Abstract
Background:
Beach volleyball is an intensive sport with high impact on the lumbar spine. Low back pain (LBP) is frequent among elite players. Increased prevalence of pathological changes on magnetic resonance imaging (MRI) in the lumbar spine of elite athletes has been reported. Hypothesis: There is an increased prevalence of disc degeneration and spondylolysis in the MRI of the lumbar spine of professional beach volleyball players.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Twenty-nine fully competitive professional male volleyball players (mean age, 28 years) completed outcomes questionnaires and underwent a complete clinical examination and an MRI of their lumbar spine.
Results:
Whereas 86% of players suffered from LBP during their career, the incidence of LBP in the last 4 weeks was 35%. Pain rated using a visual analog scale (VAS) averaged 3 points (range, 0-8). Twenty-three of 29 players (79%) had at least 1 degenerated disc of Pfirrmann grade ≥3. The most affected spinal levels were L4-5 in 14 (48%) and L5-S1 in 15 players (52%); both levels were involved in 5 players (17%). Six of 29 (21%) players showed a spondylolysis grade 4 according to the Hollenburg classification; there was evidence of spondylolisthesis in 2 players. There was no significant correlation between LBP and MRI abnormalities.
Conclusion:
In the lumbar spine MRI of professional beach volleyball players, the prevalence of disc degeneration is 79%. Spondylolysis (21%) is up to 3 times higher compared with the normal population. Abnormal MRI findings did not correlate with LBP, thus MRIs have to be interpreted with caution.
Keywords: beach volleyball, low back pain, disc degeneration, spondylolysis, MRI
Beach volleyball has been an Olympic sport since 1996. It is a fast-moving, overhead-hitting sport, similar to indoor volleyball, but played in teams of 2 on sandy ground. The stop-and-go activities with jumps and overhead hitting of the volleyball expose the lumbar spine to greater stress than normal. Excessive hip-shoulder separation angles are seen during serve and ball release motions. In addition, the lumbar spine is extended to produce a greater impact on the ball. This potentially makes the lumbar spine vulnerable. Low back pain (LBP) is frequent among professional athletes who participate in various sports18,33,38 and is a common reason for loss of playing time among competitive athletes.16,29,38
Lumbar spine abnormalities on magnetic resonance imaging (MRI) are frequently seen in high-level athletes. Disc degeneration is significantly more common in elite gymnasts than in nonathletes.42 In 1991, Bartolozzi et al2 reported that female volleyball players had significantly more abnormalities of their discs on MRI. The prevalence of lumbar spondylolysis in athletes is also higher than in the general population. This might be because of increased loads on the lumbar spine during repetitive bending movements. Several studies have shown that there is a correlation between the throwing motion and radiological abnormalities in the lumbar spine.5,11,36
Similar to the fast bowling action in cricket,5,11 volleyball players have misalignment of their shoulders relative to their pelvis during a smash or serve movement. This might place further stress on the lumbar spine, particularly on the vertebral disc and pars interarticularis.
However, the impact of beach volleyball on the lumbar spine of a high-level athlete is unknown. The purpose of this study was therefore to investigate the lumbar spine of competitive professional male beach volleyball players clinically and with MRI. We were particularly interested in he incidence of LBP and the prevalence of disc degeneration (Figure 1) and spondylolysis. Furthermore, this investigation aimed to compare the clinical findings, patient-reported outcomes, and MRI abnormalities.
Figure 1.

Sagittal T2-weighted MRI scan showing Pfirrmann grade 4 between L5-S1 and a disc protrusion at the same level without nerve compression.
Materials and Methods
Professional male beach volleyball players were examined during the 4 days at the 2012 Beach Volleyball Grand Slam Tournament in Klagenfurt, Austria. All players received written and oral information about the study procedures during the technical meeting at a previous tournament and or during the on-site technical meeting all teams were required to attend. The study protocol was reviewed and approved by the local ethics committee.
Inclusion Criteria
Inclusion criteria were fully competitive male athletes at the Grand Slam Tournament in Klagenfurt with or without back pain, a world ranking in the top 100, and willingness to undergo a detailed examination by a physician, complete a questionnaire, and participate in an MRI study of the lumbar spine. Prior lumbar spine surgery was a criterion for exclusion.
Study Population
Twenty-nine male professional players underwent clinical examination of their low back, including neurological status and bilateral lower extremity strength. All players had an MRI scan of the lumbar spine (L1-S1).
