Abstract
Background:
Lateral ulnar collateral ligament (LUCL) reconstruction requires proper understanding and identification of anatomic structures about the lateral elbow. The insertion site of the LUCL is based on the supinator tubercle.
Purpose:
To characterize the supinator tubercle relative to other surrounding anatomic landmarks.
Study Design:
Descriptive laboratory study.
Methods:
Computed tomography (CT) scans of 10 adult elbows were retrospectively reviewed. These CT scans were converted into patient-specific 3-dimensional computer models. Using a user-defined coordinate system, an ulnar Cartesian coordinate system was defined with anatomic landmarks as reference points to standardize the position of each model. The length of the supinator crest was measured. Following this, the crest was examined for a distinct raised bony tuberosity that would be consistent with the supinator tubercle. If no distinctly raised tubercle was noted, the most prominent appearing location of the crest distal to the radial notch was considered the tubercle. The distance from the proximal radial head junction to the supinator tubercle was recorded. Finally, the distance from the supinator crest at the radial head junction to the posterior cortex in the sagittal plane was measured.
Results:
The supinator tubercle was found to be prominent in 5 of 10 ulnar models. The supinator crest was 43.59 ± 13.28 mm long, and the supinator tubercle lateral extrusion was 5.60 ± 0.90 mm. The distance between the radial head junction and the supinator tubercle was found to be 15 ± 2.37 mm, and the distance from the supinator crest at the radial head junction to the posterior cortex was 10.25 ± 2.07 mm.
Conclusion:
The supinator tubercle is frequently not prominent or easily recognizable. Its relationship to other structures is of value. The proximal border of the radial head, residing 15 mm proximal to the most predictable location of the supinator tubercle, is a useful landmark when drilling tunnels during LUCL reconstructions.
Clinical Relevance:
Results of this study may aid proper anatomic LUCL reconstruction.
Keywords: posterolateral rotatory instability of the elbow, supinator tubercle, anatomy, lateral ulnar collateral reconstruction, elbow, CT imaging
Posterolateral rotatory instability (PLRI) of the elbow was first described by O’Driscoll et al13 in 1991. Since then, much research has established the importance of the lateral ulnar collateral ligament (LUCL) and other ligaments of the LUCL complex and its association with PLRI.5,10,13,17 While there is literature that suggests that the isolated damage to the LUCL complex does not lead to PLRI of the elbow, the surgical treatment of choice frequently involves reconstruction of the LUCL complex.4,8,9,13–15 Morrey and An,12 based on anatomical research, determined that the LUCL traverses from the lateral epicondyle to the supinator tubercle.
Anatomic reconstruction of the LUCL requires proper and predictable identification of the supinator tubercle.12 In addition, if the supinator tubercle cannot be identified, other predictable landmarks must be used. Therefore, the purposes of this study were to (1) establish the incidence of prominent and easily identifiable supinator tubercles and (2) determine the relationship between the supinator tubercle and other osseous structures about the lateral elbow.
Materials and Methods
After institutional review board approval was obtained, elbow computed tomography (CT) scans of 17 adults were retrospectively reviewed for inclusion in our study. These images were previously obtained for diagnostic workup of several pathologies, including valgus instability, olecranon stress fracture, and valgus extension overload. The CT scan protocol included 0.5-mm axial cuts with inclusion of the distal humerus through the proximal radius and ulna in the Digital Imaging and Communications in Medicine (DICOM) format. Exclusion criteria included poor CT quality, inadequate visualization of the entire supinator crest, and age younger than 18 years. Ten patients with adequate CT scans met criteria for inclusion in this study. These CT scans were converted into patient-specific 3-dimensional computer models of the elbow using the Materialise Interactive Medical Image Control System software (Mimics; Materialise, Ann Arbor, Michigan, USA). The use of this software to produce anatomically accurate models has been previously verified in shoulder2 and elbow3 models. These elbow models were then uploaded into Materialise’s rapid-prototyping software (Magics; Materialise), where they could be manipulated for exact measurements. Using the software’s ability to create user-defined coordinate systems, an ulnar Cartesian coordinate system was defined with anatomic landmarks as reference points to standardize the position of each model (Figure 1).16 The y-axis was defined by the longitudinal axis of the ulna, and the x-axis was the transepicondylar axis and defined as the perpendicular line connecting the y-axis with the supinator crest. The z-axis was then created as the line perpendicular to both the x- and y-axes to create a 3-dimensional coordinate system. This Cartesian coordinate system allowed us to manipulate the models in a standardized fashion, maintaining the exact positions of the ulna while making measurements.
