Abstract
Background:
Femoroacetabular impingement (FAI) is a common cause of hip pain and dysfunction among athletes. Although arthroscopic surgery is an established treatment option for FAI, there are few studies reporting detailed outcomes using validated outcome measurements specifically designed for young and active athletes.
Purpose:
To report outcomes 1 year after arthroscopic treatment of FAI in top-level athletes using validated outcome measurements adapted for a young and active population.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 85 top-level athletes (68 males, 17 females) with a mean (±SD) age of 25 ± 5 years underwent arthroscopic surgery for FAI. All athletes who reported Hip Sports Activity Scale (HSAS) levels 7 or 8 (range, 0-8) prior to symptom onset were included. The cohort was prospectively evaluated using online web-based validated health-related patient-reported outcomes measures (HR-PROMs), including the short version of the International Hip Outcome Tool (iHOT-12), the Copenhagen Hip and Groin Outcome Score (HAGOS; 6 subscales), the EuroQOL 5 dimensions questionnaire (EQ-5D; 2 subscales), the Hip Sports Activity Scale (HSAS) for physical activity level, and a visual analog scale (VAS) for overall hip function. Furthermore, patients reported their overall satisfaction with treatment.
Results:
The mean follow-up time was 12.3 ± 0.6 months. Preoperative scores compared with those obtained at the 12-month follow-up revealed statistically and clinically significant improvements (P < .0001) for all measured outcomes: iHOT-12 (42 vs 73), VAS for global hip function (52 vs 77), HSAS (4.3 vs 5.7), EQ-5D index (0.60 vs 0.83), EQ-VAS (68 vs 82), and HAGOS subscales (60 vs 83, 50 vs 73, 66 vs 86, 39 vs 75, 27 vs 70, and 34 vs 67). At the 12-month follow-up, 79 athletes (93%) reported that they were satisfied with the outcome of surgery. At follow-up, 62 athletes (73%) had returned to competitive sports (HSAS levels 5-8) and 44 (52%) to their previous HSAS level of activity (HSAS level 7 or 8). Twenty-three athletes (27%) did not return to competitive sports (HSAS level ≤4). Significantly lower levels of return to sports were seen with longer symptom duration (P < .05).
Conclusion:
Twelve months after surgery, arthroscopic treatment for FAI in top-level athletes resulted in statistically and clinically significant improvements at the group level in all outcome parameters for pain, symptoms, function, physical activity level, quality of life, and general health. One year after surgery, approximately 3 of 4 top-level athletes had returned to sports.
Keywords: hip, hip arthroscopy, femoroacetabular impingement, surgery, sports
Femoroacetabular impingement (FAI) is common among athletes.11,31,32 High physical activity in adolescents has been indicated as a causal factor of FAI.1,3,20 Sports that include repetitive hip flexion, such as ice hockey and soccer, may cause FAI and chondrolabral damage, with symptoms in the hip and groin area.6,25
Arthroscopic treatment is an established treatment method for athletes with symptoms of FAI.2,8,17 However, only a few studies have reported the outcome of arthroscopic treatment of FAI in top-level athletes.19,21 Moreover, new health-related patient-reported outcome measurements (HR-PROMs) directed specifically at the younger and more active population have been developed.7,29 Only a limited number of studies use validated outcome measurements suitable for a young and active population.2
In a recent systematic review of the treatment of FAI in athletes by Alradwan et al,2 7 studies of arthroscopic treatment were identified. These studies reported consistently good results and a high degree of return to sports after arthroscopic treatment for FAI, with a return rate of 88% to previous levels of competition. The number of athletes included in the studies varied from 16 to 200. The main PROMs were the modified Harris Hip Score (mHHS) in 5 studies, the Hip Outcome Score (HOS) in 2 studies, and the Non-Arthritic Hip Score (NAHS) in 1 study. One study reported only return to sports.
In a recent systematic review by Harris et al8 on the efficacy of surgery for femoroacetabular impingement, the most commonly used scores in the included studies were the mHHS, the modified NAHS (mNAHS), and the HOS. Some of these scores were developed for use in a more senior patient category, and their validity for use on a young and very active population such as athletes can therefore be questioned. In recent years, new outcome measurements have been developed and validated for use in young, active patients; they include the International Hip Outcome Tool (iHOT)7 and the Copenhagen Hip and Groin Outcome Score (HAGOS).29 The Hip Sports Activity Scale (HSAS)16 was adapted after the Tegner activity scale27 and modified to measure physical activity in a population with hip disorders.
