Abstract
Background:
Youth sports programs are extremely popular throughout the United States, with children starting formal sports participation as young as 4 years. This places children at greater risk for concussions and other trauma.
Purpose:
To describe the epidemiology of concussions sustained during participation in 9 organized sports prior to participation in high school athletics.
Methods:
Over an 11-year span from January 2002 to December 2012, the authors reviewed the concussions sustained by athletes aged 4 to 13 years while playing basketball, baseball, football, gymnastics, hockey, lacrosse, soccer, softball, and wrestling, as evaluated in emergency departments (EDs) in the United States and captured by the National Electronic Injury Surveillance System (NEISS) database of the US Consumer Product Safety Commission.
Study Design:
Descriptive epidemiology study.
Results:
There were 4864 (national estimate [NE] = 117,845) youth athletes evaluated in NEISS EDs as sustaining concussions from 2002 to 2012. Except for the year 2007, concussion frequencies trended upward throughout the 11-year time frame as well as with increasing age. Loss of consciousness (LOC) occurred in 499 cases (NE, 12,129; 10%). Football had the highest frequency of concussions, with 2013 (NE, 51,220; 41%), followed by basketball, with 977 (NE, 22,099; 20%), and soccer, with 801 (NE, 18,916; 17%). The majority of concussions were treated in the outpatient setting, with 4444 (91.4%) patients being treated and released; 412 (9%) patients required admission and were found to have increased frequencies of LOC (n = 17; 18.0%) compared with LOC in the total group (n = 499, 10%). The total number of player-to-player injury mechanisms mirrored the total number of concussions by year, which increased throughout the 11-year span, except for the year 2007. Subgroup analysis of athletes aged 4 to 7 years demonstrated a difference in the mechanism of injury distribution, with a ball-to-head mechanism increase of 5% from 15% to 20% and a player-to–other object mechanism of injury increase by more than double to 13% compared with the entire cohort over the 11-year time frame.
Conclusion:
Within the 4- to 13-year age range, there were a significant number of young athletes who presented to EDs with concussion as a result of playing organized sports. The 4- to 7-year age group had a disproportionately higher player-to–other object mechanism of injury.
Clinical Relevance:
Younger children are more susceptible to long-term sequelae from head injuries, and therefore, improved systems of monitoring for these athletes are required to monitor the patterns of injury, identify risk factors, and develop evidence-based prevention programs.
Keywords: concussion, epidemiology, NEISS, pediatrics, head injuries
Concussions are mild traumatic brain injuries that are generally self-limiting and are defined as a traumatically induced transient disturbance of brain function.3,8 It is believed that blows to the head that impart a linear and/or rotational force produce concussions.3,8 Experiments in rat models reveal that the brain has an increased susceptibility to a second injury until normal cellular homeostasis has returned.3,14,18 Furthermore, studies in animal models and humans reveal that second hits result in progressively more significant metabolic and cognitive dysfunction.3,14,15,18–21 In young rat models selected for interspecies age equivalence, it was found that during the recovery period, the brain functions at a reduced capacity and is less responsive to stimulation.14,18 Also, in these young rat models, metabolic and cognitive dysfunction can be potentiated, resulting in an extended recovery time if the brain is challenged with cognitive or physical exertion.14,18 Data from these studies are extrapolated to the immature brain of the developing human child, and it is surmised that youth athletes are more susceptible to functional and metabolic perturbations than are their adult counterparts. In these same youth rat models it was also found that recovery takes longer because of synaptic pathways being less developed, which when extrapolated to the developing human child would put the child at an increased risk for repeat/secondary injuries.3,14,18 Historically, very few investigations and monitoring of concussions have focused on competitive athletes prior to participation in high school sports. Therefore, valid comparisons with concussions in more mature athletes may not exist.
