Abstract
Background:
Plantar fasciitis is a common cause of foot pain, and although many episodes are self-limiting with short duration, 10% leave chronic symptoms. Recalcitrant cases can be managed surgically, with studies demonstrating good results in the short term but uncertainties over longer term outcomes.
Purpose:
To assess the outcome following surgical intervention for patients with plantar fasciitis.
Study Design:
Case series; Level of evidence, 4.
Methods:
Seventy-nine patients were identified from operative diaries undergoing plantar fasciotomy surgery between 1993 and 2009. They were contacted to investigate long-term results using self-reported outcome measures.
Results:
Sixty-eight responses were received (86% response rate), with an average of 7 years (range, 1-15 years) of follow-up. Patients reported an average reduction in pain by visual analog scale of 79%, and 84% of patients were happy with the surgical results. Greater success was achieved in patients with shorter duration of symptoms preoperatively. No deterioration in success was seen over time.
Conclusion:
Plantar fasciotomy surgery for plantar fasciitis remains controversial, with biomechanical arguments against surgery; however, this article reports good success following surgery over a long follow-up period. The results of current operative techniques need to be fully investigated for longer term success, as do the outcomes of newer nonoperative management strategies.
Keywords: ankle, foot, tendinosis, plantar fasciitis, surgery
Plantar fasciitis is a common condition causing plantar aspect foot pain, typically affecting people in their fourth and fifth decades, and is one of the most common injuries affecting runners.6,26,33 While the majority of patients will improve with conservative therapies, approximately 10% develop persisting symptoms.10 Plantar fasciitis has a multifactorial etiology, and mechanical overload is thought to play a key role.25 Despite the name “fasciitis,” histological findings from operative specimens typically only show degenerative changes, including localized fibrosis, collagen necrosis, angiofibroblastic hyperplasia, and matrix calcification, and it is possible that any proposed inflammatory reaction occurs acutely and has passed before patients reach operative intervention.28,32 Some authors therefore prefer the term plantar fasciopathy.
A diagnosis of plantar fasciitis can typically be made on clinical grounds with a classical history and examination. Investigations can be used to confirm the clinical diagnosis or to exclude other pathologies. Ultrasound is reliable and effective in the diagnosis of plantar fasciitis,11,36 although a wide variety of imaging modalities are found in the literature and were used in this study, including radiographs, magnetic resonance imaging (MRI), and triple phase bone scans.13,23,25,34
A wide range of different conservative therapies are utilized in clinical practice, often in combination.26 Despite their widespread use, evidence remains inconclusive for a range of modalities, including foot stretching,10 orthoses,18 tension night splints,24 taping,38 and extracorporeal shockwave therapy (ESWT).22
Corticosteroid injections have traditionally been performed for persistent plantar fasciitis, although the effectiveness remains unclear. There is a poorly quantified frequency and consequence of plantar fascia rupture that may be as high as 10%, which replicates the effect of a plantar fascia release although in a less controlled fashion.2,29 Studies have found short-term relief from the pain of plantar fasciitis following steroid injection,8 with the best results arising from a “peppering” injection technique.16 Other injection therapies that have been shown to have short-term benefit include autologous blood injections,16,39 botulinum toxin A injections,3 and hyperosmolar dextrose,27 although robust evidence for these in large patient numbers and in the longer term is still lacking.
Surgery for plantar fasciitis is normally considered only when conservative therapies have been ineffective and significant symptoms persist. Patients treated surgically may not therefore be typical of those presenting for the first time with plantar fasciitis.
