Abstract
Background:
The anterior cruciate ligament (ACL) is the most frequently injured ligament in the knee for which surgery is performed. United States national estimates of ACL reconstruction vary widely.
Purpose:
This study sought to use the most recently available Centers for Disease Control and Prevention data to investigate changes in the utilization of inpatient and ambulatory surgery for ACL tears in the United States.
Study Design:
Descriptive epidemiology study.
Methods:
The National Survey of Ambulatory Surgery, conducted in 1994, 1995, 1996, and 2006 (data from 1994, 1996, and 2006 were used in the study), and the National Hospital Discharge Survey, conducted between 1990 and 2007, were used to identify cases of ACL reconstruction. The data were analyzed for trends in demographics, treatment, and utilization.
Results:
Between 1994 and 2006, the population-adjusted estimate of the rate of ACL reconstructions increased by 37% (33.0/100,000 capita or 86,837 total procedures to 45.1/100,000 capita or 134,421 total procedures). There was an increase in the proportion of females undergoing reconstruction in both the ambulatory (30% to 40%) and inpatient (29% to 47%) settings over the study period, with a 304% increase in the sex-adjusted estimate of the rate of female ambulatory procedures between 1994 and 2006. Age-adjusted estimates of the rates of ambulatory ACL reconstruction increased among all age groups, with a 924% increase in patients less than 15 years of age. Concurrent meniscectomy remained relatively constant in the ambulatory (37% to 40%) and inpatient (37% to 33%) settings between 1994 and 2007. Private insurance was the largest compensator, representing 77% of cases in 2006. Between 1994 and 2006, the use of peripheral nerve blocks during ambulatory surgery increased from 0.7% to 30.8%.
Conclusion:
The rate of ACL reconstruction increased dramatically between 1990 and 2007 based on the National Survey of Ambulatory Surgery and National Hospital Discharge Survey databases, which represents the most up-to-date publicly available data. Knowledge of this increase and national practice patterns may aid policy makers and surgeons in appropriately allocating health care resources to ensure quality patient care.
Keywords: anterior cruciate ligament reconstruction, ACL, epidemiology, meniscectomy
The anterior cruciate ligament (ACL) is cited as the most frequently injured ligament in the knee that requires surgical reconstruction.17,24 Anterior cruciate ligament injuries most commonly occur in athletes playing multidirectional sports.17,32 Affected individuals suffer both time loss from sport and an increased risk of premature osteoarthritis.40,45 While a plethora of literature exists regarding ACL reconstruction techniques, graft choice, individual practice patterns, and postoperative complications, the majority of studies focus on small cohorts of patients.2,10,28,31,37
Attempts to capture population-based trends have led to the creation of ACL registries like those for college and high school athletes,41,42 as well as the MOON (Multicenter Orthopedic Outcomes Network)15 and MARS (Multicenter ACL Revision Study)34 registries. These studies account for a small percentage of the total burden of ACL injury in the United States, potentially limiting their generalizability. Additional epidemiologic studies evaluating ACL injury include the study by Dunn et al,14 who evaluated the burden of injury among US soldiers, a study by Lyman et al31 evaluating trends of ACL reconstruction in the state of New York, and a study by Nielsen and Yde43 prospectively evaluating the rate of ACL injuries over a 1-year period in emergency rooms. Resulting national estimates of the incidence of ACL reconstruction vary widely between 60,000 and 175,000.31,38
Knowledge of the incidence and patterns of disease burden are necessary for the creation of national injury prevention programs16,53 and for the appropriate allocation of limited healthcare resources. The purpose of this study was to determine national trends in resource utilization for ambulatory and inpatient ACL reconstruction with a specific focus on age, sex, concurrent meniscal surgery, surgical setting, anesthetic type, and payment method.
Materials and Methods
Data Source
Data from the National Hospital Discharge Survey (NHDS)6 and the National Survey of Ambulatory Surgery (NSAS)5 databases were used to analyze trends in the surgical management of ACL tears from 1990 to 2007. This represents the most recent, publicly available national data from the Centers for Disease Control and Prevention (CDC). The NHDS and NSAS are mutually exclusive in that cases recorded in one are not recorded in the other. Because the NSAS and NHDS are administrative datasets in which all data are deidentified and available for public use, this study was exempt from approval by our institutional review board.
