Abstract
Background:
A delay in pediatric and adolescent anterior cruciate ligament (ACL) reconstruction is associated with an increase in the number of concomitant meniscal and chondral injuries. Factors that contribute to this delay have not been well described.
Hypothesis:
Socioeconomic and demographic factors are related to ACL surgery timing.
Study Methods:
Cohort study; Level of evidence, 3.
Methods:
All subjects who underwent primary ACL reconstruction at a single tertiary pediatric hospital between 2005 and 2012 were retrospectively reviewed. Variables included concomitant knee injuries (cartilage or meniscus injuries requiring additional operative treatment) and chronologic, demographic, and socioeconomic factors. Multivariable Cox proportional-hazards analyses were used to identify factors related to ACL surgery timing.
Results:
The mean age of the 272 subjects was 15.2 ± 2.12 years. Time to surgery was significantly different among subjects who required multiple additional surgical procedures at time of ACL reconstruction (median, 3.3 months) compared with subjects with 1 (median, 2.0 months) or no additional injuries (median, 1.6 months). Subjects underwent ACL reconstruction significantly sooner if they were older at the time of injury (hazard ratio [HR], 1.2 per 1 year; 95% CI, 1.1-1.2; P < .0001) or were covered by a commercial insurance plan (HR, 2.0; 95% CI, 1.6-2.6; P < .0001). Median time to ACL surgery was 1.5 months (95% CI, 1.3-1.7) for subjects with commercial insurance plans compared with 3.0 months (95% CI, 2.3-3.3) for subjects with noncommercial insurance coverage.
Conclusion:
The risk of delayed ACL surgery was significantly higher among pediatric and adolescent subjects who were less affluent, who were covered by a noncommercial insurance plan, and who were younger. This study also confirms previous studies that have reported an association between a delay in ACL surgery and the presence of additional knee injuries requiring operative treatment, accentuating the importance of timely care.
Clinical Relevance:
Access to care is a current area of research interest and health policy formation. Information in this arena drives 2 important aspects of health: most immediately, care provided to patients, and over a broader scope, the policy that directs health care. The orthopaedic surgeon should be aware of the association between socioeconomic and demographic factors and ACL surgery timing to optimize outcomes.
Keywords: ACL reconstruction, delay in surgery, socioeconomic factors
Research has demonstrated that a delay in pediatric and adolescent anterior cruciate ligament (ACL) reconstruction for complete ligament disruption is associated with an increase in the prevalence and severity of concomitant meniscal and chondral injuries.3,5,8,9 Lawrence et al8 reported that when patients delayed their surgery for greater than 12 weeks, they were significantly more likely to present with chondral and meniscal injuries during their primary ACL reconstruction. These increased injuries portend a worse long-term prognosis, increased future medical expenses, and a need for additional surgical procedures during the ACL reconstruction. The treatment of additional injuries may also be associated with delays in the rehabilitation protocol and in return to sport.
The incidence of ACL injuries in this population has been shown to be increasing, in part due to more participation in year-round training, single-sport specialization, and an increase in high-demand sports.14 For these reasons, the pediatric ACL injury is a current area of research focus. For those patients who are symptomatic and demonstrate instability, it is now recognized that a delay to treatment of the pediatric ACL injury leads to worse outcomes. The factors that contribute to a delay in diagnosis and treatment of ACL injuries in the pediatric population have not been addressed in the literature. While there has been a paradigm shift regarding the treatment of these injuries, there is little known about the reason for continued delayed presentation to surgery among this population.4 If factors that contribute to a delay in reconstruction of the ACL are better understood, more attention, advocacy, and appropriately directed resources may help to expeditiously recognize and treat these injuries and subsequently decrease the prevalence of concomitant intra-articular pathology.
Discrepancies in the access to and delivery of health care on the basis of socioeconomic factors have received increased attention in recent years. Timely delivery of health care is especially important among patients with ACL tears due to the association between a delay in surgery and subsequent knee deterioration. Therefore, the primary purpose of this study was to identify demographic and socioeconomic factors related to the timing of ACL surgery following the initial knee injury. We hypothesized that socioeconomic and demographic factors are related to the timing of reconstruction following the initial ACL injury.