There are some theoretical risks of plantar fascia release, which have been studied in cadaveric specimens and models. One study using cadaveric specimens found that even partial plantar fasciotomy decreased the arch supporting function of the plantar fascia. This deficit started with only 25% divided, with increased impairment and extent of fasciotomy.35 However, the loading protocol did not readily simulate normal functional biomechanics. Cadaveric studies have shown that division of the plantar fascia reduced arch stiffness by 25%,14 and further work has shown that fasciotomy resulted in significant changes in joint position and a decrease in arch height to such an extent that the authors commented that plantar fasciotomy should not be performed in patients with preexisting pes planus, as this would be likely to lead to even further deterioration of foot position.17 However, this study did not take into account dynamic stabilizers and functional control, as it was utilizing cadaveric specimens only. However, another study simulated functional action in cadaveric specimens that replicated a collapse of the arch in the sagittal plane.31 Further cadaveric studies have shown significant changes to the medial and lateral columns with a release of only the medial third of the plantar fascia, which appears to lead to a strain of the calcaneocuboid ligament and joint capsule, a possible cause of persisting lateral midfoot pain seen following some surgeries.21
Research has also shown that plantar fascia release or rupture alters forefoot loading with increased loading of the second metatarsal, which was worse with complete compared with partial release.30 Studies using models created with MRI data have confirmed deformation of the arch while standing,12 although a later study showed that while the arch decreased in height, complete collapse did not occur even with additional dissection of the long plantar ligament.7
An in vivo study using in-shoe pressure measurements before and after plantar fasciotomy demonstrated a lateral shift of the center of pressure throughout the propulsive gait phase compared with control populations, which is counter to the concern that plantar fasciotomy may lead to a collapse of the medial arch, which would shift the weight medially rather than laterally.37
Overall, the biomechanical consequences after surgery are unclear; although plantar fasciotomy may appear to lead to changes in arch stability in cadaveric specimens and models, with a greater effect being seen in complete versus partial release, it is not known with certainty what effect this may have in the longer term on human subjects in vivo. The published articles vary in extent of plantar fascia release; one article describes complete plantar fascia release28 and others report 50% to 70% resection of the fascia.15 The long-term outcomes of these procedures may be different, and these have not been reported at this time.
Surgery for plantar fasciitis is not always clinically successful, with 10% to 50% of patients left unsatisfied following surgery.4,5,9,15,19,28,32,40 Complication rates vary, with some studies reporting no complications5 and others highlighting patients with perisisting pain in the heel or dorsal aspect of the foot, pain in the contralateral foot, persisting scar tissue discomfort, or chronic pain thought to be reflex sympathetic dystrophy.9,40 Worse outcomes were obtained in patients with more severe symptoms and those with a longer duration of preoperative symptoms.4 Obese patients appear to do as well as nonobese patients4; however, ethnicity may have an impact on operative outcomes.4 A change in operative technique has been noted in the literature, with endoscopic plantar fascia release (EPFR) becoming a viable alternative to the previously established open procedures.5 Recently, others have advocated a different approach to the surgical treatment for plantar fasciitis. Patients with plantar fasciitis often have resistant tightness to the calf musculotendinous complex. Encouraging early results (again, in small numbers) have been seen by surgical release of the gastrocnemius in the calf, which also avoids any local operative complications.1,20
A range of studies examining operative results have been reported using different operative techniques, but often, these are studies with small numbers, a short-term follow-up, or both, compounded by the absence of validated outcome measures. Table 1 highlights the operative results in the literature.
TABLE 1.
Summary of Results From Published Studies Investigating Surgery for Plantar Fasciitisa
| Study (Year Published) | No. of Cases | Surgery | Follow-up | Patient Outcomes |
|---|---|---|---|---|
| Snider et al32 (1983) | 9 long-distance runners (11 cases) | Open | Average, 25 mo | Excellent in 10 feet and good in 1 foot at an average follow-up time of 25 mo |
| Schepsis et al28 (1991) | 27 cases | Open—“complete plantar fascia release performed through a medial longitudinal incision” | Range, 1-3 y | 89% (24/27) were satisfied |
| Davies et al9 (1999) | 41 patients (45 feet) | “Decompression of the nerve to abductor digiti minimi with partial plantar fascia release” | Mean, 31 mo (range, 11-66 mo) | 75% were mildly painful or better; mean reduction of VAS from 8.5 to 2.5; only 49% (20/41) were totally satisfied with the outcome |
| Lundeen et al19 (2000) | 53 patients (69 feet) | EPFR | Average, 7.2 mo (range, 4-42 mo) | 81% satisfied |
| Woelffer et al40 (2000) | 30 patients (33 feet) | Open—“plantar skin incision” | 5 y | 90% were satisfied |
| Boyle and Slater5 (2003) | 17 patients (17 feet) | EPFR | 16 mo | 100% were satisfied, 82.4% had mild pain or less |
| Jerosch et al15 (2004) | 17 patients | EPFR | Average, 18.5 mo (range, 4-48 mo) | 76% (13/ 17) “improved clinically,” 13 patients had good or excellent results with Ogilvie-Harris score |
| Bazaz and Ferkel4 (2007) | 20 patients (23 feet) | EPFR | 1 y | Significant improvement in average AOFAS Ankle-Hindfoot Scale and Maryland Foot Score |
aAOFAS, American Orthopaedic Foot & Ankle Society; EPFR, endoscopic plantar fascia release; VAS, visual analog scale.
