Abstract
Background:
Proximal biceps pathology is a significant factor in shoulder pain. Surgical treatment options include biceps tenotomy and subpectoral biceps tenodesis. Tenotomy is a simple procedure, but it may produce visible deformity, subjective cramping, or loss of supination strength. Tenodesis is a comparatively technical procedure involving a longer recovery, but it has been hypothesized to achieve better outcomes in younger active patients (<55 years).
Hypothesis:
This study investigated the outcomes of younger patients who underwent either a biceps tenotomy or tenodesis as part of treatment for shoulder pain. The hypothesis was that, apart from cosmetic deformity, there will be no difference in outcome between the 2 treatment options.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Isometric strength and endurance testing of operative and nonoperative shoulders for forearm supination (FS) and elbow flexion (EF) were tested utilizing an isometric dynamometer. Objective physical assessment was also performed. Subjective outcomes using the modified American Shoulder and Elbow Surgeons score (ASES); Disability of the Arm, Shoulder, and Hand (DASH); visual analog scale (VAS); and perceived biceps symptoms were collected.
Results:
A total of 42 patients (22 tenotomy, 20 tenodesis) with an average follow-up of 3.3 years were studied. The average age at follow-up was 49.9 years. Thirty-five percent (7/20) of tenotomy patients exhibited a “Popeye” deformity, compared with 18.2% (4/22) of tenodesis patients. Strength prior to fatiguing exercise was similar between tenodesis and tenotomy for FS (6.9 vs 7.3 lbs; P < .05), EF in neutral (35.4 vs 35.4 lbs), and EF in supination (33.8 vs 34.2 lbs). Strength was not significantly different between groups for isometric strength and endurance measures. Subjective functional outcome measured by the DASH, ASES, and VAS scores were similar between groups. Frequency of complaints of cramping was higher in the tenotomy group (4/20 vs 1/22), and complaints of pain were higher in the tenodesis group (11/22 vs 5/20).
Conclusion:
Despite increased demands and activity placed on biceps function in a younger population, this study showed no differences in functional and subjective outcome measurements. The choice between biceps tenotomy and tenodesis for pathology of the proximal biceps tendon can continue to be based on surgeon and patient preference.
Keywords: biceps tendon, tenotomy, tenodesis, shoulder arthroscopy, younger patients
Lesions of the long head of the biceps tendon are a common cause of shoulder pain and are generally treated at the time of shoulder arthroscopy. Biceps tendon pathology can take on many forms, and operative intervention is typically reserved for cases of recalcitrant tenosynovitis or tendinosis, acute or degenerative tearing, or biceps instability. Failure to address symptomatic biceps pathology at the time of surgery can result in continued pain.2,3,5,9,16 Considerable debate exists as to which treatment to employ—biceps tenodesis or tenotomy—at the time of surgery.1,9,10,13–16,20,21 Both tenodesis and tenotomy have been shown to produce favorable clinical results.1,9,14,15,26 Proponents of tenotomy claim that it is simple, has low surgical morbidity, takes little operative time, avoids change to postoperative rehabilitation, and has good, predictable pain relief.6,19 Proponents of tenodesis claim that it helps avoid cosmetic deformity, may help avoid subjective cramping, and better maintains supination strength.1
Although treatment algorithms have been proposed based on patient age, activity level, and sex,18 few studies directly compare the 2 techniques.7,8,16,22,26 Some authors reporting on tenotomy have found satisfactory cosmetic results, with infrequent “Popeye” deformity.6,22 Other studies have shown as much as a 70% incidence of Popeye deformity.13 Several studies have found no statistical difference between the 2 treatments with regard to elbow flexion and supination strength.9,16,23 Conversely, others have found a 20% decrease in supination strength and an 8% to 20% decrease in elbow flexion strength compared with the contralateral side after tenotomy. Supination strength was found to decrease by as much as 40% in 1 study.19,20
As no clear consensus can be found in the literature as to when and how to employ each modality compared with the other,16 we sought to retrospectively review a series of patients treated with each alternative. Using demographic and outcomes data, we strived to better elucidate the differences, if any, between these 2 treatment options.