Clinical Assessment
Structured Interview
Each player was interviewed with a detailed questionnaire, including an assessment of career duration (number of years of high-level indoor or beach volleyball activity), the amount of weekly training duration (including games), episodes of LBP including neurological deficiency, as well as use of pain medication and conservative management such as physical therapy. Each player completed the Roland-Morris questionnaire,12 Oswestry low back pain index 2.1,13,15,25,39 and Short Form–36 (SF-36) questionnaire as well as a visual analog scale (VAS). The physical examination of the players was performed by 3 experienced orthopaedic surgeons who are trained in spine surgery (F.K., B.R., and H.F.).
Magnetic Resonance Imaging
All 29 male players who had a clinical examination and completed the questionnaires were asked to undergo a voluntary MRI examination.
All lumbar spine MRIs were done using a 1.5-T machine (Siemens Avanto; Siemens Medical Systems, Erlangen, Germany). The standard imaging protocol included the following: turbo spin echo (TSE) T1-weighted sagittal sequences (field of view [FOV]: 280 mm; repetition time/echo time [TR/TE]: 590/11 ms; slice thickness [SL]: 4 mm; slice gap [SG]: 0.4 mm; base resolution/phase resolution [BR/PR]: 384/75%), TSE T2-weighted sagittal sequences (FOV: 280 mm; TR/TE: 3000/92 ms; SL: 4 mm; SG: 0.4 mm; BR/PR: 384/75%), and TSE T2-weighted transversal sequences (FOV: 240 mm; TR/TE: 3800/108 ms; SL: 4 mm; SG: 0.4 mm; BR/PR: 384/75%). Every lumbar spine MRI was completed from L1 to S1 without fat saturation.
Two experienced musculoskeletal radiologists who were unaware of the study participants’ statuses evaluated the MRIs in consensus.
Degenerative changes to the vertebral body endplate were classified according to the Modic classification.31 The degree of disc degeneration was classified into 5 grades according to Pfirrmann,34 with grade 3 or more considered to be degenerated. In grade 1, the structure of the disc is homogeneous, with a bright hyperintense white signal intensity and normal disc height. Grade 2 shows an inhomogeneous structure of the disc, with a hyperintense white signal. The distinction between nucleus and annulus is a clear, normal disc height. In grade 3, the structure is inhomogeneous, with intermediate gray signal intensity. The distinction between nucleus and annulus is unclear, and the disc height is normal or moderately decreased. In grade 4, the structure of the disc is inhomogeneous, with a hypointense dark gray signal. There is no distinction between nucleus and annulus, and the disc height is reduced. Grade 5 includes a hypointense black signal intensity and collapsed disc space.
In addition, the MRIs were specifically evaluated for spondylolysis and spondylolisthesis (Figure 2). MRI is reliable in detecting abnormalities of the pars interarticularis.7 Stress reactions of the pars interarticularis were classified according to Hollenberg et al.22 Grade 0 is normal without signal abnormalities. Grade 1 shows stress-related marrow edema but no spondylolysis. Grade 2 shows T2-signal abnormalities and thinning, fragmentation, or irregularity of the portion. Grade 3 involves a complete unilateral or bilateral lysis, and in grade 4, there is a complete spondylolysis without T2 abnormalities. The amount of slip was classified according to Meyerding.30
Figure 2.

Sagittal T2-weighted MRI scan showing Pfirrmann grade 4 at levels L5-S1 and grade 3 at levels L3-4 and L4-5. Additionally, there is spondylolisthesis Meyerding grade 1 between L5 and S1.
Compression of the nerves was rated according to Pfirrmann et al.35 Grade 0 denotes a normal nerve exiting out of the foramen. Grade 1 indicates contact of disc material with the nerve root, and the epidural fat layer between the 2 is not evident. Grade 2 indicates that the nerve root is displaced dorsally by disc material, whereas in grade 3, the nerve root is compressed between disc material and the wall of the spinal canal.
Statistical Analysis
We used R statistical software version 2.15.2 for statistical analysis (www.r-project.org). Using the “binomial test” function of the Clopper-Pearson method, we evaluated the size of the confidence interval. The results of our study were compared to the reference we discuss later using the exact binomial test. Since the sample size was less than 30, the Mann-Whitney test was used for paired groups. The level of significance was set at P < .05.