Concussions can occur in any sport but are more commonly seen in contact or collision sports such as football, hockey, rugby, soccer, and basketball.8,9 Calculated estimates of sports-related concussions range from 1.6 to 3.8 million per year,9 with the majority of concussions occurring in football players7,13 and as many as 50% going unreported.8 Football, basketball, and soccer were the sports with the greatest number of traumatic brain injuries (which includes but is not specific to concussions) for children between the ages of 5 and 18 years in the time span from 2001 to 2005, based on a study analyzing emergency room visits.4 During this period, it was estimated that there were 2.4 million sports- and recreation-related injuries evaluated in hospital emergency departments (EDs).4
Monitoring for head injuries has increased significantly at the professional and collegiate levels but to a lesser extent at the high school level.5,6,8,10,13,17 Forty-two states and the District of Columbia have passed guidelines for the diagnosis and treatment of concussion in sports.11 These guidelines range from coaches receiving additional training in the recognition of concussions to mandatory evaluation and clearance by a trained medical professional before the athlete can return to play after a concussion has been alleged.6,8,11
The objective of this study was to describe the epidemiology of youth concussions (aged 4-13 years) for 9 sports (basketball, baseball, football, gymnastics, hockey, lacrosse, soccer, softball, and wrestling) that presented to US EDs over an 11-year period from January 2002 to December 2012 using a nationally representative database.
Methods
National Electronic Injury Surveillance System
Data were collected from the National Electronic Injury Surveillance System (NEISS), a database maintained by the US Consumer Product Safety Commission (CPSC) that collects information on injuries that present to US EDs at a network of 100 hospitals. NEISS hospitals are a stratified probability sample of hospitals in the United States and its territories. The participating hospitals have at least 6 beds and a 24-hour ED where trained coders review all ED records daily and enter demographic, injury, and treatment information into the NEISS database. Each case is assigned 1 or 2 CPSC-specific product codes that designate what products or activities were involved at the time of injury.16 National estimates can then be calculated by summing the number of cases that present to each NEISS ED after using a multiplier based on the size of the hospital and the number of hospitals similarly sized across the United States.16
Utilization of NEISS
We selected the 9 sports that we believed had the greatest contact/risk for concussion during play. Then, one author (D.B.) queried the NEISS database for all basketball-, baseball-, football-, gymnastics-, hockey-, lacrosse-, soccer-, softball-, and wrestling-related head injuries (product codes 1205, 5041, 1211, 1272, 3272, 1215, 1267, 5034, and 1270, respectively, and body part location code 75, with a diagnosis of concussion) spanning from January 2002 to December 2012. The NEISS data set provides patient demographic information (age, race, and sex) on the injury sustained, diagnosis, disposition, location of injury occurrence (school, place of recreation, home, public property, street, or highway), and a brief narrative describing how the injury occurred. Narratives are a relatively new feature that was added to the NEISS database on January 1, 2002, but are highly variable as to their content and length. However, the narrative description of the activity being performed when the injury occurred was of particular interest. This included information on injury mechanisms (player-to-player, ball-to-head, player-to-ground, or player-to–other object), loss of consciousness (LOC), and concurrently sustained fractures.
Exclusion Criteria
Each case also had a locale for where the injury occurred (eg, home, ranch/farm, street or highway, other public property, mobile home, industrial place, school, place of recreation or sport, and not recorded). With the goal of targeting concussions that occurred during organized sports participation, we excluded from our data set any case that did not occur at school or a place of recreation/sport, or did not have a location of injury recorded. The narratives provided were also reviewed for each case and sport. All cases in which the narrative described situations other than organized competitive sports participation at the time of injury were excluded. Some examples of narrative phrases that resulted in exclusion were “play with [a sibling/family member],” “play at home,” “struck with bat at batting cage,” “playing catch,” “ran into coach,” “hit head on metal sewer grate,” “pool basketball,” “injured at daycare,” “playing with ball during gymnastics,” “hanging on soccer goal,” “goalpost fell onto player,” and “climbing soccer net.” Those cases in which the narratives described bystanders who were injured in the stands or individuals who were injured while helping at practice were excluded. Cases where the injury occurred from another event and the individual was only identified as an athlete involved in a given sport were excluded. The total number of cases excluded was 748 (13% of all cases), the majority of which were due to play at a locale other than one associated with organized play.
Data Analysis
Descriptive statistical analysis was performed using Microsoft Excel (Microsoft Corp, Redmond, Washington, USA) and SPSS statistics v22 (IBM Corp, Armonk, New York, USA). Subset analysis was performed on the athletes who sustained a fracture, those who required hospital admittance, and those whose ages ranged from 4 to 7 years. National estimates of youth concussions relating to 9 sports (basketball, baseball, football, gymnastics, hockey, lacrosse, soccer, softball, and wrestling), LOC, and in the 4- to 7-year age group were also calculated utilizing NEISS hospitals as a stratified national sampling.16 The Pearson correlation coefficient was obtained to quantify the correlation between individual sports and the overall frequencies of concussions with each successive year. An alpha of .05 and an r > 0.602 indicated statistical significance.
