Abstract
Background:
Redundancies in the rotator cuff tissue, commonly referred to as “dog ear” deformities, are frequently encountered during rotator cuff repair. Knowledge of how these deformities are created and their impact on rotator cuff footprint restoration is limited.
Purpose:
The goals of this study were to assess the impact of tear size and repair method on the creation and management of dog ear deformities in a human cadaveric model.
Study Design:
Controlled laboratory study.
Methods:
Crescent-shaped tears were systematically created in the supraspinatus tendon of 7 cadaveric shoulders with increasing medial to lateral widths (0.5, 1.0, and 1.5 cm). Repair of the 1.5-cm tear was performed on each shoulder with 3 methods in a randomized order: suture bridge, double-row repair with 2-mm fiber tape, and fiber tape with peripheral No. 2 nonabsorbable looped sutures. Resulting dog ear deformities were injected with an acrylic resin mixture, digitized 3-dimensionally (3D), and photographed perpendicular to the footprint with calibration. The volume, height, and width of the rotator cuff tissue not in contact with the greater tuberosity footprint were calculated using the volume injected, 3D reconstructions, and calibrated photographs. Comparisons were made between tear size, dog ear measurement technique, and repair method utilizing 2-way analysis of variance and Student-Newman-Keuls multiple-comparison tests.
Results:
Utilizing 3D digitized and injection-derived volumes and dimensions, anterior dog ear volume, height, and width were significantly smaller for rotator cuff repair with peripheral looped sutures compared with a suture bridge (P < .05) or double-row repair with 2-mm fiber tape alone (P < .05). Similarly, posterior height and width were significantly smaller for repair with looped peripheral sutures compared with a suture bridge (P < .05). Dog ear volumes and heights trended larger for the 1.5-cm tear, but this was not statistically significant.
Conclusion:
When combined with a standard transosseous-equivalent repair technique, peripheral No. 2 nonabsorbable looped sutures significantly decreased the volume, height, and width of dog ear deformities, better restoring the anatomic footprint of the rotator cuff.
Clinical Relevance:
Dog ear deformities are commonly encountered during rotator cuff repair. Knowledge of a repair technique that reliably decreases their size, and thus increases contact at the anatomic footprint of the rotator cuff, will aid sports medicine surgeons in the management of these deformities.
Keywords: dog ear deformity, rotator cuff repair, digitization, SutureBridge, SpeedBridge, FiberLink
The transosseous-equivalent rotator cuff repair is a contemporary technique that has been devised to optimize the construct biomechanics, footprint restoration, and tendon healing of a rotator cuff tear.15 This method utilizes medially and laterally positioned suture anchors to establish a suture bridge that compresses the rotator cuff footprint, optimizes tendon-bone contact, and creates a construct that is biomechanically strong enough to withstand the physiologic stresses experienced in the early healing period. When compared with other commonly utilized rotator cuff repair techniques, transosseous-equivalent rotator cuff constructs have been shown to significantly improve footprint contact characteristics,16 exhibit superior biomechanical properties,17 and prevent extravasation of synovial fluid that inhibits tendon-bone healing.1 Although studies have not conclusively shown the superiority of this technique based on clinical results,14 multiple authors argue that this method should be the technique of choice.4
Despite the inherent advantages of this technique, the transosseous-equivalent rotator cuff repair also possesses some frequently encountered shortcomings, notably redundancies in the rotator cuff tissue, which are commonly referred to as “dog ear” deformities. Various suture patterns10–13 have been created to minimize the occurrence of these deformities or manage them once they are formed, as consequences may include inadequate footprint restoration and impaired healing of the cuff to the greater tuberosity. Commonly encountered in other surgical wounds as well, dog ear deformities are the result of an asymmetric puckering or accumulation of tissue, typically in the center or at the apices of an incision. The etiology and management of these deformities are well described in the plastic and dermatologic surgery literature2,6,7,19,21,22; however, there is a relative paucity of literature regarding the causes and implications of dog ear deformities in rotator cuff repairs. This study was performed to quantify the effects of dog ear formation on rotator cuff footprint restoration after repair as well as to assess the association between rotator cuff repair method and the formation and management of dog ear deformities in a human cadaveric model. We hypothesized that the 3 tear sizes would be equally as likely to produce a dog ear deformity and that the 3 repair methods would manage dog ear deformities equivalently.
Materials and Methods
The study used 10 fresh-frozen human cadaveric shoulders (6 male, 4 female) with a mean age of 61.2 ± 1.7 years at time of death (range, 58-70 years). Specimens were stored at –20°C and thawed completely before dissection. Each specimen was visually inspected to rule out any evidence of prior surgery or fracture. On dissection, 3 specimens were found to have massive rotator cuff tears retracted to the glenoid and were thus excluded. The remaining 7 shoulders were randomized and included in the study protocol.