Materials and Methods
After appropriate institutional review board approval was obtained, a query of International Classification of Diseases, 9th Revision (ICD-9) diagnostic and Current Procedural Terminology (CPT) procedural codes was used to identify all subjects who underwent primary ACL reconstruction surgery at a single, large-volume, tertiary-level pediatric hospital between 2005 and 2012. A retrospective chart review was used to collect demographic, clinical, and socioeconomic variables from patients younger than 19 years at the time of injury. Exclusion criteria included the following: subjects with missing information, a history of a previous ipsilateral knee trauma unrelated to their presenting complaint of ACL injury, or those patients who underwent surgery at an outside hospital.
Demographic variables of interest included: age at injury, race, ethnicity, sex, height, and weight. Body mass index (BMI) percentiles were calculated using a publicly available program on the Centers for Disease Control and Prevention’s website.1 Obesity was defined as a BMI greater than the 95th percentile.7 Socioeconomic variables included household income and insurance type. Household income was estimated based on the median income associated with each of the subject’s home ZIP codes. This information was obtained from US Census Bureau data.15 Insurance type was classified as commercial, government assisted, or uninsured.
Clinical information included time in months from injury to surgery, time from injury to initial orthopaedic evaluation, time from injury to magnetic resonance imaging (MRI) examination, and time from orthopaedic evaluation to ACL reconstructive surgery. Subjects who elected to move forward with surgery followed a standard preoperative protocol that included activity modification, therapy to regain full motion, and monitoring for resolution of effusion prior to surgery. The presence and treatment of all chondral and meniscal injuries identified during the ACL reconstruction were recorded. Knee injuries that required additional operative procedures at the time of ACL reconstruction were included in the analysis. The severity of the knee injury was defined as number of additional knee injuries requiring operative treatment (no injuries, 1 injury, or multiple injuries). For meniscal injuries, additional procedures were defined as: trephination, debridement, repair, and partial or complete meniscectomy. Cartilage procedures were categorized as chondroplasty and microfracture.
Statistical Analysis
The demographics and clinical characteristics of all subjects were summarized using descriptive statistics. A Kaplan-Meier time to event analysis was used to evaluate the relation between time to surgery and knee injury severity or the number of additional injuries requiring operative treatment. Univariate Cox proportional-hazards regression models were then used to identify demographic and socioeconomic variables related to the hazard of ACL surgery following initial injury. Hazard of surgery represents the relative likelihood of a subject undergoing ACL surgery. Factors significant at the alpha level of 0.10 were considered for inclusion in the final model. A backward selection strategy was then used to eliminate nonsignificant variables. Only variables significant at the 0.05 alpha level were included in the final multivariable Cox proportional-hazards regression model. Due to the small number of uninsured subjects in our cohort, insurance status was defined as commercial versus noncommercial. The noncommercial category included subjects with government-assisted insurance plans as well as uninsured subjects. Secondary multivariable Cox proportional-hazards regression analyses were used to determine whether variables significantly related to the time from injury to ACL surgery in the primary analysis were also related to the following time periods of interest: (1) time from injury to orthopaedic evaluation, (2) time from orthopaedic evaluation to ACL surgery, and (3) time from injury to MRI evaluation. Hazard ratios were used to estimate the effect sizes associated with all variables significantly related to the hazard of ACL surgery in the Cox proportional-hazards regression models. Finally, multivariable ordinal logistic regression analyses were used to examine the relationship between demographic and socioeconomic factors and knee injury severity. Only variables significantly related to ACL surgery timing in the primary analysis were evaluated in the multivariable ordinal logistic regression models.
Results
A total of 272 subjects were included in the cohort. Figure 1 provides a complete summary of subject enrollment. The mean age at injury was 15.2 ± 2.12 years. Based on ZIP code, the mean household income was US$66,066 ± $23,263. More information about the demographics and clinical characteristics of the subjects included in the cohort is presented in Table 1. The median number of months from initial injury to surgery was 1.95 months (range, 0.26-62.46 months).
Figure 1.
