Abstract
Background:
Large glenoid rim defects in patients with traumatic anterior shoulder instability are often regarded as a contraindication for arthroscopic Bankart repair, with a defect of 20% to 27% considered as the critical size. While recurrence of dislocations, male sex, and collision sports were reported to be the significant factors influencing large glenoid defects, the influences of subluxations and more detailed types of sports were not investigated.
Purpose:
To investigate the influence of the number of dislocations and subluxations and type of sport on the occurrence and size of glenoid defects in detail.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A total of 223 shoulders (60 with primary instability, 163 with recurrent instability) were prospectively examined by computed tomography. Glenoid rim morphology was compared between primary and recurrent instability. In patients with recurrent instability, the relationship between the glenoid defect and the number of dislocations and subluxations was investigated. In addition, glenoid defects were compared among 49 male American football players, 41 male rugby players, 27 male baseball players, and 25 female athletes.
Results:
The mean extent of the glenoid defect was 3.5% in shoulders with primary instability and 11.3% in those with recurrent instability. A glenoid defect was detected in 108 shoulders (66.2%) with recurrent instability versus 12 shoulders (20%) with primary instability. Regarding the influence of the total number of dislocations/subluxations, the average extent of the glenoid defect was 6.3% in 85 shoulders with 2 to 5 events, 12.9% in 34 shoulders with 6 to 10 events, and 19.6% in 44 shoulders with 11 or more events. The glenoid defect became significantly larger along with an increasing number of recurrences. Although recurrent subluxation without dislocation also influenced the glenoid defect size, the number of dislocations did not. The average extent of the glenoid defect was 12.0% in rugby players, 8.9% in American football players, 4.7% in female athletes, and 4.5% in baseball players. Glenoid defects were significantly smaller in male baseball players and female athletes than in male collision athletes.
Conclusion:
The glenoid defect is significantly enlarged by damage due to recurrent dislocation and subluxation; therefore, glenoid rim morphology differs markedly between primary and recurrent instability. Glenoid defect size is also influenced by sex and by the type of sport.
Keywords: traumatic anterior shoulder instability, 3-dimensional reconstructed computed tomography, inverted pear glenoid, glenoid defect
A glenoid rim with a large bony defect in patients with traumatic anterior shoulder instability is referred to as an inverted pear glenoid. Burkhart and de Beer3 reported that patients with significant bony defects, such as those with an inverted pear glenoid or an engaging Hill-Sachs lesion, are not candidates for arthroscopic Bankart repair. In previous reports, glenoid defects larger than 20% to 27% were regarded as exceeding the critical size for arthroscopic surgical repair.6,11,18 Several methods of bone grafting for large glenoid defects have been discussed recently, including the arthroscopic Latarjet procedure, the Bristow procedure, and free iliac crest bone grafting.1,9,17 However, the timing and mechanism of such large glenoid defects are still controversial.
Regarding arthroscopic Bankart repair of an inverted pear glenoid, Sugaya et al16 reported that arthroscopic repair of bony Bankart lesions with suture anchors is successful even for patients with a chronic glenoid defect because most of the bone fragments are preserved. In contrast, Boileau et al2 and Mologne et al13 reported that the risk of postoperative recurrence was significantly increased in patients with a large glenoid defect who had no bone fragments.
In a previous study,14 we investigated the correlation between the time elapsed after the primary traumatic episode and the size of the glenoid defect and associated bone fragments of bony Bankart lesions in patients with traumatic anterior shoulder instability. We reported that the glenoid defect size showed no relationship with the time after trauma but the bone fragments displayed a marked decrease in size relative to the glenoid defect within 1 year after the primary event.14 We concluded that most bone fragments showed extensive absorption within 1 year after the primary traumatic episode and that the interval since the primary trauma was significantly correlated with the extent of absorption.14 However, the possibility that the bone fragment seemed to be too small because the glenoid defect itself had been enlarged by damage due to recurrent dislocation and subluxation could not be excluded. Accordingly, the first purpose of this study was to investigate the influence of recurrent dislocation/subluxation on the occurrence and size of glenoid defects.