Although there have been a few prospective studies, there is a need for more scientific evidence to describe the outcome after the arthroscopic treatment of FAI.2,8,17 In particular, the outcome is not well known after the treatment of top-level athletes.2 Top-level athletes also have high demands in terms of physical function, and it is therefore especially important to study the outcome for this patient category.
The purpose of this study was to report outcomes 1 year after arthroscopic treatment of FAI in top-level athletes using validated outcome measurements adapted for a young and active population.
Materials and Methods
Between 2011 and 2012, a total of 85 top-level athletes (68 males, 17 females) who underwent arthroscopic surgery for FAI (total hips, 115) were followed prospectively for 1 year. All athletes who met inclusion criteria during the study period were included prospectively. The mean age (±SD) of the study participants was 25 ± 5 years.
The inclusion criteria were HSAS activity level 7 or 8 (range, 0-8) prior to symptom onset and age <40 years. HSAS level 7 corresponds to alpine skiing, skating, and dancing at a national elite level or soccer, ice hockey, tennis, martial arts, and track and field sports at a subelite level, while level 8 corresponds to sports such as soccer, martial arts, tennis, and track and field at a national and international top level. Patients who had undergone hip surgery prior to the index operation were excluded.
All hip arthroscopies were performed at 2 centers by 3 surgeons. For further patient demographics, see Table 1. Ethical approval for the study was granted by the regional ethical review board in Gothenburg, Sweden (registration number 071-12). Indications for surgery were an established diagnosis of FAI and failed nonsurgical treatment. The diagnosis of FAI was made from patient history, physical examination, and radiological findings consistent with FAI of cam-type, pincer-type, or mixed. Perioperative data were registered at the time of surgery. A description of cartilage status was made according to the classification by Konan et al10 (Table 2 and Figure 1). All procedures were performed in an outpatient setting.
TABLE 1.
Patient Demographics and Perioperative Dataa
| Total number of patients | 85 |
| Total number of hips | 115 |
| Operated side (right/left/bilateral), % | 33/30/37 |
| Sex (male/female), % | 82/18 |
| Symptom duration, mo, median/range/IQR | 24/2-240/14.0-46.5 |
| Outpatient surgery, % | 100 |
| Age, y, mean ± SD | 25 ± 5 |
| Operative time, min, mean ± SD | 74 ± 15 |
| Traction time, min, mean ± SD | 9 ± 8 |
| Joint could not be distracted, % | 8 |
aIQR, interquartile range.
TABLE 2.
Classification System for Acetabular Chondral Lesionsa
| Cartilage Damage Classification | Description |
|---|---|
| 0 | Normal cartilage |
| 1 | Wave sign |
| 2 | Cleavage tear between labrum and articular cartilage |
| 3 | Delamination of articular cartilage |
| 4 | Exposed bone in the acetabulum |
| A | <One-third of the distance from the acetabular rim to the cotyloid fossa |
| B | One-third to two-thirds of distance above |
| C | >Two-thirds of distance above |
aAccording to Konan et al.10
Figure 1.
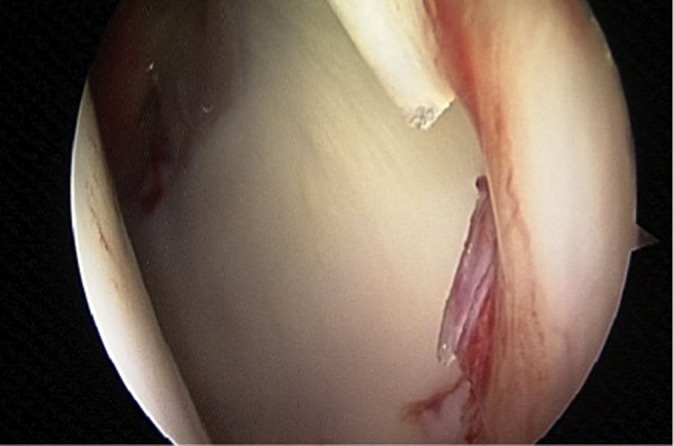
Intra-articular view. Chondrolabral damage classified as 3a according to the classification by Konan et al.10
Patient-Reported Outcomes, Physical Activity, and Follow-up
All the athletes completed self-administered, web-based HR-PROMs, including the iHOT-12 (the short version of the iHOT), the HAGOS (6 subscales), the HSAS, a visual analog scale (VAS) for overall hip function, and a standardized instrument, the EuroQOL 5 dimensions questionnaire (EQ-5D, 2 subscales), for use as a measurement of health outcome.7,16,22,29 Furthermore, the athletes reported whether they were satisfied with the surgery. All the scores have previously been validated and culturally adapted to Swedish.28 The questionnaires were completed preoperatively and 12 months postoperatively.
