Abstract
Background:
With improved understanding of the biomechanical importance of the medial patellofemoral ligament (MPFL), its reconstruction for patellar dislocation has become increasingly popular. The aim of this systematic review was to critically determine the effectiveness of MPFL reconstruction for patellar dislocation.
Hypothesis:
MPFL reconstruction for patellar dislocation leads to a low redislocation rate with improved Kujala scores.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A literature search was performed using Embase and Medline (Ovid) databases. Inclusion criteria included first-time and recurrent patellar dislocation, subluxation, or persistent instability with a minimum follow-up of 12 months and documentation of postoperative redislocation rate or Kujala score. The studies were systematically appraised, and a meta-analysis was performed.
Results:
Twenty-two studies were included: 2 randomized controlled trials, 3 parallel case series, and 17 case series. There were a total of 655 knees in the review, with an age range at time of surgery from 11 to 52 years. The pooled postoperative redislocation rate from all 17 case series showed a mean of 2.44%. The pooled preoperative Kujala scores from 12 case series showed a mean of 51.6 (95% CI, 46.71-56.49). The pooled postoperative Kujala scores from 16 case series showed a mean of 87.77 (95% CI, 85.15-90.39).
Conclusion:
Although the studies were of low quality, the meta-analysis of 17 case series shows that MPFL reconstruction for recurrent patellar dislocation results in a significant improvement in Kujala scores, a low redislocation rate, and acceptable complication rate. Randomized trials would be needed to draw influences on the superiority of MPFL reconstruction compared with other treatments.
Keywords: medial patellofemoral ligament (MPFL) reconstruction, patellar dislocation, patellar subluxation, systematic review
Patellar dislocation is the complete displacement of the patella from the trochlear groove of the femur. It nearly always involves a lateral displacement and commonly occurs during sports.4,30,38 The incidence is roughly 6 per 100,000, although it is considerably higher in children and adolescents aged between 10 and 19 years with an incidence of 31 per 100,000.30,38 Traditionally, patients are treated nonoperatively following a first-time patellar dislocation, although the rate of recurrence may be as high as 50%.22,38
Operative treatment for patellar dislocation has been published since the early 1900s, initially with an open-wedge osteotomy of the anterolateral femoral condyle. Over the past century, numerous surgical procedures have been described in the literature.3,27 Until recently, surgical treatment for recurrent dislocation has been aimed at addressing anatomical abnormalities such as trochlear dysplasia, patella alta, increased femoral antetorsion, increased external tibial torsion, increased Q angle, increased tibial tuberosity to trochlear groove distance, and valgus alignment of the lower limb.12,24 The most common techniques have traditionally included lateral release, trochleoplasty, and proximal or distal realignment procedures, or any combination of these procedures. These operations have been successful at reducing further dislocations but require postoperative restricted weightbearing, extended rehabilitation, lengthy periods of time off work, and variable results.35,41
The medial patellofemoral ligament (MPFL) is the primary soft tissue restraint to lateral dislocation of the patella, and a recent biomechanical study has shown that it must tear if the patella dislocates laterally.13,25 Advances in the understanding of the biomechanical importance of the MPFL have led to an increase in acute repair and reconstruction of this ligament. MPFL reconstruction has been most commonly performed for recurrent patellar dislocation, although there has been an increasing interest in MPFL surgery for primary patellar dislocation.30
There are multiple techniques for MPFL reconstruction using different types of grafts and varying rehabilitation protocols.21 With expanding use of MPFL reconstruction being performed worldwide for first time and recurrent patellar dislocation, the surgical technique with the best results and least complications needs to be determined.