The perceived risk of plantar fasciotomy is that it causes deterioration in foot stability in the long term. To better assess this, studies with longer term follow-up are needed to see whether clinical deterioration does occur over time.
Methods
Previous patients from the Department of Sport & Exercise Medicine at the University Hospitals of Leicester NHS Trust, Leicester, UK, who had undergone surgery for plantar fasciitis between September 1993 and July 2009 were identified from operative diaries of the single surgeon who worked in the department at that time. Patient notes and previous imaging results were obtained directly from medical records wherever possible for objective details in preoperative and perioperative management. In some cases, original case notes could not be accessed and patient letters alone were used to obtain relevant information. Patients were then contacted by the study team by phone and/or letter ascertaining current status and recalled changes and complications after surgery. The questions asked were neutrally phrased so as to try not to lead the patient, but the contact was identified as coming from the hospital department where they had previously received treatment. At least 2 further attempts were made to contact patients who did not respond to initial invitations over a 6-month period. Final results were collated using a bespoke form and entered into an Excel spreadsheet (Microsoft, Redmond, Washington, USA) for compilation and analysis.
Operative Techniques
All operations in this series were performed by a single surgeon who led the department until his retirement 4 years ago. A medial longitudinal incision centered on the anterior inferior aspect of the calcaneus approximately 3 to 4 cm below the medial malleolus was used. The origin of the plantar fascia was identified and isolated by blunt dissection from the superficial fatty layer and the deep first muscular layer. Adjacent structures, namely the medial and lateral plantar nerves, were protected. The entire plantar fascia was then divided from medial to lateral sides under vision using scissors. If a prominent bony spur was present, this was also removed based on clinical experience of the operating surgeon. A small section of fascia was typically sent for histology. Postoperatively, the foot was bandaged; patients were given crutches and were instructed to be partial weightbearing for 2 weeks when a wound check was performed. After this point, patients gradually increased weightbearing as tolerated over a further 2- to 4-week period.
Results
A total of 79 cases were identified; 61% (48/79) were female and 39% (31/79) were male. The average age at surgery was 49.5 years (range, 23-73 years), with an average duration of symptoms of 32.6 months (range, 3-120 months).
From these identified cases, we received 68 responses (86% response rate) from those who had undergone surgery. The follow-up time was 1.0 and 15.5 years (average, 7.0 years). There appeared to be no significant difference in biographical data or symptom duration for patients who responded compared with those who did not respond, and there appeared to be no significant difference in the follow-up course they followed as documented in their available hospital notes and letters.
Previous Nonoperative Management
Patients had symptoms for an average of 32 months before surgery, and during this time, received an average of 1.7 injections presurgery (range, 1-7 injections) from a range of health professionals they consulted.
Surgery is offered only when other conservative measures have failed to improve symptoms. However, from the retrospective analysis of historical medical records, it was not always clear what therapies had been tried in all patients, and available figures may be an underrepresentation of interventions tried. It is recorded that 65% (51 patients) had been referred to a podiatrist and 39% (31 patients) had been seen by the orthotics team for night splints. Thirty percent (24 patients) had been referred for formal physical therapy, although it is assumed that others had been seen by a physical therapist prior to referral, although this was not always clearly documented. Three percent (2 patients) had received acupuncture through the department before surgery. While commonly used in some centers, ESWT had historically not been available in our department.
Patients underwent a range of different investigations before surgery to exclude alternate diagnoses as well as confirmation of the clinical diagnosis. Forty-nine percent (39/79) of patients operated on were known to have had a radiograph taken prior to surgery; 48% (38 patients) had an MRI, 44% (35 patients) had a bone scan, and 6% (5 patients) had an ultrasound. A change in investigation pattern was noted over the study period; investigations with triple-phase bone scans were seen earlier in this cohort, and subsequently, greater use of MRI and ultrasound were seen.