The athletes were divided into 3 outcome groups according to HSAS level at the 12-month follow-up: 7-8 (return to previous level of sporting activity), 5-6 (return to competitive sports), and 1-4 (no return to competitive sports).
Surgical Technique
The preferred arthroscopy procedure, previously described by Sansone et al,24 utilizes an anterolateral portal and a midanterior portal with the patient in a supine position. Axial traction was used to view the central compartment for diagnostics, free-body removal, or microfracture.
Access to the peripheral compartment was achieved through a ligament-sparing capsulotomy, which was parallel to the fibers of the iliofemoral ligament and had a minimal component of transverse cut.14 By minimizing the damage to the ligaments and capsule, the risk of an iatrogenic increase in laxity of the hip can be reduced.15,23 Acetabular overcoverage (pincer) was removed using an “over-the-top” technique, where the bur was placed in the perilabral sulcus and the resection of the acetabular edge was made with the labrum in situ. In patients where small rim resections were performed, the labrum was left in situ. With larger resections, the labrum was reattached using suture anchors. A meticulous cam resection, spanning between far lateral, far medial/caudal, and posterior, as well as intraoperative dynamic assessment of impingement, was made to avoid residual impingement (Figure 2, A and B). In cases with a pistol grip deformity, resection was also made posterior and cranial to the lateral retinacular fold to correct posterior impingement. Care was always taken to preserve the lateral retinacular vessels.
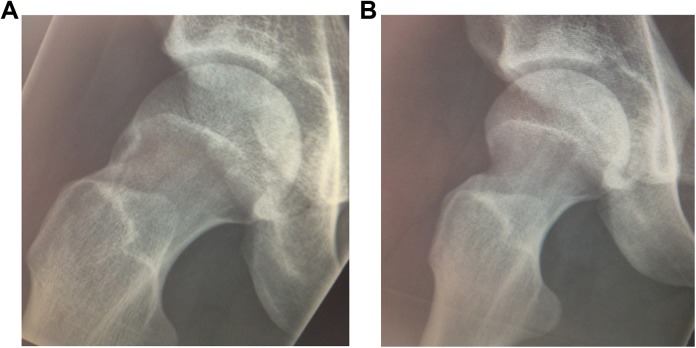
Figure 2.
(A) Preoperative image of cam deformity. (B) Postoperative image after cam resection.
Postoperatively, patients were allowed free range of motion (ROM) and full weightbearing during the early rehabilitation phases. Crutches were recommended for outdoor and longer ambulation for 1 month. Physical therapy was started directly postoperatively, with a protocol of rehabilitation exercises for ROM, strength, endurance, balance, and coordination. The intensity of the protocol was gradually increased, as tolerated by the patient, and carefully monitored by the physiotherapist. Patients were prescribed nonsteroidal anti-inflammatory medication, such as 50 mg × 3 of diclofenac for 1 month postoperatively, to minimize the risk of heterotopic ossification. Antibiotic prophylaxis was not routinely used.
We advocate “à la carte” arthroscopic hip surgery, that is, individualized patient care. This calls for high diagnostic accuracy. The identification of the cause of pain is demanding and warrants a careful evaluation of patient history, clinical findings, radiology, and intraoperative findings.26,30
Statistical Analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS, version 20; IBM Corp). Descriptive statistics were used for patient demographics. Descriptive data were reported as the mean, median, SD, and range. The Wilcoxon signed rank test was used to compare all HR-PROM values used preoperatively with those obtained at follow-up. The data were not normally distributed, and nonparametric statistical testing was therefore employed. The level of significance was set at P < .05.
Results
Of the included procedures, 54 were isolated cam resections and 49 were cam and pincer combined procedures. The labrum was sutured in 8 hips, and microfracture was performed in 2 hips (Table 3).
TABLE 3.