Results
The total number of cases was 4864 (national estimate [NE], 117,845). The distribution of male-to-female athletes over the 11-year span is provided in Table 1.
TABLE 1.
Entire Cohort by Sex (N = 4864)
| National Estimate | No. of Concussions | % of Cohort | Mean Age, y | Median Age, y | Pearson ra | |
|---|---|---|---|---|---|---|
| Youth athletes | 117,845 | 4864 | 100 | 11.1 | 12.0 | — |
| Male | 92,932 | 3905 | 80 | 11.1 | 12.0 | 1.00 |
| Female | 24,913 | 959 | 20 | 11.4 | 12.0 | 0.99 |
aPearson correlation coefficient of the subgroup compared with the entire cohort.
The prevalence of male concussions was the overwhelming majority over the entire 11-year time frame (Figure 1). Concussion frequencies trended up throughout the 11-year time frame with increasing age of the players (Figure 2). The number of concussions is broken down by race in Table 2.
Figure 1.
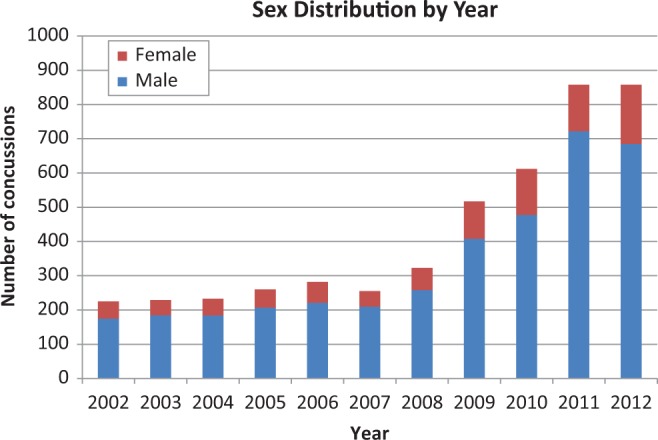
The number of concussion cases, per year, by sex, in youth athletes presenting to NEISS emergency departments over an 11-year time frame.
Figure 2.
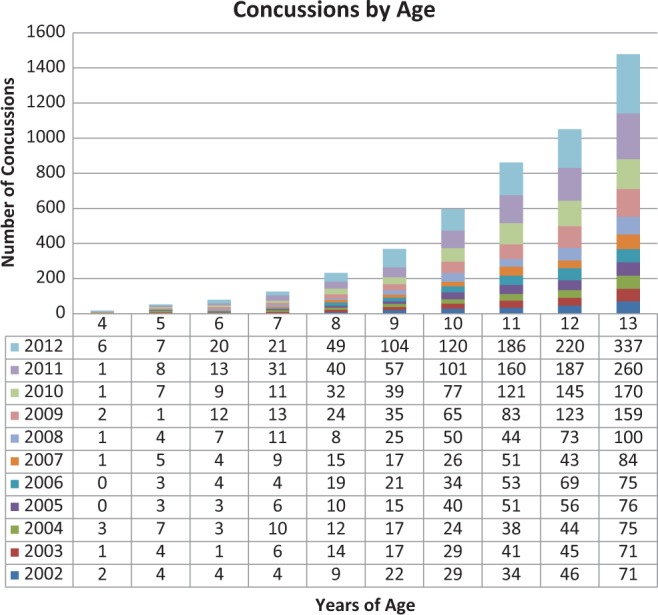
The number of concussions per year, and by age.
TABLE 2.
Entire Cohort by Race (N = 4864)
| Race | No. of Concussions | % of All Concussions | Pearson ra |
|---|---|---|---|
| White | 2339 | 48 | 1.00 |
| Black/African American | 630 | 13 | 1.00 |
| Other | 351 | 7 | 0.99 |
| Not stated | 1544 | 32 | 1.00 |
aPearson correlation coefficient of the subgroup compared with the entire cohort.
Racial distributions were consistent throughout the study period. “Other” was defined as American Indian/Alaskan Indian, Native Hawaiian/Pacific Islander, or any other race than the previously mentioned ones. The large majority (91%) of patients were treated as outpatients. Concussion breakdown by disposition is provided in Table 3.
TABLE 3.