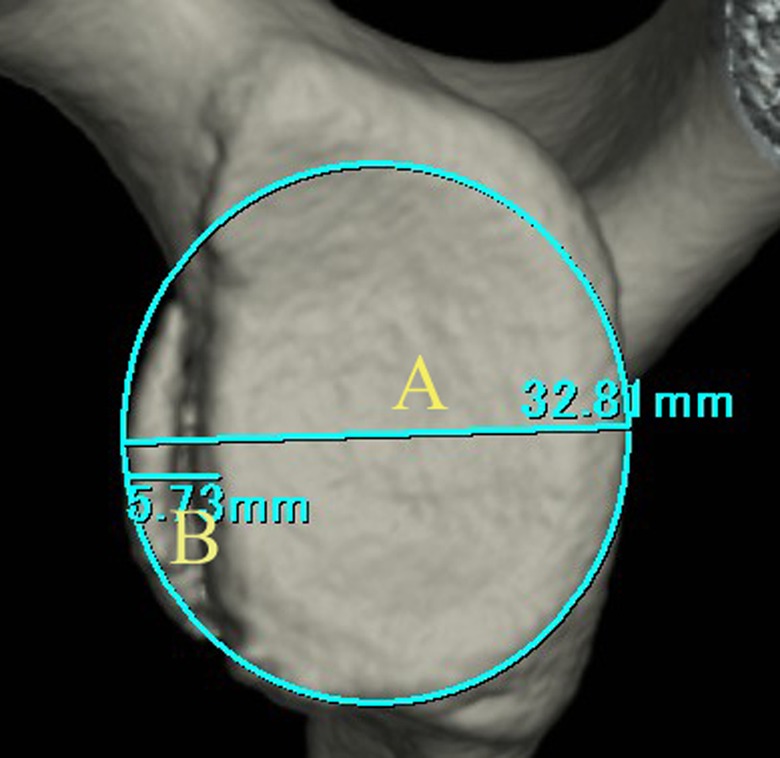
Large glenoid defects are frequently recognized in male athletes playing collision sports (Figure 1), while recurrent shoulder instability also occurs in overhead athletes. However, there have been few detailed investigations into the influence of the type of sport on glenoid defects. We hypothesized that the glenoid defects of male athletes would be larger than those of female athletes irrespective of the type of sport. Therefore, we investigated the influence of sex and type of sport on the size of glenoid defects by comparison of glenoid defects among male baseball players, male collision sports players, and female athletes.
Figure 1.

A large glenoid defect in a male collision athlete. An 18-year-old male rugby player at 1 year after primary trauma with 60 events of subluxation (glenoid defect, 26.5%).
Regarding the risk factors for glenoid defects, Milano et al12 concluded that the number of dislocations and age at first dislocation were the most significant predictors. In their reports, while recurrence of dislocations, increasing number of dislocations, male sex, and type of sport were significantly associated with the presence of the glenoid defects, the influence of subluxations and more detailed types of sports were not investigated. Griffith et al5 also investigated glenoid bone loss using computed tomography (CT) and reported that the number of dislocations correlated moderately with the severity of glenoid bone loss. While they concluded that one cannot accurately predict severity of glenoid bone loss on the basis of the number of dislocations alone, the fact that they investigated solely obvious dislocation and did not investigate subluxation events might influence moderate correlation. Thus, this study was performed to investigate factors influencing the occurrence and size of glenoid defects associated with traumatic anterior shoulder instability in detail.
Materials and Methods
The subjects were 205 patients (223 shoulders) with traumatic anterior instability, in whom glenoid rim morphology was prospectively evaluated by CT scanning at our hospital between 2007 and 2011. There were 60 patients (60 shoulders) with primary instability and 145 patients (163 shoulders) with recurrent instability. All patients had a history of an obvious traumatic episode, and patients with atraumatic instability were excluded. While major trauma was defined as high-impact injury, such as hard contact with another person during tackling, blocking, and so on, minor trauma included outstretching of the arm as in sliding for a base, making a diving catch, scrambling for a ball, and so on. An episode of major trauma was the primary event in 86 shoulders, and of minor trauma was that in 137 shoulders. Patients with recurrent instability after previous anterior stabilization (primary surgery at our hospital, 4 shoulders; at other hospitals, 6 shoulders), multidirectional instability (2 shoulders), epilepsy (3 shoulders), rotator cuff tears without a Bankart lesion (7 shoulders), and insufficient data, including no CT scans (7 shoulders), were also excluded from this study. Institutional review board approval was obtained before recruitment for the study commenced, and all subjects gave informed consent prior to participating. The patient profile is shown in Table 1. The mean age at primary trauma and at CT scanning was significantly older in the patients with primary instability than in the patients with recurrent instability (primary trauma, P < .001; CT scanning, P = .009), while other patient factors were similar for the 2 groups.