Arthroscopic Procedures Performed (N = 85 Patients [115 Hips])
| Surgical Procedure | No. of Hips |
|---|---|
| Cam | 55 |
| Cam + pincer (combined) | 49 |
| Labral suture | 8 |
| Microfracture | 2 |
| Labral resection | 1 |
The average time to follow-up was 12.3 ± 0.6 months. The reported average time of symptom duration prior to surgery was 2.8 ± 3.4 years.
The most common sporting activity was soccer, followed by ice hockey (Table 4).
TABLE 4.
Number of Patients Participating in Various Sport Activities Before Symptom Onset
| Sports Activity | No. of Patients |
|---|---|
| Soccer | 50 |
| Hockey | 15 |
| Martial arts | 3 |
| Handball | 3 |
| Figure skating | 2 |
| Floorball | 2 |
| Bandy | 2 |
| Biathlon, badminton, track and field sports, dancing, American football, basketball, scooter-cross, ballet | 8 |
A comparison of preoperative scores with those obtained at the 12-month follow-up revealed statistically and clinically significant improvements (P < .0001) for all measured outcomes: iHOT-12 (42 vs 73), VAS for global hip function (52 vs 77), HSAS (4.3 vs 5.7), EQ-5D index (0.60 vs 0.83), EQ-VAS (68 vs 82), and HAGOS different subscales (60 vs 83, 50 vs 73, 66 vs 86, 39 vs 75, 27 vs 70, and 34 vs 67) (Table 5). Figure 3 shows the change in the iHOT-12 from preoperatively to postoperatively at the individual level.
TABLE 5.
Outcome Scores for the Entire Group (N = 85) Preoperatively and at 12-Month Follow-upa
| Outcome Measure | Outcome Score | P Value | ||
|---|---|---|---|---|
| Preoperative | 12-Month Follow-up | ▵ | ||
| iHOT-12 | 42 ± 18 | 73 ± 24 | 31 | <.0001 |
| EQ-5D | 0.60 ± 0.27 | 0.83 ± 0.19 | 0.23 | <.0001 |
| EQ-VAS | 68 ± 19 | 82 ± 15 | 14 | <.0001 |
| HAGOS subscale | ||||
| Pain | 60 ± 18 | 83 ± 17 | 23 | <.0001 |
| Symptoms | 50 ± 20 | 73 ± 19 | 23 | <.0001 |
| Daily activity | 66 ± 22 | 86 ± 17 | 20 | <.0001 |
| Sports | 39 ± 21 | 75 ± 23 | 36 | <.0001 |
| Physical activity | 27 ± 28 | 70 ± 30 | 43 | <.0001 |
| Quality of life | 34 ± 21 | 67 ± 26 | 33 | <.0001 |
| VAS–overall hip function | 52 ± 21 | 77 ± 21 | 25 | <.0001 |
| HSAS | 4.3 ± 2.5 | 5.7 ± 2.2 | 1.4 | <.0001 |
| Satisfied with surgery, n (%) | NA | 79 (93) | NA | NA |
aValues are reported as mean ± SD unless otherwise indicated. EQ-5D, EuroQOL 5 dimensions; HAGOS, Copenhagen Hip and Groin Outcome Score; HSAS, Hip Sports Activity Scale; iHOT-12, International Hip Outcome Tool–short version; NA, not applicable; VAS, visual analog scale.
Figure 3.
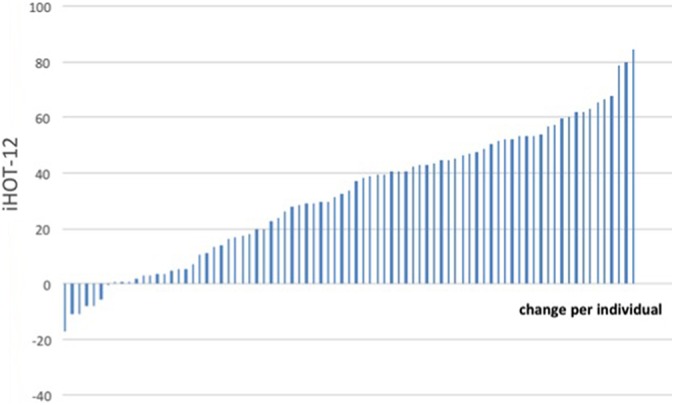
Change per individual on the International Hip Outcome Tool–short version (iHOT-12) between preoperative and 12-month follow-up.
