 |
aDLM, discoid lateral meniscus; IKDC, International Knee Documentation Committee; LM, lateral meniscus; MM, medial meniscus.
The incomplete healing group included 2 medial meniscus tears and 1 lateral meniscus tear. All 3 patients were men. The mean age of the patients was 50.3 ± 11.4 years, mean FTA was 176.7° ± 3.9° (range, 173°-182°), and mean BMI was 26.4 ± 3.4 kg/m2 (range, 23.9-30.3 kg/m2). The Lysholm score improved from 75.0 ± 5.1 points (range, 70-82 points) preoperatively to 94.0 ± 2.2 points (range, 91-96 points) postoperatively, and the IKDC subjective score improved from 29.1% ± 29.7% (range, 9.2%-63.2%) preoperatively to 80.5% ± 5.0% (range, 77.0%-86.2%) postoperatively. The surrounding cartilage condition at the time of surgery was grade 1 in 1 case and grade 2 in 2 cases.
Comparisons between the complete and incomplete healing groups showed that the mean age was higher in the incomplete healing group (P = .03), and all 3 cases were men.
There were no significant differences in FTA (P = .99) or BMI (P = .66) between the 2 groups. The postoperative IKDC subjective score tended to be lower in the incomplete healing group, and those 3 cases had mild degenerative changes in the cartilage with Outerbridge grades of 1 or 2 (Table 2).
Complications
There were no complications in this series that influenced symptoms. However, the FAST-FIX implant was removed at the follow-up arthroscopy in 1 patient with complete healing because it had moved from its original placement adjacent to the synovial capsule. This movement had not disturbed the cartilage.
Discussion
The main functions of the menisci are the distribution and transmission of load across the knee joint. The menisci act as secondary stabilizers and provide proprioceptive feedback for sensing joint position, which in return prevents meniscal injuries.3,15,28
The basic science of conventional meniscal repair is based on the experimental studies of Arnoczky et al1 and Webber et al.32 Meniscal tears located in the vascular areas termed the red-red zone and red-white zone are indications for meniscal repair because the healing potential of the meniscus depends on its vascularity. However, tears in the avascular area (white-white zone) are not indications for meniscal repair but are instead good indications for meniscectomy.
Horizontal cleavage tears of the meniscus are extensive tears from the avascular zone to the vascular zone. They are common in middle-aged individuals as a part of degenerative meniscal tears.5,7,8
Most degenerative tears occur in the posterior horns, which play an important role in shock absorption and load transmission during knee flexion, especially in the medial meniscus, which acts as a stabilizer.
Treatment of degenerative meniscal tears is controversial. There are some reports in the literature that arthroscopic evaluation of the degenerative menisci is associated with chondral lesions during early osteoarthritis.5,7 It is therefore difficult to determine the usefulness of surgical treatment for such tears, which occur spontaneously in most cases.
Aggressive treatment is not indicated for lesions because of aging and repetitive microtrauma, which are associated with pathological changes to the meniscal tissue.5,7
It is generally preferable to perform a partial meniscectomy for degenerative horizontal cleavage tears because these tears tend to extend into the avascular area of the meniscus and have a lower healing potential than acute traumatic tears.4 However, clinical deterioration often occurs after partial meniscectomy, and it is therefore of questionable value for patients in their 30s and 40s who want to continue sports activities.26,33 The amount of meniscus removed correlates with the increase in joint contact stress,2,10,11,20 and partial meniscectomy of posterior horn tears tends to have the worst outcomes.11
Several techniques used to preserve the width of the meniscus during partial meniscectomy for horizontal cleavage tears have been published, such as single-leaf resection.18 However, Haemer et al10 reported that single-leaf resection restricted to the posterior third of the meniscus decreased the contact area by 40%, and that there was no significant difference in peak contact pressure between single-leaf and double-leaf resection. To prevent osteoarthritis, we should minimize resections and restore the contact area of the meniscus to preserve the original anatomical shape and function (“meniscal preservation”). Both the width and thickness should be preserved, especially at the peripheral rim, even if there are signs of degeneration.