Results
Demographics
The mean age of the 29 players was 28 years (range, 19-39 years). The mean height was 187 cm (range, 179-205 cm), and the mean weight 85 kg (range, 63-100 kg). The athletes’ body mass index averaged 22.6 kg/m2 (range, 19.7-25.6 kg/m2). The average duration of professional beach volleyball activity was 9.8 years (range, 2-20 years) and the average training hours per week was 18.5 (range, 9-35 hours).
Clinical Results
Eighty-six percent of players experienced LBP during their career, 61% during the past 12 months and 31% during the last 4 weeks. Eight players had loss of practice time within the past 12 months because of LBP (27%). Twenty percent took nonsteroidal anti-inflammatory drugs on a regular basis for their back pain. Mean pain on the VAS was 3, with a range from 0 to 8.
Physical Examination
All 29 players showed normal muscle strength for their key muscles (L2-S1). The neurological status for reflexes and sensibility as well as the Lasègue sign were completely normal. The finger floor distance (FFD) was measured to quantify the flexibility of the lumbar spine. Twenty-five players had an FFD of 0 cm, and 4 players showed a reduced FFD, with a mean distance of 9.5 cm (range, 5-15 cm).
Questionnaires
The Roland-Morris score and the Oswestry back index showed no abnormal results for the players. Details of the SF-36 are depicted in Figure 3. According to Khanna and Tsevat,25 the SF-36 of the beach volleyball players was compared with the results of the US population. The mean Mental Component Summary score was 53.5 (range, 48.6-62.9) and the Physical Component Summary score 55.5 (range, 43.2-61.5); both results were better when compared with the normal population.
Figure 3.
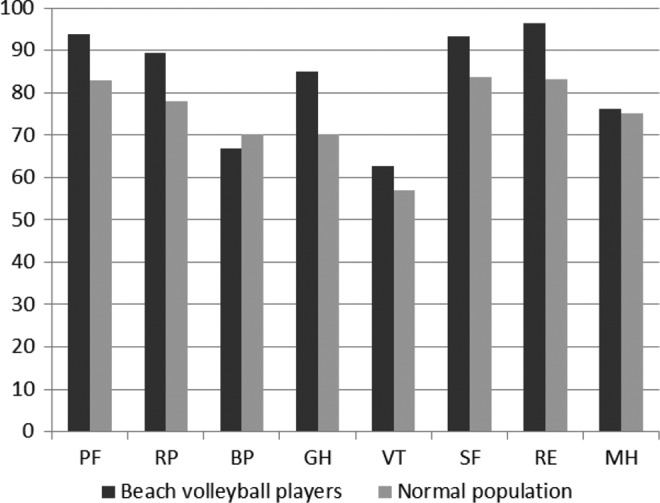
Mean values for the Short Form–36 (SF-36) questionnaire in beach volleyball players compared with the normal population. PF, physical functioning; RP, role-physical; BP, body pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Magnetic Resonance Imaging
Details of the different abnormal MRI findings are depicted in Tables 1 and 2. Twenty-three of 29 players showed a disc degeneration (Pfirrmann grade ≥3) between L1 and S1 (79%). The most affected levels were L4-5 (n = 14; 48%) and L5-S1 (n = 15; 52%). The upper lumbar levels were less degenerated, L1-2 and L3-4 were affected in 8% whereas L2-3 was affected in 10% of players. Overall, of the 145 disc levels, 40 were degenerated (28%). The presence of more than 1 degenerated disc was observed in 11 of these 23 players (48%). On average, each player had nearly 2 degenerated discs in his lumbar spine.
TABLE 1.
Frequency of Abnormal MRI Findings for Each Lumbar Level (N = 29 Players)
| Lumbar Level | |||||
|---|---|---|---|---|---|
| L1-2 | L2-3 | L3-4 | L4-5 | L5-S1 | |
| Schmorl nodes | 3 | 3 | 0 | 1 | 1 |
| Osteochondrosis | 3 | 5 | 2 | 12 | 11 |
| Disc bulging | 0 | 1 | 0 | 4 | 1 |
| Disc protrusion | 0 | 0 | 0 | 6 | 8 |
| Disc extrusion | 0 | 0 | 0 | 1 | 1 |
| Disc compression | 0 | 0 | 0 | 5 | 6 |
| Spondylolysis | 0 | 0 | 1 | 1 | 5 |
| Spondylolisthesis | 0 | 0 | 0 | 1 | 1 |
| Pfirrmann grade | |||||
| 1 | 19 | 21 | 22 | 13 | 12 |
| 2 | 6 | 3 | 4 | 2 | 3 |
| 3 | 2 | 4 | 3 | 9 | 5 |
| 4 | 2 | 1 | 0 | 5 | 9 |
| 5 | 0 | 0 | 0 | 0 | 1 |
| Modic changes grade | |||||
| 1 | 0 | 0 | 0 | 0 | 0 |
| 2 | 1 | 0 | 1 | 2 | 3 |
| 3 | 0 | 0 | 0 | 0 | 0 |
TABLE 2.