Since 1965, the National Center for Health Statistics (NCHS) has been collecting data for the NHDS database annually to compile nationally representative data on inpatient utilization of short-stay hospitals.12 Using a stratified multistage probability design, the NHDS retrieves an annual sample of more than 250,000 discharges from nonfederal short-stay hospitals (average length of stay, <30 days) in the United States and District of Columbia.22 All facilities must have at least 6 beds for patient use to be included in the study. The NHDS collects demographic information (age, sex, race), expected source of payment (insurance status), medical information of up to 7 discharge diagnoses and up to 4 procedures, length of care, hospital size, US region, and inpatient outcomes including discharge destination.36 In comparison, the NSAS is a national study involving both hospital-based and freestanding ambulatory surgery centers, which provides the most recent and comprehensive overview of ambulatory surgery in the United States.25 The survey was conducted in 1994, 1995, 1996, and in 2006 (data from 1994, 1996, and 2006 were used in this study), with medical information recorded on patient abstracts coded by NCHS contract staff. Both databases use International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes4 to classify medical diagnoses and procedures. The weighting procedure used in the NHDS and NSAS databases produces an unbiased national estimate by utilizing multistage estimate procedures, including inflation by reciprocals of the probabilities of sample selection, adjustment for no response, and population-weighting ratio adjustments.8,12
Study Population
Demographic and medical information was obtained for individuals undergoing cruciate ligament reconstruction between 1990 and 2007. The ICD-9-CM was used to identify cruciate ligament reconstruction procedures.4 Discharges with a procedure code (ICD-9-CM) of isolated cruciate ligament reconstruction (81.45) were included in the sample using previously described techniques.31,51 Notably, the ICD-9-CM code 81.45 is defined as “cruciate ligament repair,” not allowing for a differentiation between anterior and posterior cruciate ligament reconstructions. However, a previous investigation by Lyman et al31 demonstrated that 99.3% of all outpatient “cruciate ligament repair” (81.45) procedures were ACL reconstructions when compared with concurrent Current Procedural Terminology (CPT) codes. Because the CDC databases used for this study do not include CPT codes, we were unable to differentiate between anterior and posterior cruciate ligament reconstructions. However, because of the high proportion reported by Lyman et al,31 inclusion of posterior cruciate ligament reconstruction in the cohort likely represents a rare occurrence.
ICD-9 diagnosis codes identified as having a high frequency of association with ACL injury were then used to further query the databases and isolate ACL reconstructions (Table 1). Procedures with only a diagnosis of “disruption of posterior cruciate ligament” (717.84) were excluded from the analysis. The remaining procedures (ACL reconstructions) were included for data analysis. Surgical procedure codes were utilized first because reimbursement is driven more by procedures than by diagnoses, as previously described.31 The NSAS and NHDS data were then recorded for age, sex, facility type, insurance type, anesthesia type, diagnoses, and procedures. Concomitant procedures on the meniscus were recorded separately by querying the database for procedures with an ICD-9 procedure code of 80.6 (excision of semilunar cartilage of the knee). Because there is no specific ICD-9 code for meniscal repair, this study only evaluated those ACL reconstructions where concurrent meniscectomy was performed.
TABLE 1.
ICD-9 Diagnosis Codes Used for Data Analysisa
| Diagnosis Code | Diagnosis Description |
|---|---|
| 717.83 | Disruption of anterior cruciate ligament |
| 844.2 | Sprain of cruciate ligament of knee |
| 717.84 | Disruption of posterior cruciate ligament |
aICD-9, International Classification of Diseases, Ninth Revision.
Statistical Analysis
Because of the large sample size, we assumed a normal distribution of the data. Descriptive statistics consisted of means and standard errors for continuous variables and frequencies and percentages for discrete variables. We analyzed the NSAS and NHDS data using a sampling weighting method. The survey data were collected based on a probabilistic sample scheme. Therefore, we used sampling weights (the inverse of selection probability) provided by the CDC to account for unequal sampling probabilities and to produce estimates for all visits in the United States. A Taylor linearization model provided by the CDC estimates was used to calculate standard error and confidence intervals of the data. Standard error is a measure of sampling variability that occurs by chance because only a sample rather than the entire universe is surveyed. We selected a 95% confidence interval along with a point estimate to define population parameters. These confidence intervals, when compared between years, can be suggestive of statistical differences if the data are nonoverlapping. However, direct statistical comparison between years could not be performed because of sampling differences in the database. United States census data were used to obtain national population estimates for each year of the study (1990-2007).52 Rates were presented as the number of ACL reconstructions per 100,000 standard population. Applying sex-specific rates to the standard population and dividing by the total in the standard population, we calculated sex-adjusted rates for each year. For age, a direct adjustment procedure was used, and the US population in 2000 was selected as the standard population, as suggested by the director of the Department of Health and Human Services for NCHS databases.26,46 All data were analyzed using the software Statistical Package for Social Sciences (SPSS) version 20 (IBM).
Results
Total Number of Procedures
A total of 127,446 ambulatory surgical procedures (95% CI, 114,752-140,139) or 42.7 per 100,000 capita were recorded by the NSAS for the treatment of ACL tears in 2006. This represents a large increase in the total number of ambulatory procedures from 37,203 (95% CI, 34,018-40,387) in 1994 (14 per 100,000 capita) to 61,454 (95% CI, 55,191-67,717) in 1995 (23.1 per 100,000 capita) to 71,953 (95% CI, 65,908-77,997) in 1996 (26.7 per 100,000 capita) (Figure 1). Paralleling the increase in total number of procedures, the proportion of ambulatory surgical procedures performed for ACL tear also increased between 1996 and 2006. Specifically, in 2006, the NSAS database estimated a total of 34,738,440 ambulatory surgical procedures, meaning 0.37% of these procedures were for the treatment of ACL tears. In contrast, the NSAS database estimated a total of 21,236,913 ambulatory surgical procedures in 1996, meaning 0.34% were for the treatment of ACL tears. The total number of inpatient ACL reconstructions reported by the NHDS decreased over time from 45,030 (95% CI, 40,913-49,147) in 1990 (18 per 100,000 capita) to 35,247 (95% CI, 27,371-43,122) in 1996 (13 per 100,000 capita), 21,547 (95% CI, 15,846-27,248) in 2000 (7 per 100,000 capita), 6975 (95% CI, 4104-9846) in 2006 (2 per 100,000 capita), and 4043 (95% CI, 1745-9846) in 2007 (1 per 100,000 capita) (Figure 1).