The indication for meniscal repair depends on the tear type, location, length, chronicity, and level of degeneration.29 The current literature that definitively supports the repair of horizontal cleavage tears of the meniscus is limited. In 2012, Pujol et al24 described good results after open repair of horizontal tears. Additional biological innovations and procedures were recently reported for meniscal repair, including repair of tears in the avascular zone.19,22,25,29
The application of fibrin clots can augment repair and promote healing of the meniscus.1,27,31,32 Both animal models and human studies have shown that the platelets in fibrin clots contain growth factors, which promote cellular infiltration and healing.1,13,14,31 The clots are also believed to act as a scaffold during the process of meniscal healing. Recently, Ra et al25 reported good clinical repair results for complete radial tears of the meniscus evaluated with MRI and second look arthroscopy.
Other clinical applications that augment meniscal repair and promote healing include microfracture of the intercondylar notch, synovial flaps, and platelet-rich plasma.29 We chose to use fibrin clots because of the simplicity of the procedure, which allows for easy control of the grafting amount as needed for each case based on the extent of horizontal cleavage.
When the tears are symptomatic, treatment should focus on preservation and repair when possible. We previously reported a technique for repairing degenerative horizontal cleavage tears using fibrin clots, and the present study follows up on that report.16
The tear locations in our 10 cases are shown in Table 1. The patient age of the MM tear group tended to be older (52.8 ± 6.2 years), and the postoperative Lysholm and IKDC scores were lowest. The cartilage conditions were dispersed among grades 1 through 3, and the FTA was higher than in the other 2 groups (179.0° ± 4.1° vs 174.0° ± 1.7° and 176.3° ± 2.3°). The MM group results may be related to the early osteoarthritis with varus deformity. In the LM group, the mean age was in the middle (32.0 ± 10.0 years), and the time between injury and surgery was the longest among the 3 groups.
The DLM group was the youngest (17.0 ± 2.8 years), had shorter times between injury and surgery, and the postoperative Lysholm and IKDC scores were highest. All cases in that group showed cartilage conditions of grade 1. The DLM tears were involved within the meniscal tissue, which appeared after saucerization. This supports the idea of a greater healing potential in younger patients and that remnants of the meniscal tissues after saucerization are abundant for repair. However, DLM tears are well known to have histological abnormalities. Cui and Min6 showed that the collagen fibers run parallel to the periphery of the meniscus, which is ideal for resisting hoop stresses. We suggest that it is valuable both anatomically and functionally to maintain the peripheral rim, even when there is a preexisting congenital meniscal anomaly.
To summarize the characteristics of tears according to location, the order of groups by increasing age and decreasing IKDC scores was DLM, LM, and MM. Additionally, the cartilage condition in all cases in the DLM group was grade 1. However, the time between injury and surgery and the preoperative Lysholm scores were lowest in the LM group.
We believe that this tendency for increasing age and lower scores is caused by aging-related pathological changes to the knee joint that affect the cartilage condition. Particularly in the MM group, varus deformity may have influenced the results as that group had higher FTA than did the other 2 groups.
A recent study reported by Espejo-Reina et al9 concluded that chronic bucket-handle tears of the MM in patients <45 years of age showed an 83% complete healing rate. Our study showed similar results for chronic tears; however, our healing rate was lower than that of vertical tears. We suggest that age-related pathological changes leading to the lower healing potential and horizontal cleavage tears of the meniscus should be assessed as a part of joint degeneration and/or early osteoarthritis.
Mesiha et al21 found that age was significantly associated with the cellularity of a torn meniscus, with patients aged >40 years having significantly fewer cells than younger patients. This might result in menisci being more vulnerable to degeneration in older individuals.