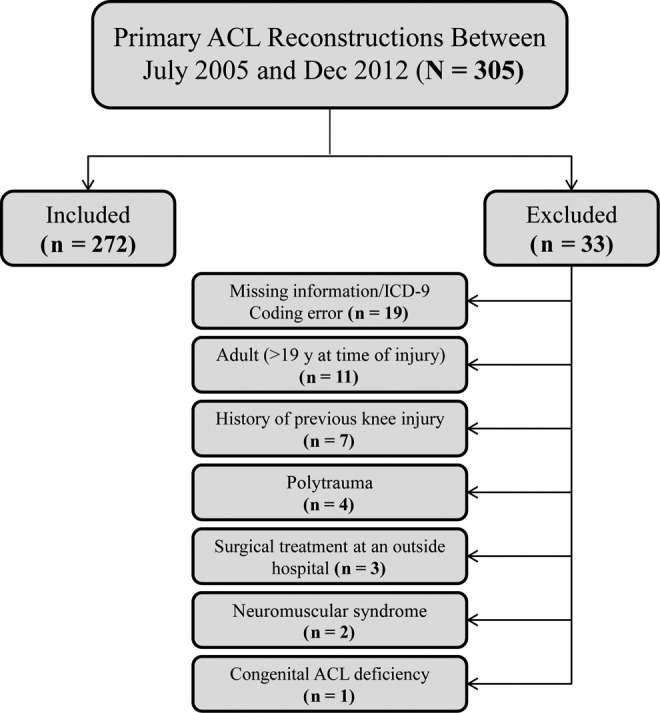
Summary of subject enrollment.
TABLE 1.
Demographics and Clinical Characteristics
| n | % | |
|---|---|---|
| Sex | ||
| Female | 125 | 45.96 |
| Male | 147 | 54.04 |
| Race | ||
| Asian | 3 | 1.12 |
| Black | 22 | 8.18 |
| White | 188 | 69.89 |
| Other | 56 | 20.82 |
| Ethnicity | ||
| Hispanic | 64 | 23.70 |
| Non-Hispanic | 206 | 76.30 |
| Insurance status | ||
| Commercial | 166 | 61.48 |
| Government-assisted | 81 | 30.00 |
| Uninsured | 23 | 8.52 |
| Obesity | ||
| Nonobese | 221 | 82.77 |
| Obese | 46 | 17.23 |
| Age at injury, y, mean ± SD | 15.2 ± 2.12 | |
| Household income, US$, mean ± SD | 66,066 ± 23,263 | |
Intraoperatively, 22% were affected by multiple additional knee injuries requiring operative treatment, 39% of subjects were affected by 1 additional injury, and 39% required ACL reconstruction only (no additional injuries). There was a significant association between knee injury severity and the time from initial injury to ACL surgery (P < .0001). The timing of ACL surgery was significantly different between subjects who presented with multiple knee injuries compared with subjects who presented with 1 additional knee injury (P < .0001) as well as subjects who did not present with any additional knee injuries (P = .0008). Median survival times based on knee injury severity are presented in Table 2.
TABLE 2.
Time to Surgery Based on the Knee Injury Severity
| Concomitant Knee Injuriesa | Time to Surgery, mo, Median (95% CI) |
|---|---|
| None | 1.56 (1.35-1.97) |
| One | 1.95 (1.54-2.23) |
| Multiple | 3.32 (2.23-4.76) |
aBased on number of concomitant knee injuries that required additional operative procedures.
Factors Related to ACL Surgery Timing
Time From Injury to ACL Surgery
In the univariable Cox proportional-hazards regression analyses, insurance coverage type (P < .0001), household income (P = .0003), and age at injury (P = .0002) were significantly associated with the risk of delayed surgery. Differences in the median time to ACL surgery based on insurance status, age, and income are illustrated in Table 3, as well as Figures 2 to 4. Sex (P = .2358), obesity (P = .1228), ethnicity (P = .2405), and race (P = .6812) were not significantly related to the risk of delayed surgery.
TABLE 3.
Time to Surgery Based on Insurance Status, Age, and Median Income
| Time to Surgery, mo, Median (95% CI) | |
|---|---|
| Insurance coverage | |
| Commercial | 1.5 (1.3-1.7) |
| Noncommercial | 3.0 (2.3-3.3) |
| Age, y | |
| >14 | 1.7 (1.5-2.1) |
| <14 | 2.6 (2.0-3.2) |
| Median income | |
| ≥75th percentilea | 1.2 (1.1-1.5) |
| <75th percentilea | 2.2 (2.0-2.6) |
aPercentiles based on study population.
Figure 2.