TABLE 1.
Patient Profile With Primary Instability and Recurrent Instability
| Primary Instability (n = 60 Shoulders) | Recurrent Instability (n = 163 Shoulders) | |
|---|---|---|
| Patient age, y, mean (range) | ||
| At primary trauma | 24.8 (13-71) | 18.4 (12-42) |
| At computed tomography | 24.8 (13-71) | 21.5 (14-55) |
| Sexa | ||
| Male | 48 | 144 |
| Female | 12 | 19 |
| No. of athletes | 52 | 148 |
| Type of sporta | ||
| Collision | 26 | 95 |
| Contact | 8 | 20 |
| Overhead | 12 | 24 |
| Other | 6 | 9 |
| Level of sporta | ||
| Competitive | 45 | 104 |
| Recreational | 7 | 44 |
| Main symptoma | ||
| Sense of instability | 53 | 151 |
| Residual pain | 7 | 12 |
aValues for sex, type of sport, level of sport, and main symptom are given as number of shoulders.
Computed tomography scanning was usually done at the first visit to our hospital. To quantify the glenoid defect, the inferior portion of the glenoid rim was approximated to a true circle on en face 3-dimensional CT scans reconstructed with elimination of the humeral head. CT scanning and image reconstruction were performed with a Toshiba whole-body x-ray CT scanner Aquilion 64 (spiral scan, 0.5-mm slice thickness, 0.3-mm reconstruction, 3-dimensional edit mode; Toshiba Medical Systems, Tochigi, Japan). Using a digital imaging and communications in medicine (DICOM) picture archiving and communication system (PACS) (Mitsubishi Heavy Industries Mechatronics Systems, Kobe, Japan), the extent of the glenoid defect was calculated as a percentage of the glenoid rim by the equation B/A × 100%, where A is the diameter of the fitted circle and B is the width of the defect (Figure 2).14,15
Figure 2.
Quantification methods for glenoid defects. On en face 3-dimensional computed tomography scans reconstructed with elimination of the humeral head, the inferior portion of the glenoid rim was approximated to a true circle. The extent of the glenoid defect was calculated as a percentage of the glenoid rim by the equation B/A × 100%, where A is the diameter of the fitted circle and B is the width of the defect.
First, glenoid rim morphology was compared between primary instability and recurrent instability. In patients with recurrent instability, the relationship between the extent of the glenoid defect and the total number of dislocations plus subluxations (the total number) was investigated, as was the number of dislocations, the number of subluxations in patients without dislocation, and the total number in patients with <1 year after primary trauma. Regarding the influence of the total number and the number of dislocations, the frequency of a large glenoid defect (>20%) and the correlation between these numbers and the extent of the glenoid defect were also investigated. In the present study, dislocation was defined as a complete instability event that required manual reduction by a health care provider, while subluxation was defined as an incomplete instability event that did not require a health care provider. So, an instability event in which a patient complained of spontaneous relocation or self-reduction was regarded as a subluxation event.
Finally, the extent of the glenoid defect was compared among 49 male American football players, 41 male rugby players, 27 male baseball players, and 25 female athletes (collision sports, n = 5; contact sports, n = 7; overhead sports, n = 9; other sports, n = 4) selected from a total of 223 patients, including those with primary instability. The profiles for each group of athletes were not significantly different with regard to the age at primary trauma, age at CT scanning, interval between primary trauma and CT scanning, total number of events (dislocations and subluxations), and number of dislocation (Table 2). However, the rate of primary instability—5% for rugby players, 27% for American football players, 22% for baseball players, and 36% for female athletes—was significantly lower in rugby players than in the other groups (P = .033). Moreover, an episode of major trauma was the primary event in 78% of rugby players, 63% of American football players, 7% of baseball players, and 8% of female athletes, with the rates for rugby players and American football players significantly higher than those in the other groups (P < .001).