Smith et al,37 in a systematic review of 8 papers, concluded that repeated literature review may be necessary to give surgeons greater confidence in the clinical or radiological outcomes of MPFL reconstruction for patella instability. The authors recommended this after MPFL reconstruction had gained further recognition, as more outcomes of surgical techniques and rehabilitation programs develop. They published another review36 in 2011; however, 10 important papers on this topic have been published since this date that add to the literature. Therefore, a systematic review with a primary outcome measure of redislocation rate and secondary outcome measures of Kujala scores and complications was undertaken. In our search, the most consistently used outcome measure was redislocation rate, and the most commonly used patient-reported measure was Kujala score. To maximize the inclusion of relevant papers, redislocation rate was chosen as our primary outcome measure and Kujala score as the secondary outcome measure. This review aimed to provide orthopaedic surgeons an improved understanding of clinical outcomes reported in the literature as well as common indications, surgical techniques, and rehabilitation programs.
Methods
Eligibility Criteria
Randomized control trials, comparative studies, case series, and case reports written in English, with a minimum 12-month follow-up, were included. A minimum follow-up of 12 months was chosen based on the time that patients get back to a normal level of function and sporting activities. There was no minimum subject number for each study set for inclusion. Studies had to include either the number of postoperative dislocations or Kujala scores in their outcome measures to be eligible for this systematic review.
All patients that had a first-time patellar dislocation, continued patellar instability, patellar subluxation, or recurrent patellar dislocation who underwent MPFL reconstruction using any technique with any graft type were included. Patients who had previous knee operations were also eligible, as this is the common clinical scenario. Subjects that underwent lateral release at the time of surgery were not excluded. However, those having any additional stabilization procedure at the time of MPFL reconstruction were excluded from the study. Studies that focused on MPFL repair were also excluded.
Study Search
The search was conducted using Embase and Medline (Ovid). The databases were searched from commencement to April 23, 2013, using a combination of keywords and subject headings (Tables 1 and 2).
TABLE 1.
Search Strategy on Medline (Ovid)a
| Searches | Results | |
|---|---|---|
| 1 | exp Patella/ or Patella*.mp. | 14,896 |
| 2 | knee cap.mp. | 28 |
| 3 | dislocation.mp. or exp Dislocations/ | 44,097 |
| 4 | dislocate*.mp. | 3924 |
| 5 | instability.mp. | 68,640 |
| 6 | sublux*.mp. | 7949 |
| 7 | MPFL.mp. | 133 |
| 8 | Medial patellofemoral ligament*.mp. | 222 |
| 9 | ligament reconstruction.mp. | 4379 |
| 10 | 1 or 2 | 14,904 |
| 11 | 3 or 4 or 5 or 6 | 112,896 |
| 12 | 7 or 8 or 9 | 4548 |
| 13 | 10 and 11 and 12 | 497 |
| 14 | limit 13 to (English language and humans) | 422 |
aSearch performed on April 23, 2013.
TABLE 2.
Search Strategy on Embase (Ovid)a
| Searches | Results | |
|---|---|---|
| 1 | Patella*.mp. or exp patella/ | 19,539 |
| 2 | Knee cap.mp. | 44 |
| 3 | exp dislocation/ or Dislocation.mp. | 57,363 |
| 4 | Dislocate*.mp. | 5128 |
| 5 | Instability.mp. | 95,061 |
| 6 | exp subluxation/ or Sublux*.mp. | 10,825 |
| 7 | exp patella dislocation/ or Patella* dislocation.mp. | 1774 |
| 8 | MPFL.mp. | 179 |
| 9 | Medial patellofemoral ligament.mp. | 292 |
| 10 | Ligament reconstruction.mp. | 6571 |
| 11 | 1 or 2 | 19,554 |
| 12 | 3 or 4 or 5 or 6 | 151,395 |
| 13 | 11 and 12 | 4313 |
| 14 | 7 or 13 | 4313 |
| 15 | 8 or 9 or 10 | 6772 |
| 16 | 14 and 15 | 612 |
| 17 | limit 16 to (human and English language) | 513 |
aSearch performed on April 23, 2013.
Review Process
The results of the searches from Embase and Medline (Ovid) were downloaded into Endnote 9.0 (Thomson Reuters). These were cross-referenced, and all duplicates were deleted. All potentially eligible publications were assessed by 2 reviewers, and any discrepancies or disagreements were resolved by discussion. A third senior reviewer was available for final review if consensus was not found. Full texts were obtained for those papers not excluded at the abstract reviewing phase. Figure 1 shows a flow diagram of the selection process.