Number of Athletes With >1 Spinal Level Affected: Distribution by MRI Parametera
| Number of Levels Affected | |||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Schmorl nodes | 24 | 3 | 1 | 1 | |
| Osteochondrosis | 11 | 8 | 6 | 3 | |
| Disc bulging | 23 | 6 | |||
| Disc protrusion | 18 | 8 | 3 | ||
| Disc extrusion | 27 | 2 | |||
| Disc compression | 24 | 1 | 3 | 1 | |
| Spondylolysis | 23 | 5 | 1 | ||
| Spondylolisthesis | 27 | 2 | |||
| Pfirrmann grade 3-5 | 15 | 12 | 1 | 1 | |
| Modic changes grade 2 | 7 | 9 | 10 | 1 | 2 |
aOnly 7 of 29 athletes had no pathological changes.
Six of 29 (20.7%) players showed a spondylolysis grade 4 according to Hollenberg et al.22 L5-S1 was the most affected level (>70%). One player showed a lysis at 2 consecutive levels (L3-4 and L4-5). In 33% of spondylolysis lesions, there was also spondylolisthesis (2 of 6 lesions).
Modic grade 1 changes were seen in 21% of the athletes; again, the highest rate was found in the last 2 levels of the lumbar spine (L4/5 and L5/S1, 71%).
Overall, 5 players (17%) showed Schmorl nodes in the upper lumbar levels, with more than two thirds at L1-2 and L2-3 levels.
Pfirrmann grade 3 nerve compression, where the nerve root is compressed between disc material and the wall of the spinal canal, was detected in 4 players—3 at the L4-5 level.
We were not able to show a significant correlation between radiological abnormalities and LBP measured using the VAS, Roland-Morris, SF-36, or Oswestry questionnaires.
Discussion
Beach volleyball is an intense sport that repetitively stresses the lumbar spine with axial and torsional loads. This cross-sectional study evaluated the lumbar spine clinically and with MRI in 29 professional male beach volleyball players.
Of these, 86% experienced LBP during at least one point of their career, more than 60% during the past 12 months, and 35% during the past 4 weeks. This incidence is higher than the 72% reported by Hangai et al,19 who analyzed students participating in competitive sports for more than 8 hours per week. Likewise, there are other published data showing that low back symptoms are significantly more common in athletes than in controlled groups.1,4,27,42 Even in retired athletes, as shown by Granhed and Morelli17 in wrestlers, LBP was still significantly higher compared with age-matched controls (59% vs 31%). There is not much in the literature regarding disc degeneration in volleyball. Auvinen et al1 stated that volleyball is among youth sports that correlate with a higher prevalence of LBP, especially in boys. Overall, our data show that LBP has not only a high prevalence in male beach volleyball players, but that this prevalence is also one of the highest reported in all sports.
Analysis of the lumbar spine MRI of the 29 beach volleyball players revealed several abnormal MRI findings, including a high prevalence of disc degeneration (80%), Modic vertebral body end plate changes (21%), spondylolysis (21%), spondylolisthesis (7%), and Schmorl nodes (17%). Twenty-three players showed disc degeneration of equal to or greater than grade 3 in at least one level. Looking specifically at each disc level, the lower levels (L4-S1) are more affected, as previously shown in the literature.4,26 Twenty-nine discs were degenerated at levels L4-5 (n = 14) and L5-S1 (n = 15). Only 4 discs at L1-2 and L2-3 and 3 discs at L3-4 showed disc degeneration of Pfirrmann grade 3 or greater. More than 1 disc was degenerated in 11 players (48%).