TABLE 2.
Patient Profile in Male Collision Sports, Baseball Players, and Female Athletes
| American Football (n = 49 Patients) | Rugby (n = 41 Patients) | Baseball (n = 27 Patients) | Female (n = 25 Patients) | |
|---|---|---|---|---|
| Patient age, y, mean (range) | ||||
| At primary trauma | 18.6 (15-28) | 17.6 (14-26) | 20.6 (13-50) | 17.8 (12-34) |
| At computed tomography | 19.5 (15-35) | 18.8 (14-30) | 22.0 (16-50) | 19.4 (14-34) |
| Time primary trauma to computed tomography, y (range) | 1.0 (0-13) | 1.3 (0-10) | 1.3 (0-5) | 1.6 (0-5) |
| Instability, No. of patients | ||||
| Primary | 13 | 2 | 6 | 9 |
| Recurrent | 36 | 39 | 21 | 16 |
| Trauma, No. of patients | ||||
| Major | 31 | 32 | 2 | 2 |
| Minor | 18 | 9 | 25 | 23 |
| Total number (dislocations and subluxations) | ||||
| Events, mean | 9.2 | 6.8 | 4.9 | 6 |
| ≥6 events, No. of patients | 15 | 16 | 4 | 10 |
| Number of dislocations | ||||
| Events, mean | 1.4 | 1.5 | 1.1 | 1.5 |
| ≥2 events, No. of patients | 5 | 13 | 6 | 3 |
Statistical analysis was completed using the chi-square test and 1-factor analysis of variance, and statistical significance was accepted at P < .05. Correlations were examined by using Pearson correlation analysis.
Results
The mean extent of the glenoid defect was 3.5% in patients with primary instability and 11.3% in those with recurrent instability, showing a significant difference between these 2 groups (P < .001). A glenoid defect was found in 108 shoulders (66.2%) with recurrent instability versus 12 shoulders (20%) with primary instability, while a large glenoid defect (>20%) was present in 33 shoulders (20.2%) with recurrent instability versus only 3 shoulders (5%) with primary instability. Both a glenoid defect and a large glenoid defect were significantly more frequent in shoulders with recurrent instability (glenoid defect, P < .001; large glenoid defect, P = .006).
Regarding the influence of the total number of dislocation/subluxation events, the average extent of the glenoid defect was 6.3% in 85 shoulders with 2 to 5 events, 12.9% in 34 shoulders with 6 to 10 events, and 19.6% in 44 shoulders with 11 or more events. The defect became significantly larger with an increase in the total number of events (P < .001) (Figure 3). A large glenoid defect (>20%) was found in 6 shoulders (7.1%) with 2 to 5 events, 8 shoulders (23.5%) with 6 to 10 events, and 19 shoulders (43.2%) with 11 or more events, and the frequency of such defects also differed significantly among the 3 groups (P < .001). With a correlation coefficient of 0.4523, there was a modest correlation between them.
Figure 3.
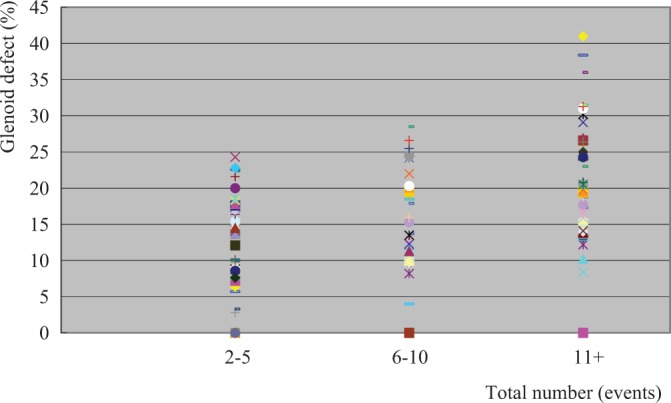
Glenoid defect versus the total number of dislocations and subluxations.