The mean HSAS level improved from 4.3 ± 2.5 preoperatively to 5.7 ± 2.2 at the 12-month follow-up. At follow-up, 62 athletes (73%) had returned to competitive sports, defined as HSAS levels 5 through 8, of whom 44 (52%) returned to their previous HSAS level of activity (HSAS level 7 or 8). Twenty-three athletes (27%) did not return to competitive sports (HSAS level ≤4).
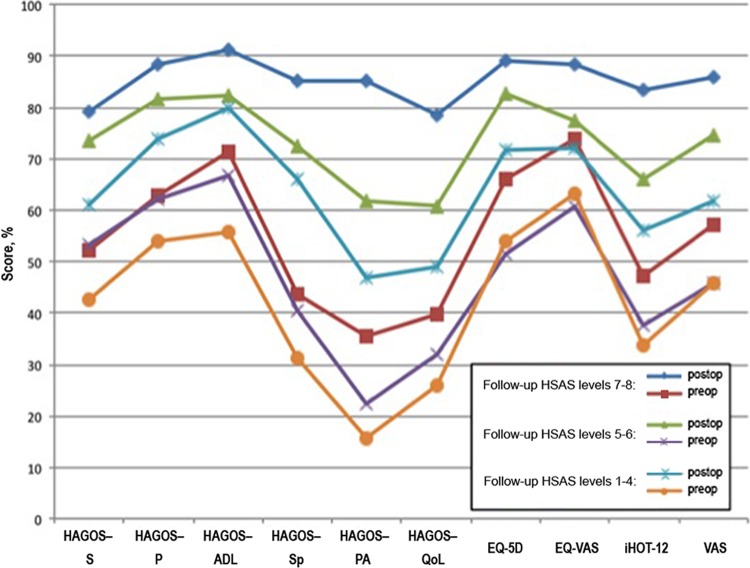
There were significant differences in all follow-up HSAS scores between subgroups (HSAS levels 7-8, 5-6, and 1-4) between pre- and postoperative measurements (Figure 4).
Figure 4.
Pre- and postoperative HAGOS, iHOT12, EQ-5D, and VAS–hip function scores for the 3 subgroups of athletes with follow-up HSAS levels 7-8, 5-6, and 1-4. ADL, activities of daily living; EQ-5D, EuroQOL 5 dimensions questionnaire; HAGOS, Copenhagen Hip and Groin Outcome Score; HSAS, Hip Sports Activity Scale; iHOT-12, International Hip Outcome Tool–short version; P, pain; PA, physical activity; QoL, hip-related quality of life; S, symptoms; Sp, sports; VAS, visual analog scale.
There was a significantly (P < .05) higher return to sports among athletes with short symptom duration (<12 months; 87%) compared with athletes with longer symptom duration (>12 months; 61%). The corresponding values for returning to the previous level of physical activity were 74% and 64%, respectively (P < .05).
Three reoperations (4%) were performed during the first year after the index surgery. The reasons for reoperation were persistent impingement (n = 2) and adhesions (n = 1).
Seventy-nine (93%) of 85 athletes reported that they were satisfied with their outcome of surgery. One of the 6 unsatisfied patients had undergone reoperation.
There were reports of chondral damage in 71 of 115 hips (62%). The incidence and distribution of chondral damage are shown in Table 6.
TABLE 6.
Hips With Cartilage Damage (N = 115 Hips)
| Cartilage Damage Classificationa | n (%) |
|---|---|
| 0 | 32 (27.8) |
| 1a | 6 (5.2) |
| 1b | 0 (0) |
| 1c | 0 (0) |
| 2 | 37 (32.2) |
| 3a | 21 (18.2) |
| 3b | 1 (0.8) |
| 3c | 0 (0) |
| 4a | 4 (3.4) |
| 4b | 2 (1.7) |
| 4c | 0 (0) |
| Missing values | 3 (2.6) |
| Joint not distractible | 9 (7.8) |
| Total | 115 (100) |
aAccording to the classification system of acetabular chondral lesions by Konan et al.10
Discussion
The most important finding in the present study was that the outcome after the arthroscopic treatment of FAI in top-level athletes was favorable, with statistically and clinically significant improvements in all outcome measurements. Despite long-standing hip and/or groin pain, 1 in 2 top-level athletes was able to return within 1 year after surgery to the same sport and the same level as before symptom onset.
