Abstract
Background:
Hip dysplasia has been shown to be a cause of early arthritis. The decrease in bony coverage has shown increased stress on the acetabular labrum as it shares an increased load.
Purpose/Hypothesis:
The purpose of this study was to divide a cohort of patients by radiographic measures of dysplastic and nondysplastic hips for comparison with regard to labral size at 4 anatomic locations. The hypothesis was that dysplastic hips will have significantly larger labral size compared with nondysplastic hips.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A prospective study was conducted at a single institution. A total of 130 patients underwent hip arthroscopy during the study period from September 2011 to February 2012. Intraoperatively, arthroscopic measurements were taken at 4 quadrants on the acetabular clockface: anterosuperior (12-3 o’clock), anteroinferior (3-6 o’clock), posterosuperior (9-12 o’clock), and posteroinferior (6-9 o’clock). Three radiographic parameters for dysplasia were used to substratify the study population base: lateral center-edge angle (LCEA) ≤25° and LCEA >25°, acetabular inclination (AI) ≤10° and AI >10°, and anterior center-edge angle (ACEA) ≤20° and ACEA >20°.
Results:
For the LCEA ≤25° group, there were 28 hips with mean LCEA of 20.96° ± 3.40°. Patients with LCEA ≤25° had larger labral width in all 4 quadrants (P < .05). For AI >10°, there were 12 hips with the mean AI 12.92° ± 2.50°. Patients with AI >10° had larger labral size in the posteroinferior quadrant only (P < .05). For ACEA ≤20°, there were 4 hips with a mean ACEA of 11.25° ± 5.19°. The anteroinferior and posteroinferior quadrants had a significant increase in labral size when substratified by ACEA ≤20° (P < .05).
Conclusion:
Labral size was significantly larger in dysplastic hips compared with nondysplastic hips. The posteroinferior quadrant labrum was larger in size in dysplastic hips, as measured by any of the 3 radiographic measurements of dysplasia. Hips with LCEA ≤25° had larger labra in all 4 quadrants.
Keywords: hip arthroscopy, hip dysplasia, hip imaging, hip labrum
Hip dysplasia has been shown to be a cause of early osteoarthritis14 secondary to underlying instability due to decreased acetabular coverage applying more stress to the articular cartilage and acetabular labrum.15 The labrum is a triangular fibrocartilaginous structure attached to the rim of the acetabulum. It may increase the depth of the acetabulum, resulting in extended coverage of the femoral head and increased joint stability.5,16 Alternatively, the labrum in the setting of dysplasia may increase contact pressures secondary to decreased available surface area. Dysplastic hips have been shown to have an increased labral size in the anterosuperior quadrant,12 suggesting this is the primary area of initial fatigue. A recent finite element analysis model has shown that in dysplastic hips, the labrum supported 4% to 11% of the total load transferred across the joint, while the normal model supported 1% to 2% of the total load.7
There are several radiographic measurements used to define acetabular undercoverage. Most commonly, the lateral center-edge angle (LCEA) has been used to categorize dysplasia in patients with an angle measuring less than 25°. This angle is calculated on an anteroposterior (AP) pelvis radiograph subtended by a line drawn from the center of the femoral head to the lateral aspect of the sourcil and a vertical line drawn through the center of the femoral head. Additionally, acetabular inclination (AI) and anterior center-edge angle (ACEA) have also been used to categorize hip dysplasia with measurements >10° and <20°, respectively, considered dysplastic.1,4
The purpose of this study was to evaluate a cohort of patients by substratification into groups of dysplastic hips and nondysplastic hips with regard to labral size at 4 anatomic locations: anterosuperior, anteroinferior, posterosuperior, and posteroinferior. Our hypothesis was that dysplastic hips will have significantly larger labral size compared with nondysplastic hips at all quadrants.