Figure 1.
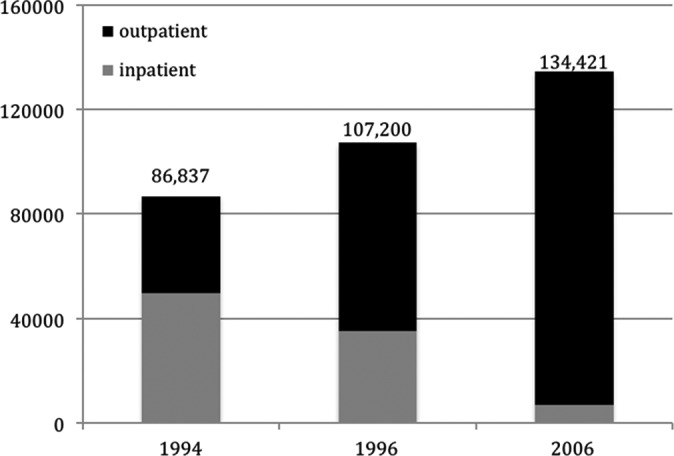
Volume of inpatient and ambulatory national anterior cruciate ligament reconstructions in 1994, 1996, and 2006.
Sex
During the study period, more men than women underwent ACL reconstruction in both the inpatient and outpatient settings, though the difference diminished over time. In 1994, 69.8% of outpatient ACL reconstructions were performed on males (20.5 per 100,000 capita male vs 8.4 per 100,000 capita female). However, in 2006, the gap between males and females narrowed, with 60.0% of outpatient ACL reconstructions being performed on males (53.1 per 100,000 capita male vs 34.0 per 100,000 capita female). These findings are similar to the results of the NHDS dataset. In 1990, 71.1% of the inpatient ACL reconstructions were performed on males (26.0 per 100,000 per capita male vs 10.1 per 100,000 per capita female). In contrast, in 1996, 55.9% of the inpatient ACL reconstructions were performed on males (15.2 per 100,000 per capita male vs 11.5 per 100,000 per capita female), and in 2006, 53.4% of inpatient ACL reconstructions were performed on males (2.9 per 100,000 per capita male vs 2.2 per 100,000 per capita female). Tables 2 and 3 demonstrate the sex differences in population-adjusted rates of ACL surgery and the percent change between 1994 and 2006 overall and divided by surgical setting, respectively.
TABLE 2.
Changes in Population- and Sex-Adjusted Rates of All ACL Reconstructions in the USa
| 1994 | 1996 | 2006 | Percentage Change (2006 vs 1994) | |
|---|---|---|---|---|
| Male | 46.9 | 52.7 | 55.7 | 19 |
| Female | 20.5 | 28.7 | 36.2 | 77 |
| Overall | 33 | 39.8 | 45.1 | 37 |
aValues are reported as rate per 100,000 capita. ACL, anterior cruciate ligament; US, United States.
TABLE 3.
Changes in Population- and Sex-Adjusted Rates of Ambulatory and Inpatient ACL Reconstructionsa
| 1994 | 1996 | 2006 | Percentage Change (2006 vs 1994) | |
|---|---|---|---|---|
| Ambulatory | ||||
| Male | 20.5 | 31.6 | 53.1 | 160 |
| Female | 8.4 | 15.6 | 34.0 | 304 |
| Overall | 14.1 | 26.7 | 42.7 | 202 |
| Inpatient | ||||
| Male | 26.4 | 15.2 | 2.6 | −924 |
| Female | 13 | 11.5 | 2.2 | −498 |
| Overall | 18.9 | 13.1 | 2.3 | −706 |
aValues are reported as rate per 100,000 capita. ACL, anterior cruciate ligament.
Age
The mean patient age for outpatient procedures remained constant between 1994 (28.8 years; 95% CI, 25.7-31.8) and 2006 (28.7 years; 95% CI, 26.6-30.8). Similarly, the mean patient age for inpatient ACL reconstructions remained constant between 1990 (27.0 years; 95% CI, 24.7-29.4), 1996 (27.7 years; 95% CI, 24.0-31.4), and 2007 (26.0 years; 95% CI, 16.6-35.5). The age-adjusted rate of ambulatory ACL reconstruction increased for all age groups, with the largest increase (924%) seen in patients younger than 15 years (Table 4). Conversely, the age-adjusted rate of inpatient procedures decreased among all age groups, with the largest decrease seen in the population aged 15 to 34 years (Table 4).