In patients who had undergone meniscal repair using our technique in the present study, follow-up arthroscopy showed a vascular layer on the regenerated meniscus in both the complete and incomplete healing groups. There was no significant difference in the mean postoperative Lysholm score between the complete and incomplete healing groups. Additional comparisons between the complete and incomplete healing groups showed that the mean age was higher in the incomplete healing group and that all 3 cases were men. There were no significant differences in FTA (P = .99) or BMI (P = .66) between the 2 groups. Conversely, there was a significant difference in the mean postoperative IKDC subjective score (91.0% vs 80.5%; P = .039). The differences in patient characteristics between the complete and incomplete healing groups that may have influenced the results include the mean patient age (29.6 vs 50.3 years), all 3 patients in the incomplete healing group being men, and 2 patients in the incomplete healing group being smokers. Contrary to our expectations, the DLM tears healed well.
Even though it is challenging to induce healing in these cases, we believe that meniscal repair is a better primary surgical treatment for horizontal cleavage tears than extensive meniscectomy. However, because there was no control group in this study, we could not determine conclusively that this procedure produces better results than other possible procedures.
We believe that our technique is effective for the treatment of stable knees, though the outcomes depend on age as for conventional meniscal repair.4,21 Despite these promising results, it remains unclear whether menisci repaired using our technique can withstand shear stress. We therefore cannot generalize the usefulness of this technique at present.
The major limitation of this study is the lack of a control group for comparison. It would be valuable to compare patients who underwent repair using fibrin clots with patients who underwent partial meniscectomy, suture repair without fibrin clots, or no treatment. The study is also limited by the small number of patients who met the inclusion criteria, the lack of pathological and MRI diagnoses, the relatively short follow-up period, the wide age range of the patients, and the inclusion of patients with discoid menisci. However, the short-term clinical results are encouraging, and this technique could be considered as a treatment option for young and middle-aged patients who wish to return to sports activities. We speculate that the reason why most of our patients had good clinical results, including those with incomplete healing, is that the preservation of the meniscal tissue contributes to nutrition and lubrication of the adjacent meniscus and the knee joint. We did not determine the extent to which these factors may be influenced by growth factors in the fibrin clots. Further research is needed to determine the specific indications and optimal candidates for this procedure.
Conclusion
We suggest that the meniscal repair procedure described in this article could be considered as a treatment option for patients with a degenerative horizontal cleavage tear, especially younger patients with a stable knee.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Arnoczky SP, Warren RF, Spivak JM. Meniscal repair using an exogenous fibrin clot. An experimental study in dogs. J Bone Joint Surg Am. 1988;70:1209–1217. [PubMed] [Google Scholar]
- 2. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14:271–275. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92:1398–1408. [DOI] [PubMed] [Google Scholar]
- 4. Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176–181. [DOI] [PubMed] [Google Scholar]
- 5. Christoforakis J, Pradhan R, Sanchez-Ballester J, Hunt N, Strachan RK. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy. 2005;21:1366–1369. [DOI] [PubMed] [Google Scholar]
- 6. Cui JH, Min BH. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy. 2007;23:635–641. [DOI] [PubMed] [Google Scholar]
- 7. Englund M. The role of the meniscus in osteoarthritis genesis. Rheum Dis Clin North Am. 2008;34:573–579. [DOI] [PubMed] [Google Scholar]
- 8. Englud M, Roos EM, Roos HP, Lohmander LS. Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology. 2001;40:631–639. [DOI] [PubMed] [Google Scholar]