To our knowledge, only 1 study has been published on indoor volleyball players. Bartolozzi et al2 showed a prevalence of disc alterations (including disc degeneration, bulging, and herniation) of 44%, which is clearly lower than our data. The higher prevalence in our study might be because of better imaging techniques and the use of an MRI classification system for disc degeneration. One would expect a lower number of degenerated discs in beach volleyball as it is played on softer ground than indoor volleyball. Having examined only 29 male beach volleyball players, we are not able to extrapolate these data to the sport as a whole.
Disc degeneration is also known in other sports. Swärd et al42 found a 75% incidence of degenerated disc in elite gymnasts. In 2003, Ong et al32 analyzed 31 Olympic athletes at the Sydney Games in 2000 who presented with lower back pain and/or sciatica. In their study population, 72% had degenerated discs at the L5-S1 level.32 In young cricket fast bowlers, the prevalence of intervertebral disc abnormalities was 65%.19 Burnett et al,6 in a follow-up study, showed that there was a significant increase in the occurrence of disc degeneration within 4 years in young cricket players. However, in most studies, the exact criteria used to distinguish between mild and severe disc degeneration were not given. Therefore, it is not possible to compare our data directly with these results as we used the Pfirrmann classification for disc degeneration.
Comparing disc degeneration in athletes with nonathletes in the literature, there was clearly more degeneration in athletes.20,21,28,37,42 Cheung et al,9 in their MRI study on 1043 subjects, showed that the prevalence of disc degeneration in individuals younger than 30 years was 40%, whereas in most studies, the prevalence was higher than 65%.
These data confirm our second hypothesis, that the prevalence of spondylolysis is higher in beach volleyball players than in the general population, where the defect in the pars interarticularis is approximately 5%, as reported by Hu et al.23 Within this cohort, 21% had a lysis, with L5 being the most affected level (72%).
The prevalence of spondylolysis seems to be higher in specific sports. Divers, wrestlers, weight lifters, and throwing athletes tend to have a higher prevalence (23%-30%) than the general population.40,41 In the present study, 2 players had a grade 1 slip and a lysis at the same level. Overall, we only identified 2 players with a slip in our study population (6.7%). This might be because of the fact that we used MRI, where a slip may be reduced because of the supine position of the patient.
It is widely believed that repetitive loading on the lumbar spine leads to stress fractures. Stress on the disc can cause annulus tears, which can lead to nuclear desiccation and loss of proteoglycan content. This may start the degenerative cascade in a motion segment. There are several potential pain generators within the intervertebral segment that might induce LBP. In a review, Bono4 showed that large forces are produced during athletic maneuvers. During a blocking maneuver in football, shear forces on a motion segment can reach 3300 N and compressive loads can reach up to 8600 N. A golf swing produces up to 7500 N of compressive force on the lumbar spine, rowing action produces compressive forces of approximately 6100 N, and weight lifting more than 17,000 N.8,10,14,22
Elliott et al11,12 studied the correlation between the motion of young fast cricket bowlers and MRI changes in the disc. They saw a significant association between the degree of shoulder and hip rotation and disc degeneration.11,12 Furthermore, they were able to show that the incidence and progression of lumbar disc degeneration significantly decreased in concert with reduced shoulder counter-rotation.
Analogous to fast bowling in cricket, volleyball players put a mechanical load on their lumbar spine during the jump serve motion. Excessive hip-shoulder separation angles are seen during serve and ball release motions, which might increase the shear forces and place additional stress on the lumbar discs. Shear forces are also increased during a blocking maneuver, analogous to football but less accentuated. This repetitive stress on the disc might be responsible for the increased incidence in bony and disc abnormalities in professional beach volleyball players.
It remains unclear if there is an association between radiologic abnormalities and LBP. In a study on Japanese college football players, spondylolysis and disc space narrowing were significant risk factors for LBP.24 Decreased signal intensity within the disc of athletes correlates positively with LBP.42,43 Interestingly, LBP is more strongly predicted by life dissatisfaction, neuroticism, hostility, extroversion, and poor sleep quality.3
The present study did not show an association between radiologic abnormalities and LBP. The small sample size with only male players is one of the weaknesses of our study. Only male players were investigated because our ethics committee did not allow inclusion of female beach volleyball players without a pregnancy test. As we mainly focused on pain in association with radiologic abnormalities, we did not investigate the correlation between spine mobility and pain. Because of the special on-site study setting, we did not analyze the sagittal and coronal alignment of the spine. Furthermore, our ethics committee had serious concerns about using spine radiographs for this study.