We compared strength and subjective patient and surgeon outcomes between 2 groups of patients treated by 1 surgeon from 2005 to 2012. The 2 groups include those having a subpectoral biceps tenodesis versus those that have undergone a proximal biceps tendon tenotomy. We hypothesized that there would be no difference between the 2 groups in terms of subjective outcomes and isometric strength and endurance testing. Secondarily, we hypothesized that there would be a difference in cosmetic result, with more of the biceps tenotomy patients reporting a Popeye deformity.
Materials and Methods
A systematic search using surgical Current Procedural Terminology (CPT) codes 23430, 29822, and 29999 from the participating surgeon were reviewed for cases including biceps tenotomy or biceps tenodesis. Charts were then reviewed for accuracy of the diagnosis and satisfaction of inclusion criteria. All individuals aged 55 years or younger at the time of surgery who underwent a biceps tenodesis or biceps tenotomy at least 1 year prior to the study start date were initially contacted. Of 82 patients contacted, 42 agreed to participate in the study (22 tenodesis, 20 tenotomy). Of these patients, 9 also underwent rotator cuff repair only (4 tenodesis, 5 tenotomy), 7 had a subacromial decompression only (3 tenodesis, 4 tenotomy), and 8 (4 tenodesis, 4 tenotomy) had both procedures concurrently with their biceps procedure. The study was approved by an institutional review board, and all participants provided written informed consent prior to undertaking any study procedures.
Operative Technique and Rehabilitation
Patients in whom biceps tendon pathology was suspected based on clinical evaluation underwent counseling regarding different treatment options. Preoperative suspicion of biceps pathology was considered when the patient had bicipital groove pain, a positive Speeds or Yergeson test, or when a patient had complaints of pain over the anterior shoulder region, especially with radiation down the anterior brachium but not below the elbow. On magnetic resonance imaging, significant edema in the bicipital groove, biceps adhesions or tendinopathy, biceps dislocation from the groove, or partial tears were significant. Intraoperative findings that led to biceps treatment included a confirmed superior labral anterior-posterior lesion greater than stage 1, biceps instability with dislocation into the upper subscapular border, or significant biceps degenerative tearing or tendinopathy. After confirmation of proximal biceps pathology intraoperatively, either tenodesis or tenotomy was performed at the discretion of the treating surgeon. All patients underwent surgery in the beach-chair position and had a diagnostic arthroscopy performed. For tenodesis, an incision was made in the axillary crease centered over the lower border of the pectoralis muscle belly. The pectoralis major was then retracted proximally, and a Homan retractor was placed over the lateral aspect of the humerus, exposing the biceps tendon and bicipital groove. Next, the bicipital groove was prepared with a curette to encourage bone-tendon healing, and a 4.5-mm doubly loaded bioabsorbable suture anchor was placed in the center of the bicipital groove. Both sutures were then passed through the tendon and tied in place, after which the tendon was severed just above the suture anchor. This ensured that tension on the biceps was unchanged from its native position. Subsequently, during the arthroscopic portion of the procedure, the biceps was released near its insertion at the superior labrum, and the bicipital stump was removed from the shoulder. For tenotomy, the proximal biceps was cut at its insertion at the biceps labral complex; subsequently, the superior labrum was debrided.
After a tenodesis procedure, no active biceps motion was allowed for a period of 4 weeks after surgery, and no biceps-related strengthening was done for 8 weeks postoperatively. A sling was worn for 4 weeks postoperatively or longer if necessitated by concomitant treated pathology. For a tenotomy procedure without concomitant pathology, a sling was worn for 1 week followed by early active flexion of the elbow and shoulder with advancement of strength and activity as tolerated. However, if there was additional pathology (ie, rotator cuff tear), the rehabilitation was dictated by those injuries.
Testing
Participants underwent a physical examination assessing total shoulder range of motion, signs of tenderness including impingement, and other pathological findings of a shoulder injury (eg, crepitus, atrophy). Medical Research Council grading was used to determine strength against resistance. Patient and surgeon perception of biceps muscle deformity including a Popeye sign were noted. Maximum isometric strength testing included elbow flexion in the neutral position (ie, hammer curl), elbow flexion in the supinated position (ie, traditional biceps curl), and forearm supination (rotation from neutral to a supinated position). Testing was performed using a handheld dynamometer (Commander Muscle Tester; Jtech Medical Industries) by a single tester for every participant to enhance reliability and validity of testing method.17
Patient strength was tested in the seated position with knees bent at 90° to minimize lower body forces exerted during testing. The patient’s arm was positioned at 90° to the table to isolate biceps strength. Biceps flexion strength in the neutral position was tested first followed by biceps flexion strength with the forearm in a supinated position and then forearm supination strength. In each test, the right arm was tested 3 times followed by testing on the left side 3 times. Patients were given 3 to 4 minutes of rest between strength testing positions.