Regarding the influence of the number of dislocations, the average extent of the glenoid defect was 11.8% in 76 shoulders without dislocation, 10.0% in 24 shoulders with 1 dislocation, 7.9% in 19 shoulders with 2 dislocations, and 12.4% in 44 shoulders with dislocation 3 times or more, showing no statistically significant difference among the 4 groups. A large glenoid defect (>20%) was found in 17 shoulders (22.4%) without dislocation, 4 shoulders (16.7%) with 1 dislocation, 2 shoulders (10.5%) with 2 dislocations, and 10 shoulders (22.7%) with dislocation 3 times or more, and there was also no significant difference among the 4 groups. The correlation coefficient was 0.206, indicating a very weak correlation.
The influence of the number of subluxation episodes without dislocation was assessed in 76 shoulders, and the average extent of the glenoid defect was found to be 6.7% in 40 shoulders with 2 to 5 episodes of subluxation, 13.4% in 18 shoulders with 6 to 10 episodes, and 21.6% in 18 shoulders with 11 or more episodes. The glenoid defect became significantly larger because of an increasing number of subluxations without dislocation (P < .001).
Moreover, the influence of the total number of episodes was assessed in 49 shoulders with <1 year after primary trauma was assessed in 49 shoulders, revealing that the average extent of the glenoid defect was 6.3% in 38 shoulders with 2 to 5 episodes, 14.8% in 8 shoulders with 6 to 10 episodes, and 22.4% in 3 shoulders with 11 or more episodes. Thus, the defect was shown to become significantly larger with repetition of dislocation/subluxation even in a relatively short period after primary trauma (P = .001).
Regarding the influence of sex and the type of sport, the average extent of the glenoid defect was 12.0% in male rugby players, 8.9% in male American football players, 4.7% in female athletes, and 4.5% in male baseball players (Figure 4). In rugby players and American football players, the defect was significantly larger than in female athletes and baseball players (P = .002), while baseball players were similar to female athletes. The frequency of a large glenoid defect (>20%) was 22% (n = 9 shoulders) in rugby players, 16% (n = 8 shoulders) in American football players, 7% (n= 2 shoulders) in baseball players, and 4% (n = 1 shoulder) in female athletes. Although more frequent in collision athletes, there was no significant difference. On the other hand, there was no glenoid defect in 70% (n = 19 shoulders) of baseball players, 68% (n = 17 shoulders) of female athletes, 45% (n = 27 shoulders) of American football players, and 27% (n = 11 shoulders) of rugby players. The frequency of no glenoid defect was significantly higher in baseball players and female athletes than in American football and rugby players. Among female athletes, as the average extent of the glenoid defect was 6.8% in collision sports, 2.2% in contact sports, 5.0% in overhead sports, and 6.2% in the other sports, there were no statistically differences regarding the type of sport.
Figure 4.
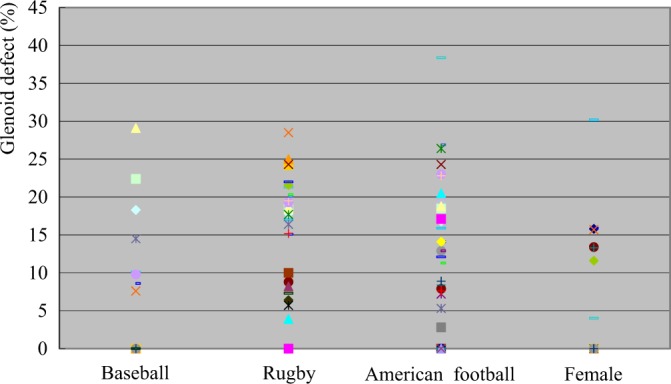
Glenoid defect versus sex and type of sport.
Discussion
This study showed that the frequency of glenoid defects was significantly higher and the defects were larger in shoulders with recurrent instability than in shoulders with primary instability; glenoid rim morphology was markedly different between these 2 groups. In addition, the glenoid defect was significantly enlarged by damage due to recurrent dislocation and subluxation or by recurrent subluxation without dislocation, and this was noted even at <1 year after primary trauma. Furthermore, the glenoid defect was significantly different in size between male baseball players and collision sports athletes, while the size of the glenoid defect was similar between male baseball players and female athletes. While Milano et al12 and Griffith et al5 have already reported on the same topic, we have shown in the present study that not only the number of dislocations but also the number of subluxations significantly enlarged the glenoid defects. Moreover, regarding the type of sport, the detailed character of each sport among male athletes could be shown.
