Abstract
Background:
There is a dearth of research on the current health of former collegiate athletes.
Purpose:
To examine the current health and related correlates in a cohort of former collegiate athletes who played in a diverse range of men’s and women’s sports with various levels of contact.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Former collegiate athletes (N = 3657) were asked to complete an online questionnaire addressing sports history, medical history, and demographics. The questionnaire also included the Veterans RAND 12-Item Health Survey (VR-12), which yielded 2 composite scores for physical (PCS) and mental (MCS) health. The VR-12 PCS and MCS scores were compared with published US normative data using t tests and analyses of variance.
Results:
Mean PCS and MCS scores of the 797 respondents with complete data (21.9% of target sample; average, 14.5 years since last played collegiate sport) were 53.0 ± 6.1 and 51.7 ± 9.4, respectively. When stratified by age and sex, PCS and MCS scores were similar to normative scores in the United States. Lower PCS scores were associated with sustaining ≥3 concussions, playing in collision sports during college, and sustaining a career-ending injury (all, P < .001). No association was found between concussion and MCS scores (P = .06). Among former collegiate athletes, prevalent medical conditions included anxiety (16.2%), hypercholesterolemia/high cholesterol (10.6%), and depression (10.4%). Additionally, 5.8% screened positive for alcohol dependence, and 5.8% screened positive for disordered eating (eg, binge eating, purging). These findings were more prevalent than those reported by the World Health Organization as representative of the US population. Conversely, there was a lower prevalence of depression, bipolar disorders, and attention deficit disorder, with or without hyperactivity (ADD/ADHD), than in the World Health Organization US population data sample.
Conclusion:
Former collegiate athletes appear similar to the general US population on many aspects of mental and physical health. However, observed health deficits associated with previous sports injuries warrant ongoing monitoring of the health and well-being of former collegiate athletes.
Keywords: physical health, mental health, injury, epidemiology, traumatic brain injury
Sports place high levels of physical and mental demands on elite athletes. Elite athletes undertake a long duration and high intensity of training, frequently specialize in their sport from an early age, experience high numbers of repetition of specific sport skills, and constantly seek to elevate the difficulty of the athletic skills they practice and possess.20 Accordingly, the performance-oriented paradigm of sport encourages many athletes to constantly push their bodies in an effort to optimize performance, sometimes ignoring recovery demands and their bodies’ warning signs of pain and overuse.12 As participation in organized sports at the youth, high school, and collegiate levels continues to increase,22,23,36 it becomes even more important to understand the benefits and burden of sports participation and explore methods to accurately characterize its potential effects on long-term athlete health and well-being.
Most findings related to the current health of former athletes originate from empirical examinations of retired National Football League (NFL) players. In comparison with the general American male population, retired NFL players (mean age, 53.8 ± 13.4 years; average professional football playing career of 6.6 ± 3.6 years) reported higher prevalences and earlier onsets of Alzheimer disease and osteoarthritis.8,9 In addition, recurrent concussion in retired NFL players was associated with a higher prevalence of significant memory problems,9 reported bodily pain,29 and clinical diagnoses of mild cognitive impairment and depression.6,10,15,29
Studies of former NFL player populations have the potential to improve access to and quality of care for current and former professional athletes. However, there has been little research to date on those athletes who compete at the elite amateur level but do not always reach the professional level. The National Collegiate Athletic Association (NCAA), a large American governing body for intercollegiate sport, estimates that the percentage of NCAA senior student-athletes who are drafted into professional sports is low, ranging from 0.7% in men’s soccer to 9.7% in baseball.21 With over 450,000 NCAA student athletes active during the 2012-2013 school year,22 former collegiate athletes are an important population of former high-performance athletes in need of further study. However, to date, only 1 published study has examined the current health of former collegiate athletes.30 In a cohort of 232 former collegiate athletes ranging in age from 40 to 65 years, levels of health-related quality of life were compared to nonathlete controls of similar ages that were physically active 3 to 5 times a week during college. The former athletes reported lower scores for physical function, depression, fatigue, sleep, and pain interference.
To address this important knowledge gap, our study examined the current physical and mental health in a cohort of former collegiate athletes who played in a diverse range of men’s and women’s sports. We then sought to explore the role of demographics and sports-related factors (including concussion history) as contributors to current levels of self-reported physical and mental functioning. Last, we examined the prevalence of a wide range of medical conditions and maladaptive behavioral conditions.
Methods
The study utilized a cross-sectional design. An online, self-administered questionnaire was sent to the e-mail addresses of 3657 former collegiate athletes from an NCAA Division I university in the southern United States. The inclusion criteria for eligibility into the study cohort were (1) played at least 1 season of a collegiate sport between 1987 and 2012 at the host university, (2) aged 18 years or older, (3) had an e-mail address provided by the university alumni association, and (4) able to speak and understand English.
The online, self-administered questionnaire collected information on sports history, concussion history, current physical and mental health, and demographics. Many of its components originate from the retired NFL players cohort health survey.15 The online questionnaire used Qualtrics software and was extensively pilot-tested and revised prior to data collection. Reminder e-mails were sent every other week throughout a 3-month data collection window (April to June 2013). A copy of the questionnaire is available on request.
Sports Health History
Demographics and Sports History
We collected data on sex, age, weight, height, relationship status, education level, work status, race/ethnicity, and disability status. We also collected information on collegiate sports played. Those former collegiate athletes who played more than 1 sport in college were asked to identify 1 sport as primary (ie, most invested in participation). Respondents then reported the school grade at which they began playing their primary sport, whether they had played their primary sport professionally, or sustained a career-ending injury at any point in their sports career.