Comorbidities
Thirty-seven percent (29/79) of patients were recorded as being overweight or obese (body mass index at least 25) at the time of surgery, and 4% (3/79) had a diagnosis of type 2 diabetes mellitus. A number of patients had a range of co-existing musculoskeletal disorders, including 10% (8/79) with knee osteoarthritis, 6% (5/79) with first metatarsophalangeal joint osteoarthritis, and 11% (9/79) with osteoarthritis elsewhere in the foot. Four percent (3/79) of patients suffered from noninsertional/midsubstance Achilles tendinopathy, 3% (2/79) from insertional Achilles tendinopathy, and 1% (1 patient) from rheumatoid arthritis.
Operative Results
Overall, 84% (57/68) of respondents were satisfied with the results of their surgery; 16% (11/68) rated themselves as neutral or dissatisfied.
The mean postoperative improvement in pain measured using a visual analog scale (VAS) was 79% (range, 0%-100%). Seventy-four percent of patients rated their pain improvement as 80% or greater. Half of the patients were pain free following the surgery, but 10% had not improved. No patients rated themselves as worse after surgery.
Table 2 shows the number of respondents across a self-rated 7-part satisfaction scale and the mean improvement reported for each satisfaction band. As expected, reported patient satisfaction and the degree of improvement in postoperative pain were similar.
TABLE 2.
Patient Satisfaction Outcomes and Postoperative Improvement in Pain Score
| Respondents, No. (%) | % Improvement in Symptoms, Average | |
|---|---|---|
| Extremely satisfied | 34 (50) | 97 |
| Very satisfied | 15 (22) | 92 |
| Satisfied | 8 (12) | 66 |
| Neutral | 4 (6) | 27 |
| Dissatisfied | 4 (6) | 28 |
| Very dissatisfied | 2 (3) | 0 |
| Extremely dissatisfied | 1 (1) | 0 |
The results appeared to be better for patients with a shorter duration of symptoms. Patients with symptoms lasting ≤12 months who underwent surgery rated themselves at 90% improved on average; those with symptoms for 1 to 2 years rated at 81%, for 2 to 3 years rated an average of 78%, and patients with symptoms for more than 3 years at the time of surgery had an average improvement of 69%.
As displayed in Figure 1, female patients had an average of 34 months of symptoms prior to surgery and reported an average of 81% improvement; male patients on had an average of 30 months of symptoms and reported an average of 76% improvement. It was not clear whether sex is an independent outcome measure or, as previously discussed, whether any difference seen relates to the length of symptoms preoperatively.
Figure 1.
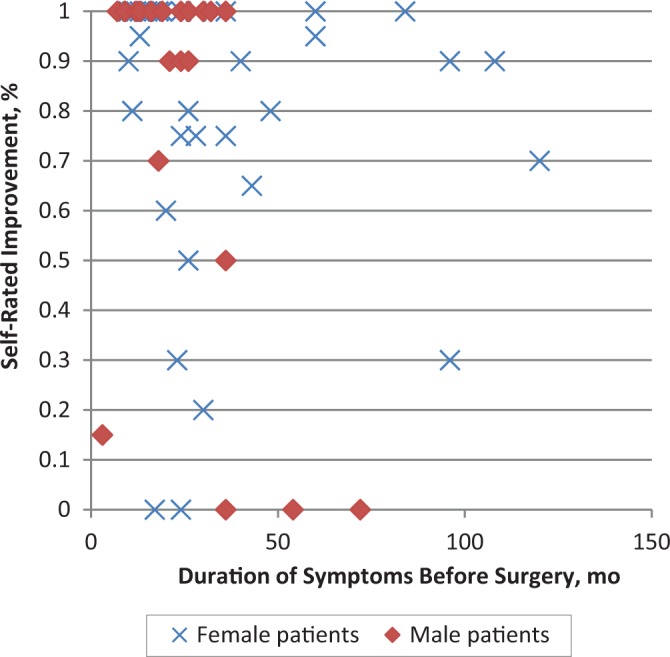
Self-rated postoperative improvement for male and female patients compared with preoperative duration of symptoms.