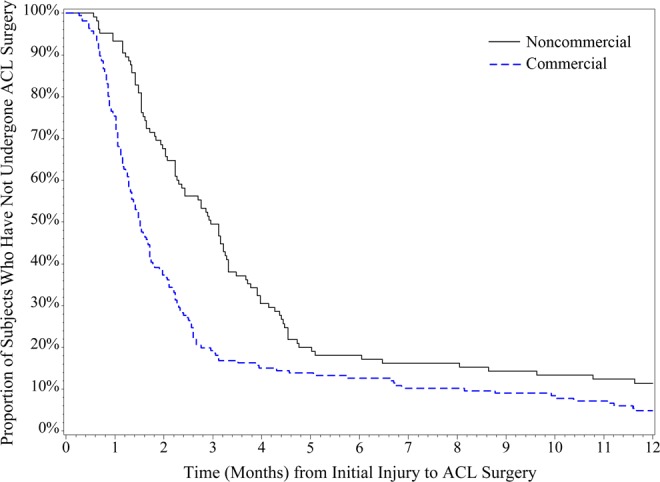
Insurance status. Difference in anterior cruciate ligament (ACL) surgery timing among subjects with commercial versus noncommercial insurance plans in the first 2 years following their initial injury.
Figure 4.
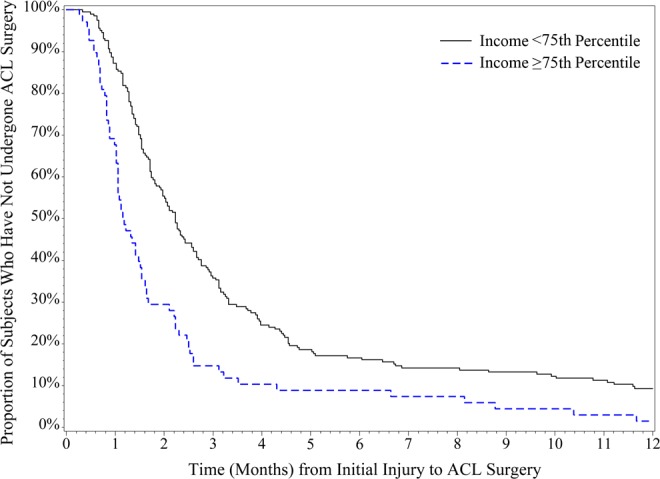
Household income. Relationship between household income and anterior cruciate ligament (ACL) surgery timing in the first 2 years after the initial injury. The top line represents the time to ACL surgery among subjects with a household income <75th percentile for the entire study population. The bottom line represents the time to ACL surgery among subjects with a household income ≥75th percentile for the entire study population.
Figure 3.
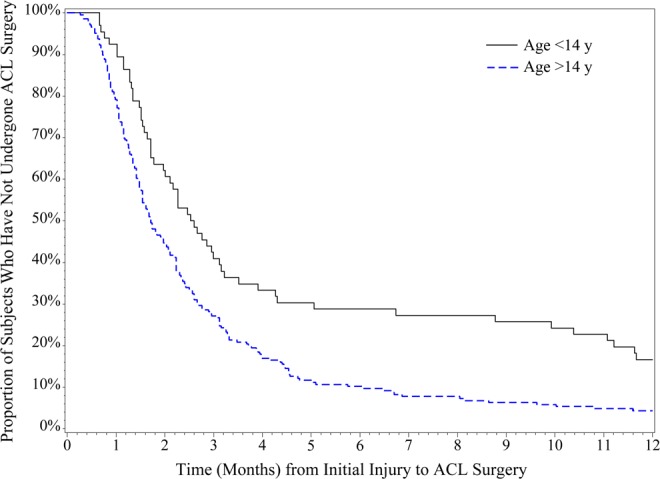
Age at initial injury. Difference in anterior cruciate ligament (ACL) surgery timing among subjects older than 14 years versus those younger than 14 years at initial injury.