Conclusion
This study proved our hypothesis that there is a high prevalence of disc degeneration and spondylolysis in the lumbar spine of professional beach volleyball players. We found no correlation between LBP and MRI abnormalities in our study subjects.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Mutanen PO, Karppinen JI. Musculoskeletal pains in relation to different sport and exercise activities in youth. Med Sci Sports Exerc. 2008;40:1890–1900. [DOI] [PubMed] [Google Scholar]
- 2. Bartolozzi C, Caramella D, Zampa V, Dal Pozzo G, Tinacci E, Balducci F. The incidence of disk changes in volleyball players. The magnetic resonance findings. Radiol Med. 1991;82:757–760. [PubMed] [Google Scholar]
- 3. Bono CM. Interspinous process devices in the lumbar spine. J Spinal Disord Tech. 2007;20:255–261. [DOI] [PubMed] [Google Scholar]
- 4. Bono CM. Low-back pain in athletes. J Bone Joint Surg Am. 2004;86-A:382–396. [DOI] [PubMed] [Google Scholar]
- 5. Burnett AF, Barrett CJ, Marshall RN, Elliott BC, Day RE. Three-dimensional measurement of lumbar spine kinematics for fast bowlers in cricket. Clin Biomech (Bristol Avon). 1998;13:574–583. [DOI] [PubMed] [Google Scholar]
- 6. Burnett AF, Khangure MS, Elliott BC, Foster DH, Marshall RN, Hardcastle PH. Thoracolumbar disc degeneration in young fast bowlers in cricket: a follow-up study. Clin Biomech (Bristol Avon). 1996;11:305–310. [DOI] [PubMed] [Google Scholar]
- 7. Campbell RS, Grainger AJ, Hide IG, Papastefanou S, Greenough CG. Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol. 2005;34:63–73. [DOI] [PubMed] [Google Scholar]
- 8. Cappozzo A, Felici F, Figura F, Gazzani F. Lumbar spine loading during half-squat exercises. Med Sci Sports Exerc. 1985;17:613–620. [PubMed] [Google Scholar]
- 9. Cheung KM, Karppinen J, Chan D, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009;34:934–940. [DOI] [PubMed] [Google Scholar]
- 10. Cholewicki J, McGill SM, Norman RW. Lumbar spine loads during the lifting of extremely heavy weights. Med Sci Sports Exerc. 1991;23:1179–1186. [PubMed] [Google Scholar]
- 11. Elliott B, Khangure M. Disk degeneration and fast bowling in cricket: an intervention study. Med Sci Sports Exerc. 2002;34:1714–1718. [DOI] [PubMed] [Google Scholar]
- 12. Elliott BC, Hardcastle PH, Burnett AE, Foster DH. The influence of fast bowling and physical factors on radiologic features in high performance young fast bowlers. Sports Med Train Rehabil. 1992;3:113–130. [Google Scholar]
- 13. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 14. Foster D, John D, Elliott B, Ackland T. Back injuries to fast bowlers in cricket: a prospective study. Br J Sports Med. 1989;23:150–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther. 2001;81:776–788. [DOI] [PubMed] [Google Scholar]
- 16. Gatt CJ, Jr, Hosea TM, Palumbo RC, Zawadsky JP. Impact loading of the lumbar spine during football blocking. Am J Sports Med. 1997;25:317–321. [DOI] [PubMed] [Google Scholar]
- 17. Granhed H, Morelli B. Low back pain among retired wrestlers and heavyweight lifters. Am J Sports Med. 1988;16:530–533. [DOI] [PubMed] [Google Scholar]
- 18. Hainline B. Low back injury. Clin Sports Med. 1995;14:241–265. [PubMed] [Google Scholar]
- 19. Hangai M, Kaneoka K, Hinotsu S, et al. Lumbar intervertebral disk degeneration in athletes. Am J Sports Med. 2008;37:149–155. [DOI] [PubMed] [Google Scholar]
- 20. Hangai M, Kaneoka K, Okubo Y, et al. Relationship between low back pain and competitive sports activities during youth. Am J Sports Med. 2010;38:791–796. [DOI] [PubMed] [Google Scholar]
- 21. Hellström MM, Jacobsson BB, Swärd LL, Peterson LL. Radiologic abnormalities of the thoraco-lumbar spine in athletes. Acta Radiol. 1990;31:127–132. [PubMed] [Google Scholar]