Concussions by Treatment Disposition (N = 4864)
| Treatment | No. of Concussions | % of All Concussions |
|---|---|---|
| Outpatient treatment | 4444 | 91 |
| Admitted or transferred | 412 | 9 |
| Left against medical advice | 4 | <0.1 |
| No recorded disposition | 4 | <0.1 |
The majority (60%) of concussions occurred at a place of recreation or sports. Concussion breakdown by location of injury is found in Table 4.
TABLE 4.
Concussions by Place of Occurrence (N = 4864)
| Occurrence | No. of Concussions | % of All Concussions | Pearson ra |
|---|---|---|---|
| Place of recreation or sports | 2893 | 60 | 0.98 |
| School | 1185 | 24 | 0.85 |
| Not recorded | 786 | 16 | 0.90 |
aPearson correlation coefficient of the subgroup compared with the entire cohort.
In total, there were 499 concussions (NE, 12,128; 10%), in the entire cohort. The frequencies of players experiencing LOC had an overall upward trend (Figure 3).
Figure 3.
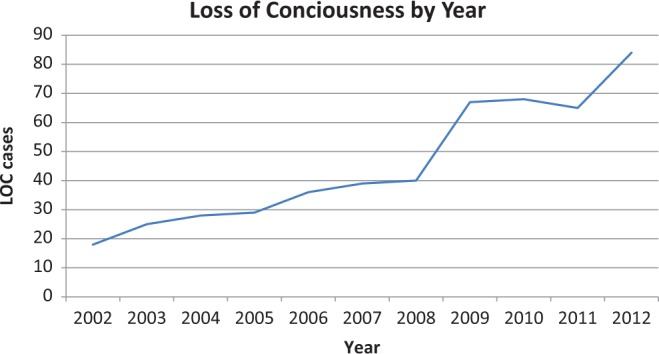
Concussion cases associated with a loss of consciousness (LOC) by year.
The mechanism of injury with the greatest number of concussions was player-to-player, with a total of 1943 (40%) concussions (Table 5, Figure 4).
TABLE 5.
Concussions by Mechanism of Injury (N = 4864)
| Mechanism of Injury | No. of Concussions | % of All Concussions | Mean Age, y | Median Age, y |
|---|---|---|---|---|
| Player-to-player | 1944 | 40 | 11.4 | 12 |
| Player-to-ground | 856 | 18 | 11 | 11 |
| Ball-to-head | 720 | 15 | 10.8 | 11 |
| Player-to–other object | 271 | 5 | 10.6 | 11 |
| Not specified | 1073 | 22 | 11.2 | 12 |
Figure 4.
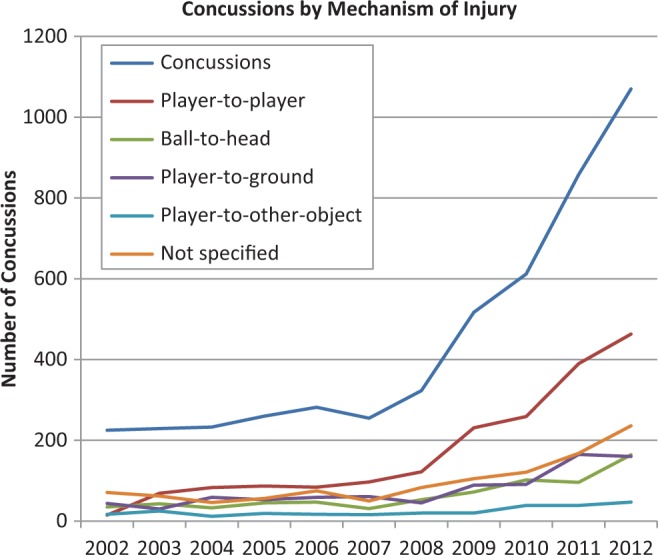
Number of concussions trended over the 11-year time frame by mechanism of injury.
The entire cohort contained a total of 34 fractures. The distribution of fractures by type is broken down in Table 6. Subgroup analysis of the players who sustained a concussion with a concurrent fracture demonstrated 4 severe injuries, defined as “no permanent functional disability but severe injury” by the National Catastrophic Injury project at the University of North Carolina,12 consisting of 2 skull fractures and 2 thoracic spine compression fractures. There was also a case associated with a subdural hematoma without a fracture.
TABLE 6.