TABLE 4.
Observed and Age-Adjusted Rates of ACL Reconstruction With Use of the US Population in 2000 as the Controla
| Outpatient Age, y | NSAS 1994 | NSAS 1995 | NSAS 1996 | NSAS 2006 | Percentage Change Adjusted Rate (2006 vs 1994) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Observedb | Age-Adjusted | Observedb | Age-Adjusted | Observedb | Age-Adjusted | Observedb | Age-Adjusted | ||
| 0-14 | 8.55 | 1.84 | 17.52 | 3.76 | 15.32 | 3.29 | 87.8 | 18.85 | 924 |
| 15-34 | 346.53 | 95.02 | 580.56 | 159.2 | 623.29 | 170.92 | 1073.2 | 294.29 | 210 |
| 35-54 | 121.86 | 36.24 | 198.94 | 59.17 | 267.93 | 79.69 | 476.6 | 141.76 | 291 |
| ≥55 | 11.03 | 2.36 | 7.64 | 1.63 | 37.89 | 8.09 | 42.8 | 9.15 | 288 |
| Inpatient Age, y | NHDS 1990 | NHDS 1994 | NHDS 1996 | NHDS 2006 | Percentage Change Adjusted Rate (2006 vs 1994) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Observedb | Age-Adjusted | Observedb | Age-Adjusted | Observedb | Age-Adjusted | Observedb | Age-Adjusted | ||
| 0-14 | 10.6 | 2.28 | 21.76 | 4.67 | 12.65 | 2.72 | 12.84 | 2.76 | −69 |
| 15-34 | 483.4 | 132.56 | 489.79 | 134.31 | 341.93 | 93.76 | 54.55 | 14.96 | −798 |
| 35-54 | 91.02 | 27.07 | 131.17 | 39.02 | 91.65 | 27.26 | 18.57 | 5.52 | −607 |
| ≥55 | 9.63 | 2.06 | 12.78 | 2.73 | 21.53 | 4.59 | 10.11 | 2.16 | −26 |
aNHDS, National Hospital Discharge Survey; NSAS, National Survey of Ambulatory Surgery; US, United States.
bRate per 100,000 capita.
Facility Type
As the total number of surgeries performed over the study period increased, so did the proportion of procedures performed in an ambulatory setting. In 1994, 13.8% of outpatient surgeries for ACL reconstruction were performed in a freestanding ambulatory facility. In 2006, 53.4% of these procedures took place in a freestanding ambulatory facility, representing an increase of 39.6% (Figure 2). The observed rate of outpatient surgical procedures increased by 300% (14.1 to 42.7 per 100,000 capita) between 1994 and 2007 while inpatient surgical procedures decreased 706% (18.9 per 100,000 to 2.3 per 100,000 capita) between 1994 and 2006 (Table 3). At all time points, NHDS data demonstrated that the majority (70.9%-85.5%) of inpatient ACL reconstructions occurred in nonprofit facilities. Additionally, the proportion of inpatient ACL reconstructions taking place in proprietary hospitals decreased from 17.5% in 1990 to 4.8% in 2006.
Figure 2.
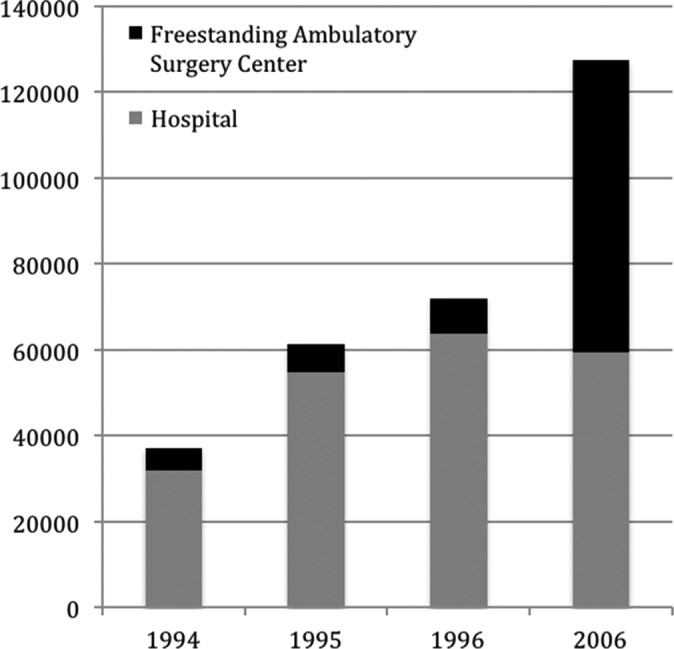
Proportion of outpatient anterior cruciate ligament reconstructions performed in a freestanding ambulatory surgery center versus hospital-based ambulatory center.