- 22. Hollenberg GM, Beattie PF, Meyers SP, Weinberg EP, Adams MJ. Stress reactions of the lumbar pars interarticularis: the development of a new MRI classification system. Spine. 2002;27:181–186. [DOI] [PubMed] [Google Scholar]
- 23. Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008;90:656–671. [PubMed] [Google Scholar]
- 24. Iwamoto J, Abe H, Tsukimura Y, Wakano K. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school and college football players. Am J Sports Med. 2004;32:781–786. [DOI] [PubMed] [Google Scholar]
- 25. Khanna D, Tsevat J. Health-related quality of life—an introduction. Am J Manag Care. 2007;13(suppl 9):S218–S223. [PubMed] [Google Scholar]
- 26. Kjaer P, Leboeuf-Yde C, Korsholm L, Sorensen JS, Bendix T. Magnetic resonance imaging and low back pain in adults: a diagnostic imaging study of 40-year-old men and women. Spine. 2005;30:1173–1180. [DOI] [PubMed] [Google Scholar]
- 27. Kujala UM, Taimela S, Erkintalo M, Salminen JJ, Kaprio J. Low-back pain in adolescent athletes. Med Sci Sports Exerc. 1996;28:165–170. [DOI] [PubMed] [Google Scholar]
- 28. Lundin O, Hellström M, Nilsson I, Swärd L. Back pain and radiological changes in the thoraco-lumbar spine of athletes. A long-term follow-up. Scand J Med Sci Sports. 2001;11:103–109. [DOI] [PubMed] [Google Scholar]
- 29. McCarroll JR, Miller JM, Ritter MA. Lumbar spondylolysis and spondylolisthesis in college football players. A prospective study. Am J Sports Med. 1986;14:404–406. [DOI] [PubMed] [Google Scholar]
- 30. Meyerding HW. Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg. 1956;26(part 1):566–591. [PubMed] [Google Scholar]
- 31. Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168:177–186. [DOI] [PubMed] [Google Scholar]
- 32. Ong A, Anderson J, Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003;37:263–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Orchard J, James T, Alcott E, Carter S, Farhart P. Injuries in Australian cricket at first class level 1995/1996 to 2000/2001. Br J Sports Med. 2002;36:270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. [DOI] [PubMed] [Google Scholar]
- 35. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004;230:583–588. [DOI] [PubMed] [Google Scholar]
- 36. Portus M, Mason BR, Elliott BC, Pfitzner MC, Done RP. Technique factors related to ball release speed and trunk injuries in high performance cricket fast bowlers. Sports Biomech. 2004;3:263–284. [DOI] [PubMed] [Google Scholar]
- 37. Rachbauer F, Sterzinger W, Eibl G. Radiographic abnormalities in the thoracolumbar spine of young elite skiers. Am J Sports Med. 2001;29:446–449. [DOI] [PubMed] [Google Scholar]
- 38. Ranson CA, Kerslake RW, Burnett AF, Batt ME, Abdi S. Magnetic resonance imaging of the lumbar spine in asymptomatic professional fast bowlers in cricket. J Bone Joint Surg Br. 2005;87:1111–1116. [DOI] [PubMed] [Google Scholar]
- 39. Rocchi MB, Sisti D, Benedetti P, Valentini M, Bellagamba S, Federici A. Critical comparison of nine different self-administered questionnaires for the evaluation of disability caused by low back pain. Eura Medicophys. 2005;41:275–281. [PubMed] [Google Scholar]
- 40. Rossi F, Dragoni S. Lumbar spondylolysis: occurrence in competitive athletes. Updated achievements in a series of 390 cases. J Sports Med Phys Fitness. 1990;30:450–452. [PubMed] [Google Scholar]
- 41. Soler T, Calderón C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000;28:57–62. [DOI] [PubMed] [Google Scholar]
- 42. Swärd L, Hellström M, Jacobsson B, Nyman R, Peterson L. Disc degeneration and associated abnormalities of the spine in elite gymnasts. A magnetic resonance imaging study. Spine. 1991;16:437–443. [DOI] [PubMed] [Google Scholar]
- 43. Videman TT, Sarna SS, Battié MC, et al. The long-term effects of physical loading and exercise lifestyles on back-related symptoms, disability, and spinal pathology among men. Spine. 1995;20:699–709. [DOI] [PubMed] [Google Scholar]