Figure 1.

Filtering process for studies found with the search strategy.
Data Analysis
The primary outcome measure was postoperative recurrence of patellar dislocation. The secondary outcome measures were Kujala scores and complications. As measures of variance were not available for the studies identified by the search, data were pooled across all studies using a weighted mean, with weights given by the study sample size for Kujala scores; 95% CIs for the pooled means were based on between-study variation and assumed asymptotic normality. For complication and redislocation rates, a 2-sided (clipped) 95% CI was calculated for each study based on assumed normality and a pooled estimate of the overall rate and CI obtained in a similar manner using data summed across studies. Data are presented on forest plots, with symbol sizes for means scaled to indicate study sample sizes. All statistical analyses were undertaken in R software (R Core Team 2013; R Foundation for Statistical Computing).
Results
First-time Dislocation
The only study that assessed first-time dislocation was by Bitar et al.5 This was a randomized controlled trial comparing MPFL reconstruction to nonoperative treatment. They included patients with first-time traumatic patellar dislocation within 3 weeks of treatment in patients older than 12 years. There were 21 patients (21 knees) undergoing MPFL reconstruction using patellar tendon graft compared with 18 patients (20 knees) who had bracing for 3 weeks and physical therapy. At 2-year follow-up, there were no dislocations in the operative group and 7 dislocations in the nonoperative group. Kujala scores in the operative group and the nonoperative group at final follow-up were 88.9 and 70.8, respectively (P = .001). They concluded that MPFL reconstruction produced better results than nonoperative treatment. This study provides some evidence that MPFL reconstruction may be superior to nonoperative treatment in first-time patellar dislocation. However, there are some methodological flaws that limit the strength of the recommendations. The description of the randomization method and allocation concealments was inadequate, which risks a flawed randomization. Second, the assessors were not blinded to the treatment the patients received, which risks measurement bias.
Recurrent Dislocations
There were a total of 614 knees treated for recurrent patellar dislocation. This included 1 retrospectively reviewed randomized controlled trial comparing 2 different methods of graft fixation.23 There was 1 parallel case series comparing a static and dynamic technique for MPFL reconstruction.16 There were 2 further parallel case series: 1 comparing MPFL reconstruction to MPFL with vastus medialis advancement and another comparing MPFL reconstruction to the Roux-Goldthwait procedure.35,42 In addition to this, there were 17 case series using various surgical techniques and grafts for MPFL reconstruction.§
Clinical Outcome
Redislocation Rate
The pooled postoperative dislocation percentage from all 17 case series showed a mean (95% CI) of 2.44% (1.29%-4.46%). Figure 2 is a forest plot of these data. The randomized study by Mikashima et al23 reported no redislocations in either group. The parallel case series by Wang et al42 shows no recurrent redislocations, although 8 (28.6%) in the MPFL reconstruction group and 3 (7.3%) in the MPFL reconstruction with vastus medialis advancement had a lateral patellar shift exceeding 1.5 cm (P < .05). The parallel case series by Sillanpää et al35 had 1 (6.7%) redislocation in the MPFL reconstruction group and 3 (14.3%) in the Roux-Goldthwait group. All 4 cases underwent further patellar stabilization procedures. Additionally, there were 2 patients with painful subluxations in each group, of which 1 in the MPFL reconstruction group underwent further patellar stabilisation procedure.35 The study by Gomes16 reported that there were no dislocations in either group, although there was 1 subluxation in the adductor magus static group.
Figure 2.