Specimen Preparation
Specimens were mounted upright in standard fashion via a vice clamp to the scapula. Skin, superficial fat, and the deltoid were dissected from the scapula, clavicle, and proximal humerus to reveal the rotator cuff musculature and its tendon insertions. The acromion was removed at its base, and the clavicle was excised for improved visualization of the rotator cuff tendons. A nonabsorbable suture was placed in running, locking fashion into the muscle belly of the supraspinatus for approximately 6 cm, beginning just medial to the musculotendinous junction. The free ends of the suture were tied and draped over a pulley, and a 200-g weight was applied to provide constant tension on the rotator cuff repairs (Figure 1, A and B). A 7-mm drill hole was made from lateral to medial 8 cm distal to the greater tuberosity for passage of traction sutures used to reduce the cuff to the lateral footprint in the tear creation portion of the protocol (Figure 2).
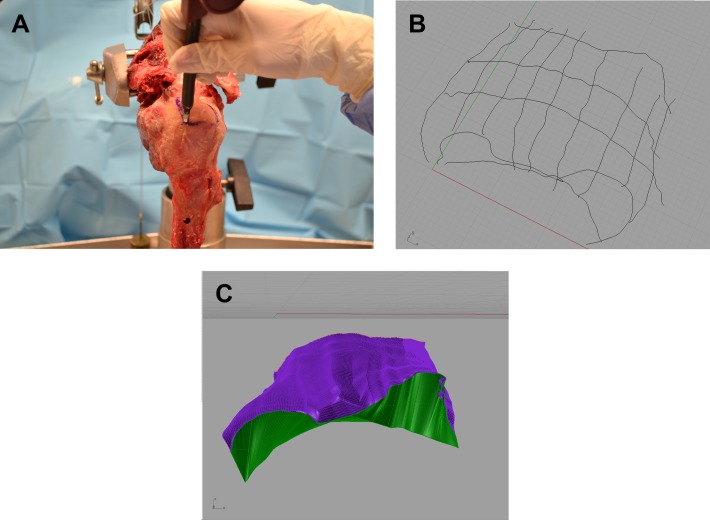
Figure 1.
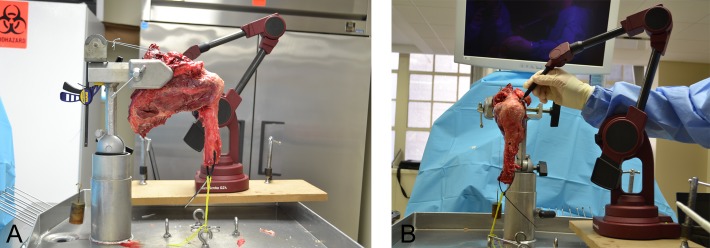
(A and B) Setup. The scapula is clamped, soft tissues dissected, and a suture/pulley construct used to maintain constant tension on the rotator cuff.
Figure 2.
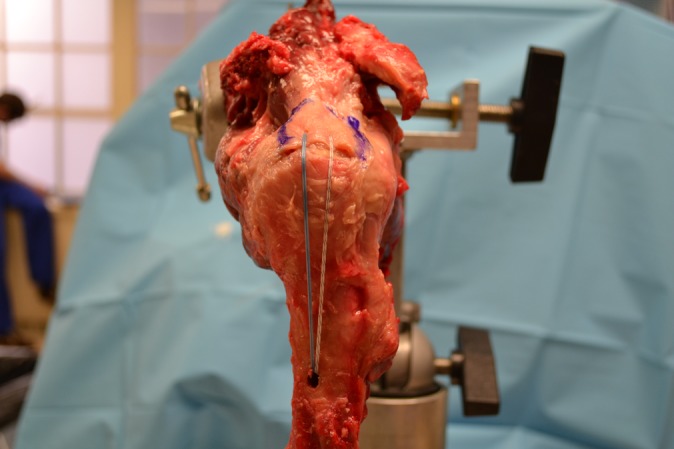
Traction sutures through the edge of the cuff “tear” passed from lateral to medial through the 7-mm hole.
Tear Creation
Tears were systematically created in the supraspinatus tendon by sharply dividing it from its insertion on the greater tuberosity, starting anteriorly at the posterior aspect of the bicipital groove and extending 3 cm posteriorly. Serial ellipses of tissue were resected, creating elliptical-shaped tears of 0.5, 1.0, and 1.5 cm at the apex in the medial to lateral direction, thereby modeling the spectrum from crescent to U-shaped tears and simulating tear retraction. Two 4.5-mm PEEK Corkscrew FT suture anchors (Arthrex, Naples, Florida, USA) were placed at the articular margin evenly spaced from anterior to posterior (1 cm apart in the 3-cm tear space) at 45° relative to the footprint surface (the deadman angle20). After each tear was created, a microsuture lasso was used to pass the medial row sutures in a horizontal mattress fashion from deep to superficial 1 cm medial to the lateral edge of the rotator cuff tear, centered over each corresponding suture anchor. Rather than tying these sutures, they were tensioned, passed through the 7-mm drill hole in the midshaft of the humerus, and clamped on the medial aspect of the humerus to maintain reduction of the lateral edge of the rotator cuff to the greater tuberosity. Resulting dog ear deformities were injected with an acrylic resin mixture, and the rotator cuff was digitized from its lateral insertion to 1.6 cm medial5 using the MicroScribe 3D Digitizer (Solution Technologies, Oella, Maryland, USA). Calibrated photographs were taken perpendicular to the footprint by photographing the rotator cuff and a 2-cm ruler. The sutures were then removed from the rotator cuff tissue, and an additional ellipse of rotator cuff measuring 5 mm medial to lateral at its apex was resected. Sutures were replaced 1 cm from the newly formed edge of the cuff, and the sequence of injection, photographs, and digitization was repeated. This same sequence was again repeated on a tear size of 1.5 cm in the medial-lateral direction.