Concussion History
Respondents reported the number of concussions sustained during participation in sports, including at the high school, college, and (if applicable) professional levels (see the Appendix, available separately online). In addition, respondents reported the number of non–sports related concussions (eg, from a car crash, fall, or violence). We reminded respondents that these non–sports related concussions may also include any childhood injuries that they had been told about but may not remember. Concussions were defined as “occurring typically, but not necessarily, from a blow to the head followed by a variety of symptoms that may include any of the following: headache, dizziness, loss of balance, blurred vision, ‘seeing stars,’ feeling in a fog or slowed down, memory problems, poor concentration, nausea, or throwing-up.” Participants were reminded that getting “knocked out” or being unconscious does not always occur with a concussion.
Outcome Measures
Overall Physical and Mental Health
The Veterans RAND 12-Item Health Survey (VR-12) is a self-administered health survey instrument in the public domain that assesses health status and estimates how well individuals function with activities of daily living. The VR-12 was developed from the Veterans RAND 36-Item Health Survey (VR-36), which was adapted from the RAND 36-Item Health Survey (SF-36) in the RAND Corporation and the Medical Outcomes Study.14 The VR-12 is similar to an abridged version of the SF-36 known as the 12-Item Short Form Health Survey (SF-12), but it replaces yes/no responses from 2 items on the SF-12 with 5-point response choices.13
The VR-12 measure yielded 2 composite scores: first, a physical health composite score (PCS; α = .79), which included scores of physical functioning, role physical, bodily pain, and general health, and second, a mental health composite score (MCS; α = .86), which included scores of vitality, social functioning, role emotional, and mental health.14 Higher PCS and MCS scores indicated better physical and mental health, respectively. Scores were standardized to the general US population data using norm-based scoring, which employed a linear t-score transformation with a mean of 50 and a standard deviation of 10. Thus, scores higher than 50.0 suggest better physical or mental health than the general US population.
Medical Conditions
Respondents were prompted with a list of medical conditions (eg, depression; anxiety; attention deficit disorder, with or without hyperactivity [ADD/ADHD]) and endorsed any condition for which they felt they met the diagnostic criteria. Respondents noting that they had any of the listed conditions were then asked whether they (1) had ever been diagnosed by a physician or health professional with the condition, (2) had received medicine or treatment for the condition, and (3) had symptoms currently or within the last 3 months from the condition.
Maladaptive Behavioral Conditions
Alcohol dependence was assessed using the CAGE (cutting down, annoyance by criticism, guilty feeling, and eye-openers) questionnaire.7 The measure has been validated in multiple clinical and research settings.3,18 Respondents also identified whether they ever felt that they had problems with other behaviors, such as gambling, substance use other than alcohol, and uncontrolled eating (ie, binge eating, purging).
Statistical Analyses
Race was dichotomized as “non-Hispanic white” and “Hispanic or nonwhite.” Age (in years) was categorized as 24 years and younger, 25 to 34, 35 to 44, and 45 years and older. Body mass index (BMI) was computed based on World Health Organization classifications: underweight/normal (<25.0 kg/m2), overweight (25.0-29.9 kg/m2), and obese (≥30.00 kg/m2).37 To assess the relationship of contact level with study outcomes, we categorized primary sports as collision sports (eg, football, wrestling), high-contact sports (eg, basketball, field hockey, lacrosse, soccer), and low/noncontact sports (eg, baseball, cheerleading, diving, rowing, track and field). The school grade at which participants began playing their primary sport was categorized as grade school (grades kindergarten–grade 5), middle school (grades 6-8), high school (grades 9-12), and college. Consistent with previous research,9,10,15 we stratified concussion history data into 3 categories: 0 (referent), 1 to 2, and 3 or more concussions. We examined each maladaptive behavioral condition individually. CAGE scores were recoded into a dichotomous variable, with scores of 3 and 4 indicating alcohol dependence.18
PCS and MCS scores were compared with US normative data for the SF-36, overall, and by sex and age.35 Past research found that SF-36 and SF-12 scores had a high level of agreement and represent congruent markers of mental and physical health.34 Because our former collegiate athlete cohort did not include anyone younger than 18 years or older than 54 years, data from the 24-and-under and 45-and-over groups were compared respectively to the US normative data 18-to-24 and 45-to-54 age strata. Independent-sample t tests compared mean PCS and MCS scores between the former collegiate athlete cohort and the US population. Independent-sample t tests and analyses of variance (ANOVAs) with Tukey post hoc analyses compared mean PCS and MCS scores within the former collegiate athlete cohort by demographic, sports history, and concussion history groups.
Levels of significance for all analyses were set a priori at P < .05. All analyses were conducted with SAS version 9.3 (SAS Institute). The Institutional Review Board at the University of North Carolina at Chapel Hill approved all aspects of this study.
Results
We received data from 808 former collegiate athletes, of which 11 were excluded for incomplete data, leaving 797 for analysis. In addition, 10 members of the target population contacted us to inform us that they were former student managers as opposed to former athletes. This resulted in a completion rate of 21.9%. The majority of respondents were female (52.8%) and non-Hispanic white (86.1%) (Table 1). Ages ranged from 22 to 51 years, with most being between the ages of 25 and 44 years (79.4%). Most former collegiate athletes were underweight/normal weight (55.6%), although 22.2% of the 588 who were underweight/normal weight during the final year of their participation in collegiate sports were now overweight or obese, and 23.3% of those who were overweight were now obese.
TABLE 1.