As demonstrated in Figure 2, there was no apparent drop-off for success over time following surgery, and if anything, there appears to have been an increasing reduction in pain. The average reduction in postoperative VAS (± standard deviation) for different periods of time was as follows: 0-3 years postoperatively, 68% ± 0.35%; 3.1-5.0 years, 74% ± 0.37%; 5.1-7.0 years, 80% ± 0.34%; 7.1-10 years, 86% ± 0.27%; >10 years, 88% ± 0.26%. The differences between these groups were not found to be significant.
Figure 2.
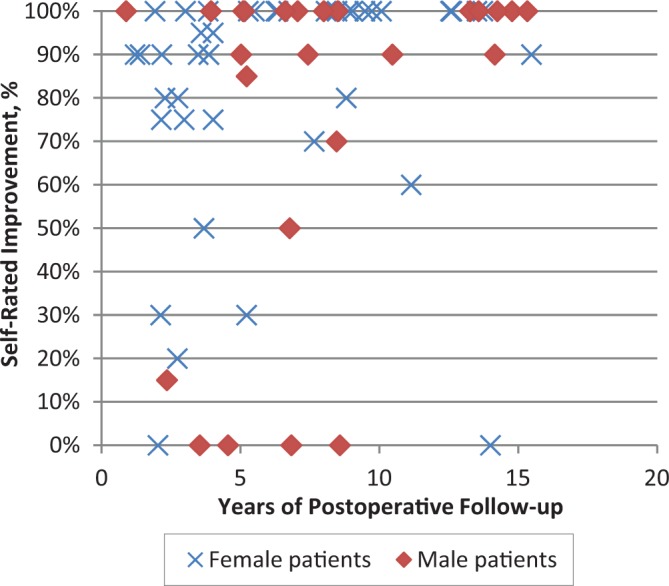
Subjective improvement with length of time postoperatively.
Eighteen percent of subjects had suffered either a recurrence of or ongoing symptoms since surgery, but only 11% had consulted other health professionals because of these symptoms.
Discussion
A retrospective cohort study design inevitably has some flaws. There is inherent bias in retrospective studies, and missing data may give an underrepresentation of the extent of conservative therapies tried prior to surgery. Although from the information available there were no significant differences, the outcome results in those who were unavailable for follow-up may be different from those who responded. Nevertheless, this approach has permitted an assessment of the outcome and long-term durability of plantar fasciotomy. Our response rate was favorable, and from the demographics available, it was thought that patients who did respond were representative of the entire group.
From this case series, 75% of patients would recommend surgery to a friend or family member. The results show that half of the patients were pain free following surgery, with an overall average reduction in VAS of 79%, and these figures are consistent with the outcomes of other published studies, even more favorable than some.4,5,9,15,19,28,32,40 Unlike the projected outcomes from biomechanics studies, which anticipate a deterioration in foot function over time, from this case series there appears to be no reduction in improvement seen with increasing length of time postsurgery, and if anything, a nonsignificant improvement. Unfortunately, there was insufficient information from the hospital notes and records to investigate any effect on the arch of the foot, but there are not records suggesting that this was thought to be a problem postoperatively.
This study adds to the evidence base that surgery for plantar fasciitis remains an appropriate treatment option for a patient who does not respond to conservative therapeutic options. Surgery has reasonable success even in the long term, with results that do not seem to deteriorate over time and, in keeping with other studies, better outcomes are achieved if surgery is conducted within 1 or 2 years of the onset of symptoms.
Open plantar fasciotomy remains an option in the management of recalcitrant plantar fasciitis but only after nonoperative measures have been explored. Currently, there is a trend toward novel conservative therapies such as ESWT or autologous blood or platelet-rich plasma injections. While studies are encouraging, it is not known whether these techniques will prove to have good long-term outcomes and whether these treatment options will have an effect on the number of patients who might otherwise undergo surgical management.