After initial strength testing, patients performed biceps curls on their right side using a 10-lb weight to fatigue the biceps, and strength tests in each position (biceps flexion in neutral, biceps flexion in supinated position, and forearm supination) were repeated. Patients then performed biceps curls to fatigue the left side followed by strength testing of the left arm in each position. Each patient was tested in the same sequence regardless of hand dominance to maintain consistency of the exam.
Patients completed a written questionnaire including a quadruple visual analog scale (VAS); Disabilities of the Arm, Shoulder, and Hand (DASH); and American Shoulder and Elbow Surgeons score (ASES). Subjective deformity, pain, weakness, cramping, and demographic information were also collected.
Statistics
Statistical analysis included independent-samples t tests for comparison of group demographics (sex, age, follow-up-time) and questionnaire results (VAS, DASH, and ASES). Maximum strength testing was assessed using repeated-measures analysis of variance comparing operative versus nonoperative arm (treatment) before and after fatigue (time). Significance level was set at P < .05.
Results
Demographic information for each group is listed in Table 1. Patients were asked to report any additional surgeries on the affected shoulder since the surgery in question. There was no significant difference between reported additional surgeries between patients (tenodesis, 2/22; tenotomy, 4/20). Participation in sports, as measured by response to the DASH sport subscale, was not statistically different for the tenodesis or tenotomy groups (17/22 and 11/20, respectively).
TABLE 1.
Demographic Information of Study Participantsa
| Tenodesis Group (n = 22) | Tenotomy Group (n = 20) | P Value | |
|---|---|---|---|
| Sex, male:female, n | 15:7 | 16:4 | .397 |
| Age at surgery, y, mean ± SD | 42.2 ± 8.2 | 50.7 ± 4.2 | <.001 |
| Age at FU, y, mean (SD) | 45.4 ± 8.6 | 54.8 ± 4.4 | <.001 |
| FU time, y, mean (SD) | 2.7 ± 1.1 | 3.8 ± 1.9 | .032 |
| Concomitant procedures, n | 21 | 20 | |
| RCR | 9 | 8 | |
| RCR with SAD | 6 | 3 | |
| SAD | 0 | 2 | |
| Debridement | 5 | 6 | |
| Other | 1 | 1 |
aFU, follow-up; RCR, rotator cuff repair; SAD, subacromial decompression.
The presence of a Popeye deformity was not significantly different between groups. Both groups demonstrated no Popeye deformity at rest. Popeye with resistance was not significantly different between groups (4/22 tenodesis, 7/20 tenotomy; P = .226). Of all Popeye deformities, only 1 was present in a female, which represented 8% of the total female patient population of this study.
Strength Testing
In the tenodesis group, the difference in maximum elbow flexion strength in the neutral position between the operative and nonoperative arm (34.3 ± 16.6 lbs vs 34.8 ± 16.7 lbs, respectively) was not significantly different from the tenotomy group for each arm (36.6 ± 15.4 lbs vs 36.8 ± 16.8 lbs, respectively; P = .056). There was no difference in the rate of fatigue between the operative and nonoperative arm between surgery types (P > .05) (Figure 1).
Figure 1.
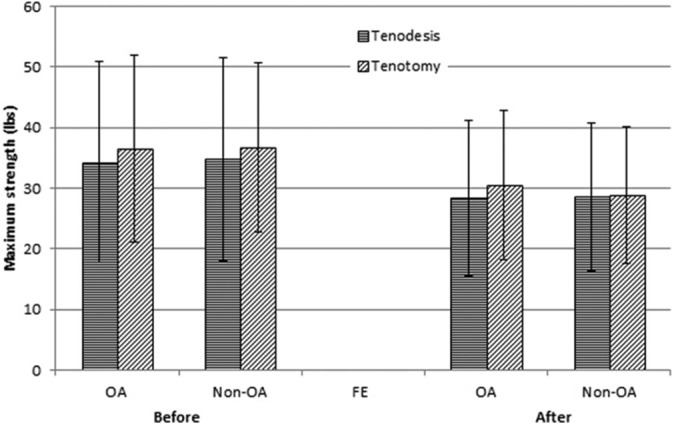
Maximum isometric strength of elbow supination in the neutral position for tenodesis and tenotomy before and after fatiguing exercise. FE, fatiguing exercise; non-OA, nonoperative arm; OA, operative arm.