Injection Technique
A mixture of 2 mL poly-methylmethacrylate (Acraweld Repair Powder; Henry Schein, Melville, NY, USA) and 1 mL acrylic liquid was placed into a 1-mL syringe. An 18-gauge intravenous catheter tip was used on the end of the syringe for the injection. The edge of the tissue forceps was used to compress the rotator cuff to the humerus 1.6 cm medial to the lateral edge (Figure 3). This dam prevented the acrylic resin mixture from passing medially into the patulous intra-articular space medial to the rotator cuff footprint. The mixture was then injected into the dog ears in similar fashion to cementing techniques, retracting the syringe as the potential space was filled with the compound. The volume of acrylic resin mixture required to fill the dog ear deformity was recorded to quantify the size of the dog ear deformity. After injection, 30 seconds were allotted to allow the mixture to cure and harden, providing a firm surface to digitize using the MicroScribe 3D Digitizer. The resin was then completely removed from the specimen after each repair technique was performed.
Figure 3.
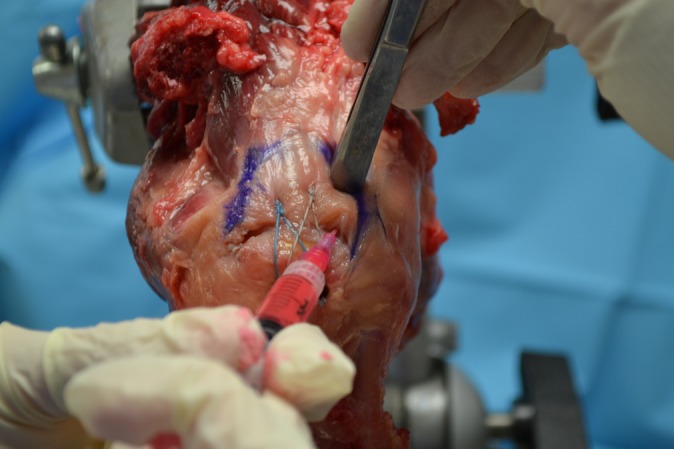
Creating a dam. A tissue forceps is used to create a dam 1.6 cm medial to the edge of the footprint to prevent the acrylic resin from extruding into the joint.
Repair Techniques
The 3 × 1.5–cm tear was repaired by 3 methods on each specimen in a randomized order. These techniques included a traditional transosseous-equivalent repair (SutureBridge; Arthrex), a knotless transosseous-equivalent repair with nonabsorbable suture tape (SpeedBridge; Arthrex), and a knotless transosseous-equivalent repair with the addition of peripheral looped FiberLink (Arthrex) sutures placed at the apex of the subsequently created dog ears. All measurements for placement of anchors and passage of sutures through the supraspinatus tendon were carefully performed with a ruler to standardize the technique for each specimen. A single surgeon performed all repairs on all specimens.
SutureBridge
This repair was performed with 2 4.5-mm PEEK Corkscrew FT suture anchors medially and 2 knotless 4.75-mm SwiveLock anchors (Arthrex) laterally. The medial row anchors were placed at the lateral edge of the articular margin of the humeral head evenly spaced from anterior to posterior (1 cm apart in the 3-cm tear space) at 45° relative to the footprint surface (deadman angle20). The medial row sutures were passed in a horizontal mattress fashion 1 cm medial to the lateral edge of the rotator cuff tear, centered over each corresponding suture anchor. Both medial row knots were tied with a sliding double half-hitch knot first, followed by 3 alternating simple half-hitches. One limb from each suture anchor was threaded through each of the 2 lateral knotless anchors. The lateral row anchors were then inserted 1.5 cm lateral to the rotator cuff footprint, spaced 1 cm apart (Figure 4). If a specimen was randomized to either of the 2 SpeedBridge arms prior to the SutureBridge, 5.5-mm PEEK Corkscrew FT suture anchors were substituted for the 4.5-mm medial suture anchors to accommodate the larger medial anchor holes from the previously placed 4.75-mm anchors.
Figure 4.
Lateral row anchors were inserted 1.5 cm lateral to the rotator cuff footprint, spaced 1 cm apart.