Fractures by Type
| Type of Fracture | No. of Fractures | % of All Fractures |
|---|---|---|
| Facial bones | 22 | 65 |
| Clavicle | 3 | 9 |
| Skull | 2 | 6 |
| Distal radius | 2 | 6 |
| Thoracic spine | 2 | 6 |
| Forearm | 1 | 3 |
| Toe | 1 | 3 |
| Tibia/fibula | 1 | 3 |
| Total | 34 | 100 |
A subgroup for inpatient (admitted or transferred) athletes was created and then analyzed (Table 7). The mechanism of injury causing the greatest number of concussions was player-to-player (45%). Also, 83% of concussed youths in the inpatient subgroup were male (Table 8).
TABLE 7.
Concussions Grouped by Mechanism of Injury in the Inpatient Subgroup (n = 412)
| Mechanism of Injury | No. of Concussions | % of Inpatient Subgroup | Mean Age, y | Median Age, y |
|---|---|---|---|---|
| Player-to-player | 185 | 45 | 11.7 | 12 |
| Player-to-ground | 82 | 20 | 11.1 | 12 |
| Ball-to-head | 49 | 12 | 10.8 | 11 |
| Player-to–other object | 22 | 5 | 11.1 | 12 |
| Not specified | 74 | 18 | 11.3 | 12 |
TABLE 8.
Patient Sex and Loss of Consciousness Distribution in the Inpatient Subgroup (n = 412)
| No. of Concussions | % of Inpatient Subgroup | Mean Age, y | Median Age, y | |
|---|---|---|---|---|
| Loss of consciousness | 74 | 18 | 11.4 | 12 |
| Male | 61 | 83 | 11.4 | 12 |
| Female | 13 | 17 | 11.2 | 12 |
All concussion cases with associated fractures were then grouped together, and fracture frequency was grouped by mechanism of injury (Table 9).
TABLE 9.
Mechanism of Injury Distribution in the Fracture Subgroup
| Fracture Subgroup | No. of Fractures | % of Fractures | Mean Age, y | Median Age, y |
|---|---|---|---|---|
| Total fractures | 34 | 100 | 11.5 | 12 |
| Player-to-player | 16 | 47 | 11.4 | 12 |
| Player-to-ground | 1 | 3 | — | — |
| Ball-to-head | 8 | 24 | 11.6 | 12 |
| Player-to–other object | 4 | 12 | 10.3 | 10 |
| Not specified | 5 | 15 | 12.4 | 12 |
The number of concussions by sport is broken down in Table 10. The frequency of concussions had an overall upward trend for each sport over the 11-year time span. The frequency of concussions per sport, trended over the 11-year time frame, is illustrated in Figure 5.
TABLE 10.
Concussions by Sport
| Sport | National Estimate | No. of Concussions | % of All Concussions | Pearson ra | Increaseb |
|---|---|---|---|---|---|
| Football | 51,220 | 2013 | 41 | 1.00 | 6.1× |
| Basketball | 22,099 | 977 | 20 | 1.00 | 3.6× |
| Soccer | 18,916 | 801 | 17 | 1.00 | 5.6× |
| Baseball | 12,610 | 525 | 11 | 0.99 | 2.8× |
| Softball | 4005 | 146 | 3 | 0.98 | 2.8× |
| Wrestling | 2824 | 117 | 2 | 0.95 | 4.2× |
| Lacrosse | 1600 | 99 | 2 | 0.99 | 30× |
| Hockey | 1550 | 76 | 2 | 0.97 | 5.5× |
| Gymnastics | 1550 | 76 | 2 | 0.98 | 6.0× |
aPearson correlation coefficient comparing specified sport with the entire cohort.
bComparison in the number of concussions between years 2012 and 2002.
Figure 5.
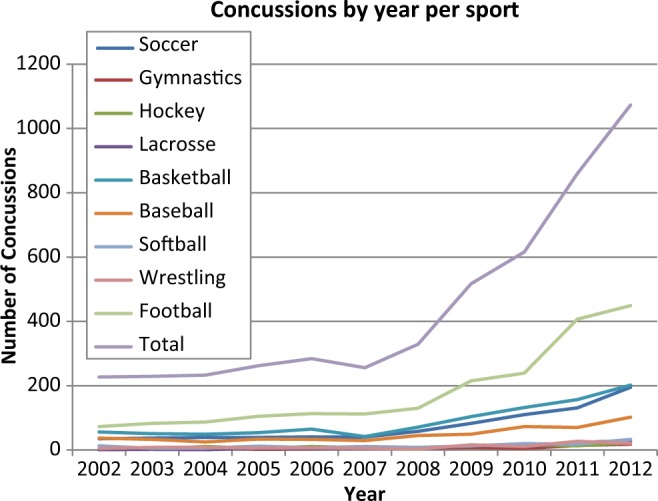
Eleven-year trend on the number of concussions by sport.