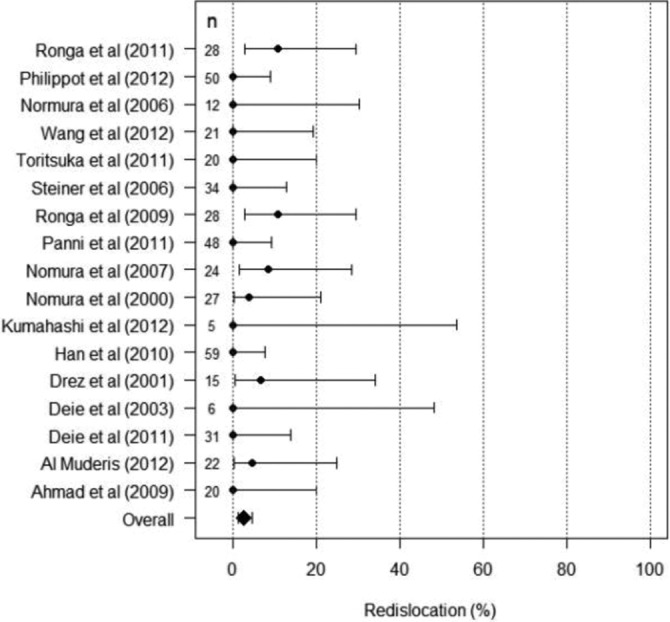
Forest plot of postoperative dislocations.
Kujala Score
The pooled preoperative Kujala scores from 12 case series showed a mean of 51.6 (95% CI, 46.71-56.49). The pooled postoperative Kujala scores from 16 case series showed a mean of 87.77 (95% CI, 85.15-90.39). Figures 3 and 4 are forest plots from the case series. The randomized trial comparing 2 different methods of graft fixation reported a mean preoperative Kujala score of 30.5 (range, 28-38) and at final follow-up, 95.2 (range, 82-100). They did not provide a breakdown between the 2 randomized arms. The study by Wang et al42 found an improvement in Kujala scores in the MPFL reconstruction group from 51.3 to 79.9 and in the MPFL reconstruction with vastus medialis advancement group from 53.7 to 83.9 at 42 months. The differences were not statistically significant. The study by Sillanpää et al35 reported a median postoperative Kujala score of 88 in the MPFL reconstruction group at a median of 10.1 years and 86 in the Roux-Goldthwait group at a median of 7.0 years (P = .68).
Figure 3.

Preoperative Kujala scores.
Figure 4.

Postoperative Kujala scores.
Complications
The pooled postoperative complication rate from all 17 case series showed a mean of 5.78% (95% CI, 3.88%-8.46%). Figure 5 represents the pooled postoperative complication data. Throughout all of the studies, 3 (0.45%) patellar fractures were reported as complications. Mikashima et al23 reported 2 patellar fractures from the group of patients in which they used a patellar bone tunnel as part of the fixation of the graft. There was 1 (2.1%) patellar fracture in the case series by Panni et al31 in which they used a double patellar tunnel technique for graft fixation.
Figure 5.

Forest plot of complications.
Indications
The indications for MPFL reconstruction in the included studies ranged from habitual subluxation to recurrent subluxations to recurrent lateral patellar dislocations. The majority of studies were on patients defined to have recurrent patellar dislocations. In contrast, Ahmad et al1 had a mixed patient group: 2 patients had recurrent subluxations, 2 dislocated once, 4 dislocated twice, and 12 had experienced habitual dislocations. They further defined that all patients in this group who experienced dislocation also had recurrent subluxations after their initial dislocation. Each of these patients had a failed trial of nonoperative treatment, including bracing and physical therapy, prior to being eligible for MPFL reconstruction surgery.
Surgical Technique
There was no consistent surgical technique used throughout the papers assessed. The angle of knee flexion most commonly applied when the graft was tensioned was 60° in 6 studies.1,16,17,26,28,29 However, knee flexion angles of 20°,31 30°,32 45°,40 and 60° to 90°39 were also used. One case series also carried out this part of the procedure with the knee in full extension.14 Screw fixation was the most used method of graft fixation to the femur in 9 studies.∥ Alternative methods of fixation of the graft to the femur were the use of an Endobutton (Smith & Nephew), staples, or sutures. Fixation of the graft to the patella was most commonly performed by sutures. Six papers used a 2–patellar tunnel technique,1,17,31,33,34,40 8 used a single patellar tunnel,2,16,23,26,28,29,39,42 and 8 used techniques that did not require a patellar tunnel.5,10,11,20,32,35,43 Lateral release was used in some patients depending on the surgeon’s preference and the individual patient’s pathology/patellar alignment.