Acknowledgment
The authors would like to offer their sincere thanks to Mr Mike J. Allen, who performed all operations in this series. He originally founded the Leicester Sports Medicine Department in 1993, working there until his retirement in 2009, and was the surgeon whose cases are detailed in this study.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Abbassian A, Kohls-Gatzoulis J, Solan MC. Proximal medial gastrocnemius release in the treatment of recalcitrant plantar fasciitis. Foot Ankle Int. 2012;33:14–19. [DOI] [PubMed] [Google Scholar]
- 2. Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19:91–97. [DOI] [PubMed] [Google Scholar]
- 3. Babcock MS, Foster L, Pasquina P, Jabbari B. Treatment of pain attributed to plantar fasciitis with botulinum toxin a: a short-term, randomized, placebo-controlled, double-blind study. Am J Phys Med Rehabil. 2005;84:649–654. [DOI] [PubMed] [Google Scholar]
- 4. Bazaz R, Ferkel RD. Results of endoscopic plantar fascia release. Foot Ankle Int. 2007;28:549–556. [DOI] [PubMed] [Google Scholar]
- 5. Boyle RA, Slater GL. Endoscopic plantar fascia release: a case series. Foot Ankle Int. 2003;24:176–179. [DOI] [PubMed] [Google Scholar]
- 6. Buchbinder R. Plantar fasciitis. N Engl J Med. 2004;350:2159–2166. [DOI] [PubMed] [Google Scholar]
- 7. Cheung JT, An KN, Zhang M. Consequences of partial and total plantar fascia release: a finite element study. Foot Ankle Int. 2006;27:125–132. [DOI] [PubMed] [Google Scholar]
- 8. Crawford F, Atkins D, Young P, Edwards J. Steroid injection for heel pain: evidence of short-term effectiveness. A randomized controlled trial. Rheumatology. 1999;38:974–977. [DOI] [PubMed] [Google Scholar]
- 9. Davies MS, Weiss GA, Saxby TS. Plantar fasciitis: how successful is surgical intervention? Foot Ankle Int. 1999;20:803–807. [DOI] [PubMed] [Google Scholar]
- 10. DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective, randomized study. J Bone Joint Surg Am. 2003;85:1270–1277. [DOI] [PubMed] [Google Scholar]
- 11. Fabrikant JM, Park TS. Plantar fasciitis (fasciosis) treatment outcome study: plantar fascia thickness measured by ultrasound and correlated with patient self-reported improvement. Foot (Edinb). 2011;21:79–83. [DOI] [PubMed] [Google Scholar]
- 12. Gefen A. Stress analysis of the standing foot following surgical plantar fascia release. J Biomech. 2002;35:629–637. [DOI] [PubMed] [Google Scholar]
- 13. Grasel R, Schweitzer M, Kovalovich A, et al. MR imaging of plantar fasciitis: edema, tears, and occult marrow abnormalities correlated with outcome. AJR Am J Roentgenol. 1999;173:699–701. [DOI] [PubMed] [Google Scholar]
- 14. Huang CK, Kitaoka HB, An KN, Chao EY. Biomechanical evaluation of longitudinal arch stability. Foot Ankle Int. 1993;14:353–357. [DOI] [PubMed] [Google Scholar]
- 15. Jerosch J, Schunck J, Liebsch D, Filler T. Indication, surgical technique and results of endoscopic release in plantar fasciitis. Knee Surg Sports Traumatol Arthrosc. 2004;12:471–477. [DOI] [PubMed] [Google Scholar]
- 16. Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinc TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc. 2009;99:108–113. [DOI] [PubMed] [Google Scholar]
- 17. Kitaoka HB, Luo ZP, An KN. Mechanical behavior of the foot and ankle after plantar fascia release in the unstable foot. Foot Ankle Int. 1997;18:8–15. [DOI] [PubMed] [Google Scholar]
- 18. Landorf KB, Keenan A-M, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006;166:1305–1310. [DOI] [PubMed] [Google Scholar]
- 19. Lundeen RO, Aziz S, Burks JB, Rose JM. Endoscopic plantar fasciotomy: a retrospective analysis of results in 53 patients. J Foot Ankle Surg. 2000;39:208–217. [DOI] [PubMed] [Google Scholar]