A similar study published by Bakhos et al2 had an age cutoff of 8 years; however, we analyzed a subgroup of individuals from ages 4 to 7 years, which, to our knowledge, has never been reported on in the literature. The number of concussions in the 4- to 7-year-old subgroup was 277 (NE, 6769; 6%). In this same subgroup, 19 (7%) required inpatient treatment (Table 11). This subgroup was added so that any differences between younger and older youth athletes could be addressed in the development of future studies that focus more on this younger population.
TABLE 11.
Patient Sex and Inpatient Distribution in the 4- to 7-Year Age Group (n = 277)
| No. of Concussions | % Concussions in Subgroup | Mean Age, y | Median Age, y | |
|---|---|---|---|---|
| Male | 228 | 82 | 6.2 | 6 |
| Female | 49 | 18 | 5.8 | 6 |
| Inpatient treatment | 19 | 7 | 6.2 | 7 |
The player-to-player mechanism of injury was also the highest in this subgroup (n = 71, 26%). The number of concussions by mechanism of injury in this subgroup is given in Table 12.
TABLE 12.
Mechanism of Injury in the 4- to 7-Year Subgroup
| Mechanism of Injury | No. of Concussions | % of Concussions in Subgroup | Mean Age, y | Median Age, y |
|---|---|---|---|---|
| Player-to-player | 71 | 26 | 6.4 | 7 |
| Player-to-ground | 62 | 22 | 6.1 | 6 |
| Ball-to-head | 55 | 20 | 6.1 | 6 |
| Player-to–other object | 36 | 13 | 5.7 | 6 |
| Not specified | 53 | 19 | 6.1 | 7 |
Discussion
Our data report that football, basketball, and soccer are associated with the greatest number of concussions in decreasing order. Our data are consistent with previous studies that identify football as the sport associated with the greatest number of concussions.2,5,10 However, our data indicate basketball and soccer as the second and third highest sports associated with the greatest number of concussions, which is in contrast to the study by Lincoln et al,10 which found that lacrosse is second to football and soccer comes in third when males and females are grouped together. Lincoln et al10 conducted an epidemiologic study analyzing concussion frequencies in high school sports. They prospectively gathered data for 25 schools in a large public school system and reported 2651 concussions over an 11-year period. One factor that may contribute to the difference between that study and the present one is a potential difference in the popularity of sports between age groups. Another potential explanation for this difference between our study and that by Lincoln et al10 is the differences in the popularity of specific sports by geographic location.1 The sequence of concussion prevalence by sports in our study matches that published by the Centers for Disease Control and Prevention4 in decreasing order: football, basketball, and soccer.
All sports were found to have a high correlation of concussion frequencies when compared with the entire group over the 11-year time span. The sports with the highest correlation to the total number of concussions included football (r = 1.00), basketball (r = 1.00), and soccer (r = 1.00). The sport with the lowest correlation was wrestling (r = 0.95). Lacrosse had a 30-fold increase in the number of concussion cases. This may be attributed to an increasing popularity of the sport, as there was only 1 concussion associated with the sport in 2002, and/or to an increased awareness of concussions associated with the sport.
The increase in concussion frequencies by age may be because of an increasing number of participants as well as a more aggressive play by maturing athletes (see Figure 2). The number of concussions increased throughout the entire 11-year time frame except from 2006 to 2007, in which there was a drop from 282 to 255 (see Figure 1). This decrease in concussions for the year 2007 is most likely due to a real drop in concussions for the year, as it is unlikely that awareness about concussions would decrease for that specific year. Furthermore, the proportion of males to females appeared to stay consistent (see Figure 1), and we do not believe that differences in sex played a significant role in the observed trends. The increasing trend in the number of concussions for each age group with successive years may be because of an increased awareness by the involved parties (parents/athletes/coaches) and therefore may explain the increasing trend with the progression in time.