Several studies of the outcome of the arthroscopic treatment of FAI in athletes have revealed significant improvements in terms of HR-PROMs at follow-up.2,8,17 In the review by Alradwan et al,2 5 studies used the mHHS, and the mean improvement was 20 points (95% CI, 18-23). The limitations of these studies were small cohorts, retrospective design, selection bias, and older outcome measurements with low validity.
Nho et al18 reported significant improvements after the arthroscopic treatment of FAI in 33 athletes with a minimum of 1 year of follow-up. The mHHS and HOS (20- and 12-point increase, respectively) were used as outcome measurements. They reported a 73% return to sports at the 2-year follow-up. Malviya et al13 reported significant improvements after the arthroscopic treatment of FAI in 80 athletes using the NAHS and mHHS. The same group also found a high (82%) return to previous levels of activity 1 year postoperatively in a study of 80 patients.12 Philippon et al19 reported a high level of return to professional sports (78%) in 45 athletes treated arthroscopically for FAI, with a mean follow-up of 1.6 years. Brunner et al4 reported significant improvements in a group of recreational athletes measured by the NAHS and VAS (31 and 4, respectively). In this group, 69% achieved a full return at the 2.4-year follow-up, while an additional 13% returned to a lower level. Byrd and Jones5 reported prospectively on 200 athletes with a minimum follow-up of 12 months. A significant improvement in terms of functional outcome was reported using the mHHS. Ninety percent of these athletes returned to sports. Taken together, it appears that previous studies on arthroscopic treatment of FAI in athletes show favorable results.
The magnitude of improvement in the present study is consistent with the improvements reported in other studies of the outcome of the arthroscopic treatment of FAI.8 However, the same outcome measurements were not used. In the present study, 73% returned to sports, whereas 52% returned at the same activity level. Previous studies present levels of return to sports between 69% and 90%.12 However, return to sports is often not clearly defined in these studies. Only 1 study reports a clear definition.4 One other study retrieved the information at follow-up from medical records, and the other 3 have no clear definition. Return to sports could therefore be the subject of bias. More careful and uniform definitions of return to sports are therefore warranted in future studies. In the present study, we found a significantly higher level of activity postoperatively in athletes with shorter (<1 year) symptom duration. Although susceptible to bias, this could mean that symptom duration might be regarded as a prognostic factor for outcome. Future analyses of predictors of both positive and negative outcomes would therefore be valuable.
The multitude and type of outcome measurements is to be considered as a major strength in the present study. The iHOT-12, HAGOS, and HSAS are modern, validated scores developed to study this young and active patient category. The EQ-5D is a valid and reliable quality-of-life score that is commonly used. The present study is thus an improvement compared with older studies that used few, nonvalidated scores developed mainly for osteoarthritis patients, such as the Harris Hip Score. Furthermore, the present study is one of the first publications to use the iHOT-12, HSAS, and HAGOS scores as outcome measurements. It would be valuable if more studies used the same outcome measurements in similar study populations to be able to compare results.
The iHOT-12 was chosen instead of the iHOT-33 to limit the size of the complete protocol presented to the athletes. The iHOT-33 is developed for research and may therefore have been better suited, but the size of the complete protocol might then influence patient compliance. The iHOT-12 has been shown to be valid, reliable, and responsive and to have characteristics that are very similar to the originally validated 33-item questionnaire.7
In the present study, significant (P < .0001) and clinically relevant improvements were found in all outcome measurements used. Some preoperative values, such as the iHOT-12, HAGOS sports, and HAGOS physical activity, are low, reflecting the major symptoms and disabilities in the studied cohort preoperatively.
Six (7%) athletes were not satisfied with the outcome of surgery and reported fair or poor functional outcomes. The main causes of failure were considered to be persistent back pain in 2 cases, persistent pubalgia in 1 case, severe general joint hyperlaxity with possible hip instability in 1 case, and severe cartilage damage in 1 case. The last nonsatisfied patient was, however, able to return to the same level of sports. In the present study, long symptom duration was a factor contributing to inferior outcome.
We consider the measured mean changes in the HSAS (from 4.3 ± 2.5 to 5.7 ± 2.2) to be clinically relevant.