Variables significantly (P < .05) or marginally significantly associated with ACL surgery timing were considered for inclusion in the multivariable model. During the model building step of the analysis, insurance type and median income were found to be significantly correlated (r2 = 0.2, P < .0001). Due to concerns regarding multicollinearity, only insurance status was considered for inclusion in the final model. We elected to include insurance status instead of median income because insurance status was a stronger predictor of ACL surgery timing and because median household income was an indirect measure of family income (based on ZIP codes). Age at injury (P < .0001) and insurance coverage type (P < .0001) were significantly associated with ACL surgery timing in the final, multivariable model. After controlling for age, the risk of delayed surgery among subjects with a commercial insurance plan was 2.0 (95% CI, 1.6-2.6) times the risk of delayed surgery among subjects with government-assisted plans or no insurance. In other words, there was a 67% chance that a subject with a commercial insurance plan underwent ACL surgery before a subject with a noncommercial insurance plan underwent ACL surgery. After controlling for insurance coverage type, the risk of delayed surgery was 1.2 times (95% CI, 1.1-1.2) higher for every 1-year increase in age.
Time From Injury to Orthopaedic Evaluation
Variables significantly related to the time from injury to the initial orthopaedic evaluation included age at injury (hazard ratio [HR] per 1-year increase in age, 1.1; 95% CI, 1.1-1.2; P < .0001) and commercial versus noncommercial insurance type (HR, 2.0; 95% CI, 1.5-2.6; P < .001).
Time From Orthopaedic Evaluation to Surgery
Variables significantly related to the time from initial orthopaedic evaluation to ACL reconstructive surgery included only commercial versus noncommercial insurance type (HR, 1.5; 95% CI, 1.2-2.0; P = .0007) and age (HR per 1-year increase in age, 1.1; 95% CI, 1.0-1.1; P = .0416).
Time From Injury to MRI Evaluation
Age (HR per 1-year increase in age, 1.1; 95% CI, 1.0-1.2; P = .0032) and commercial versus noncommercial insurance type (HR, 1.8; 95% CI, 1.4-2.4; P < .0001) were significantly related to time from initial injury to MRI.
Factors Related to Presence of Additional Knee Injuries
Age at injury and insurance type were significantly related to the number of additional injuries noted during the primary ACL reconstruction in the multivariable ordinal logistic regression analysis. After controlling for insurance type, the odds of a subject presenting with additional knee injuries were 1.1 (95% CI, 1.0-1.2; P = .0491) times higher for every 1-year increase in age at initial injury. After controlling for age at injury, the odds of a subject presenting with multiple additional knee injuries were 1.7 (95% CI, 1.1-2.8; P = .0206) times higher among subjects with noncommercial insurance coverage compared with subjects with commercial insurance coverage. The unadjusted relationship between insurance status and the presence of additional knee injuries is described in greater detail in Table 4.
TABLE 4.
Subjects With Additional Knee Injuries Requiring Operative Treatment According to Insurance Statusa
| Insurance Status | No Injuries | 1 Injury | Multiple Injuries |
|---|---|---|---|
| Uninsured/government-assisted | 31 (29.52) | 44 (41.91) | 30 (28.57) |
| Commercial | 74 (44.58) | 62 (37.35) | 30 (18.07) |
aValues are expressed as n (%).
Discussion
This study demonstrates that pediatric patients who are older, live in a more affluent ZIP code, and have commercial insurance coverage progress to surgery for ACL reconstruction more quickly do than younger, less affluent, and non–commercially insured patients. This study also confirms previous research3,8,9 that has reported an association between a delay in ACL surgery and the presence of additional knee injuries requiring operative treatment.
Insurance type was identified as the strongest predictor of ACL surgery timing in the univariate analysis. This finding is consistent with several recent studies that have described discrepancies in access to orthopaedic-related health care on the basis of insurance coverage.2,6,11,12 Skaggs et al12 randomly surveyed orthopaedic surgeons’ offices in 50 states about their willingness to accept Medicaid patients. Of the 230 offices that completed the survey, 38% reported they limited the number of Medicaid patients they were willing to see, and 18% reported they would not see a Medicaid patient under any circumstance. Pierce et al10 contacted orthopaedic surgeons in the Greater Cincinnati area about their willingness to see a fictitious 14-year-old with an MRI-confirmed ACL tear. There was a significant (P < .0001) difference in the proportion of offices willing to offer a clinic appointment within 2 weeks of the date of the phone call for a patient with private insurance (90%) versus a patient with Medicaid (14%).