- 9. Espejo-Reina A, Sarrano-Fernández JM, Martin-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30:492–496. [DOI] [PubMed] [Google Scholar]
- 10. Haemer JM, Wang MJ, Carter DR, Giori NJ. Benefit of single-leaf resection for horizontal meniscus tear. Clin Orthop Relat Res. 2007;457:194–202. [DOI] [PubMed] [Google Scholar]
- 11. Hede A, Larsen E, Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16:122–125. [DOI] [PubMed] [Google Scholar]
- 12. Hefti F, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. [DOI] [PubMed] [Google Scholar]
- 13. Henning CE, Lynch MA, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA. Arthroscopic meniscal repair using an exogenous fibrin clot. Clin Orthop Relat Res. 1990;252:64–72. [PubMed] [Google Scholar]
- 14. Henning CE, Yearout KM, Vequist SW, Stallbaumer RJ, Decker KA. Use of the fascia sheath coverage and exogenous fibrin clot in the treatment of complex meniscal tears. Am J Sports Med. 1991;19:626–631. [DOI] [PubMed] [Google Scholar]
- 15. Hsieh HH, Walker PS. Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am. 1976;58:87–93. [PubMed] [Google Scholar]
- 16. Kamimura T, Kimura M. Repair of horizontal meniscal cleavage tears with exogenous fibrin clots. Knee Surg Sports Traumatol Arthrosc. 2011;19:1154–1157. [DOI] [PubMed] [Google Scholar]
- 17. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim JM, Bin SI, Kim E. Inframeniscal portal for horizontal tears of the meniscus. Arthroscopy. 2009;25:269–273. [DOI] [PubMed] [Google Scholar]
- 19. Kopf S, Birkenfeld F, Becker R, et al. Local treatment of meniscal lesions with vascular endothelial growth factor. J Bone Joint Surg Am. 2010;92:2682–2691. [DOI] [PubMed] [Google Scholar]
- 20. McDermott ID, Amis AA. The consequences of meniscectomy. J Bone Joint Surg Br. 2006;88:1549–1556. [DOI] [PubMed] [Google Scholar]
- 21. Mesiha M, Zurakowski D, Soriano J, Nielson JH, Zarins B, Murray MM. Pathologic characteristics of the torn human meniscus. Am J Sports Med. 2007;35:103–112. [DOI] [PubMed] [Google Scholar]
- 22. Narita A, Takahara M, Sato D, et al. Biodegradable gelatin hydorogels incorporating fibroblast growth factor 2 promote healing of horizontal tears in rabbit meniscus. Arthroscopy. 2012;28:255–263. [DOI] [PubMed] [Google Scholar]
- 23. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. [DOI] [PubMed] [Google Scholar]
- 24. Pujol N, Bohu Y, Bisrenoult P, Macdes A, Beaufils P. Clinical outcomes of open meniscal repair of horizontal meniscal tears in young patients. Knee Surg Sports Traumatol Arthrosc. 2013;27:1530–1533. [DOI] [PubMed] [Google Scholar]
- 25. Ra HJ, Ha JK, Jang SH, Lee DW, Kim JG. Arthroscopic inside-out repair of complete radial tears of the meniscus with fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013;21:2126–2130. [DOI] [PubMed] [Google Scholar]
- 26. Schimmer RC, Brülhart KB, Duff C, Glinz W. Arthroscopic partial meniscectomy: a 12-year follow up and two-step evaluation of the long-term course. Arthroscopy. 1998;14:136–142. [DOI] [PubMed] [Google Scholar]
- 27. Sethi PM, Cooper A, Jokl P. Technical tips in orthopaedics: meniscal repair with use of an in situ fibrin clot. Arthroscopy. 2003;19:E44. [DOI] [PubMed] [Google Scholar]
- 28. Slauterbeck JR, Kousa P, Clifton BC, et al. Geographic mapping of meniscus and cartilage lesions associated with anterior cruciate ligament injuries. J Bone Joint Surg Am. 2009;91:2094–2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Taylor SA, Rodeo SA. Augmentation techniques for isolated meniscal tears. Curr Rev Musculoskelet Med. 2013;6:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tegner Y, Lysholm J. Rating systems in evaluation of knee ligament injuries. Clin Orthop. 1985;198:43–49. [PubMed] [Google Scholar]
- 31. van Trommel MF, Simonian PT, Potter HG, Wickiewicz TL. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy. 1998;14:360–365. [DOI] [PubMed] [Google Scholar]
- 32. Webber RJ, York JL, Vanderschilden JL, Hough AJ., Jr An organ culture model for assaying wound repair of the fibrocartilaginous knee joint meniscus. Am J Sports Med. 1989;17:393–400. [DOI] [PubMed] [Google Scholar]
- 33. Yocum LA, Kerlan RK, Jobe FW, et al. Isolated lateral meniscectomy. A study of twenty-six patients with isolated tears. J Bone Joint Surg Am. 1979;61:338–342. [PubMed] [Google Scholar]