Figure 1.
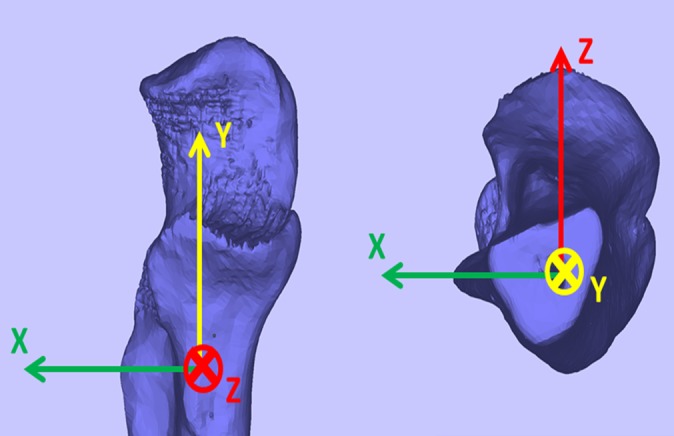
Ulnar model created with use of specific Cartesian coordinate system standardizing the positions of each model based on anatomic landmarks. The y-axis was defined by the longitudinal axis of the ulna, and the x-axis was the transepicondylar axis.
Measurements of the supinator crest were made by examining the lateral aspect of the ulnar models in the sagittal plane. The length of the supinator crest was measured from the proximal origin at the posterior aspect of the radial notch to the point at which it became indistinguishable from the normal contours of the ulnar cortex (Figure 2). The crest was then examined for a distinct raised bony tuberosity, which would represent the supinator tubercle (Figure 3). The tubercle extrusion of the tubercle from the existing ulnar cortex was measured in the coronal plane (Figure 2). If no distinctly raised tubercle was noted, then the most prominent appearing location of the crest distal to the radial notch was considered the tubercle. The 3-dimensional model of the radius was overlaid on the ulnar model to determine the projection of the center of the radial head onto the ulna, and the distance from this radial head junction to the supinator tubercle was recorded (Figure 2). Finally, the distance from the supinator crest at the radial head junction to the posterior cortex in the sagittal plane was measured, as proximal ulnar tunnels, when used, are in this location.
Figure 2.
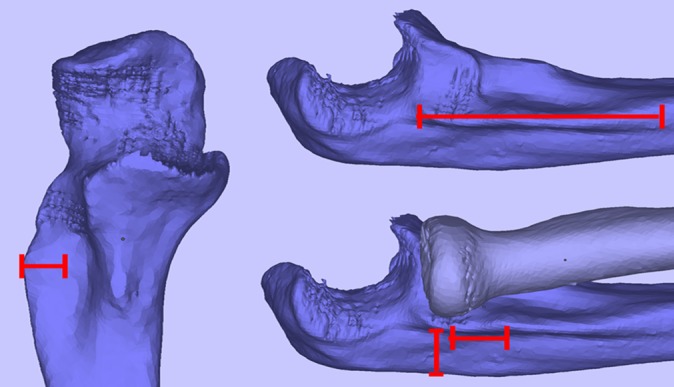
Supinator crest measurements in multiple planes. Specifically, measuring the length, height, and width of the crest.