Physical Health and Mental Health Composite Scores for Former Collegiate Athletes (N = 797)a
| Demographic Variable | % (n) | PCS, mean ± SD | MCS, mean ± SD |
|---|---|---|---|
| Total | 100.0 (797) | 53.0 ± 6.1 | 51.7 ± 9.4 |
| Sex | |||
| Male | 47.2 (376) | 52.7 ± 6.3 | 52.0 ± 9.3 |
| Female | 52.8 (421) | 53.2 ± 5.9 | 51.3 ± 9.5 |
| P | .28 | .29 | |
| Race/ethnicity | |||
| Non-Hispanic white | 86.1 (686) | 53.1 ± 6.0 | 51.5 ± 9.6 |
| Hispanic or nonwhiteb | 13.9 (111) | 52.3 ± 6.3 | 52.7 ± 8.6 |
| P | .19 | .19 | |
| Age, y | |||
| ≤24 | 5.4 (43) | 53.8 ± 5.1 | 48.9 ± 11.0 |
| 25-34 | 38.6 (308) | 53.6 ± 5.4 | 51.5 ± 9.7 |
| 35-44 | 40.8 (325) | 52.6 ± 6.5 | 52.6 ± 8.5 |
| ≥45 | 15.2 (121) | 52.3 ± 6.6 | 50.3 ± 10.2 |
| P | .08 | .02 | |
| BMI,c kg/m2 | |||
| Underweight/normal (<25.0) | 55.6 (443) | 54.0 ± 5.3 | 51.6 ± 9.4 |
| Overweight (25.0-29.9) | 33.1 (264) | 52.1 ± 6.6 | 51.9 ± 9.5 |
| Obese (≥30.00) | 11.3 (90) | 50.5 ± 6.8 | 51.2 ± 9.5 |
| P | <.001 | .82 |
aAll P values are from independent-samples t tests and analyses of variance comparing mean PCS and MCS scores among demographic groups. BMI, body mass index; MCS, mental health composite score; PCS, physical health composite score.
bOf the 111 “Hispanic or nonwhite” respondents, 71 were non-Hispanic black, 11 were non-Hispanic Asian/Pacific Islander, 9 were Hispanic, and 20 were mixed race.
cWorld Health Organization classifications.
Physical and Mental Health
Mean PCS and MCS scores (±SD) for the sample of former collegiate athletes were reported as 53.0 ± 6.1 and 51.7 ± 9.4, respectively. These scores were slightly higher than mean PCS and MCS scores for the US population (both mean, 50.0 ± 10.0; both P < .001).
Association of Demographics With Physical and Mental Health
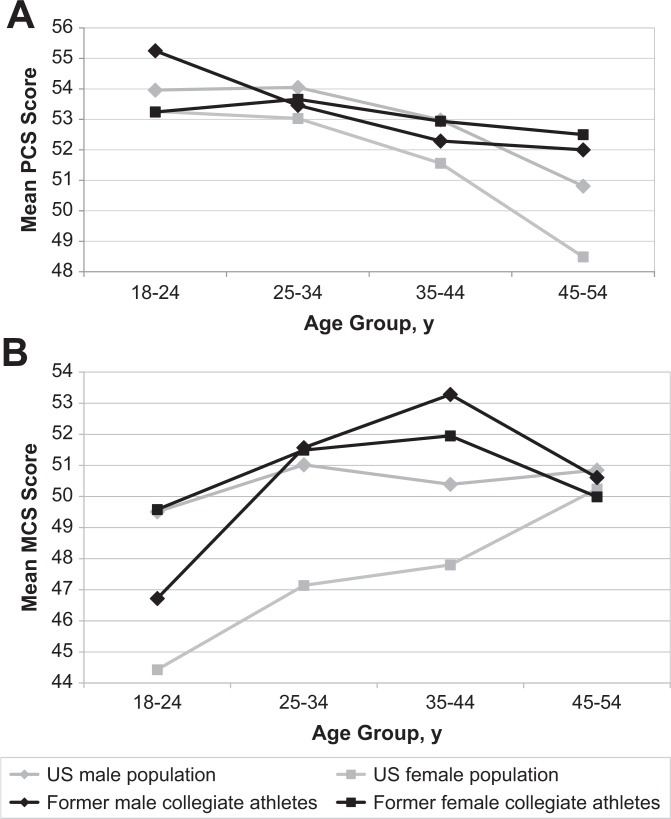
Because US population data included older individuals, we also computed scores for age and sex strata (Table 2). Although higher PCS scores were seen among the former collegiate athletes compared with US normative data, significant differences were only seen for females aged 35 to 44 years (difference, 1.4; P = .02) and 45 to 54 years (difference, 4.0; P < .001). Compared with US normative data, the downward trend in mean PCS scores across the life span was not as steep in the former collegiate athlete sample (Figure 1A). Mean MCS scores for former collegiate athletes were higher than those of US normative data among younger individuals (Figure 1B). However, significant differences were seen only among the 35 to 44–year age group for males (difference, 2.9; P < .001) and female groups younger than 45 years (18-24: difference, 5.2 [P = .02]; 25-34: difference, 4.4 [P < .001]; 35-44: difference, 4.1 [P < .001]). The PCS scores differed by BMI (P < .001), with underweight/normal-weight individuals having the highest scores. The MCS scores differed by age (P = .02), with mental health increasing from the 24-and-under to the 35-to-44 groups, and then decreasing in the 45-and-over group.
TABLE 2.