Maximum isometric elbow flexion strength in the supinated position was significantly different from operative to nonoperative arm in both surgical groups (P < .05) (Figure 2). In the tenodesis group, elbow flexion strength in the supinated position between the operative and nonoperative arm (32.7 ± 15.3 lbs vs 34.4 ± 15.2 lbs, respectively) was not significantly different from the tenotomy group (36.1 ± 15.7 lbs vs 34.7 ± 14.4 lbs, respectively). There was no difference in fatigue rates between the operative and nonoperative arm between surgery types (P > .05) (Figure 2). Forearm supination maximal strength was not significantly different between groups before or after fatiguing exercise (P > .05) (Figure 3). Hand dominance did not influence the differences between the operative and nonoperative arms.
Figure 2.
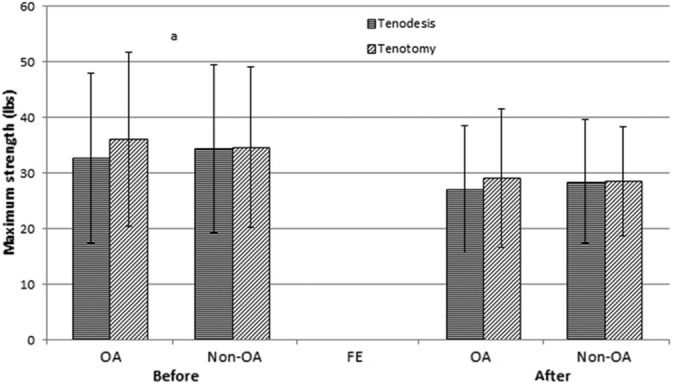
Maximum isometric strength of elbow supination in the supine position for tenodesis and tenotomy before and after fatiguing exercise. aSignificant difference between operative and nonoperative arm, P < .05. FE, fatiguing exercise; non-OA, nonoperative able arm; OA, operative arm.
Figure 3.
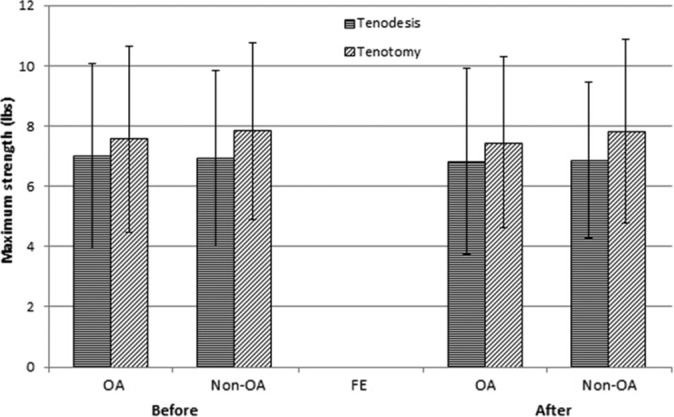
Maximum isometric strength of forearm supination for tenodesis and tenotomy before and after fatiguing exercise. FE, fatiguing exercise; non-OA, nonoperative able arm; OA, operative arm.
Questionnaire Results
The scores were lower in the tenodesis group for “pain level at its best” (VAS) compared with the tenotomy group, but this did not reach significance (P = .053) (Table 2). There were no significant differences in the DASH or ASES test score results between tenotomy and tenodesis groups.
TABLE 2.