Figure 3.
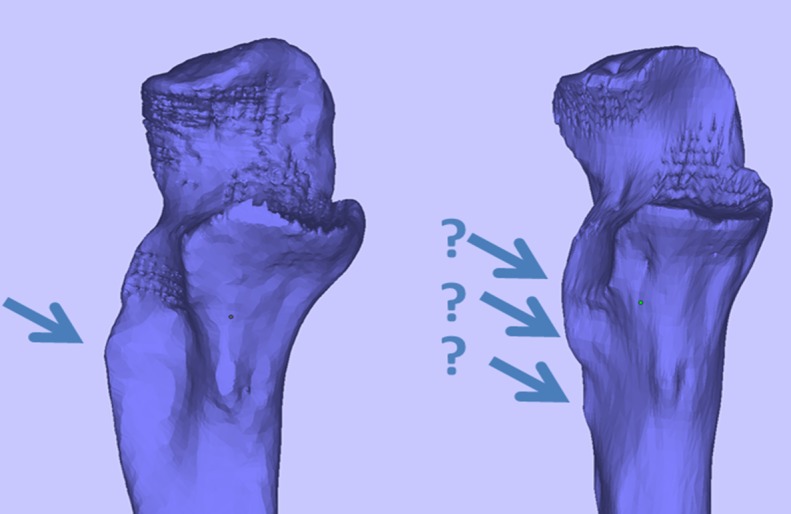
Functional anatomy of the ligaments of the elbow. Evaluation of supinator tubercle on supinator crest. These models evaluated the presence of specific bony protuberance in the supinator crest that would represent the supinator tubercle.
Results
Of the 17 elbows assessed, 10 satisfied our inclusion and exclusion criteria and were included. The average age of the study group was 29.4 years (range, 19-61 years). The supinator tubercle was found to be prominent in 5 of 10 (50%) ulnar models and was in the distal half of the supinator crest in all cases. Measurements are given as mean ± standard deviation. The supinator crest was 43.592 ± 13.28 mm long and present in all models, and the supinator tubercle extrusion was 5.604 ± 0.90 mm. The distance between the radial head junction and the supinator tubercle was found to be 15.003 ± 2.37 mm, and the distance from the supinator crest at the radial head junction to the posterior cortex was 10.253 ± 2.07 mm (Table 1, Figure 4).
TABLE 1.
Anatomy of the Supinator Tuberclea
| Prominence of tubercle, % | 50 |
| Supinator crest length, mm | 43.592 ± 13.28 |
| Extrusion of tubercle, mm | 5.604 ± 0.90 |
| Radial head junction to supinator tubercle, mm | 15.003 ± 2.37 |
| Supinator crest to posterior cortex, mm | 10.253 ± 2.07 |
aValues are expressed as mean ± standard deviation unless otherwise indicated.
Figure 4.
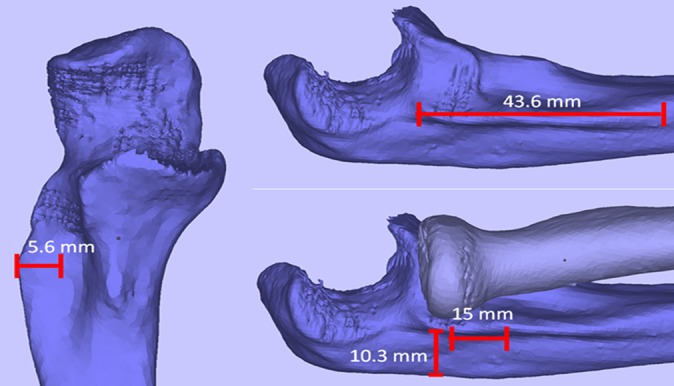
Ulnar models with respective measurements of interest. Specifically, the length, width, height, and distance from the radial head to the supinator crest.