Physical Health and Mental Health Composite Scores by Sex and Age for Former Collegiate Athletes (N = 797) and US Population Normsa
| Variable | PCS, mean ± SD | MCS, mean ± SD |
|---|---|---|
| Sex = male, age = 18-24 y | ||
| Former collegiate athletes | 55.3 ± 5.7 | 46.7 ± 10.4 |
| US population norms | 54.0 ± 7.0 | 49.5 ± 7.1 |
| P a | .57 | .29 |
| Sex = male, age = 25-34 y | ||
| Former collegiate athletes | 53.5 ± 5.8 | 51.6 ± 10.5 |
| US population norms | 54.1 ± 6.6 | 51.0 ± 7.6 |
| P | .36 | .51 |
| Sex = male, age = 35-44 y | ||
| Former collegiate athletes | 52.3 ± 6.6 | 53.3 ± 7.8 |
| US population norms | 53.0 ± 7.6 | 50.4 ± 9.6 |
| P | .28 | <.001 |
| Sex = male, age = 45-54 y | ||
| Former collegiate athletes | 52.0 ± 6.5 | 50.6 ± 9.8 |
| US population norms | 50.8 ± 9.4 | 50.9 ± 10.1 |
| P | .32 | .85 |
| Sex = female, age = 18-24 y | ||
| Former collegiate athletes | 53.2 ± 4.8 | 49.6 ± 11.2 |
| US population norms | 53.3 ± 7.2 | 44.4 ± 11.4 |
| P | .99 | .02 |
| Sex = female, age = 25-34 y | ||
| Former collegiate athletes | 53.7 ± 5.2 | 51.5 ± 9.1 |
| US population norms | 53.0 ± 7.9 | 47.1 ± 10.7 |
| P | .31 | <.001 |
| Sex = female, age = 35-44 y | ||
| Former collegiate athletes | 52.9 ± 6.5 | 51.9 ± 9.2 |
| US population norms | 51.6 ± 8.6 | 47.8 ± 10.4 |
| P | .02 | <.001 |
| Sex = female, age = 45-54 y | ||
| Former collegiate athletes | 52.5 ± 6.7 | 50.0 ± 10.7 |
| US population norms | 48.5 ± 10.5 | 50.2 ± 9.8 |
| P | <.001 | .85 |
aAll P values are from independent-samples t tests and analyses of variance comparing mean PCS and MCS scores between former collegiate athletes and US population norms. MCS, mental health composite score; PCS, physical health composite score.
Figure 1.
Mean VR-12 physical health composite scores (A) and mental health composite scores (B) of former collegiate athletes, compared with US population, by sex. MCS, mental health composite score; PCS, physical health composite score; VR-12, Veterans RAND 12-Item Health Survey.
Sports and Concussion History
Respondents played in 29 primary sports during college (Table 3), with the largest proportions of respondents having played men’s football (9.4%), women’s rowing (8.3%), men’s fencing (6.8%), women’s track and field (6.5%), and women’s fencing (6.0%). Most respondents began playing their primary collegiate sport in grade school (45.3%) (Table 4). Also, 11.5% played their primary sport professionally. Last, 16.2% sustained a career-ending injury, which was sustained an average 14.2 ± 7.7 years ago. However, the difference between current and college BMI in those with a career-ending injury (mean, 1.6 ± 3.1 kg/m2) and those without a career-ending injury (mean, 1.3 ± 3.0 kg/m2) did not differ (P = .25).
TABLE 3.
Distributions of Former Collegiate Athlete Cohort by Sport
| Sport | Former Collegiate Athlete Cohort | |
|---|---|---|
| n | % | |
| Men’s baseball | 31 | 3.9 |
| Men’s basketball | 22 | 2.8 |
| Men’s cross-country | 8 | 1.0 |
| Men’s fencing | 54 | 6.8 |
| Men’s football | 75 | 9.4 |
| Men’s lacrosse | 35 | 4.4 |
| Men’s soccer | 22 | 2.8 |
| Men’s swimming and diving | 44 | 5.4 |
| Men’s tennis | 13 | 1.6 |
| Men’s track and field | 34 | 4.3 |
| Men’s wrestling | 27 | 3.4 |
| Women’s basketball | 14 | 1.8 |
| Women’s cross-country | 14 | 1.8 |
| Women’s fencing | 48 | 6.0 |
| Women’s field hockey | 29 | 3.6 |
| Women’s golf | 16 | 2.0 |
| Women’s gymnastics | 21 | 2.6 |
| Women’s lacrosse | 25 | 3.1 |
| Women’s rowing | 66 | 8.3 |
| Women’s soccer | 30 | 3.8 |
| Women’s softball | 30 | 3.8 |
| Women’s swimming and diving | 45 | 5.6 |
| Women’s tennis | 11 | 1.4 |
| Women’s track and field | 52 | 6.5 |
| Women’s volleyball | 27 | 3.4 |
| Cheerleading | 3 | 0.4 |
| Equestriana | 1 | 0.1 |
| Total | 797 | 100.0 |
aEquestrian was considered a club sport.
TABLE 4.