We reported in a previous study14 that in shoulders with glenoid defects, reported that the bone fragments of bony Bankart lesions were smaller than the defects, suggesting that resorption of the bone fragment occurs in all shoulders with recurrent instability. We also reported that bone fragment resorption became more severe with an increasing frequency as the interval since primary trauma increased. In the present study, the glenoid defect was shown to be enlarged significantly by recurrence of dislocation/subluxation. Accordingly, bone fragments might be mistakenly judged to be small and partly resorbed because of enlargement of the glenoid defect itself. To determine which theory is correct, primary trauma patients with bone fragments would need to be observed over time. However, there is no doubt that the size mismatch between glenoid defect and bone fragment becomes more marked as the number of dislocations and subluxations increases and the period after primary trauma becomes longer.
In our prior study,14 we also investigated the influence of glenoid defect size, the presence of bone fragments, and postoperative union of bone fragments in relation to postoperative recurrence of instability after arthroscopic Bankart repair. The recurrence rate was 0% in shoulders without a glenoid defect while it was 17.5% in shoulders with a glenoid defect, showing a statistically significant difference. Moreover, among shoulders with a glenoid defect, the recurrence rate was 38.5% for those without a bone fragment, 50% for shoulders without bone union, and 8.3% for shoulders with bone union. Though there was no difference with regard to the presence/absence of a bone fragment, there was a significant difference between union and nonunion of the bone fragment (rate of union, 80%). We concluded that if the patient had a sufficiently large bone fragment, the short-term clinical outcome was good after achieving bone union. Jiang et al7 recently reported that arthroscopic reduction and fixation of a bony Bankart lesion can achieve good results, but the size of the reconstructed glenoid is crucial to the success of this surgery. The size of the reconstructed glenoid was <80% in 3 of 4 cases that failed while it was >80% in all successful cases. While the nonunion rate was 13.5%, the planned glenoid size (sum of the preoperative residual surface area of the glenoid and the surface area of the bone fragment) and the actual postoperative reconstructed glenoid size showed no statistical differences in the patients with bone union. They concluded that a large glenoid defect may not be reconstructed adequately even with anatomical reduction and good healing of a small bone chip. Kitayama et al8 investigated the long-term outcome and glenoid morphology after arthroscopic osseous Bankart repair for shoulders with glenoid bone loss of >15% and 5 to 8 years of follow-up. Recurrence occurred before bone union was achieved in 1 of 32 patients, but a successful outcome without recurrence was obtained in the others after bone union. The mean postoperative glenoid bone loss improved from 20.5% to –2.3%, and glenoid morphology was normalized postoperatively in all patients. They did not mention the precise size of the bone fragments so there may have been a few cases with small fragments. These 3 reports suggest the importance of early repair of a bony Bankart lesion prior to an increase of the size mismatch between the glenoid defect and bone fragment as well as the importance of reconstructing the glenoid at an appropriate size after bone union.
In the present study, we concluded that the glenoid defect was enlarged by further damage due to recurrent dislocation/subluxation. Compared with primary instability, the frequency of glenoid defects and large glenoid defects was significantly higher in recurrent instability, and the actual glenoid defects were also larger. Glenoid rim morphology was obviously different between the cases of recurrent instability and primary instability, so the possibility that shoulders with large glenoid defects due to primary trauma are more likely to develop recurrent instability was not excluded. Larrain et al10 reported a favorable outcome of arthroscopic Bankart repair in 204 male rugby players. However, they excluded large glenoid defects (>25%) from the indications for arthroscopic surgery as well as humeral avulsion of the glenohumeral ligament and large HS lesions. In their report, a large glenoid defect (>25%) was not recognized among 40 cases of primary instability but was found in 25 of 158 patients (15.8%) with recurrent instability, so open Bankart repair was performed. While their findings were compatible with our results, to confirm our hypothesis about enlargement of the glenoid defect over time, primary trauma cases would need to be observed.