Discussion
Myriad techniques for performing LUCL reconstructions exist. However, the principle remains to achieve anatomic re-creation of the native ligament with the use of autograft or allograft. Surgical management is recommended in properly selected patients with PLRI of the elbow that have failed nonoperative management. While most authors describe placement of the ulnar tunnel at or close to the site of the supinator tubercle, we have found from clinical practice that the supinator tubercle, unlike the supinator crest, is sometimes difficult to identify with certainty intraoperatively. Therefore, we sought to determine specific parameters and measurements relative to the supinator crest. We believe that anatomic landmarks relative to the supinator tubercle can serve as secondary queues and aid in confirmation of proper tunnel placement intraoperatively.
In this study, we noted the supinator tubercle to be prominent in 50% of the cadaver specimens. In addition, it extruded approximately 5.6 mm on average lateral to the supinator crest. Therefore, it is possible that a significant number of LUCL reconstructions may be nonanatomic at the ulnar insertion site. This is important as the native LUCL is known to be nonisometric in nature, shortening and lengthening in extension and flexion, respectively.1,6,11 Therefore, it is plausible that significant variations from normal anatomy will lead to an ineffective reconstruction or failure. Intraoperative assessment is likely to be more accurate than imaging modalities, and we recommend thorough assessment for the likely insertion of the native LUCL. However, excessive dissection should be avoided to limit risks to neurologic structures (specifically the posterior interosseous nerve) and/or further ligamentous damage. We do not routinely use fluoroscopy to identify the supinator tubercle; however, it may be a helpful tool. In addition, selected tunnels can be confirmed under fluoroscopy as being safe from the radiocapitellar joint. While studies evaluating outcomes after LUCL reconstructions are limited, there have been some reports of relatively high failure rates. In the study by Jones et al,7 a recurrence rate of 25% was noted in their series of patients with PLRI that underwent reconstructions. Sanchez-Sotelo et al,15 in a study of 44 patients who underwent surgical management for PLRI (11 repairs and 33 reconstructions), noted that 5 (11%) had postoperative instability. The cause of failure following surgery is likely multifactorial; however, improper tunnel placement is a possible etiology.
Use of predictable anatomic landmarks can be useful if the supinator tubercle is not easily apparent. Within a small standard deviation, we noted that the tubercles were 15 ± 2.37 mm distal to the proximal margin of the radial head. Goren et al6 performed a cadaveric study attempting to identify the most isometric origin and insertion points for LUCL reconstructions using 1.8-mm drill holes and electromagnetic sensors. The points along the ulna were along the supinator crest and were spaced 4 mm apart beginning 4 mm proximal to the radial head. They were unable to create an isometric construct but noted that tunnels placed on the supinator crest within 16 to 20 mm produced the most isometric configurations with the least change in length with motion.6 The supinator tubercle was not identified in this study. Based on the data noted in our study, we recommend that the dissection along the ulna be carried beyond 15 mm distal to the proximal aspect of the radial head and that the distal ulnar tunnel be placed in this location.
There are limitations to this study. Although the methods of this study have been used and validated in others, it may not be as accurate as a cadaveric study and is subject to potential accuracy errors and inter- and intraobserver discrepancies. The study would be further strengthened by cadaveric confirmation, which we will be performing. Ten adult patients with no history of lateral elbow pathology were included in this study. A larger patient cohort would prevent potential bias and increase accuracy and repeatability of our findings. However, the small standard deviation of our measurements indicates consistency despite the small size. As this study is observational and not comparative, a power analysis was not needed. This study may serve as a pilot for larger scale studies.