Physical Health and Mental Health Composite Scores for Former Collegiate Athletes (N = 797) by Sports Historya
| Characteristic | % (n) | PCS, mean ± SD | MCS, mean ± SD |
|---|---|---|---|
| Level of contact in sportb | |||
| Collision | 12.8 (102) | 51.4 ± 7.3 | 53.0 ± 8.7 |
| High contact | 22.2 (177) | 51.9 ± 6.5 | 51.4 ± 11.0 |
| Low/noncontact | 65.0 (518) | 53.6 ± 5.6 | 51.5 ± 9.0 |
| P | <.001 | .29 | |
| Time started playing collegiate sport | |||
| Grade school (grades K to 5) | 45.3 (348) | 52.9 ± 6.3 | 52.0 ± 9.1 |
| Middle school (grades 6-8) | 22.6 (174) | 52.7 ± 5.5 | 52.6 ± 9.7 |
| High school (grades 9-12) | 14.3 (110) | 52.7 ± 6.4 | 50.3 ± 10.8 |
| College | 17.8 (137) | 54.0 ± 5.2 | 51.0 ± 8.3 |
| Missing | 28 | ||
| P | .17 | .16 | |
| Played professional sports | |||
| No | 88.5 (705) | 53.0 ± 6.1 | 51.5 ± 9.3 |
| Yes | 11.5 (92) | 52.6 ± 6.0 | 52.6 ± 10.1 |
| P | .48 | .30 | |
| Sustained career-ending injury | |||
| No | 83.8 (667) | 53.5 ± 5.5 | 51.4 ± 9.5 |
| Yes | 16.2 (129) | 50.3 ± 8.1 | 52.8 ± 9.1 |
| Missing | 1 | ||
| P | <.001 | .11 | |
| Total number concussions sustained | |||
| 0 | 61.2 (485) | 53.4 ± 5.5 | 52.3 ± 8.9 |
| 1-2 | 26.9 (213) | 52.9 ± 6.5 | 50.7 ± 10.1 |
| ≥3 | 11.9 (94) | 50.9 ± 7.6 | 50.4 ± 10.5 |
| Missing | 5 | ||
| P | <.001 | .06 |
aSports history pertains to primary sport (ie, the sport in which the respondent was most invested). All P values are from independent-samples t tests and analyses of variance comparing mean PCS and MCS scores among demographic groups. MCS, mental health composite score; PCS, physical health composite score.
bLevels of contact in sport: collision = men’s football and wrestling; high contact = men’s basketball, lacrosse, soccer, and women’s basketball, field hockey, lacrosse, and soccer; low/noncontact = men’s baseball, cross-country, diving, fencing, swimming, tennis, track and field, and women’s cross-country, diving, equestrian, fencing, golf, gymnastics, rowing, softball, swimming, tennis, track and field, volleyball, and cheerleading.
A total of 307 (38.8%) former collegiate athletes sustained at least 1 concussion (Table 4). Of these, 94 sustained 3 or more concussions.
Associations of Sports and Concussion History With Physical and Mental Health
Differences in mean PCS scores existed among sport contact levels, with former collegiate athletes from low-contact/noncontact sports having higher PCS scores than former collegiate athletes from collision and high-contact sports (P < .001) (Table 4). Those sustaining a career-ending injury also had lower PCS scores (50.3 vs 53.5; P < .001). In addition, PCS scores decreased with a longer duration of time since sustaining a career-ending injury (Pearson r, –0.18; P = .04). There were no differences in MCS scores according to sports history. No association was found between MCS scores and longer duration of time since sustaining a career-ending injury (Pearson r, 0.04; P = .67).
PCS scores were lowest among those sustaining 3 or more concussions in total (P < .001) (Table 4). However, MCS scores were not significantly different (P = .06).
History of Medical Conditions and Maladaptive Behavioral Conditions
The medical conditions most commonly self-reported by the former collegiate athlete cohort included general anxiety (16.2%), hypercholesterolemia/high cholesterol (10.6%), depression (10.4%), and ADD/ADHD (9.7%) (Table 5). Across all conditions probed, physicians diagnosed 61.9% of the 619 medical conditions reported. In addition, 58.0% were currently symptomatic or had been symptomatic in the past 3 months, and 40.5% were currently being treated for the medical condition endorsed.
TABLE 5.
Medical History in Cohort of Former Collegiate Athletes (N = 797)
| Medical Condition | With Medical Condition, % (n) | With Physician Diagnosis, % (n) |
|---|---|---|
| Cardiovascular | ||
| Coronary heart disease/heart attack | 0.9 (7) | 0.6 (5) |
| Hypercholesterolemia/high cholesterol | 10.6 (84) | 9.3 (74) |
| High blood pressure/hypertension | 8.7 (69) | 6.6 (53) |
| Sleep apnea | 6.2 (49) | 3.4 (27) |
| Cognitive | ||
| Mild cognitive impairment/memory impairment | 3.8 (30) | 0.6 (5) |
| Learning disability | 2.9 (23) | 2.3 (18) |
| Mental health | ||
| Depression | 10.4 (82) | 7.3 (58) |
| Bipolar disorder | 0.8 (6) | 0.5 (4) |
| Impulse control disorder/conduct disorder | 1.1 (9) | 0.4 (3) |
| Attention deficit disorder, with or without hyperactivity | 9.7 (77) | 5.4 (43) |
| Anxiety | 16.2 (128) | 7.8 (62) |
| Physical health | ||
| Vestibular disorder/vertigo | 2.0 (16) | 1.4 (11) |
| Chronic headache syndrome | 4.9 (39) | 2.5 (20) |
There were 92 (11.5%) respondents who endorsed maladaptive behavioral conditions. The most commonly cited maladaptive behavioral conditions were uncontrolled eating (5.8%) and alcohol dependence (5.8%) (Table 6).
TABLE 6.
Maladaptive Behavioral Conditions in Cohort of Former Collegiate Athletes (N = 797)
| Maladaptive Behavioral Condition | % (n) |
|---|---|
| Alcohol dependence | |
| No | 94.2 (733) |
| Yes | 5.8 (45) |
| Missing | 19 |
| Substance usea | |
| No | 97.1 (774) |
| Yes | 2.9 (23) |
| Gambling | |
| No | 99.0 (789) |
| Yes | 1.0 (8) |
| Uncontrolled eatingb | |
| No | 94.2 (751) |
| Yes | 5.8 (46) |
aIncludes cigarettes, cigars, and illicit substances.
bIncludes binge eating and purging.