SpeedBridge
This technique was performed with 4 knotless 4.75-mm SwiveLock anchors, with the 2 medial anchors loaded with FiberTape (Arthrex). The medial row anchors were placed in the same locations previously described. Both limbs of the FiberTape from each anchor were passed through the supraspinatus tendon 1 cm medial to the lateral edge of the rotator cuff tear. One FiberTape limb from each medial anchor was threaded through each of the 2 lateral knotless anchors. As previously described, the lateral anchors were inserted 1.5 cm lateral to the rotator cuff footprint, spaced 1 cm apart.
SpeedBridge + FiberLink
This technique was performed as previously described for the SpeedBridge with the addition of peripheral looped FiberLink sutures. A microsuture lasso was used to penetrate the cuff 5 mm posterior to the bicipital groove and 1 cm medial to the lateral edge of the rotator cuff tear, at the apex of the dog ear deformity. The FiberLink was then shuttled through the cuff tissue, ensuring that the loop was on the superior aspect of the cuff. This step was repeated for the posterior dog ear deformity, placing a second looped peripheral FiberLink suture 5 mm posterior to the posterior medial row anchor. The tails of the FiberLink sutures were incorporated into the knotless lateral row anchors (Figure 5).
Figure 5.
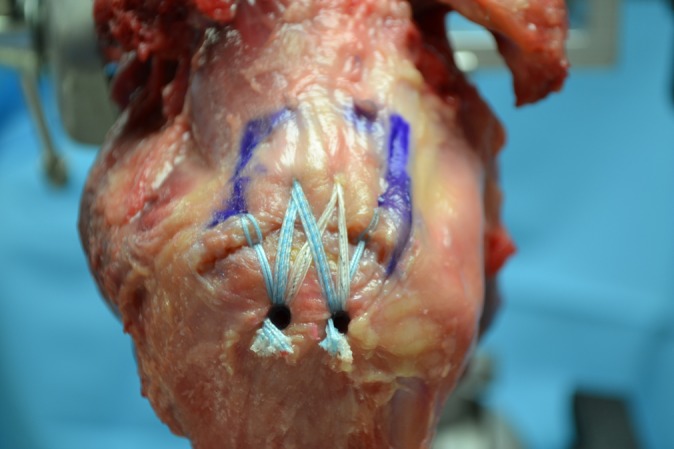
SpeedBridge with peripheral looped FiberLink repair.
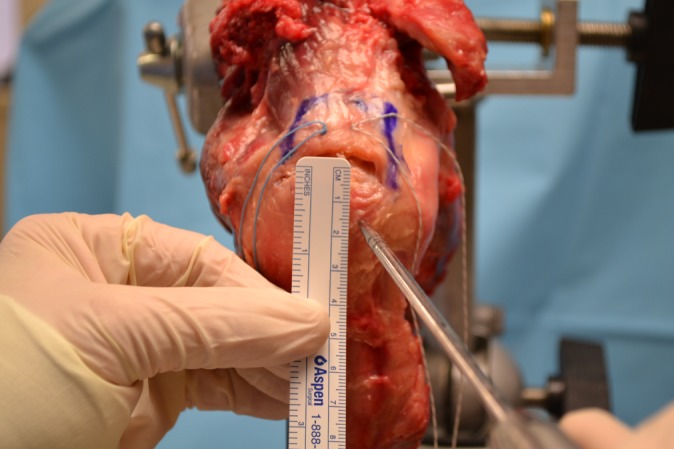
Measurement of Dog Ear Deformities
Immediately following each successive tear creation as well as after each of the 3 repair techniques of the 1.5-cm tear, the rotator cuff tissue and greater tuberosity footprint were digitized using the MicroScribe 3D system via creation of point clouds. Digitization was performed by a single member of the research team in a systematic fashion, using a probe to outline the rotator cuff with multiple medial to lateral lines starting anteriorly and moving posteriorly (Figure 6A). The boundaries of the rotator cuff footprint were then outlined systematically starting with the medial border, followed by the lateral cuff edge, then finally the greater tuberosity footprint edge (Figure 6B). Surface curves were traced, lofted, and smoothed with Rhinoceros software (McNeel North America, Seattle, Washington, USA) to create 3-dimensional volumetric representations of each repair (Figure 6C). Dog ear height, width, and volume of rotator cuff tissue not in contact with the greater tuberosity footprint were calculated for the anterior and posterior dog ear in each repair. Dog ear height and width were then measured from the calibrated photographs of the specimens previously described (Figure 7).
Figure 6.
(A) Digitizing the rotator cuff. (B) Digitized rotator cuff. An unsmoothed representation of the rotator cuff and dog ears. (C) Smoothed 3-dimensional digitization. Surface curves were traced, lofted, and smoothed with Rhinoceros software.
Figure 7.