Graft Type
Artificial grafts for MPFL reconstruction were used in 3 case series. Al Muderis et al2 used 3 different artificial materials as the ligament augmentation graft. The authors did not further specify the materials used. A mesh-type polyester artificial ligament (Neoligaments Ltd) was used in both of the case series by Nomura et al.26,29 The recruitment periods overlapped in these studies; therefore, some of the same patients may be in both studies. All other studies used autografts except Ahmad et al,1 who used semitendinosus allograft in 2 patients and tibialis anterior allograft in 2 patients who underwent MPFL reconstruction. They used allografts in patients who wanted to have minimal pain and/or required limited use of analgesia postoperatively. The other 16 patients in this study had semitendinosus autografts for their ligament reconstruction. The most common autograft was the semitendinosus tendon; however, gracilis, iliotibial band, and adductor tendons were also used. In addition, Steiner et al39 used bone–quadriceps tendon and bone–patellar tendon autografts. In the majority of studies, a single tendon graft was used to re-create the torn MPFL ligament. However, Tortisuka et al40 used a double-looped semitendinosus tendon autograft for reconstruction in contrast to Gomes,16 who used half-width (hemi-tendon) semitendinosus autograft. The case series by Deie et al11 used a combined semitendinous and gracilis tendon autograft in 5 patients.
Rehabilitation
The rehabilitation program following MPFL reconstruction varied widely throughout the studies. In 3 case series the postoperative rehabilitation program was not described.11,32,33 All other included case series, with the exception of 1, used a knee brace or a knee immobilizer as part of their rehabilitation protocol.16 The duration of brace use and whether patients were allowed to bear weight partially or fully varied greatly. In the majority of studies, quadriceps strengthening exercises were featured in their rehabilitation programs. In 8 studies using different rehabilitation protocols, patients returned to full sporting activities at or around 6 months after MPFL reconstruction.10,14,20,23,31,34,42,43 Three studies stated patients could go back to full sports following MPFL reconstruction at 3 months,26,28,29 1 study at 4 months,1 1 study between 4 and 6 months,17 and 1 study between 2½ to 3 months.5
Follow-up
The studies had follow-up times ranging from a minimum of 12 months to a maximum of 17.2 years. The prospective case series by Nomura et al,29 who used a polyester tape for MPFL reconstruction, had the longest mean follow-up of 11.9 years (range, 8.5-17.2 years). The largest study, with 69 patients, compared isolated MPFL reconstruction to a group of patients who had MPFL reconstruction with vastus medialis advancement and had an average follow-up of 42 months (range, 12-65 months).42 The randomized control trial by Bitar et al5 had a mean follow-up of 44 months (range, 24-61 months).
Discussion
This systematic review was conducted to update previous research evaluating MPFL reconstruction for first-time and recurrent patellar dislocation. There were few high-quality studies, with the vast majority being case series with small numbers of patients. Several articles use the terms subluxation and dislocation interchangeably. However, these are different pathologies, which makes it even more difficult to compare the postoperative outcomes.
First-time Patellar Dislocation
There was 1 randomized controlled trial on first-time patellar dislocation by Bitar et al.5 There was no recurrent subluxation or dislocation in the group who underwent MPFL reconstruction. In comparison, the group of patients managed conservatively had 7 patients (35%) who had a recurrent dislocation or subluxation. The mean Kujala score was significantly lower in the nonoperative group in comparison with the surgical reconstruction group. Although the results were good, caution in drawing conclusions is warranted given that this was a single study with small numbers and methodological flaws.