Anesthesia
The use of general anesthesia alone decreased over the study period from 83.3% of the total anesthesia usage in 1994 to 60.9% in 2006 (Table 5). The use of regional anesthesia combined with general anesthesia increased from 0.1% in 1994 to 25.7% in 2006. The use of regional anesthesia alone increased from 0.7% in 1994 to 5% in 2006. Intravenous anesthesia use was 3.0% in 1994 and increased to 7.4% in 2006.
TABLE 5.
Type of Anesthesia Used for Outpatient ACL Reconstructionsa
| NSAS 1994 | NSAS 1995 | NSAS 1996 | NSAS 2006 | |
|---|---|---|---|---|
| Regional block | 0.7 | 0.2 | 2.6 | 5.0 |
| Regional block with general | 0.1 | 0.5 | 1.0 | 25.7 |
| General alone | 84.3 | 81.3 | 75.3 | 60.9 |
| Monitored anesthesia care | 0.6 | 0.5 | 1.1 | 1.0 |
| Intravenous sedation | 3.0 | 4.4 | 7.5 | 7.4 |
aValues are reported as percentages. ACL, anterior cruciate ligament; NSAS, National Survey of Ambulatory Surgery.
Insurance
Between 1994 and 2007, private insurance was the primary source of payment for ACL reconstruction in both the inpatient and outpatient setting (Figure 3). An increasing trend was seen in Medicare, Medicaid, and other governmental payment for inpatient procedures, which represented 4.6% in 1990, 5.5% in 1996, and 13.8% in 2007.
Figure 3.
Primary source of payment for inpatient and outpatient anterior cruciate ligament reconstructions between 1990 and 2007. HMO, health maintenance organization; NHDS, National Hospital Discharge Survey; NSAS, National Survey of Ambulatory Surgery; PPO, preferred provider organization.
Concurrent Meniscus Surgery
The percentage of patients undergoing concurrent meniscus surgery during their ACL reconstructions is represented in Table 6. In 1994, 37.0% (5.2 per 100,000 capita) of the patients undergoing outpatient ACL reconstruction underwent concurrent meniscus surgery. Similarly, in 2006, 39.9% (17.0 per 100,000 capita) of patients undergoing outpatient ACL reconstructions underwent concurrent meniscus surgery. From the NHDS data, the proportion of inpatient ACL reconstructions performed with concomitant meniscus surgery in 1990 was 23.7% (4.3 per 100,000 capita), 36.5% (6.9 per 100,000 capita) in 1994, and 32.8% in 2007 (0.4 per 100,000 capita).
TABLE 6.
Proportion of ACL Reconstructions Undergoing Concurrent Meniscus Surgerya
| Outpatient | Inpatient | |||||||
|---|---|---|---|---|---|---|---|---|
| NSAS 1994 | NSAS 1995 | NSAS 1996 | NSAS 2006 | NHDS 1990 | NHDS 1994 | NHDS 1996 | NHDS 2006 | |
| Total | 13,769 | 24,446 | 23,905 | 50,798 | 10,652 | 18,127 | 10,224 | 2276 |
| % ACL | 37.0 | 39.8 | 33.2 | 39.9 | 23.7 | 36.5 | 29.0 | 32.6 |
| Rateb | 5.2 | 9.2 | 8.9 | 17.0 | 4.3 | 6.9 | 3.8 | 0.76 |
| % male | 76.1 | 74.7 | 65.4 | 65.9 | 74.8 | 71.0 | 53.8 | 47.4 |
aACL, anterior cruciate ligament; NHDS, National Hospital Discharge Survey; NSAS, National Survey of Ambulatory Surgery.
bPer 100,000 capita.