The fact that patients on some occasions reduce their activity level despite satisfaction with the surgical results imposes a risk of bias. This reduction in physical activity level could be due to social or other reasons, especially in a group with long symptom duration, as in the present study. Moreover, the development of substantial cartilage damage, seen in about 1 in 4 athletes, with cartilage damage grade 3 to 4 in the present study, could inhibit the return to previous levels of physical activity. Furthermore, there might be a recall bias of the HSAS level before symptom onset.
The Swedish translated and culturally adapted version of the HSAS score is shown in Table 7.
TABLE 7.
Hip Sports Activity Scale (HSAS) Activity Score, English Versiona
| Please mark from the following list your current highest level of sports or recreational activity: | |
| Level | |
| 8 | Competitive sports (elite level): Soccer, ice hockey, field hockey, American football/rugby, martial arts, tennis, track and field, indoor sports,b beach volleyball, lacrosse, baseball/softball |
| 7 | Competitive sports (elite level): Downhill skiing, snowboarding |
| Competitive sports (minor leagues/collegiate): Soccer, ice hockey, field hockey, American football/rugby, martial arts, tennis, track and field, indoor sports,b beach volleyball, lacrosse, baseball/softball | |
| 6 | Competitive sports (elite level): Golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing/biathlon, horseback riding, cricket |
| Competitive sports (minor leagues/collegiate): Downhill skiing, snowboarding | |
| 5 | Competitive sports (minor leagues/collegiate): Golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing/biathlon, horseback riding, cricket |
| 4 | Recreational sports: Tennis, downhill skiing, snowboarding, indoor sports,b baseball/softball |
| 3 | Recreational sports: Aerobics, jogging, lower extremity weightlifting, horseback riding, cricket |
| 2 | Recreational sports: Golf, bicycle riding, mountain biking, swimming, rowing, cross-country skiing/biathlon, dancing, inline skating |
| 1 | Recreational sports: Swimming, cycling, hiking, Nordic walking (quick walking with ski poles) |
| 0 | No recreational or competitive sports |
| Please indicate your preferred sport: | |
aFrom Naal et al.16
bIndoor sports: basketball, squash, racquetball, handball, badminton, volleyball.
A subgroup analysis showed that those who returned to HSAS levels 7 to 8 had higher baseline values for all scores compared with those who returned to HSAS levels 5 to 6 and 1 through 4, in that order (see Figure 2). All groups improved, but this suggests that the more symptoms the patients have preoperatively, the smaller the probability of a return to higher levels of sports. This could be due to cartilage damage, osteoarthritis, or other factors. This is further emphasized by the finding in the present study that longer symptom duration is associated with a significantly lower return to sports.
For the iHOT-12 and HAGOS scores, the smallest detectable changes have been found to be 3.6 and 2.2, respectively, in this group of patients. Moreover, minimally important changes have been shown to be 8.9 for the iHOT-12 and 9 to 17 for the HAGOS subscales.9,28 Since the improvements shown in this study exceed these values, they mirror true changes in perceived pain and function in terms of these 2 HR-PROMs.
It is difficult to compare these results with other studies, since, to our knowledge, there are no publications to date that use the same outcome measurements.
The nonrandomized study design, lack of control group, and short time to follow-up are limitations in the present study. On the other hand, prospective register studies describe the actual outcome without selection bias, which could increase the external validity of the results.
All athletes that reported HSAS level 7 or 8 prior to symptom debut were included, and symptom duration before surgery was reported up to 20 years in the present study. This fact further underlines the strength of the finding that 52% of athletes returned to the level of sports activity they had had prior to symptom onset.