Discussion
Although much research has focused on the current health of former professional athletes,8–10,15,29 there is a dearth of literature related to those athletes that had participated at lower, yet still elite, levels of competition. Our findings, which utilized a diverse cohort of 797 former collegiate athletes that included both males and females from 29 different sports, found that PCS and MCS scores in our sample were similar to those of the general US population, after adjusting for age and sex. In addition, we found that the age-related decline in physical health among former collegiate athletes was not as rapid as that of the general US population, which may illustrate a long-term benefit of elite sport participation. Although not directly examined in the current study, athletes competing at the elite levels may have established a pattern of physical activity and nutrition that when continued, may provide benefits in physical health beyond formal sport participation. Longitudinal research using valid and reliable measures of physical activity (eg, pedometers, accelerometers, activity logs) and nutrition (eg, detailed nutrition logs) is needed to substantiate this possibility. We also caution that this finding may also reflect subtle selection factors (eg, a person with chronic illnesses may be less likely to become a collegiate athlete).
Caution must be taken in interpreting such findings. First, although we report statistically significant differences between groups, these differences may be too small and within the range of the minimum clinically important differences (MCIDs) for the VR-12, which various studies have stipulated range from 2.0 to 5.0.1,24,31 Second, compared with the sample of Simon and Docherty30 (aged 40-65 years), our sample was younger, ranging from 22 to 51 years. Our age- and sex-stratified data were also based on cross-sections by age, and we thus cannot determine causality by age. Moving forward, longitudinal studies should further examine the physical and mental health of former collegiate athletes across the life span to better ascertain comparisons and interpretations relative to normative data. Furthermore, research that includes nonathlete controls and incorporates additional moderating variables, such as socioeconomic status and access to medical care, could add meaning to future work by further delineating current findings.
Simon and Docherty30 utilized the Patient-Reported Outcomes Measurement Information System (PROMIS) to evaluate health-related quality of life in a cohort of former collegiate athletes. Former athletes reported lower scores for physical function, depression, fatigue, sleep, and pain interference than did “nonathlete” controls of similar ages who were physically active during college. However, compared with general US population data, former collegiate athletes only had lower scores for physical function and pain interference. The authors speculated that former athletes might sustain injuries during college that inhibit later quality of life, whereas nonathletes may not engage in enough rigorous physical activity to affect their later health. Likewise, we found in our study that despite career-ending injuries occurring on average 14 years ago, those former collegiate athletes in our cohort with career-ending injuries may have lower levels of physical health than do former collegiate athletes without career-ending injuries. Accordingly, sports-related injuries that athletes sustain during their sports careers may have important long-term effects on their future physical health. These injuries may inhibit the former athletes’ ability to stay physically active. Although weight gain, as measured by change in BMI, was not found to be larger among those individuals that had sustained a career-ending injury, it is important to utilize measures of physical health such as the VR-12 to better examine numerous facets of health and well-being.
Nevertheless, the previous research and the current findings suggest a number of former collegiate athletes have deficiencies in their mental and physical health associated with their sports participation that may require additional care. Thus, former athletes may need assistance in obtaining the necessary resources to manage and treat both specific physical and mental conditions beyond their intercollegiate athletic careers. Organizations for professional sports, such as the NFL Players Association, offer postcareer health insurance to its former players. As a result of the needs identified in the current study, transition programming including education on health care resources and/or postcareer health insurance for a predetermined amount of time postretirement may both be beneficial for former collegiate athletes. If the NCAA were to offer such resources, it would need to conduct feasibility studies that evaluate need, demand, and cost in relation to former collegiate athlete mental and physical health outcomes across the life span.
Athletes that sustained a career-ending injury but had a longer period of time out of sports may have had sufficient time since sustaining the injury to cope with initial disenchantment with retirement and transition successfully into a post–sports career lifestyle.2,4,11 This is consistent with conceptual models describing injury as an important factors in an athlete’s psychological responses to career transition.32 However, we did not find an association between mental health and duration since sustaining a career-ending injury. Because of the cross-sectional nature of the data, future prospective cohort studies should examine the association of injury and markers of physical and mental health longitudinally. Still, study results support the need for clinicians working with former athletes to acquire a detailed injury history (including concussion history) to better understand and attend to their current health needs.
Independent of having sustained a career-ending injury, we found that a large number of former collegiate athletes were currently overweight/obese despite having a normal BMI during their collegiate sports careers. Such weight gain is of concern given the associated increased risk of cardiovascular disease.25 Although increases in BMI occur with age among nonathletes,28 student-athletes transitioning from college sports in particular may decrease their physical activity yet maintain their dietary habits, while struggling sans guidance from their former collegiate team staff. Interventions beginning at the end of a collegiate athlete’s career may help former student athletes independently manage their physical activity levels and dietary needs upon leaving collegiate sports.
Approximately 4 in 10 former collegiate athletes reported sustaining at least 1 concussion. Former collegiate athletes’ physical health was associated with recurrent self-reported concussion history, which adds to the increasing number of recent studies that have examined the long-term effects of multiple self-reported concussions in former athletes.9,10,15 However, despite the large prevalence of former athletes reporting concussions, our study did not find an association between recurrent concussion and markers of mental health. It is possible that our sample was too young to detect suggested earlier onsets of mental health issues in former professional athletes.10 Building on study findings, we advocate continued examination of the physical and mental health of former collegiate and professional athletes. Such work will help to better determine more precise age ranges at which disparities in health due to concussion symptomology and the onset of negative mental health outcomes may occur. This important knowledge could inform targeted intervention and treatment efforts designed to mitigate the potential negative long-term outcomes of concussion in former athlete populations.