In this study, we concluded that the glenoid defect was significantly enlarged by damage due to recurrent dislocations and subluxations or by recurrent subluxations without any dislocation. Generally, as a dislocation event is thought to be more harmful than a subluxation event, recurrent subluxations are often overlooked. However, it was shown that recurrent subluxations were critical enough for the enlargement of glenoid defects. The distinction between dislocation and subluxation is quite difficult. As described, the definition of dislocation and subluxation was usually distinguished by the requirement of manual reduction by a health care provider. As spontaneous relocation or self-reduction is regarded as a subluxation event, though the humeral head transiently should be dislocated in such situations, the glenoid defect might be enlarged by such subluxation events without dislocation. Accordingly, we think that it would be better to consider such situations as dislocation. On the other hand, we often experience the large glenoid fracture with large bone fragment at the time of primary instability, especially in collision athletes. At that time, patients sometimes complained of “dead arm sensation” of their shoulder though their shoulder was not apparently dislocated. As such, a dead arm event is generally defined as a subluxation, and large glenoid defects might occur by repetitive subluxations.
Regarding the influence of the type of sport, glenoid defects were frequently recognized and were relatively large in male collision sports athletes. As they frequently had a history of major trauma, it seems that high-impact injury causes a large glenoid defect. There have been few reports regarding the relation between the size of the glenoid defect and the type of sport. Burkhart and de Beer3 studied 101 collision sports athletes (96 rugby players, 5 American football players) and found significant bone defects in 9, all of whom were rugby players. Postoperative recurrence was noted in 8 (89%) of 9 rugby players with a significant bone defect versus only 6 (7%) of 87 rugby players without a significant bone defect. On the other hand, there was no postoperative recurrence in the 5 American football players. They suggested that there would be a different mechanism of injury in the 2 groups because of differences in shoulder position during play. When a rugby player performs a “stiff-arm” maneuver, the axially directed force acts on the anterior glenoid rim and causes an intra-articular fracture (bony Bankart lesion) rather than avulsion of soft tissue from bone. In our series, glenoid defects were also more frequent and larger in rugby players than in American football players, but large glenoid defects were not rare in American football players. The larger glenoid defects of rugby players in our study might have been related to their higher rate of recurrent instability.
On the other hand, most baseball players did not have a glenoid defect, and most of the defects in this group were small. As the mechanism of injury, relatively minor trauma was frequent, such as sliding for a base or making a diving catch, and major trauma was rare. In our series, a glenoid defect was detected in 8 of 27 baseball players, but a large glenoid defect (>20%) was only seen in 2 players. These 2 players had a history of major trauma while all other players (including those without a glenoid defect) had a history of minor trauma. Since the rate of major trauma at the time of primary injury was significantly lower in baseball players than in collision athletes and was similar to female athletes, lower impact injury was thought to result in smaller glenoid defects. As far as we know, there has been no previous report that glenoid defects are smaller in baseball players, so this was an interesting finding. As another factor that could influence glenoid defects, joint laxity should be considered, though we did not investigate it in this study. Joint laxity was frequent in baseball players and female athletes, while absence of glenoid defects was common in male collision athletes with joint laxity. Accordingly, we would like to investigate the influence of joint laxity on glenoid defects in the future.
A limitation of this study was the retrospective design, so each patient was not observed over time. To confirm our hypothesis about enlargement of glenoid defects by recurrent events, patients with primary trauma would need to be observed over time. Though it is difficult to observe the natural course of a large glenoid defect without operation, it is possible to manage patients without a large defect conservatively. Thus, enlargement of the glenoid defect and absorption of bone fragment could be assessed by investigation of such patients. Another limitation was our method for quantification of glenoid defects. We used a simple and convenient method, which assumes that the inferior portion of the glenoid rim can be approximated to a true circle on the en face 3-dimensional reconstructed CT image. However, there were some cases in which fitting a circle was difficult. If the circle is set too large, the size of the glenoid defect will be exaggerated. In the future, to evaluate glenoid defects more precisely, it will be essential to employ other methods, such as comparison with glenoid rim morphology on the healthy opposite side.4 Because of these limitations of our method and because comparison with the contralateral side becomes difficult in cases of bilateral shoulder instability (common in collision sports), it will be necessary to develop new measuring methods. With regard to investigation of the influence of the type of sport on glenoid defects, both primary and recurrent cases were included in the present study, which is another limitation. Since the glenoid defect was enlarged by recurrence of dislocation and subluxation, it is impossible to conclude that the differences of defect size that we noted were purely related to the type of sport. To investigate the influence of the type of sport, a study based on primary trauma cases would be appropriate. However, the number of patients with primary instability was too small, especially among rugby players in this study, so we would need to enroll more primary cases for investigation in the future.