VAS, ASES, and DASH Questionnaire Resultsa
| Tenodesis Group (n = 22) | Tenotomy Group (n = 20) | P Value | |
|---|---|---|---|
| VAS scoreb | |||
| Pain right now | 0.85 ± 1.6 | 1.1 ± 1.4 | .603 |
| Average pain | 0.90 ± 1.3 | 1.4 ± 1.8 | .333 |
| Pain at best | 0.15 ± 0.37 | 0.60 ± 0.94 | .053 |
| Pain at worst | 3.1 ± 2.5 | 3.7 ± 3.4 | .563 |
| ASES scorec | 85.2 ± 16.1 | 83.8 ± 21.4 | .812 |
| DASH score (total)d | 11.2 ± 11.6 | 13.9 ± 19.0 | .571 |
| Sport subscalee | 30.1 ± 31.7 (n = 17) | 18.8 ± 22.4 (n = 11) | .288 |
| Work subscalee | 12.8 ± 22.5 (n = 22) | 13.2 ± 27.7 (n = 18) | .959 |
| Pain at bicipital groove, n | 9 | 5 | |
| Patient complaints, n | |||
| Deformity | 5 | 5 | |
| Pain | 11 | 5 | |
| Weakness | 9 | 9 | |
| Cramping | 1 | 4 |
aValues are reported as mean ± SD unless otherwise indicated. ASES, American Shoulder and Elbow Surgeons score; DASH, Disabilities of the Arm, Shoulder, and Hand; VAS, visual analog scale.
bQuadruple scale asking to classify and score pain.
cMaximum score, 100.
dMaximum score, 100.12
eDASH Sport and Work subscales12 were reported for individuals who completed the questionnaire section. Maximum score for each, 100.
Discussion
The unsettled debate between biceps tenodesis and tenotomy is challenging to providers and patients. While this study does not attempt to resolve all questions, it does contribute to the decision making for younger patients (<55 years of age) in evaluating function for both elbow flexion and supination strength as well as perceived cosmetic deformity. The purpose of this study was to retrospectively analyze a group of similar patients treated by either biceps tenodesis or tenotomy and determine whether outcomes at longer than 1 year are different between groups. Our findings have demonstrated that there is little difference in either function or subjective outcomes in patients undergoing tenodesis or tenotomy of the biceps tendon.
One of the main strengths of this study is that we specifically included only patients younger than 55 years. The purpose was to target younger patients who would theoretically demonstrate a detectable clinical difference as they place greater demands on their bodies. Most studies have combined all ages in looking at outcomes and the differences between the 2 procedures.6,16,22,27 The majority of studies have failed to find a functional difference when directly comparing the 2 procedures.7,16,22,24 Hsu et al11 and Koh et al16 advocated the use of tenodesis in heavy laborers and patients younger than 50 years and tenotomy in an older, more sedentary population. Our findings demonstrated that DASH, VAS, and ASES scores were similar between tenotomy and tenodesis groups despite being a younger and generally more active population. Interestingly, the subjective findings, including cramping, deformity, and perceived weakness, were also similar in this active population. Concomitant procedures consisting of rotator cuff repair, subacromial decompression, and debridement were similar between groups, which is consistent with the current literature.2,22,27
Another strength of this study is that a single surgeon performed all operative procedures. This allowed minimization of surgical technique variations, as there are many ways to perform a biceps tenodesis. Many studies have compared pullout strength and mechanical properties for the different biceps tenodesis procedures, but this was not the aim of this study.14 Instead, our focus was to determine whether tenodesis in itself demonstrated superior outcomes as compared with tenotomy.
The long head of the biceps tendon has been shown to contribute to both elbow flexion and supination strength. This was observed in the study performed by Mariani et al,19 who compared elbow flexion and supination strength on proximal biceps tendon ruptures treated operatively and nonoperatively. They found a 21% decrease in supination strength and 8% decrease in flexion strength on the injured side as compared with the uninjured side in those treated nonoperatively. We attempted to isolate both functions of the biceps tendon with isometric testing through a handheld dynamometer.5 We found no significant difference in strength between the 3 measures. This is consistent with the findings of Shank et al,23 who found no difference in forearm supination or elbow flexion strength when using isokinetic testing. However, Koh et al16 demonstrated a 20% decrease in elbow flexion and supination power after tenotomy, as well as an increase in the incidence of biceps cramping pain. Our study evaluated the biceps not only at absolute strength but also endurance strength by fatiguing the biceps tendon and repeating the measures. Our results demonstrated no difference in endurance strength, which is consistent with the isometric findings of Kelly et al.13 Wittstein et al27 also found no difference in isokinetic endurance testing with elbow flexion and supination. However, they did find that the operative side peak supination torque was significantly decreased relative to the nonoperative side in the tenotomy group. In addition, others have cited hand dominance as a reason to perform a biceps tenodesis as it is thought that the loss in supination strength in a dominant arm would be affected. However, in our study hand dominance and the side that the operation was performed on did not affect outcome or apparent supination strength.