Surgery for first-time patellar dislocation is less frequent than for recurrent dislocations. Traditionally, first-time dislocations have been treated nonoperatively; however, because of high rates of redislocation and the development of late-onset anterior knee pain, surgical treatment may become more common.38 Depending on the patient group, 44% to 70% of those who have had 1 patellar dislocation will go on to have a recurrent dislocation.18,36,38 Prognostic factors for poor nonoperative outcomes include a palpable defect in the vastus medialis obliquus, adductor mechanism, and a grossly dislocatable patella.19
A systematic review by Stefancin and Parker,38 based on 70 articles, recommends initial nonoperative treatment for first-time traumatic patellar dislocation with some clinical exceptions. The specific circumstances that they recommend surgical treatment for include the presence of an osteochondral fracture, substantial disruption of the medial patellar stabilizers, a laterally subluxated patella with normal alignment of the contralateral knee, a second dislocation, or patients not improving with appropriate rehabilitation.38
Recurrent Patellar Dislocation
This meta-analysis of 17 case series including 450 knees provides evidence that MPFL reconstruction for recurrent patellar dislocation has good functional outcomes with low redislocation and complication rates. However, most of the case series had low numbers.
There are several alternative operative treatments for recurrent patellar dislocation. Operative procedures to correct a large tibial tuberosity–trochlear groove distance, patella alta, trochlear dysplasia, or deficient soft tissue restraints can improve patellofemoral stability. Recurrent dislocation following trochleoplasty for significant trochlear dysplasia is rare; however, persistent pain and articular cartilage damage are not unusual after this procedure.6
Distal realignment such as the Elmslie-Trillat procedure is also a common procedure used to treat patella dislocation. Brown et al7 reported 27 knees that underwent the Elmslie-Trillat procedure for recurrent patellar dislocation, subluxation, or abnormally high Q angle associated with positive apprehension test in an asymptomatic patient. Using the Cox grading system, 81% of patients rated their postoperative outcome as good or excellent. In this group, 8% rated their outcome as poor and there were 3 perioperative complications. Dannawi et al9 evaluated a modified Elmslie-Trillat procedure for patellofemoral dysfunction with a follow-up of 45 months for 29 knees. There was no reported redislocations postoperatively in this group, and 62% of patients rated their outcomes as good or excellent using the Cox grading system. Insall’s proximal realignment procedure is another operative technique used for recurrent patellar dislocation. The case series by Efe et al15 evaluated the clinical outcome of the Insall procedure in 45 patients. No statistically significant improvements in Kujala scores were found, and 10 patients suffered from recurrent dislocations. There are no randomized controlled trials that have been used to establish the gold standard for surgical treatment of patellar dislocation or subluxation. Consequently, comparison or determination of superiority cannot be drawn between the different surgical techniques. However the pooled results of MPFL reconstruction of a 36-point increase in Kujala score and 2.4% redislocation rate do appear to be favorable when compared with other surgical treatments.
Limitations
The studies included in this systematic review had a minimum follow-up of 12 months, which may be too short to assess the outcome of patients over a medium- and long-term time frame. However, many studies have a minimum follow-up of 1 to 2 years, and excluding these studies would limit the number of studies reviewed. Future studies could determine whether the prevalence of recurrent dislocation is similar at over 20 years follow-up, as Carney et al8 showed for the Roux-Elmslie-Trillat procedure.
Only published studies were searched for, which risks exacerbating publication bias. Secondly, only literature published in the English language was included, as costs of translations would have been required; this may have limited our search.
Conclusion
This systematic review and meta-analysis demonstrates that MPFL surgery for recurrent patellar dislocation results in a significant improvement in Kujala scores, a low redislocation rate, and an acceptable complication rate. Despite this, there is no consensus on indications for MPFL reconstruction, graft type, surgical technique, and rehabilitation program. Randomized controlled studies conducted in line with the CONSORT statement are needed to test the hypothesis that MPFL reconstruction leads to better outcomes for patients with recurrent patellar dislocation. The inclusion criteria for future studies will be highly important, and consensus agreement within an expert panel should be sought prior to undertaking such a study.