The frequency of LOC associated with concussion increased each year throughout the 11-year time frame except for 2011, which dropped to 8% from 11% in 2010 (see Figure 3). As the sample size for LOC is small, a possible explanation for the observed difference may be random chance. The frequency of LOC was strongly correlated (r = 0.98) with the frequency of concussions over the same period. However, the frequency of LOC increased by 68% from 2008 to 2009 and by 29% from 2011 to 2012. This trend was reflected in the frequency of total number of concussions, which increased by 60% from 2008 to 2009 and by 25% from 2011 to 2012. The increase in the prevalence of LOC closely correlated with the increase in the number of concussions, and therefore, a plausible explanation may be an increased awareness and therefore reporting of concussion cases. An increased awareness is a better explanation for the increased LOC than a more aggressive style of play, as one would expect a disproportionate increase in the prevalence of LOC when compared with the prevalence of concussions if a more aggressive style of play was the case.
We found that fractures occurred in older children (mean age, 11.5 years) and closely coincided with our overall data set mean age of 11.1 years. Within the fracture subgroup, LOC occurred in 29% of patients, which is almost triple that of the overall frequency of 10% in the overall cohort. The majority (71%) of these fractures involved the head, demonstrating additional injuries to the head other than concussion. These data suggest that older children may be at greater risk for sustaining a fracture because of more aggressive play by the maturing athlete as well as increased forces associated with increasing body weight of the involved athletes.
We found that fewer hospital admissions (7%) were observed in the 4- to 7-year-old subgroup versus the overall group (9%). The proportion of males (82%) versus females (18%) in this subgroup is equivocal to the entire group of (80% male, 20% female). The decreased frequency of fractures with decreasing age may be explained by the fact that younger bones have greater plasticity and therefore may be less likely to fracture. Furthermore, this group consisted of lighter subjects, and it is hypothesized that there was reduced force transmission during collisions. The younger group may also be associated with an overall less aggressive style of play.
The ball-to-head mechanism of injury increased from 15% in the overall cohort to 20% in the 4- to 7-year-old subgroup. The player-to–other object mechanism of injury more than doubled from 6% in the overall cohort to 13% in the younger subgroup, suggesting that the origins of concussions in this subgroup are drastically different from the older children. Consequently, this population would most likely require a different approach to interventions targeted at reducing the number of concussions. The mechanism-of-injury data suggests that interventions focusing on altering the environment, with the goal of removing objects or obstacles from or around the field of play, would have an increasing disproportionate benefit to this subgroup. The addition of protective head gear may also be of greater benefit for the 4- to 7-year-old subgroup, which would target the ball-to-head mechanism of injury.
Out of the entire cohort, 9% required hospital admission or transfer after presentation to the ED, suggesting a more serious injury. Of the concussions in the admitted subgroup, 18% were associated with LOC, which is almost double the overall group frequency of LOC (10%), further implying a more serious injury. Otherwise, the other mechanisms of injury in this subgroup remained similar to the overall data.
The NEISS data set provides valuable epidemiological information on concussion frequencies in youth athletics over a variety of sports. However, the heterogeneity of the narrative descriptions of the mechanism/situation around which the injury occurred leaves noteworthy gaps in the data set and therefore may be a source of information bias. This potential bias is an inherent weakness of the database and is out of our control. The creation of a national database, with standardized narrative input, focused on head injuries associated with all levels of organized sports from youth leagues to the professional levels would be an invaluable tool in identifying risk factors associated with specific sports by age groups. A standardized national database may also provide a method for monitoring the effects of the implementation of new safety measures, such as innovative protective equipment (eg, helmets, braces, mouth guards, pads, flooring, etc), rule changes, and education programs focusing on proper technique and injury prevention.
Another potential source of bias would be an uneven geographic sampling of emergency rooms throughout the nation. The ED sampling is supposedly a national representation of all EDs in the country. As such, one assumption of this study is that clustering of departments in the sample is controlled. Another potential source of bias may occur in the method used to exclude cases. Excluding some of the accidental injuries outside the exact sport (eg, “goalpost fell onto player”) may have introduced a measurement bias. The highly variable narrative is illustrated in the example above, such that the reviewer cannot know the circumstances involving the injury (eg, whether it was related to horseplay, during competitive play, or as an incidental occurrence in a nonathlete). We did not assume that these ambiguous cases were associated with competitive play, and therefore, our results may be an underestimate. However, these cases were within a small minority, and bias is believed to be minimal.