Materials and Methods
Data were collected prospectively on all patients undergoing hip preservation surgery with institutional review board approval. During the study period from September 2011 to February 2012, a total of 130 patients underwent hip arthroscopy for symptomatic labral tears secondary to femoroacetabular impingement refractory to at least 6 weeks of physical therapy. Patients were excluded for previous hip surgery, absence of intraoperative labral size measurement data, and inadequate preoperative radiographs, including AP pelvic and false-profile views. Data were collected prospectively but retrospectively reviewed. There were 102 (81.6%) patients (102 hips) who met inclusion criteria and were included in the study. Three radiographic parameters for dysplasia were used to substratify the study population: LCEA ≤25° and >25°, AI ≤10° and >10°, and ACEA ≤20° and >20°.
Clinical Evaluation
Plain radiographs included AP pelvic, Dunn, cross-table lateral, and false-profile views.6,13,17 Measurements were made from these views including the AI angle using the method described in Jessel et al,9 the LCEA of Wiberg,18 and ACEA.3 Dysplasia was characterized using 3 separate radiographic measurements. Most commonly, the LCEA is used to classify dysplasia as measured on AP pelvic radiographs. An LCEA ≤25° in our study was classified as a dysplastic hip. Additionally, an AI >10° and ACEA ≤20° were also used as additional classifications for dysplasia in our study. Separate groups were analyzed based on all 3 of these criteria. The same orthopaedic surgeon (B.G.D.) made all measurements using a picture archiving and computer system (PACS).
Surgical Procedure
All hip arthroscopies were performed at a tertiary referral center dedicated to hip arthroscopy and preservation. All operations were performed by the senior author (B.G.D.) with the assistance of an orthopaedic fellow. All were performed in the modified supine position using a minimum of 2 portals (anterolateral and midanterior).2,10 A diagnostic arthroscopy was initially performed after capsulotomy to assess intra-articular pathology. At this time, the labrum was measured in 4 quadrants: anterosuperior, anteroinferior posterosuperior, and posteroinferior, representing 12 to 3, 3 to 6, 9 to 12, and 6 to 9 on the clockface, respectively (Figure 1). Measurements were only taken on intact labrum. There were no labral tears large enough to preclude measurements from any of the 4 quadrants. Arthroscopic measurements were performed using an arthroscopic probe with 5-mm interval markings at the distal end. The tip of the arthroscopic probe was placed on the articular edge of the labrum in each quadrant. Using the 5-mm interval markings on the probe, we measured the width of the labrum to the capsulolabral junction.
Figure 1.
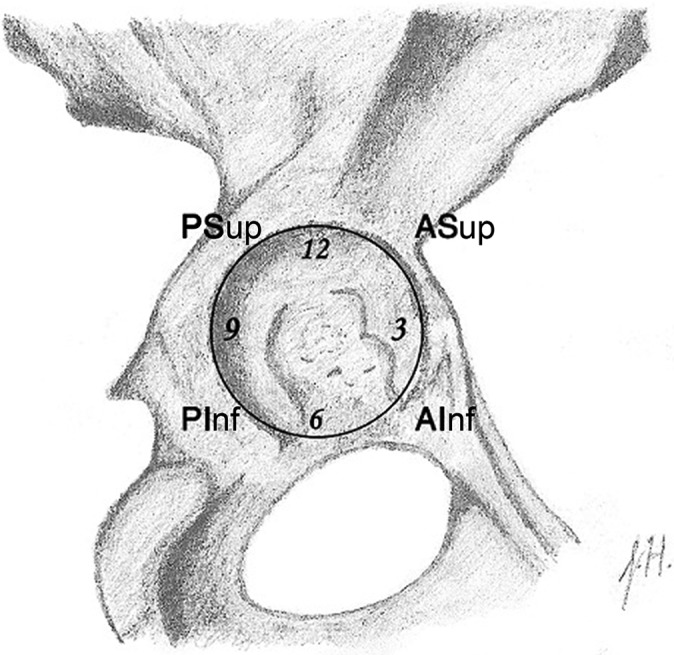
Acetabulum with clockface. AInf, anteroinferior; ASup, anterosuperior; PInf, posteroinferior; PSup, posterosuperior.