Discussion
This descriptive epidemiologic study investigated trends in inpatient and ambulatory surgery for ACL reconstruction between 1990 and 2007 using the NSAS5 and the NHDS.6 Our results demonstrated that the total number of ACL reconstructions performed in the United States increased from 33.0 per 100,000 capita in 1994 to 45.1 per 100,000 capita in 2006. The number of procedures performed in the ambulatory setting increased from 14 per 100,000 capita in 1994 to 43 per 100,000 capita in 2006, whereas the number of inpatient ACL reconstructions decreased from 18 to 1 per 100,000 capita between 1990 and 2007. The total number of ACL reconstructions (inpatient and ambulatory) increased from 86,837 (33 per 100,000 capita) in 1994 to 134,421 (45 per 100,000 capita) in 2006. Our findings are similar to those predicted by Lyman et al,31 who extrapolated their data in New York State to the Healthcare Cost and Utilization Project National Inpatient Sample to predict a total of 62,637 total procedures in 1997 and 105,118 in 2006. Many explanations exist for the rise in ACL reconstruction over time. It is possible that the increased frequency represents an increase in the frequency of ACL injury. It is also possible that the increase represents an increased likelihood of reconstruction should an injury occur, which has previously been suggested by Dunn et al.14 When compared with population-adjusted rates observed in other nations, the results of this study demonstrate the United States has the second highest known rate of ACL reconstruction behind Australia (52.0 per 100,000 capita between 2003 and 2008),24 with national estimates from other countries, including Denmark (38 per 100,000 capita),30 New Zealand (37.8 per 100,000),17 Norway (34 per 100,000),19 and Sweden (32 per 100,000).20 One possible explanation for the higher rates of ACL reconstruction in the United States than in European countries may be a treatment bias, or an increased likelihood of having surgery when presenting with an ACL tear, in the United States. As the compensation of many US surgeons is correlated with productivity, it is possible this trend reflects an increased likelihood to operate, whereas surgeons in many other countries are salaried. It is also possible that the increased rate of ACL reconstructions correlates with the increased use of artificial turf, which has been shown to be associated with a 1.39 times higher rate of ACL injury than grass surfaces among National Collegiate Athletic Association football players.13
Overall, this study found that the proportion of ambulatory ACL reconstructions performed on males decreased from 69.8% in 1994 to 60.0% in 2006. Similarly, inpatient ACL reconstructions among males decreased from 71.1% in 1990 to 52.7% in 2007. These findings are similar to those reported by Csintalan et al,9 who evaluated Kaiser Permanente’s database and noted the overall number of males suffering an ACL injury was higher than the number of females (68.4% vs 31.0%). One explanation for the higher proportion of males compared with females is participation bias, with males participating in sports associated with ACL injury more frequently than females. However, between 1994 and 2006, our study demonstrated a 177% increase in the sex-adjusted rate of women undergoing ACL reconstruction, with a 404% increase in the outpatient setting. Not surprisingly, an increased rate of ACL reconstruction among females parallels the finding that female participation in sports has reached an all-time high.54 Previous studies have shown a higher prevalence of knee injuries in female athletes11,23,45 as well as sex differences in ACL tears among national elite athletes.1 It is also possible that the increased rate of ACL reconstructions among females reflects an indirect effect of the Title IX law, which states that on the basis of sex, people cannot be excluded from participation or denied benefits or subjected to discrimination under education programs or activities receiving federal financial assistance. Thus, a greater proportion of females are likely playing “change of direction” sports into the college years, increasing their exposure to potential ACL injury. Interestingly, this dramatic rise in ACL reconstructions occurred despite the introduction of neuromuscular and proprioceptive injury prevention programs that have been shown to reduce the incidence of ACL tears up to 74%.33 Knowledge regarding this increased rate of reconstruction among female athletes can further aid in the design of preventive programs targeting this high-risk population.
Over the study period, age-adjusted rates of ACL reconstruction increased by 924% among patients younger than 15 years, which likely reflects an increased participation in youth sports among adolescents in the United States.44 It is also possible that the increase in ACL reconstructions among the youth population reflects a treatment bias, with the emerging field of pediatric sports medicine. Furthermore, it is possible the increase reflects reporting bias. Recently, studies have reported similar findings regarding an increase in ACL injuries among young athletes,27,28,47 with many surgeons recommending reconstruction due to the risk of subsequent meniscal injury and early osteoarthritis in the affected knee.18,29
This study evaluated the incidence of concurrent meniscus surgery during ACL reconstruction. We found that between 1994 and 2006, the proportion of ACL reconstructions with a concurrent meniscus surgery remained constant in both the ambulatory (37.0% and 39.9%) and inpatient (36.5% and 32.8%) settings. Previous studies have reported the incidence of concomitant meniscal injury in ACL tears ranges from 55% to 65%,3,7,49 with multiple reports demonstrating better clinical outcomes when menisci are intact or repaired at the time of ACL reconstruction.3,48 Because of limitations in ICD-9 coding, this study was only able to evaluate the rates of meniscectomy. However, our results are similar to those reported by Musahl et al,39 who found 34% of patients undergoing ACL reconstruction underwent concomitant partial meniscectomy. Understanding the burden of concomitant meniscal injury at the time of index surgery may help surgeons during preoperative planning.
The present study demonstrated that anesthesia for ACL reconstruction has changed over time. Between 1994 and 2006, there was a large increase in the number of procedures performed using regional blocks (0.7% to 30.8%), with or without concomitant general anesthesia. Peripheral nerve blocks are a safe and cost-effective method of pain control for knee surgery when compared with general anesthesia,50 and the increased rate of regional blocks will likely continue to parallel the rise in ambulatory procedures moving forward.