Conclusion
Twelve months after surgery, arthroscopic treatment for FAI in top-level athletes resulted in statistically significant and clinically relevant improvements at group level in all outcomes for pain, symptoms, function, physical activity level, quality of life, and general health. One year after surgery, approximately 3 of 4 top-level athletes had returned to sports.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Agricola R, Bessems JH, Ginai AZ, et al. The development of cam-type deformity in adolescent and young male soccer players. Am J Sports Med. 2012;40:1099–1106. [DOI] [PubMed] [Google Scholar]
- 2. Alradwan H, Philippon MJ, Farrokhyar F, et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy. 2012;28:1567–1576. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Lynch EB, Sibilsky Enselman ER, et al. Elevation in circulating biomarkers of cartilage damage and inflammation in athletes with femoroacetabular impingement. Am J Sports Med. 2013;41:2585–2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Brunner A, Horisberger M, Herzog RF. Sports and recreation activity of patients with femoroacetabular impingement before and after arthroscopic osteoplasty. Am J Sports Med. 2009;37:917–922. [DOI] [PubMed] [Google Scholar]
- 5. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39 (suppl):7S–13S. [DOI] [PubMed] [Google Scholar]
- 6. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Griffin DR, Parsons N, Mohtadi NG, Safran MR. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28:611–616. [DOI] [PubMed] [Google Scholar]
- 8. Harris JD, Erickson BJ, Bush-Joseph CA, Nho SJ. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med. 2013;6:207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jonasson P, Baranto A, Karlsson J, et al. A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement: cross-cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg Sports Traumatol Arthrosc. 2014;22:826–834. [DOI] [PubMed] [Google Scholar]
- 10. Konan S, Rayan F, Meermans G, Witt J, Haddad FS. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br. 2011;93:332–336. [DOI] [PubMed] [Google Scholar]
- 11. Larson CM, Sikka RS, Sardelli MC, et al. Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate National Football League prospects. Arthroscopy. 2013;29:405–410. [DOI] [PubMed] [Google Scholar]
- 12. Malviya A, Paliobeis CP, Villar RN. Do professional athletes perform better than recreational athletes after arthroscopy for femoroacetabular impingement? Clin Orthop Relat Res. 2013;471:2477–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Malviya A, Stafford GH, Villar RN. Is hip arthroscopy for femoroacetabular impingement only for athletes? Br J Sports Med. 2012;46:1016–1018. [DOI] [PubMed] [Google Scholar]
- 14. Martin HD, Savage A, Braly BA, Palmer IJ, Beall DP, Kelly B. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24:188–195. [DOI] [PubMed] [Google Scholar]
- 15. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. [DOI] [PubMed] [Google Scholar]
- 16. Naal FD, Miozzari HH, Kelly BT, Magennis EM, Leunig M, Noetzli HP. The Hip Sports Activity Scale (HSAS) for patients with femoroacetabular impingement. Hip Int. 2013;23:204–211. [DOI] [PubMed] [Google Scholar]
- 17. Ng VY, Arora N, Best TM, Pan X, Ellis TJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med. 2010;38:2337–2345. [DOI] [PubMed] [Google Scholar]
- 18. Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39 (suppl):14S–19S. [DOI] [PubMed] [Google Scholar]
- 19. Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–1580. [DOI] [PubMed] [Google Scholar]
- 21. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38:99–104. [DOI] [PubMed] [Google Scholar]
- 22. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33:337–343. [DOI] [PubMed] [Google Scholar]
- 23. Sansone M, Ahlden M, Jonasson P, Sward L, Eriksson T, Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013;21:420–423. [DOI] [PubMed] [Google Scholar]
- 24. Sansone M, Ahlden M, Jonasson P, et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg Sports Traumatol Arthrosc. 2014;22:774–780. [DOI] [PubMed] [Google Scholar]
- 25. Siebenrock KA, Ferner F, Noble PC, Santore RF, Werlen S, Mamisch TC. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res. 2011;469:3229–3240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Silvis ML, Mosher TJ, Smetana BS, et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. 2011;39:715–721. [DOI] [PubMed] [Google Scholar]
- 27. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 28. Thomee R, Jonasson P, Thorborg K, et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2014;22:835–842. [DOI] [PubMed] [Google Scholar]
- 29. Thorborg K, Holmich P, Christensen R, Petersen J, Roos EM. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med. 2011;45:478–491. [DOI] [PubMed] [Google Scholar]
- 30. Tibor LM, Leunig M. The pathoanatomy and arthroscopic management of femoroacetabular impingement. Bone Joint Res. 2012;1:245–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weir A, de Vos RJ, Moen M, Holmich P, Tol JL. Prevalence of radiological signs of femoroacetabular impingement in patients presenting with long-standing adductor-related groin pain. Br J Sports Med. 2011;45:6–9. [DOI] [PubMed] [Google Scholar]
- 32. Yuan BJ, Bartelt RB, Levy BA, Bond JR, Trousdale RT, Sierra RJ. Decreased range of motion is associated with structural hip deformity in asymptomatic adolescent athletes. Am J Sports Med. 2013;41:1519–1525. [DOI] [PubMed] [Google Scholar]