Discrepancies in the delivery of orthopaedic-related care among patients with noncommercial insurance plans have also been described. Kocher et al6 reported a significant difference in median time from symptom onset to slipped capital femoral epiphysis (SCFE) diagnosis among patients with Medicaid (12 weeks) versus those with private insurance (7.5 weeks). Sabharwal et al11 retrospectively reviewed 125 pediatric patients who underwent fracture management in an academic emergency department. The odds of receiving orthopaedic treatment for an extremity fracture within 24 hours of the initial injury were 4 times greater among patients with private insurance compared with those with Medicaid (P = .015). In a prospective study of adults and children who had been diagnosed with an ACL tear in South Florida, Baraga et al2 demonstrated that patients with private insurance underwent surgery sooner than those with Medicaid (HR, 2.15; P = .012). A significant (P < .001) increase in the median number of days from injury to diagnosis was also noted among subjects with Medicaid (56 days) versus private insurance (14 days).
Overall, insurance status has been shown to delay treatment of SCFE,6 ACL tears,2 and extremity fractures.11 However, these studies did not investigate whether insurance status was related to the severity and/or subsequent treatment of the orthopaedic injury. In our study, the number of knee injuries requiring additional operative treatment was used as a surrogate marker for knee injury severity. Insurance status was significantly associated with increased knee injury severity. After controlling for age at injury, odds of presenting with additional knee injuries were significantly higher among subjects with noncommercial insurance coverage. This is not to suggest that injury severity is directly related to insurance type. Instead, insurance type is likely a mediator in the relationship between a delay in surgery and the development of concomitant knee injuries. In other words, insurance type may delay the time from injury to surgery, and consequently, this delay in surgery results in an increase in the number of concomitant knee injuries requiring additional operative treatment.
A lack of resources, appointment times, and providers willing to see patients with noncommercial insurance have been implicated as potential reasons why treatment may be delayed among patients with noncommercial insurance plans.10,12 Financial motivators have also been suggested. Skaggs et al12 demonstrated there was significant correlation between an orthopaedic office’s willingness to see Medicaid patients and their state-based reimbursement rates for orthopaedic procedures. Despite the absence of any known or facilitated limitation in appointment availability for patients with noncommercial insurance plans at our institution, there was a 67% chance that a subject with commercial insurance underwent ACL surgery before a patient with a noncommercial insurance plan. Furthermore, when the time to ACL surgery was divided into more specific treatment-related time periods, noncommercial insurance coverage was associated with a significantly higher risk of delayed care when compared with commercial insurance coverage during the time from initial injury to MRI evaluation, time from initial injury to orthopaedic evaluation, as well as time from orthopaedic evaluation to surgery. This suggests that the source of the delay among patients with noncommercial insurance was not related to one specific component of the postinjury treatment process. Instead, the delay was present across all treatment phases.
It is important to appreciate the fact that navigating the diagnostic, operative, and postsurgical appointments associated with the surgical management of an ACL rupture places substantial burden on the patient and their family. Families with noncommercial insurance or lower household income may not be able to juggle these demands as effectively as families with more resources. At our institution, dedicated nurse coordinators have been successfully used to help patients with complex musculoskeletal disorders navigate through their pre- and postsurgical needs. Implementation of a similar care model in sports medicine may be beneficial in helping patients at increased risk for delaying ACL surgery coordinate their medical appointments in a timely manner.
Early, appropriately timed surgical intervention is now the preferred method for managing the ACL-deficient adolescent.4 The goal of early intervention is to restore knee stability and limit the development of additional knee injuries. The results of the current study confirm previous research regarding the relationship between a delay in surgery and development of multiple additional knee injuries. Median time to surgery was significantly increased among subjects who presented with multiple additional knee injuries (3.3 months) compared with subjects who did not present with any additional injury in this study (1.6 months). This suggests that a delay in surgery may be related to the presence of multiple injuries. It is recognized that certain injuries often accompany the initial traumatic event to the ACL. Additionally, the development of multiple injuries may occur as a result of continued knee instability, and thus lead to subsequent injuries to meniscal and cartilaginous structures in the knee joint that require additional operative treatment during the primary ACL reconstruction.
The strengths of our study include a large study population and the collection of data from a contiguous patient cohort at a single, large-volume, tertiary pediatric hospital. This is the first study of its kind that we are aware of in the pediatric population. However, this study was not without limitations. Using the median income of the patient’s home ZIP code as a surrogate for household income is not an ideal measure of wealth. Given the difficulty in obtaining this information, especially for the purposes of a retrospective study, this is the best surrogate that was available. The average household income in our study was markedly higher than the national average of $29,056 for the year 2010.13 Furthermore, additional factors that may potentially contribute to a delay in treatment such as skeletal maturity level, parental education, and level of care available at the site of the injury and initial evaluation were not collected in this study.