References
- 1. Ahmad CS, Brown GD, Stein BS. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37:2021–2027. [DOI] [PubMed] [Google Scholar]
- 2. Al Muderis M, Stein S, Krimly A, Shamsuldin A, Bosley B. Minimally invasive surgical technique in treating recurrent patellar dislocation. J Sci Med Sport. 2012;15 (suppl 1):S132–S133. [Google Scholar]
- 3. Albee F. The bone graft wedge in the treatment of habitual dislocation of the patella. Med Rec. 1915;88:257–259. [Google Scholar]
- 4. Atkin DM, Fithian DC, Marangi KS, Stone ML, Dobson BE, Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472–479. [DOI] [PubMed] [Google Scholar]
- 5. Bitar A, Demange M, D’Elia C, Camanho G. Reconstruction of the medial patellofemoral ligament was effective for traumatic patellar dislocation. Am J Sports Med. 2012;40:114–122. [DOI] [PubMed] [Google Scholar]
- 6. Bollier M, Fulkerson J. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19:8–16. [DOI] [PubMed] [Google Scholar]
- 7. Brown DE, Alexander AH, Lichtman DM. The Elmslie-Trillat procedure: evaluation in patellar dislocation and subluxation. Am J Sports Med. 1984;12:104–109. [DOI] [PubMed] [Google Scholar]
- 8. Carney JR, Mologne TS, Muldoon M, Cox JS. Long-term evaluation of the Roux-Elmslie-Trillat procedure for patellar instability: a 26-year follow-up. Am J Sports Med. 2005;33:1220–1223. [DOI] [PubMed] [Google Scholar]
- 9. Dannawi Z, Khanduja V, Palmer CR, El-Zebdeh M. Evaluation of the modified Elmslie-Trillat procedure for patellofemoral dysfunction. Orthopedics. 2010;33:13. [DOI] [PubMed] [Google Scholar]
- 10. Deie M, Ochi M, Adachi N, Shibuya H, Nakamae A. Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med. 2011;39:140–145. [DOI] [PubMed] [Google Scholar]
- 11. Deie M, Ochi M, Sumen Y, Yasumoto M, Kobayashi K, Kimura H. Reconstruction of the medial patellofemoral ligament for the treatment of habitual or recurrent dislocation of the patella in children. J Bone Joint Surg Br. 2003;85:887–890. [PubMed] [Google Scholar]
- 12. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. [DOI] [PubMed] [Google Scholar]
- 13. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65. [DOI] [PubMed] [Google Scholar]
- 14. Drez D, Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. [DOI] [PubMed] [Google Scholar]
- 15. Efe T, Seibold J, Geßlein M, et al. Non-anatomic proximal realignment for recurrent patellar dislocation does not sufficiently prevent redislocation. Open Orthop J. 2012;6:114–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gomes JE. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24:430–435. [DOI] [PubMed] [Google Scholar]
- 17. Han H, Xia Y, Yun X, Wu M. Anatomical transverse patella double tunnel reconstruction of medial patellofemoral ligament with a hamstring tendon autograft for recurrent patellar dislocation. Arch Orthop Trauma Surg. 2011;131:343–351. [DOI] [PubMed] [Google Scholar]
- 18. Hing CB, Smith TO, Donell S, Song F. Surgical versus nonsurgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2011;(11):CD008106. [DOI] [PubMed] [Google Scholar]
- 19. Hinton R, Sharma K. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am. 2003;34:385–396. [DOI] [PubMed] [Google Scholar]
- 20. Kumahashi N, Kuwata S, Tadenuma T, Kadowaki M, Uchio Y. A “sandwich” method of reconstruction of the medial patellofemoral ligament using a titanium interference screw for patellar instability in skeletally immature patients. Arch Orthop Trauma Surg. 2012;132:1077–1083. [DOI] [PubMed] [Google Scholar]
- 21. Lenschow S, Schliemann B, Gestring J, Herbort M, Schulze M, Kösters C. Medial patellofemoral ligament reconstruction: fixation strength of 5 different techniques for graft fixation at the patella. Arthroscopy. 2013;29:766–773. [DOI] [PubMed] [Google Scholar]