- 20. Maskill JD, Bohay DR, Anderson JG. Gastrocnemius recession to treat isolated foot pain. Foot Ankle Int. 2010;31:19–23. [DOI] [PubMed] [Google Scholar]
- 21. Murphy GA, Pneumaticos SG, Kamaric E, Noble PC, Trevino SG, Baxter DE. Biomechanical consequences of sequential plantar fascia release. Foot Ankle Int. 1998;19:149–152. [DOI] [PubMed] [Google Scholar]
- 22. Ogden JA, Alvarez RG, Marlow M. Shockwave therapy for chronic proximal plantar fasciitis: a meta-analysis. Foot Ankle Int. 2002;23:301–308. [DOI] [PubMed] [Google Scholar]
- 23. Potter VAJ. Investigating plantar fasciitis. Foot Ankle Online J. 2009;2(11):4. [Google Scholar]
- 24. Powell M, Post WR, Keener J, Wearden S. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int. 1998;19:10–18. [DOI] [PubMed] [Google Scholar]
- 25. Puttaswamaiah R, Chandran P. Degenerative plantar fasciitis: a review of current concepts. Foot (Edinb). 2007;17:3–9. [Google Scholar]
- 26. Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25:303–310. [DOI] [PubMed] [Google Scholar]
- 27. Ryan MB, Wong AD, Gillies JH, Wong J, Taunton JE. Sonographically guided intratendinous injections of hyperosmolar dextrose/lidocaine: a pilot study for the treatment of chronic plantar fasciitis. Br J Sports Med. 2009;43:303–306. [DOI] [PubMed] [Google Scholar]
- 28. Schepsis AA, Leach RE, Gorzyca J. Plantar fasciitis: etiology, treatment, surgical results, and review of the literature. Clin Orthop Relat Res. 1991;266:185–196. [PubMed] [Google Scholar]
- 29. Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15:376–381. [DOI] [PubMed] [Google Scholar]
- 30. Sharkey NA, Donahue SW, Ferris L. Biomechanical consequences of plantar fascial release or rupture during gait. Part II: alterations in forefoot loading. Foot Ankle Int. 1999;20:86–96. [DOI] [PubMed] [Google Scholar]
- 31. Sharkey NA, Ferris L, Donahue SW. Biomechanical consequences of plantar fascial release or rupture during gait. Part I: disruptions in longitudinal arch conformation. Foot Ankle Int. 1998;19:812–820. [DOI] [PubMed] [Google Scholar]
- 32. Snider MP, Clancy WG, Mcbeath AA. Plantar fascia release for chronic plantar fasciitis in runners. Am J Sports Med. 1983;11:215–219. [DOI] [PubMed] [Google Scholar]
- 33. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Theodorou DJ, Theodorou SJ, Kakitsubata Y, et al. Plantar fasciitis and fascial rupture: MR imaging findings in 26 patients supplemented with anatomic data in cadavers. Radiographics. 2000;20(suppl 1):S181–S197. [DOI] [PubMed] [Google Scholar]
- 35. Thordarson DB, Kumar PJ, Hedman TP, Ebramzadeh E. Effect of partial versus complete plantar fasciotomy on the windlass mechanism. Foot Ankle Int. 1997;18:16–20. [DOI] [PubMed] [Google Scholar]
- 36. Tsai WC, Chiu MF, Wang CL, Tang FT, Wong MK. Ultrasound evaluation of plantar fasciitis. Scand J Rheumatol. 2000;29:255–259. [DOI] [PubMed] [Google Scholar]
- 37. Tweed JL, Barnes MR, Allen MJ. An evaluation of the long-term effects of total plantar fasciotomy—a preliminary study. Foot. 2009;19:75–79. [DOI] [PubMed] [Google Scholar]
- 38. van de Water ATM, Speksnijder CM. Efficacy of taping for the treatment of plantar fasciosis: a systematic review of controlled trials. J Am Podiatr Med Assoc. 2010;100:41–51. [DOI] [PubMed] [Google Scholar]
- 39. Wheeler P. Autologous blood injections for chronic plantar fasciitis—a pilot case-series study shows promising results. Int Musculoskelet Med. 2013;35:3–7. [Google Scholar]
- 40. Woelffer KE, Figura MA, Sandberg NS, Snyder NS. Five-year follow-up results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg. 2000;39:218–223. [DOI] [PubMed] [Google Scholar]