Last, our study examined the prevalence of specific medical conditions and maladaptive behavioral conditions in the cohort of former collegiate athletes. Approximately 40% of the reported medical conditions were not diagnosed by a physician, nor were they being treated. However, it is possible that many medical conditions were undiagnosed and untreated because athletes were asymptomatic at the time of study participation. In addition, compared with recent World Health Organization data representative of the US population,16,17 former collegiate athletes had a higher prevalence of both alcohol dependence and eating disorders and a lower prevalence of depression, bipolar disorders, and ADD/ADHD. Although differences may reflect methodological differences in data collection and demographics, the findings suggest there could be a benefit to providing former collegiate athletes with medical care to treat and manage a variety of mental health conditions. At the same time, former athletes may benefit from continued social support from other former athletes and other significant members of their social networks (eg, parents, spouse, nonsport friends). Extant research5 supports a conceptual model that highlights the importance of social support to the psychological health of current student-athletes27 and athletes transitioning into retirement.19 However, no social support interventions exist, to our knowledge, that aim to enhance the experience of former professional or high-level amateur athletes who have been out of sports for an extended period. Accordingly, the development and careful evaluation of such programs represents a potentially fruitful area for future research and practice.
Limitations
Our primary limitation is that only 21.9% of all eligible former collegiate athletes provided complete responses. In addition, our sample was recruited from 1 Division I (highest competition level for NCAA athletics) university and was restricted to those that had played at least 1 season in 1987-2012. Thus, our findings may be prone to selection bias and may not be generalizable to other populations of former athletes from other schools, divisions, regions, or playing levels. Future research examining former athletes from multiple sports organizations of varying competition levels would present a broader perspective on the mental and physical health of former athletes. Second, because single-item measures account for many of the domains (ie, bodily pain, social functioning) that yield the VR-12 PCS and MCS scores, our measures may not have assessed overall current physical and mental health accurately and/or with much depth. In addition, unlike the longer VR-36 and SF-36 modules, it is not recommended that VR-12 and SF-12 be used to examine domain scores.33 We opted for the VR-12 to deter survey fatigue, as our questionnaire covered a wide range of topics related to current health, medical history, and sports history. However, future research may opt to use the VR-36 for more in-depth examinations of specific components of physical and mental health. Third, our examination of medical conditions was subjective, and we were not able to ascertain recurrence or severity. At the same time, we did not have any method to link current health to playing college sports. We also did not include additional medical conditions such as those related to musculoskeletal conditions. These delimitations of the sample afford future study, as chronic and severe medical conditions may exhibit a stronger negative association with current athlete mental and physical health than acute or less severe conditions. Fourth, it is possible that social desirability bias may have affected our ascertainment of data related to maladaptive behavioral conditions. To address this important concern, future research could attempt to oversample specifically diagnosed or impaired groups, triangulate recollections of collegiate injury experiences with athletic department records, and/or utilize measures with imbedded social desirability indices. Despite these limitations, our study provides estimates of the current mental and physical health in a large and unique population of former collegiate athletes.
Conclusion
In contrast to previous research,30 our study found that the overall physical and mental health of former collegiate athletes is similar to that of the general US population. However, the health and well-being of some groups of former collegiate athletes may be negatively affected by previously sustained injuries, particularly concussions and injuries that were career ending. The number of medical conditions and mental health issues that affect this cohort emphasize the need for access to health care resources for former high-level athletes across their postsports life span. Although much emphasis has been placed on the postretirement health of professional athletes,15,26 our findings warrant attention to the health of former collegiate athletes as well, particularly given the large number of high-level collegiate athletes that never play professionally.21 Future studies can help inform, develop, and implement interventions that utilize multiple forms of social support and facilitate health care access to help positively influence the physical and mental health and well-being of former collegiate athletes.
Supplementary Material
Acknowledgment
The Veterans RAND 12-Item Health Survey was developed from the Veterans RAND 36-Item Health Survey, which was developed and modified from the original RAND version of the 36-item Health Survey version 1.0 (also known as the MOS SF-36).
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: The Matthew A. Gfeller Sport-Related Traumatic Brain Injury Research and The Center for the Study of Retired Athletes are funded by private donations and various grant funding agencies interested in understanding the current and late-life consequences and benefits of sports participation. The Injury Prevention Research Center is partially supported by the National Center for Injury Prevention and Control to facilitate research that increases our knowledge of the consequences of injuries and opportunities for injury prevention.