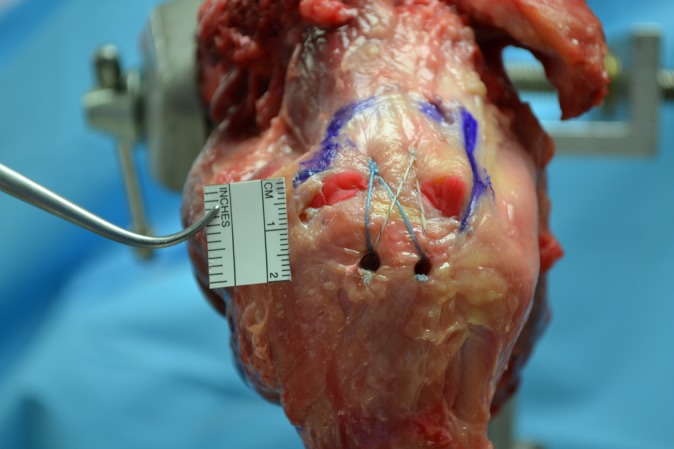
Calibrated photograph.
Data Analysis
The volume, height, and width of rotator cuff tissue not in contact with the greater tuberosity footprint were calculated using the volume injected, MicroScribe-derived 3D reconstructions, and the calibrated photographs. Comparisons were made between tear sizes, dog ear measurement techniques, and repair methods utilizing 2-way general linear model analysis of variance (GLM ANOVA) and Student-Newman-Keuls multiple-comparison tests. Statistical significance was defined a priori as P < .05.
Intrarater Reliability
As dog ear deformities have not been previously quantified in the literature, novel methods of measuring these redundancies were created. Therefore, intrarater reliability testing was performed to demonstrate the reproducibility of our data collection methodology.
To determine the repeatability of the calculations used to compute the dimensions of the heights and widths of the anterior and posterior dog ears as measured from photographs, a single observer computed the dimensions on 3 separate occasions, separated by at least 1 week between each calculation. Two-way ANOVAs (SAS, Cary, North Carolina, USA) were run for each dimension, with the condition of the cuff (0.5-mm tear, 1.0-cm tear, 1.5-cm tear, SutureBridge repair, SpeedBridge repair, and FiberLink repair) as one factor and measurement (first trial, second trial, third trial) as the second factor. Both factors were repeated on the 7 subjects that were studied. Student-Newman-Keuls multiple comparison tests were run to discern differences between levels of a factor if significant differences were found (P < .05).
Results
No statistical differences were found between trials for the anterior height (P = .9767), posterior height (P = .9035), anterior width (P = .7496), or posterior width (P = .2139). Repeatability was not affected by the condition of the rotator cuff for the anterior height (P = .9568), posterior height (P = .7030), the anterior width (P = .6437), and posterior width (P = .0659). In terms of the precision of the length calculations, the standard deviation for all 3 trials was divided by the mean of all 3 trials for each condition for all subjects. The averages and standard deviations of these values in terms of percentage were 3.46% ± 4.57% for anterior heights, 4.67% ± 6.56% for posterior heights, 3.47% ± 2.59% for anterior widths, and 6.29% ± 5.38% for posterior widths. Therefore, on average, the variation in all dimensions computed was within 6.5%.
To determine the repeatability of the calculations used to compute the volumes of the anterior and posterior dog ears when a 1.6 cm–deep dog ear was selected, a single observer computed the volumes on 3 separate occasions, separated by at least 1 week between each calculation. Two-way ANOVAs (SAS) were run for each volume, with the condition of the cuff (0.5-cm tear, 1-cm tear, 1.5-cm tear, SutureBridge repair, SpeedBridge repair, and FiberLink repair) as one factor and measurement (first trial, second trial, third trial) as the second factor. Both factors were repeated on the 5 subjects that were studied. Student-Newman-Keuls multiple-comparison tests were run to discern differences between levels of a factor if significant differences were found (P < .05).
No statistical differences were found between trials for the anterior dog ear volume (P = .2025) or posterior volume (P = .7103). Repeatability was not affected by the condition of the rotator cuff for both the anterior measurement (P = .7750) and posterior measurement (P = .1627). In terms of the precision of the volume calculations, the standard deviation for all 3 trials was divided by the mean of all 3 trials for each condition for all subjects. The averages and standard deviations of these values in terms of percentage were 4.58% ± 5.63% for the anterior volumes and 4.90% ± 4.16% for the posterior volumes. Therefore, on average, the variation in volumes computed was within 5% for both anterior and posterior volumes.
Tear Creation
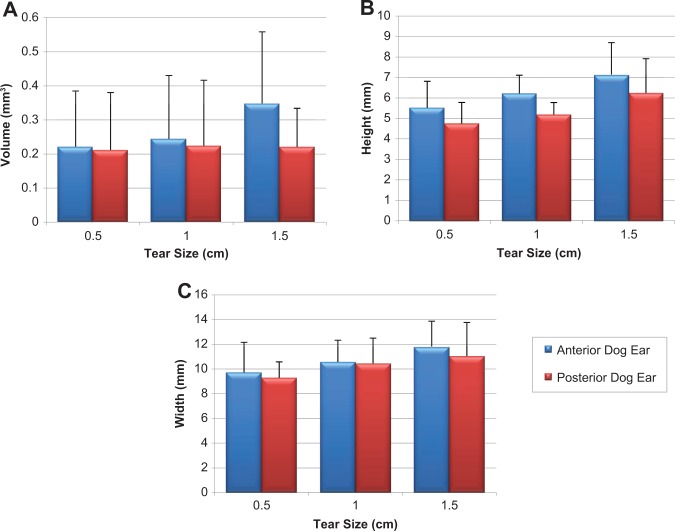
Dog ear volumes and heights trended larger for the 1.5-cm tear, but there was no statistical difference between 0.5-cm, 1.0-cm, and 1.5-cm tears with any measurement modality (Figure 8, A-C).