Limitations
There may be some limitation with our testing parameters with the handheld dynamometer. It has been validated as a way to test strength.5 In a recent systematic review, Stark et al25 found that strength assessment by handheld dynamometry correlated well with the gold standard isokinetic dynamometry. They concluded that considering the handheld dynamometer's ease of use, portability, cost, and compact size compared with isokinetic devices, this instrument can be regarded as a reliable and valid device for muscle strength assessment in a clinical setting.25 Biodex isokinetic testing was utilized in a recent study investigating bicep tenodesis versus tenotomy, and 31% of individuals contacted agreed to participate in the study.27 In our study, we were able to achieve a 51% rate of participation. We attribute this higher recruitment number, at least in part, to the ease of participation in the study through flexibility in location of testing with use of the portable handheld dynamometer.
The desire to avoid a Popeye deformity has been touted as a reason to perform a tenodesis over a tenotomy.23 In this study, the perceived Popeye deformity by the patient was not significantly different between the 2 groups. Five patients in each group felt that they had deformity of the biceps tendon. Perceived weakness was similar in each group, and this may reflect the concomitant rotator cuff pathology more than actual biceps weakness, as true weakness was not determined in testing. Cramping was noted to be more prevalent in the tenotomy group (4 vs 1), as expected. However, almost half of our patients in the tenodesis group reported pain at the bicipital groove as well as overall pain. This suggests that there may be some morbidity in performing a tenodesis at the bicipital groove. While no reoperations were performed in our study for the biceps tendon, biceps tenodesis has been reported to have a 15% reoperation rate.4
In looking at outcome measure scores, there may be some crossover effect between concomitant procedures that were performed and the biceps tenotomy versus tenodesis. It is possible that VAS, DASH, and ASES scores are unable to differentiate biceps pathology from other associated pathology, such as a rotator cuff tear. The concomitant procedures may have more of an effect on patient outcome than the actual biceps procedure. As there was no difference in the distribution of concomitant procedures, it follows that there was likely no difference between the 2 procedures.
Our inability to find an objective difference in this study may have been an effect of underpowering. This study had adequate power to detect a 20% difference in each strength measure between the 2 sample groups. To our knowledge, a clinically significant difference in each strength measure (biceps flexion in neutral position, biceps flexion in supinated position, and forearm supination) has not been defined in the literature.
Conclusion
This is one of the largest studies comparing biceps tenotomy versus tenodesis specific to a younger population. Both procedures result in high patient satisfaction and pain relief. Subjectively, the patients in our study had similar results with regard to perceived cramping, weakness, and deformity. Pain at the bicipital groove may be greater for those undergoing a subpectoral biceps tenodesis. More refined indications for one procedure over the other still remain elusive. The choice of biceps tenodesis versus tenotomy for the younger patient with biceps tendon pathology continues to be decided on through a dialogue between patient and surgeon. However, considerations for cost and rehabilitation time are measures that were not addressed in our study and may also play into the decision-making process in the future.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Ahmad CS, ElAttrache NS. Arthroscopic biceps tenodesis. Orthop Clin North Am. 2003;4:499–506. [DOI] [PubMed] [Google Scholar]
- 2. Ahrens PM, Boileau P. The long head of biceps and associated tendinopathy. J Bone Joint Surg Br. 2007;89:1001–1009. [DOI] [PubMed] [Google Scholar]
- 3. Barber A, Field LD, Ryu R. Biceps tendon and superior labrum injuries: decision making. J Bone Joint Surg Am. 2007;89:1844–1855. [DOI] [PubMed] [Google Scholar]