Another potential source of bias in this study stems from the nature of reporting of concussions using the NEISS database. This study only takes into account the athletes with concussions who presented to the ED. It might be the case that these athletes are a minority of the total number of youth athletes suffering from concussion. Furthermore, the same group of athletes who presented to the ED may have experienced more severe concussions (eg, higher incidence of fractures, LOC, spine injury, etc). These biases may provide an underestimate and a greater severity of concussions than is actually the case. Future studies may be able to address this if a national database is used in which all concussion cases are reported at the time and location of occurrence (eg, on the playing field) such that the level of severity (eg, vomiting, LOC, and deteriorating symptoms) may be recorded and subsequently analyzed.
Despite these limitations, the NEISS data set is the only nationally representative stratified probability sample of concussions occurring in youth athletics in the United States. It is the only system that allows querying of concussions occurring in athletes prior to participation in high school sports. Additionally, the stability of the NEISS database allows monitoring for changes over time by overall concussion prevalence or by specific sport. This study provides valuable information about risk of injury among youth athletes participating in pre–high school athletics.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. 2012-13 High School Athletics Participation Survey. Indianapolis, IN: National Federation of State High School Associations; 2013. [Google Scholar]
- 2. Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–e556. [DOI] [PubMed] [Google Scholar]
- 3. Barkhoudarian G, Hovda DA, Giza CC. The molecular pathophysiology of concussive brain injury. Clin Sports Med. 2011;30:33–48. [DOI] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries from sports and recreation activities—United States, 2001-2005. MMWR Morb Mortal Wkly Rep. 2007;59:733–737. [PubMed] [Google Scholar]
- 5. Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42:495–503. [PMC free article] [PubMed] [Google Scholar]
- 6. Guskiewicz KM, Bruce SL, Cantu RC, et al. National Athletic Trainers’ Association position statement: management of sport-related concussion. J Athl Train. 2004;39:280–297. [PMC free article] [PubMed] [Google Scholar]
- 7. Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. [DOI] [PubMed] [Google Scholar]
- 8. Harmon KG, Drezner JA, Gammons MA, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47:15–26. [DOI] [PubMed] [Google Scholar]
- 9. Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21:375–378. [DOI] [PubMed] [Google Scholar]
- 10. Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011;39:958–963. [DOI] [PubMed] [Google Scholar]
- 11. Lowrey KM. Summary Matrix of State Laws Addressing Concussions in Youth Sports 2012. St Paul, MN: The Network for Public Health Law; 2012. [Google Scholar]
- 12. Mueller FO, Cantu RC. Catastrophic Sports Injury Research, 28th Annual Report. Chapel Hill, NC: University of North Carolina; 2010. [Google Scholar]
- 13. Powell JW, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282:958–963. [DOI] [PubMed] [Google Scholar]
- 14. Prins ML, Hales A, Reger M, Giza CC, Hovda DA. Repeat traumatic brain injury in the juvenile rat is associated with increased axonal injury and cognitive impairments. Dev Neurosci. 2010;32:510–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Putukian M. Repeat mild traumatic brain injury: how to adjust return to play guidelines. Curr Sports Med Rep. 2006;5:15–22. [DOI] [PubMed] [Google Scholar]
- 16. Schroeder R, Ault K. The NEISS Sample (Design and Implementation) 1997 to Present. Washington, DC: Division of Hazard and Injury Data Systems, US Consumer Product Safety Commission; 2001. http://www.cpsc.gov/PageFiles/106617/2001d011-6b6.pdf. Accessed March 8, 2014. [Google Scholar]
- 17. Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160:937–944. [DOI] [PubMed] [Google Scholar]
- 18. Shrey DW, Griesbach GS, Giza CC. The pathophysiology of concussions in youth. Phys Med Rehabil Clin N Am. 2011;22:577–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tavazzi B, Vagnozzi R, Signoretti S, et al. Temporal window of metabolic brain vulnerability to concussions: oxidative and nitrosative stresses—part II. Neurosurgery. 2007;61:390–395. [DOI] [PubMed] [Google Scholar]
- 20. Vagnozzi R, Signoretti S, Tavazzi B. Temporal window of metabolic brain vulnerability to concussion: a pilot 1H-magnetic resonance spectroscopic study in concussed athletes—part III. Neurosurgery. 2008;62:1286–1295. [DOI] [PubMed] [Google Scholar]
- 21. Vagnozzi R, Tavazzi B, Signoretti S, et al. Temporal window of metabolic brain vulnerability to concussions: mitochondrial-related impairment—part I. Neurosurgery. 2007;61:379–388. [DOI] [PubMed] [Google Scholar]