Figure 8.
(A) Dog ear volume, (B) height, and (C) width. Volume, height, and width trended larger for the 1.5-cm tear, but there was no significant difference.
Repair Methods of 1.5-cm Tear
Volume Measurements
When comparing volume measurement modalities, MicroScribe-derived volumes were significantly larger compared with injection volumes (P < .001). This result was expected, as the MicroScribe volume includes the thickness of the rotator cuff tissue while the volume of injected acrylic resin only fills the potential space of the dog ear deformity. Anterior dog ear volume was significantly smaller for rotator cuff repair with peripheral FiberLink sutures compared with SutureBridge (P < .05) or SpeedBridge (P < .05) alone (Figure 9). This result was similar utilizing both MicroScribe- and injection-derived volumes for the anterior dog ear (P = .2851) and posterior dog ear (P = .1446). There was no statistically significant difference between repair methods for the posterior dog ear volume using any measurement modality.
Figure 9.
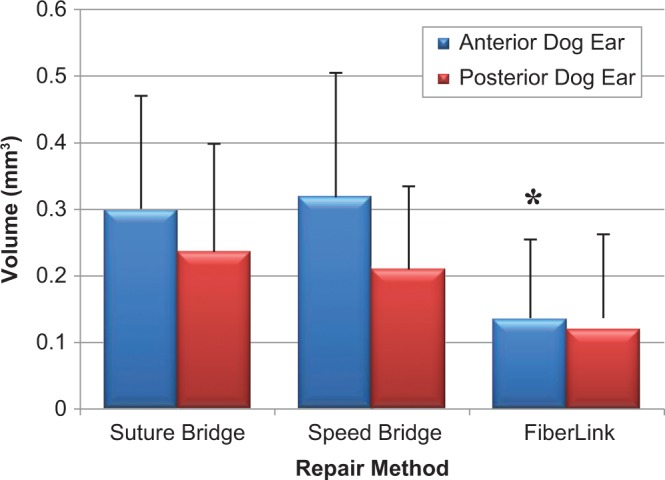
Dog ear volume. Anterior dog ear volume was significantly smaller for repair with FiberLink compared with SutureBridge or SpeedBridge alone. *Significant difference.
Height and Width
Utilizing both MicroScribe- and calibrated photograph–derived dimensions, anterior dog ear height and width were significantly smaller for rotator cuff repair with peripheral FiberLink sutures compared with SutureBridge (P < .05) or SpeedBridge alone (P < .05). Similarly, posterior height and width were significantly smaller for rotator cuff repair with peripheral FiberLink sutures compared with SutureBridge alone (P < .05). When comparing measurement modalities, there was no statistical difference in the measurements between calibrated photograph– and MicroScribe-derived data for anterior height (P = .2114), posterior height (P = .1753), anterior width (P = .6502), or posterior width (P = .1226).
Discussion
Our study has shown reduced dog ear deformity volume for repair with peripheral looped FiberLink sutures compared with SutureBridge or SpeedBridge transosseous-equivalent techniques alone. The additional peripheral looped suture further compresses the rotator cuff tendon against the bone and can be placed at the apex of a dog ear deformity, maximizing tendon-bone contact. With this increased contact area at the greater tuberosity footprint, we would expect better healing, in part because of less fluid extravasation and thus less interference with healing.1 While we were unable to determine a threshold tear size at which the surgeon should expect marginal dog ear deformities, with larger tears, the surgeon should be prepared to address these deformities with either the modified suture bridge11 or peripheral FiberLink sutures, as described here.
The goals of a rotator cuff repair include restoration of the anatomic footprint without excessive tension, minimizing gap formation, and stable initial fixation that can be sustained until healing.18 The transosseous-equivalent technique of rotator cuff repair achieves these goals in the majority of cases. However, the formation of peripheral dog ear deformities is not uncommon with this method.10 A marginal dog ear deformity after repair may be considered similar to a bursal-sided partial-thickness rotator cuff tear as it can result in the lack of contact between a substantial portion of the rotator cuff and the greater tuberosity. Beyond the understanding that dog ear deformities are more frequent in large tears than in medium tears,10 knowledge of how these deformities are created and their impact on rotator cuff footprint restoration is limited. The ability to characterize, quantify, and manage these imperfections will prove useful to all who perform arthroscopic rotator cuff repairs. To our knowledge, this is the first quantitative study assessing the creation and management of dog ear deformities in rotator cuff repairs in a human cadaveric model.