Conclusion
In shoulders with traumatic anterior instability, the glenoid defect is enlarged by damage due to recurrent dislocation and subluxation. As a result, glenoid rim morphology is different between recurrent instability and primary instability. Glenoid defects were also influenced by sex and the type of sport.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Boileau P, Bicknell RT, El Fegoun AB, Chuinard C. Arthroscopic Bristow procedure for anterior instability in shoulders with a stretched or deficit capsule: the “belt-and-suspenders” operative technique and preliminary results. Arthroscopy. 2007;23:593–601. [DOI] [PubMed] [Google Scholar]
- 2. Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. [DOI] [PubMed] [Google Scholar]
- 3. Burkhart SS, de Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repair: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677–694. [DOI] [PubMed] [Google Scholar]
- 4. Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008;24:376–382. [DOI] [PubMed] [Google Scholar]
- 5. Griffith JF, Antonio GE, Yung PS, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol. 2008;190:1247–1254. [DOI] [PubMed] [Google Scholar]
- 6. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82:35–46. [DOI] [PubMed] [Google Scholar]
- 7. Jiang CY, Zhu YM, Liu X, Li FL, Lu Y, Wu G. Do reduction and healing of the bony fragment really matter in arthroscopic bony Bankart reconstruction? A prospective study with clinical and computed tomography evaluations. Am J Sports Med. 2013;41:2617–2623. [DOI] [PubMed] [Google Scholar]
- 8. Kitayama S, Sugaya H, Takahashi N, et al. Glenoid morphology after arthroscopic osseous Bankart repair for recurrent anterior glenohumeral instability: a 5- to 8-year follow-up. Arthroscopy. 2013;29:e150–e151. [Google Scholar]
- 9. Lafosse L, Lejeune E, Bouchard A, Kakuda C, Gobezie R, Kochhar T. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242e1–1242.e5. [DOI] [PubMed] [Google Scholar]
- 10. Larrain MV, Montenegro HJ, Mauas DM, Collazo CC, Pavón F. Arthroscopic management of traumatic anterior shoulder instability in collision athletes: analysis of 204 cases with a 4- to 9-year follow-up and results with the suture anchor technique. Arthroscopy. 2006;22:1283–1289. [DOI] [PubMed] [Google Scholar]
- 11. Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy. 2004;20:169–174. [DOI] [PubMed] [Google Scholar]
- 12. Milano G, Grasso A, Russo A, et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39:1870–1876. [DOI] [PubMed] [Google Scholar]
- 13. Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB. Arthroscopic stabilization in patients with inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med. 2007;35:1276–1283. [DOI] [PubMed] [Google Scholar]
- 14. Nakagawa S, Mizuno N, Hiramatsu K, Tachibana Y, Mae T. Absorption of the bone fragment in shoulders with bony Bankart lesions caused by recurrent anterior dislocations or subluxations: when does it occur? Am J Sports Med. 2013;41:1380–1386. [DOI] [PubMed] [Google Scholar]
- 15. Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85:878–884. [DOI] [PubMed] [Google Scholar]
- 16. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 2005;87:1752–1760. [DOI] [PubMed] [Google Scholar]
- 17. Taverna E, Golanò P, Pascale V, Battistella F. An arthroscopic bone graft procedure for treating anterior-inferior glenohumeral instability. Knee Surg Sports Arthrosc. 2008;16:872–875. [DOI] [PubMed] [Google Scholar]
- 18. Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37:949–954. [DOI] [PubMed] [Google Scholar]