References
- 1. Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391. [DOI] [PubMed] [Google Scholar]
- 2. Atchley R, Barusch A. Social Forces and Aging. Belmont, CA: Wadsworth; 2004. [Google Scholar]
- 3. Bernadt MW, Mumford J, Taylor C, Smith B, Murray RM. Comparison of questionnaire and laboratory tests in the detection of excessive drinking and alcoholism. Lancet. 1982;1 (8267):325–328. [DOI] [PubMed] [Google Scholar]
- 4. Dave D, Rashad R, Spasojevic J. The effects of retirement on physical and mental health outcomes. South Econ J. 2008;75:497–523. [Google Scholar]
- 5. DeFreese J, Smith AL. Teammate social support, burnout, and self-determined motivation in collegiate athletes. Psychol Sport Exerc. 2013;14:258–265. [Google Scholar]
- 6. Didehbani N, Cullum CM, Mansinghani S, Conover H, Hart J. Depressive symptoms and concussions in aging retired NFL players. Arch Clin Neuropsychol. 2013;28:418–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905–1907. [DOI] [PubMed] [Google Scholar]
- 8. Golightly YM, Marshall SW, Callahan LF, Guskiewicz K. Early-onset arthritis in retired National Football League players. J Phys Act Health. 2009;6:638–643. [DOI] [PubMed] [Google Scholar]
- 9. Guskiewicz KM, Marshall SW, Bailes J, et al. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005;57:719–726. [DOI] [PubMed] [Google Scholar]
- 10. Guskiewicz KM, Marshall SW, Bailes J, et al. Recurrent concussion and risk of depression in retired professional football players. Med Sci Sports Exerc. 2007;39:903–909. [DOI] [PubMed] [Google Scholar]
- 11. Holcomb TF, Miller TW. Transitioning into retirement as a stressful life event In: Miller TW, ed. Handbook of Stressful Transitions Across the Lifespan. New York, NY: Springer; 2010:133–146. [Google Scholar]
- 12. Kallus KW, Kellmann M. Burnout in athletes and coaches In: Hanin YL, ed. Emotions in Sport. Champaign, IL: Human Kinetics; 2000:209–230. [Google Scholar]
- 13. Kazis LE, Miller DR, Clark JA, et al. Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the Veterans Health Study. J Ambul Care Manage. 2004;27:263–280. [DOI] [PubMed] [Google Scholar]
- 14. Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DRV. Veterans RAND 12-item Health Survey (VR-12): A white paper summary. 2008. http://www.hosonline.org/surveys/hos/download/Veterans_RAND_12_Item_Health_Survey_White_Paper_Summary.pdf. Accessed March 10, 2014.
- 15. Kerr ZY, Marshall SW, Harding HP, Guskiewicz KM. Nine-year risk of depression diagnosis increases with increasing self-reported concussions in retired professional football players. Am J Sports Med. 2012;40:2206–2212. [DOI] [PubMed] [Google Scholar]
- 16. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. [DOI] [PubMed] [Google Scholar]
- 17. Kessler RC, Berglund PA, Chiu WT, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health surveys. Biol Psychiatry. 2013;73:904–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kitchens JM. Does this patient have an alcohol problem? JAMA. 1994;272:1782–1787. [PubMed] [Google Scholar]
- 19. Lavallee D, Gordon S, Grove JR. Retirement from sport and the loss of athletic identity. J Person Interperson Loss. 1997;2:129–147. [Google Scholar]
- 20. Malina RM. Early sport specialization: roots, effectiveness, risks. Curr Sports Med Rep. 2010;9:364–371. [DOI] [PubMed] [Google Scholar]
- 21. National Collegiate Athletic Association. Estimated probability of competing in athletics beyond the high school interscholastic level. 2012. http://www.ncaa.org/wps/wcm/connect/public/ncaa/pdfs/2012/estimated+probability+of+competing+in+athletics+beyond+the+high+school+interscholastic+level. Accessed March 9, 2014.
- 22. National Collegiate Athletic Association. NCAA student-athlete participation hits 450,000. 2013. http://www.ncaa.org/wps/wcm/connect/public/NCAA/Resources/Latest+News/2012/September/NCAA+student-athlete+participation+hits+450000 . Accessed March 9, 2014. [Google Scholar]
- 23. National Federation of State High School Associations. High school sports participation increases for 24th consecutive year. 2013. http://www.nfhs.org/content.aspx?id=9628. Accessed March 9, 2014.
- 24. Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–592. [DOI] [PubMed] [Google Scholar]
- 25. Pihl E, Jürimäe T. Relationships between body weight change and cardiovascular disease risk factors in male former athletes. Int J Obes Relat Metab Disord. 2001;25:1057–1062. [DOI] [PubMed] [Google Scholar]
- 26. Reider B. Melancholy thoughts. Am J Sports Med. 2012;40:2197–2199. [DOI] [PubMed] [Google Scholar]
- 27. Richman JM, Hardy CJ, Rosenfeld LB, Callanan RA. Strategies for enhancing social support networks in sport: a brainstorming experience. J Appl Sport Psychol. 1989;1:150–159. [Google Scholar]
- 28. Saarni S, Rissanen A, Sarna S, Koskenvuo M, Kaprio J. Weight cycling of athletes and subsequent weight gain in middleage. Int J Obes. 2006;30:1639–1644. [DOI] [PubMed] [Google Scholar]
- 29. Schwenk TL, Gorenflo DW, Dopp RR, Hipple E. Depression and pain in retired professional football players. Med Sci Sports Exerc. 2007;39:599–605. [DOI] [PubMed] [Google Scholar]
- 30. Simon JE, Docherty CL. Current health-related quality of life is lower in former Division I collegiate athletes than in non-collegiate athletes. Am J Sport Med. 2014;42:423–429. [DOI] [PubMed] [Google Scholar]
- 31. Strand V, Singh JA. Improved health-related quality of life with effective disease-modifying antirheumatic drugs: evidence from randomized controlled trials. Am J Manag Care. 2007;13 (suppl 9):S237–S251. [PubMed] [Google Scholar]
- 32. Taylor J, Lavallee D. Career transitions among elite athletes: is there life after sports? In: Williams JM, ed. Applied Sport Psychology: Personal Growth to Peak Performance. 6th ed New York, NY: McGraw-Hill; 2010:542–562. [Google Scholar]
- 33. Ware J, Jr, Kosinski M, Keller SD. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed] [Google Scholar]
- 34. Ware J, Kosinski M, Keller S. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston, MA: The Health Institute; 1994. [Google Scholar]
- 35. Ware J, Kosinski M, Keller S. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scores. 3rd ed Lincoln, RI: QualityMetric; 1998. [Google Scholar]
- 36. Woods R. Social Issues in Sports. Champaign, IL: Human Kinetics; 2011. [Google Scholar]
- 37. World Health Organization. BMI classification. 2013. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed March 9, 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.