Dog ear deformities are well documented in the plastic and dermatologic surgical literature. Jaibaji et al8 define a dog ear as a characteristic puckering of the skin occurring after wound closure. Dzubow6 defined dog ears as tissue redundancies secondary to length inequalities, rotation, or contour changes. Weisberg et al21 further describe that wounds closed under excessive tension will cause a depression of the central portion and vertical displacement of the apices, thus creating the appearance of dog ears. Wounds on convex surfaces, similar to the rotator cuff footprint at the greater tuberosity, are more susceptible to this deformity.21 Techniques used in plastic and dermatologic surgery to manage dog ear deformities, including fusiform excision, S-plasty, M-plasty, and V-excision,2,6–8,19,21,22 are not applicable to dog ear deformities in rotator cuff repairs.
For large, retracted, U-shaped tears, margin convergence can be used to minimize formation of dog ear deformities.3 Kandemir et al9 introduced the concept of a repair ratio as a guide for application of margin convergence. The authors defined a repair ratio as the ratio of the length of the torn tendon edge and the length of the avulsed insertion site. For a repair ratio of 1, the entire avulsed tendon edge can be repaired to the greater tuberosity footprint. However, for a repair ratio of 2, only 50% of the tendon edge can be repaired to bone. The authors state that the remainder of the torn edge that cannot be repaired to bone should be repaired in a side-to-side fashion. Some tears, however, are not amenable to side-to-side repair and are destined to form dog ears at the periphery. While our data show that larger tears were more likely to result in larger dog ears, it lacked the power to show this relationship to be statistically significant. Alternatively, Kim et al11 reported on a technique of using the suture tails from the lateral row anchors to create an additional site of compression in the marginal dog ear deformity, the so-called modified suture bridge. Other authors have purported using additional anchors11 or a triple-mattress repair with a single row of triple-loaded suture anchors12,13 to manage these deformities. However, there is no literature to quantify the size of these dog ear deformities before and after these various repair techniques.
This is the first study to quantify the height, width, and volume of dog ear deformities after various rotator cuff repair methods. It was performed on human cadavers with ages consistent with the pathology of rotator cuff tears. Several limitations regarding this study should be considered. First, many variations in rotator cuff repair methods exist for the transosseous-equivalent repair. This study does not attempt to determine the dog ear deformity characteristics for all possible configurations, including the multitude of tear configurations, suture anchor designs, and suture material, but rather provides a simple comparison between suture bridge, transosseous-equivalent repair with 2-mm fiber tape, and transosseous-equivalent repair with 2-mm fiber tape and peripheral No. 2 nonabsorbable looped sutures incorporated in the lateral row anchors. We felt that these repair methods were representative of rotator cuff repair methods that are in clinical use.
The dog ear volume determined by injection of the acrylic resin mixture may have been influenced by leakage into the glenohumeral joint space medially. An attempt was made to obstruct the escape of the mixture into the glenohumeral joint using tissue forceps compressing the cuff 1.6 cm medial to the repair edge (the mean medial to lateral width of the supraspinatus footprint).5 The influence of this factor is negligible based on the fact that there was no statistical difference between the injection- and MicroScribe-derived volumes.
One goal of our study was to determine a threshold of tear retraction at which a sizeable dog ear deformity can be expected. We did not show a significant difference in the dog ear sizes between tears with simulated retraction of 0.5, 1.0, and 1.5 cm. Tears of these sizes may behave differently in an in vivo model as they are likely to retract over time, a phenomenon that we did not observe in our cadavers. Our study only looked at 1 tear configuration, a 3-cm ellipse with a maximum 1.5-cm retraction. Further knowledge could be gained if this study were to be repeated on more cadavers with differing tear geometries, including large U-shaped tears. This is a potential limitation since massive tears with further retraction to the glenoid were not assessed. Perhaps with larger medial to lateral tear sizes we would be able to determine a threshold tear that leads to sizeable dog ear deformities. This information would prove useful for preoperative planning purposes. While this study quantifies dog ears and demonstrates a reproducible method for their management, further studies are needed to assess the biomechanical and clinical impact such deformities have on healing and postoperative function.
Conclusion
In characterizing dog ear deformities and assessing the factors impacting their creation, this study helps the surgeon better understand how to avoid and manage these irregularities in rotator cuff repair. When combined with a transosseous repair technique, peripheral looped FiberLink sutures significantly decreased the volume, height, and width of dog ear deformities, better restoring the anatomic footprint of the rotator cuff.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This project was funded by an educational grant from Arthrex Inc. Cadavers and implants for this research were provided by Arthrex Inc. The Arthrex company and granting agency had no influence over the design or conduct of the study or the analysis or interpretation of the study data. None of the authors or the departments with which they are affiliated has received anything of value from or owns stock in a commercial company or institution related directly or indirectly to the subject of this article.