Drawing inferences from large data sets has limitations. Like all large databases, the NSAS and NHDS are subject to coding error25 or error in data entry.21,35 For example, because ICD-9-CM codes were used to retrieve the diagnoses and procedures, there is a possibility of misclassification error. However, the database administrators correct for this by using a multistage estimate procedure with weighting adjustments for no response and population weighting ratio adjustments.25 Similarly, the use of the ICD-9 code 81.45 (cruciate ligament repair) may have resulted in misclassification because it does not differentiate between anterior and posterior cruciate ligament reconstructions. However, a study by Lyman et al31 demonstrated that when using the ICD-9 code 81.45 to search for ACL reconstructions, 99.3% of all procedures were ACL reconstructions. In addition, we used the ICD-9 diagnosis code 717.84 (disruption of posterior cruciate ligament) to exclude isolated posterior cruciate ligament reconstructions. Therefore, misidentification of a posterior cruciate ligament reconstruction as an ACL reconstruction was likely a rare occurrence in this study, and we believe the data presented are representative of national trends in ACL reconstruction. Additionally, the use of the ICD-9 code 80.6 (excision of semilunar cartilage of knee) allowed for the identification of concurrent meniscectomy. However, this study cannot identify trends in meniscus repair, as there are no ICD-9 codes specific for repair. Another limitation of this study is its lack of clinical detail such as mechanism of injury or complexity of the procedure, as procedure codes are general and do not allow differentiation between specific patients. Finally, the results of this study are limited to practice patterns in the United States from 1990 to 2007. As trends in health care utilization can have substantial effects on policy and allocation of resources, this study demonstrates a need for additional national funding into surveys such as the NSAS beyond 2006.
In conclusion, this study demonstrates that the population-adjusted rate of ACL surgery has increased in the United States between 1990 and 2006 to 45.1 per 100,000 capita. This analysis of nationally representative data allows investigators to draw conclusions about national trends in ACL reconstruction, which may help guide future questions that can be tested in a clinical setting.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded by the Miami Center for Orthopaedic Research and Education.
References
- 1. Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524–530. [DOI] [PubMed] [Google Scholar]
- 2. Bradley JP, Klimkiewicz JJ, Rytel MJ, Powell JW. Anterior cruciate ligament injuries in the National Football League: epidemiology and current treatment trends among team physicians. Arthroscopy. 2002;18:502–509. [DOI] [PubMed] [Google Scholar]
- 3. Cannon WD, Jr, Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med. 1992;20:176–181. [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention/National Center for Health Statistics. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed February 12, 2014.
- 5. Centers for Disease Control and Prevention. National Survey of Ambulatory Surgery. http://www.cdc.gov/nchs/nsas.htm. Accessed June 6, 2014.
- 6. Centers for Disease Control and Prevention. National Hospital Discharge Survey. http://www.cdc.gov/nchs/nhds.htm. Accessed June 6, 2014.
- 7. Cerabona F, Sherman MF, Bonamo JR, Sklar J. Patterns of meniscal injury with acute anterior cruciate ligament tears. Am J Sports Med. 1988;16:603–609. [DOI] [PubMed] [Google Scholar]
- 8. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94:227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Csintalan RP, Inacio MC, Funahashi TT. Incidence rate of anterior cruciate ligament reconstructions. Perm J. 2008;12 (3):17–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632–644. [DOI] [PubMed] [Google Scholar]
- 11. de Loes M, Dahlstedt LJ, Thomee R. A 7-year study on risks and costs of knee injuries in male and female youth participants in 12 sports. Scand J Med Sci Sports. 2000;10:90–97. [DOI] [PubMed] [Google Scholar]
- 12. Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat 1. 2000;(39):1–42. [PubMed] [Google Scholar]
- 13. Dragoo JL, Braun HJ, Harris AH. The effect of playing surface on the incidence of ACL injuries in National Collegiate Athletic Association American football. Knee. 2013;20:191–195. [DOI] [PubMed] [Google Scholar]
- 14. Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG. The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med. 2004;32:1906–1914. [DOI] [PubMed] [Google Scholar]
- 15. Dunn WR, Spindler KP, Amendola A, et al. Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am J Sports Med. 2010;38:1778–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Finch CF, Boufous S. Do inadequacies in ICD-10-AM activity coded data lead to underestimates of the population frequency of sports/leisure injuries? Inj Prev. 2008;14:202–204. [DOI] [PubMed] [Google Scholar]
- 17. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009;12:622–627. [DOI] [PubMed] [Google Scholar]
- 18. Graf BK, Lange RH, Fujisaki CK, Landry GL, Saluja RK. Anterior cruciate ligament tears in skeletally immature patients: meniscal pathology at presentation and after attempted conservative treatment. Arthroscopy. 1992;8:229–233. [DOI] [PubMed] [Google Scholar]
- 19. Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008;36:308–315. [DOI] [PubMed] [Google Scholar]
- 20. Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop. 2009;80:563–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gray DT, Hodge DO, Ilstrup DM, Butterfield LC, Baratz KH. Concordance of Medicare data and population-based clinical data on cataract surgery utilization in Olmsted County, Minnesota. Am J Epidemiol. 1997;145:1123–1126. [DOI] [PubMed] [Google Scholar]