- 22. Mäenpää H, Huhtala H, Lehto M. Recurrence after patellar dislocation. Redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68:424–426. [DOI] [PubMed] [Google Scholar]
- 23. Mikashima Y, Kimura M, Kobayashi Y, Miyawaki M, Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg. 2006;72:65–71. [PubMed] [Google Scholar]
- 24. Mizuno Y, Kumagai M, Mattessich S, et al. Q-angle influences tibiofemoral and patellofemoral kinematics. J Orthop Res. 2001;19:834–840. [DOI] [PubMed] [Google Scholar]
- 25. Mountney J, Amis AA. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87-B(1):36–40. [PubMed] [Google Scholar]
- 26. Nomura E, Horiuchi Y, Kihara M. A mid-term follow-up of medial patellofemoral ligament reconstruction using an artificial ligament for recurrent patellar dislocation. Knee. 2000;7:211–215. [DOI] [PubMed] [Google Scholar]
- 27. Nomura E, Inoue M. Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy. 2003;19:E47. [DOI] [PubMed] [Google Scholar]
- 28. Nomura E, Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years’ follow-up. Arthroscopy. 2006;22:787–793. [DOI] [PubMed] [Google Scholar]
- 29. Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35:1851–1858. [DOI] [PubMed] [Google Scholar]
- 30. Panni A, Vasso M, Cerciello S. Acute patellar dislocation. What to do? Knee Surg Sports Traumatol Arthrosc. 2013;21:275–278. [DOI] [PubMed] [Google Scholar]
- 31. Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39:2647–2655. [DOI] [PubMed] [Google Scholar]
- 32. Philippot R, Stamilla M, Farizon F, Gresta G. Medial patellofemoral ligament ligamentoplasties in case of objective patellar instability. J Orthop Traumatol. 2012;13:S112. [Google Scholar]
- 33. Ronga M, Oliva F, Longo U, Teata V, Capasso G, Maffulli N. Isolated medial patellar femoral ligament reconstruction for recurrent patella dislocation: a prospective cohort study. J Orthop Traumatol. 2011;12:S137–S138. [Google Scholar]
- 34. Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37:1735–1742. [DOI] [PubMed] [Google Scholar]
- 35. Sillanpää P, Mattila VM, Visuri T, Mäenpää H, Pihlajamäki H. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466:1475–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Smith T, Song F, Donell S, Hing C. Operative versus nonoperative management of patellar dislocation. A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:988–998. [DOI] [PubMed] [Google Scholar]
- 37. Smith TO, Walker J, Russell N. Outcomes of medial patellofemoral ligament reconstruction for patellar instability: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2007;15:1301–1314. [DOI] [PubMed] [Google Scholar]
- 38. Stefancin J, Parker R. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93–101. [DOI] [PubMed] [Google Scholar]
- 39. Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34:1254–1261. [DOI] [PubMed] [Google Scholar]
- 40. Toritsuka Y, Amano H, Mae T, et al. Dual tunnel medial patellofemoral ligament reconstruction for patients with patellar dislocation using a semitendinosus tendon autograft. Knee. 2011;18:214–219. [DOI] [PubMed] [Google Scholar]
- 41. Utting M, Mulford J, Eldridge J. A prospective evaluation of trochleoplasty for the treatment of patellofemoral dislocation and instability. J Bone Joint Surg Br. 2008;90:180–185. [DOI] [PubMed] [Google Scholar]
- 42. Wang F, Kang HJ, Chen BC, Chen W, Su YL, Zhang YZ. Combination of medial patellofemoral ligament reconstruction with vastus medialis advancement for chronic patellar dislocation. Chin Med J (Engl). 2010;123:3024–3029. [PubMed] [Google Scholar]
- 43. Wang JL, Li HP, Liu YJ, et al. Reconstruction of the medial patellofemoral ligament with a suture-tie technique of patellar side fixation. Chin Med J (Engl). 2012;125:1884–1888. [PubMed] [Google Scholar]