References
- 1. Ahmad CS, Vorys GC, Covey A, Levine WN, Gardner TR, Bigliani LU. Rotator cuff repair fluid extravasation characteristics are influenced by repair technique. J Shoulder Elbow Surg. 2009;18:976–981. [DOI] [PubMed] [Google Scholar]
- 2. Borges AF. Dog-ear repair. Plast Reconstr Surg. 1982;69:707–713. [DOI] [PubMed] [Google Scholar]
- 3. Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335–338. [DOI] [PubMed] [Google Scholar]
- 4. Burkhart SS, Cole BJ. Bridging self-reinforcing double-row rotator cuff repair: we really are doing better. Arthroscopy. 2010;26:677–680. [DOI] [PubMed] [Google Scholar]
- 5. Curtis AS, Burbank KM, Tierney JJ, Scheller AD, Curran AR. The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy. 2006;22:609.e1. [DOI] [PubMed] [Google Scholar]
- 6. Dzubow LM. The dynamics of dog-ear formation and correction. J Dermatol Surg Oncol. 1985;11:722–728. [DOI] [PubMed] [Google Scholar]
- 7. Hudson-Peacock MJ, Lawrence CM. Comparison of wound closure by means of dog ear repair and elliptical excision. J Am Acad Dermatol. 1995;32:627–630. [DOI] [PubMed] [Google Scholar]
- 8. Jaibaji M, Morton JD, Green AR. Dog ear: an overview of causes and treatment. Ann R Coll Surg Engl. 2001;83:136–138. [PMC free article] [PubMed] [Google Scholar]
- 9. Kandemir U, Allaire RB, Debski RE, Lee TQ, McMahon PJ. Quantification of rotator cuff tear geometry: the repair ratio as a guide for surgical repair in crescent and U-shaped tears. Arch Orthop Trauma Surg. 2010;130:369–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kim KC, Rhee KJ, Shin HD. Deformities associated with the suture-bridge technique for full-thickness rotator cuff tears. Arthroscopy. 2008;24:1251–1257. [DOI] [PubMed] [Google Scholar]
- 11. Kim KC, Rhee KJ, Shin HD, Kim YM. A modified suture-bridge technique for a marginal dog-ear deformity caused during rotator cuff repair. Arthroscopy. 2007;23:562.e1–562.e4. [DOI] [PubMed] [Google Scholar]
- 12. Lorbach O, Kieb M, Raber F, Busch LC, Kohn D, Pape D. Comparable biomechanical results for a modified single-row rotator cuff reconstruction using triple-loaded suture anchors versus a suture-bridging double-row repair. Arthroscopy. 2012;28:178–187. [DOI] [PubMed] [Google Scholar]
- 13. Lorbach O, Pape D, Raber F, Kohn D, Kieb M. Arthroscopic rotator cuff repair using a single-row of triple-loaded suture anchors with a modified suture configuration. Arch Orthop Trauma Surg. 2011;131:1073–1076. [DOI] [PubMed] [Google Scholar]
- 14. Nho SJ, Slabaugh MA, Seroyer ST, et al. Does the literature support double-row suture anchor fixation for arthroscopic rotator cuff repair? A systematic review comparing double-row and single-row suture anchor configuration. Arthroscopy. 2009;25:1319–1328. [DOI] [PubMed] [Google Scholar]
- 15. Park MC, Elattrache NS, Ahmad CS, Tibone JE. “Transosseous-equivalent” rotator cuff repair technique. Arthroscopy. 2006;22:1360e1–1360.e5. [DOI] [PubMed] [Google Scholar]
- 16. Park MC, ElAttrache NS, Tibone JE, Ahmad CS, Jun BJ, Lee TQ. Part I: footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461–468. [DOI] [PubMed] [Google Scholar]
- 17. Park MC, Tibone JE, ElAttrache NS, Ahmad CS, Jun BJ, Lee TQ. Part II: biomechanical assessment for a footprint-restoring transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:469–476. [DOI] [PubMed] [Google Scholar]
- 18. Provencher MT, Kercher JS, Galatz LM, Elattrache NS, Frank RM, Cole BJ. Evolution of rotator cuff repair techniques: are our patients really benefiting? Instr Course Lect. 2011;60:123–136. [PubMed] [Google Scholar]
- 19. Salasche SJ, Roberts LC. Dog-ear correction by M-plasty. J Dermatol Surg Oncol. 1984;10:478–482. [DOI] [PubMed] [Google Scholar]
- 20. Strauss E, Frank D, Kubiak E, Kummer F, Rokito A. The effect of the angle of suture anchor insertion on fixation failure at the tendon-suture interface after rotator cuff repair: deadman’s angle revisited. Arthroscopy. 2009;25:597–602. [DOI] [PubMed] [Google Scholar]
- 21. Weisberg NK, Nehal KS, Zide BM. Dog-ears: a review. Dermatol Surg. 2000;26:363–70. [DOI] [PubMed] [Google Scholar]
- 22. Zitelli JA. Tips for wound closure. Pearls for minimizing dog-ears and applications of periosteal sutures. Dermatol Clin. 1989;7:123–128. [PubMed] [Google Scholar]