- 4. Becker DA, Cofield RH. Tenodesis of the long head of the biceps brachii for chronic bicipital tendinitis. Long-term results. J Bone Joint Surg Am. 1989;71:376–381. [PubMed] [Google Scholar]
- 5. Bohannon RW. Test-retest reliability of hand-held dynamometry during a single session of strength assessment. Phys Ther. 1986;66:206–209. [DOI] [PubMed] [Google Scholar]
- 6. Boileau P, Baque F, Valerio L, Ahrens PM, Chuinard C, Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. J Bone Joint Surg Am. 2007;89:747–757. [DOI] [PubMed] [Google Scholar]
- 7. Edwards TB, Walch G, Sirveaux F, et al. Repair of tears of the subscapularis. Surgical technique. J Bone Joint Surg Am. 2006;88 (suppl 1):1–10. [DOI] [PubMed] [Google Scholar]
- 8. Franceschi F, Longo U, Ruzzini L, Papalia R, Rizzello G, Denaro V. To detach the long head of the biceps tendon after tenodesis or not: outcome analysis at the 4-year follow-up of two different techniques. Int Orthop. 2007;31:537–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frost A, Zafar MS, Maffulli N. Tenotomy versus tenodesis in the management of pathologic lesions of the tendon of the long head of the biceps brachii. Am J Sport Med. 2009;37:828–833. [DOI] [PubMed] [Google Scholar]
- 10. Gill TJ, McIrvin E, Mair SD, Hawkins RJ. Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10:247–249. [DOI] [PubMed] [Google Scholar]
- 11. Hsu AR, Ghodadra NS, Provencher CDRMT, Lewis PB, Bach BR. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326–332. [DOI] [PubMed] [Google Scholar]
- 12. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602–608. [DOI] [PubMed] [Google Scholar]
- 13. Kelly AM, Drakos MC, Fealy S, Taylor SA, O’Brien SJ. Arthroscopic release of the long head of the biceps tendon. Am J Sport Med. 2005;33:208–213. [DOI] [PubMed] [Google Scholar]
- 14. Kim S-H, Yoo JC. Arthroscopic biceps tenodesis using interference screw: end-tunnel technique. Arthroscopy. 2005;21:1405. [DOI] [PubMed] [Google Scholar]
- 15. Klinger KM, Spahn G, Baums MH, Steckel H. Arthroscopic debridement of irreparable massive rotator cuff tears: a comparison of debridement alone and combined procedure with biceps tenotomy. Acta Chir Belg. 2005;105:297–301. [DOI] [PubMed] [Google Scholar]
- 16. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears. Am J Sport Med. 2010;38:1584–1590. [DOI] [PubMed] [Google Scholar]
- 17. Kolber MJ, Cleland JA. Strength testing using hand-held dynamometry. Phys Ther Rev. 2005;10:99–112. [Google Scholar]
- 18. Lam F, Mok D. Treatment of the painful biceps tendon—tenotomy or tenodesis? Curr Orthopaed. 2006;20:370–375. [Google Scholar]
- 19. Mariani EM, Cofield RH, Askew LJ, Li G, Chao EY. Rupture of the tendon of the long head of the biceps brachii surgical versus nonsurgical treatment. Clin Orthop Relat Res. 1988;(228):233–239. [PubMed] [Google Scholar]
- 20. Maynou C, Mehdi N, Cassagnaud X, Audebert S, Mestdagh H. Clinical results of arthroscopic tenotomy of the long head of the biceps brachii in full thickness tears of the rotator cuff without repair: 40 cases [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:300–306. [DOI] [PubMed] [Google Scholar]
- 21. Murthi AM, Vosburgh CL, Neviaser TJ. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–385. [DOI] [PubMed] [Google Scholar]
- 22. Osbahr DC, Diamond AB, Speer KP. The cosmetic appearance of the biceps muscle after long-head tenotomy versus tenodesis. Arthroscopy. 2002;18:483–487. [DOI] [PubMed] [Google Scholar]
- 23. Shank J, Singleton SB, Braun S, et al. A comparison of forearm supination and elbow flexion strength in patients with long head of the biceps tenotomy or tenodesis. Arthroscopy. 2011;27:9–16. [DOI] [PubMed] [Google Scholar]
- 24. Slenker NR, Lawson K, Ciccotti MG, Dodson CC, Cohen SB. Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy. 2012;28:576–582. [DOI] [PubMed] [Google Scholar]
- 25. Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. Phys Med Rehabil. 2011;3:472–479. [DOI] [PubMed] [Google Scholar]
- 26. Walch G, Edwards TB, Boulahia A, Nové-Josserand L, Neyton L, Szabo I. Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elbow Surg. 2005;14:238–246. [DOI] [PubMed] [Google Scholar]
- 27. Wittstein JR, Queen R, Abbey A, Toth A, Moorman CT. Isokinetic strength, endurance, and subjective outcomes after biceps tenotomy versus tenodesis. Am J Sport Med. 2011;39:857–865. [DOI] [PubMed] [Google Scholar]