Conclusion
We believe this study represents the first to evaluate the supinator tubercle anatomy in relation to the supinator crest and radial head. The supinator tubercle may be absent or not easily identified in some patients. This is of importance during LUCL reconstructions. In these situations, we recommend that the ulna tunnel be drilled approximately 15 mm distal to the proximal margin of the radial head.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. Orthop Clin North Am. 2008;39:141–154. [DOI] [PubMed] [Google Scholar]
- 2. Bryce CD, Pennypacker JL, Kulkarni N, et al. Validation of three-dimensional models of in situ scapulae. J Shoulder Elbow Surg. 2008;17:825–832. [DOI] [PubMed] [Google Scholar]
- 3. Byram IR, Khanna K, Gardner TR, Ahmad CS. Characterizing bone tunnel placement in medial ulnar collateral ligament reconstruction using patient-specific 3-dimensional computed tomography modeling. Am J Sports Med. 2013;41:894–902. [DOI] [PubMed] [Google Scholar]
- 4. DeLaMora SN, Hausman M. Lateral ulnar collateral ligament reconstruction using the lateral triceps fascia. Orthopedics. 2002;25:909–912. [DOI] [PubMed] [Google Scholar]
- 5. Dunning CE, Zarzour ZD, Patterson SD, Johnson JA, King GJ. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83–A: 1823–1828. [DOI] [PubMed] [Google Scholar]
- 6. Goren D, Budoff JE, Hipp JA. Isometric placement of lateral ulnar collateral ligament reconstructions: a biomechanical study. Am J Sports Med. 2010;38:153–159. [DOI] [PubMed] [Google Scholar]
- 7. Jones KJ, Dodson CC, Osbahr DC, et al. The docking technique for lateral ulnar collateral ligament reconstruction: surgical technique and clinical outcomes. J Shoulder Elbow Surg. 2012;21:389–395. [DOI] [PubMed] [Google Scholar]
- 8. Lee BP, Teo LH. Surgical reconstruction for posterolateral rotatory instability of the elbow. J Shoulder Elbow Surg. 2003;12:476–479. [DOI] [PubMed] [Google Scholar]
- 9. Lin KY, Shen PH, Lee CH, Pan RY, Lin LC, Shen HC. Functional outcomes of surgical reconstruction for posterolateral rotatory instability of the elbow. Injury. 2012;43:1657–1661. [DOI] [PubMed] [Google Scholar]
- 10. McAdams TR, Masters GW, Srivastava S. The effect of arthroscopic sectioning of the lateral ligament complex of the elbow on posterolateral rotatory stability. J Shoulder Elbow Surg. 2005;14:298–301. [DOI] [PubMed] [Google Scholar]
- 11. Moritomo H, Murase T, Arimitsu S, Oka K, Yoshikawa H, Sugamoto K. The in vivo isometric point of the lateral ligament of the elbow. J Bone Joint Surg Am. 2007;89:2011–2017. [DOI] [PubMed] [Google Scholar]
- 12. Morrey BF, An KN. Functional anatomy of the ligaments of the elbow. Clin Orthop Relat Res. 1985;(201):84–90. [PubMed] [Google Scholar]
- 13. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73:440–446. [PubMed] [Google Scholar]
- 14. Olsen BS, Sojbjerg JO. The treatment of recurrent posterolateral instability of the elbow. J Bone Joint Surg Br. 2003;85:342–346. [DOI] [PubMed] [Google Scholar]
- 15. Sanchez-Sotelo J, Morrey BF, O’Driscoll SW. Ligamentous repair and reconstruction for posterolateral rotatory instability of the elbow. J Bone Joint Surg Br. 2005;87:54–61. [PubMed] [Google Scholar]
- 16. Shiba R, Sorbie C, Siu DW, Bryant JT, Cooke TD, Wevers HW. Geometry of the humeroulnar joint. J Orthop Res. 1988;6:897–906. [DOI] [PubMed] [Google Scholar]
- 17. Takigawa N, Ryu J, Kish VL, Kinoshita M, Abe M. Functional anatomy of the lateral collateral ligament complex of the elbow: morphology and strain. J Hand Surg Br. 2005;30:143–147. [DOI] [PubMed] [Google Scholar]