The classification of insurance status as private versus combined government-assisted and uninsured is also not ideal. Future studies that are appropriately powered to allow for more specific classification would be informative. As demonstrated by Skaggs et al,12 physician willingness to accept new patients with Medicaid was significantly correlated to state-based Medicaid reimbursement rates. Therefore, influence of health insurance on access to and delivery of health care is likely to differ in other regions of the country with different demographic, ethnic, and socioeconomic environments. Multicenter and regional investigations would be beneficial. A prospective collection of patient/parent employment status, single-parent household status, and interaction of athletic trainers or others experienced with this type of injury in the pediatric population would also be ideal for future studies.
Conclusion
Younger age, noncommercial insurance status, and decreased household income were associated with a significantly greater risk of delayed ACL surgery. Additionally, knee injury severity was significantly increased among patients with noncommercial insurance coverage. These disparities are likely multifactorial, being composed of patient-, provider-, and resource-related factors.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.F.V. received honoraria from MTF for speaking engagements unrelated to the present study. This study was supported in part by NIH/NCRR Colorado CTSI Grant Number UL1 RR025780.
References
- 1. A SAS Program for the CDC Growth Charts. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease and Prevention and Health Promotion. Center for Disease Control and Prevention; Available at: http://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. [Google Scholar]
- 2. Baraga MG, Smith MK, Tanner JP, Kaplan LD, Lesniak BP. Anterior cruciate ligament injury and access to care in South Florida: does insurance status play a role? J Bone Joint Surg Am. 2012;94:e183. [DOI] [PubMed] [Google Scholar]
- 3. Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears relationship of treatment time and patient-specific factors. Am J Sports Med. 2012;40:2128–2133. [DOI] [PubMed] [Google Scholar]
- 4. Frank JS, Gambacorta PL. Anterior cruciate ligament injuries in the skeletally immature athlete: diagnosis and management. J Am Acad Orthop Surg. 2013;21 (2):78–87. [DOI] [PubMed] [Google Scholar]
- 5. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja R. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8:229–233. [DOI] [PubMed] [Google Scholar]
- 6. Kocher MS, Bishop JA, Weed B, et al. Delay in diagnosis of slipped capital femoral epiphysis. Pediatrics. 2004;113:e322–325. [DOI] [PubMed] [Google Scholar]
- 7. Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120 (suppl 4):S193–228. [DOI] [PubMed] [Google Scholar]
- 8. Lawrence JTR, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–2587. [DOI] [PubMed] [Google Scholar]
- 9. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18:955–959. [DOI] [PubMed] [Google Scholar]
- 10. Pierce TR, Mehlman CT, Tamai J, Skaggs DL. Access to care for the adolescent anterior cruciate ligament patient with Medicaid versus private insurance. J Pediatr Orthop. 2012;32:245–248. [DOI] [PubMed] [Google Scholar]
- 11. Sabharwal S, Zhao C, McClemens E, Kaufmann A. Pediatric orthopaedic patients presenting to a university emergency department after visiting another emergency department: demographics and health insurance status. J Pediatr Orthop. 2007;27:690–694. [DOI] [PubMed] [Google Scholar]
- 12. Skaggs DL, Lehmann CL, Rice C, et al. Access to orthopaedic care for children with medicaid versus private insurance: results of a national survey. J Pediatr Orthop. 2006;26:400–404. [DOI] [PubMed] [Google Scholar]
- 13. The Organisation for Economic Co-operation and Development, OECD.StatExtracts. Available at: http://stats.oecd.org/.
- 14. Utukuri M, Somayaji H, Khanduja V, Dowd G, Hunt D. Update on paediatric ACL injuries. Knee. 2006;13:345–352. [DOI] [PubMed] [Google Scholar]
- 15. Zip Code Characteristics: Mean and Median Household Income. Population Studies Center, Institute for Social Research. University of Michigan; Available at: http://www.psc.isr.umich.edu/dis/census/Features/tract2zip/index.html. [Google Scholar]