- 22. Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;(29):1-20, 24. [PubMed] [Google Scholar]
- 23. Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: part 1, mechanisms and risk factors. Am J Sports Med. 2006;34:299–311. [DOI] [PubMed] [Google Scholar]
- 24. Janssen KW, Orchard JW, Driscoll TR, van Mechelen W. High incidence and costs for anterior cruciate ligament reconstructions performed in Australia from 2003-2004 to 2007-2008: time for an anterior cruciate ligament register by Scandinavian model? Scand J Med Sci Sports. 2012;22:495–501. [DOI] [PubMed] [Google Scholar]
- 25. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. [DOI] [PubMed] [Google Scholar]
- 26. Klein R, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. From the Centers for Disease Control and Prevention/National Center for Health Statistics. Healthy People 2010 Statistical Notes. 2001;20 (1);1–10. [PubMed] [Google Scholar]
- 27. Kocher MS, Micheli LJ, Zurakowski D, Luke A. Partial tears of the anterior cruciate ligament in children and adolescents. Am J Sports Med. 2002;30:697–703. [DOI] [PubMed] [Google Scholar]
- 28. Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and the ACL Study Group. J Pediatr Orthop. 2002;22:452–457. [PubMed] [Google Scholar]
- 29. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39:2582–2587. [DOI] [PubMed] [Google Scholar]
- 30. Lind M, Menhert F, Pedersen AB. The first results from the Danish ACL reconstruction registry: epidemiologic and 2 year follow-up results from 5,818 knee ligament reconstructions. Knee Surg Sports Traumatol Arthrosc. 2009;17:117–124. [DOI] [PubMed] [Google Scholar]
- 31. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321–2328. [DOI] [PubMed] [Google Scholar]
- 32. Magnussen RA, Granan LP, Dunn WR, et al. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18:98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mandelbaum BR, Silvers HJ, Watanabe DS, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing anterior cruciate ligament injuries in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003–1010. [DOI] [PubMed] [Google Scholar]
- 34. MARS Group, Wright RW, Huston LJ, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38:1979–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Memtsoudis SG. Limitations associated with the analysis of data from administrative databases. Anesthesiology. 2009;111:449. [DOI] [PubMed] [Google Scholar]
- 36. Memtsoudis SG, González Della Valle A, Besculides MC, Gaber L, Sculco TP. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res. 2008;466:2617–2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mirza F, Mai DD, Kirkley A, Fowler PJ, Amendola A. Management of injuries to the anterior cruciate ligament: results of a survey of orthopaedic surgeons in Canada. Clin J Sport Med. 2000;10:85–88. [DOI] [PubMed] [Google Scholar]
- 38. Miyasaka KC, Daniel DM, Stone ML, Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:3–8. [Google Scholar]
- 39. Musahl V, Jordan SS, Colvin AC, Tranovich MJ, Irrgang JJ, Harner CD. Practice patterns for combined anterior cruciate ligament and meniscal surgery in the United States. Am J Sports Med. 2010;38:918–923. [DOI] [PubMed] [Google Scholar]
- 40. Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39:127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. National Collegiate Athletic Association. NCAA Injury Surveillance System Summary. Indianapolis, IN: National Collegiate Athletic Association; 2002. [Google Scholar]
- 42. National Federation of State High School Associations. 2002 High School Participation Survey. Indianapolis, IN: National Federation of State High School Associations; 2002. [Google Scholar]
- 43. Nielsen AB, Yde J. Epidemiology of acute knee injuries: a prospective hospital investigation. J Trauma. 1991;31:1644–1648. [DOI] [PubMed] [Google Scholar]
- 44. Pate RR, Trost SG, Levin S, Dowda M. Sports participation and health-related behaviors among US youth. Arch Pediatr Adolesc Med. 2000;154:904–911. [DOI] [PubMed] [Google Scholar]
- 45. Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shalala DE. HHS policy for changing the population standard for age adjusting death rates. Memorandum from the Secretary. August 26, 1998. [Google Scholar]
- 47. Shea KG, Pfeiffer R, Wang JH, Curtin M, Apel PJ. Anterior cruciate ligament injury in pediatric and adolescent soccer players: an analysis of insurance data. J Pediatr Orthop. 2004;24:623–628. [DOI] [PubMed] [Google Scholar]
- 48. Shelbourne KD, Carr DR. Meniscal repair compared with meniscectomy for bucket-handle medial meniscal tears in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2003;31:718–723. [DOI] [PubMed] [Google Scholar]
- 49. Smith JP 3rd, Barrett GR. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med. 2001;29:415–419. [DOI] [PubMed] [Google Scholar]
- 50. Stein BE, Srikumaran U, Tan EW, Freehill MT, Wilckens JH. Lower-extremity peripheral nerve blocks in the perioperative pain management of orthopaedic patients: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94:e167. [DOI] [PubMed] [Google Scholar]
- 51. Stundner O, Kirksey M, Chiu YL, et al. Demographics and perioperative outcome in patients with depression and anxiety undergoing total joint arthroplasty: a population-based study. Psychosomatics. 2013;54:149–157. [DOI] [PubMed] [Google Scholar]
- 52. US Department of Commerce. United States Census Bureau. http://www.census.gov/. Accessed June 6, 2014.
- 53. van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. 1992;14:82–99. [DOI] [PubMed] [Google Scholar]
- 54. Wolverton B. Female participation in college sports reaches all-time high. The Chronicle of Higher Education. January 22, 2012 http://chronicle.com/article/Female-Participation-in/130431/. Accessed November 26, 2014. [Google Scholar]