Statistical Analysis
Unpaired t tests were used to compare means between groups. Analysis of variance was used to compare labral size at the various quadrants for each group. A P value of <.05 was considered significant. Statistical analysis was performed using Microsoft Excel 2007 (Microsoft Corp) and IBM SPSS 12.0 for Windows (IBM Corp). There are no previous studies to allow a calculation of adequate sample size. Therefore, a post hoc analysis was performed to determine whether the study was adequately powered. For a sample size of 130 patients, the observed power for a 2-tailed hypothesis was 0.37, suggesting that the study is not adequately powered for the differences observed. Interrater variability was assessed for 25 radiographs for the makers of dysplasia (LCEA, AI, and ACEA) and for 10 arthroscopies for the measurement of labral size. The magnitude of the kappa values was 0.62 and 0.53 for radiographic and arthroscopic measurements, respectively, suggesting fair to good interrater variability.
Results
Demographics
A total of 102 patients (102 hips) were included in the study, and demographic information is presented in Table 1. We had 34 males and 68 females; the mean body mass index for the dysplastic group was 24.29 kg/m2 and for the nondysplastic group was 25.90 kg/m2 (P = .13). There were 41 left hips and 61 right hips. Table 2 shows demographic data for patients with an LCEA ≤25° compared with patients with an LCEA >25°.
TABLE 1.
Patient Demographics (N = 102 Patients)
| Mean age, y | 38.72 |
| Sex, n (%) | |
| Male | 34 (33.33) |
| Female | 68 (66.67) |
| Side, n (%) | |
| Left | 41 (40.2) |
| Right | 61 (59.8) |
| Mean body mass index, kg/m2 | 25.47 |
TABLE 2.
Demographics Based on Lateral Center-Edge Angle (LCEA) Classification
| LCEA ≤25° (n = 28 Hips) | LCEA >25° (n = 74 Hips) | P | |
|---|---|---|---|
| Mean age, y | 35.87 | 40.15 | .17 |
| Sex, n | .27 | ||
| Male | 7 | 27 | |
| Female | 21 | 47 | |
| Side, n | .91 | ||
| Left hip | 11 | 30 | |
| Right hip | 17 | 44 | |
| Mean body mass index, kg/m2 | 24.29 | 25.90 | .13 |
Labral Size and Radiographic Measurement
Lateral Center-Edge Angle
Groups were divided into LCEA ≤25° and >25°. For LCEA ≤25°, there were 28 hips (mean age, 35.87 years) (Figure 2). For the group with an LCEA >25°, there were 74 hips (mean age, 40.15 years). The mean LCEA was 20.96° ± 3.40° for the first mentioned group compared with 32.09° ± 5.14° for the latter. All 4 quadrants had a statistically significant increase in labral size for the group with LCEA ≤25°.
Figure 2.
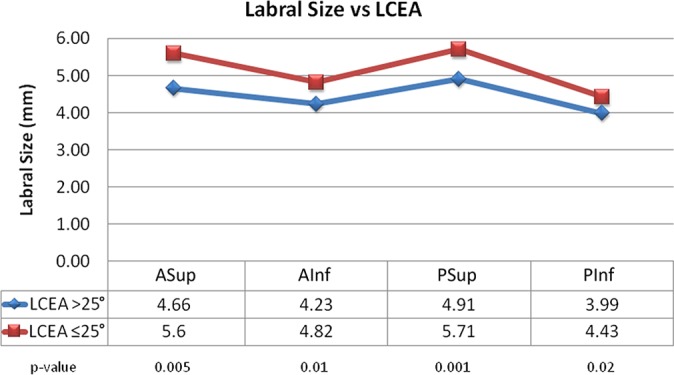
Labral size at each quadrant based on lateral center-edge angle (LCEA). AInf, anteroinferior; ASup, anterosuperior; PInf, posteroinferior; PSup, posterosuperior.
Acetabular Inclination
For AI >10°, there were 12 hips (mean age, 43.53 years) (Figure 3). The mean AI was 12.92° ± 2.50° for the dysplastic group. Only the posteroinferior quadrant had a statistically significant increase in labral size when substratified by AI >10°. For AI ≤10°, there were 90 hips (mean age, 38.12 years). The mean AI was 3.63° ± 4.31°.
Figure 3.
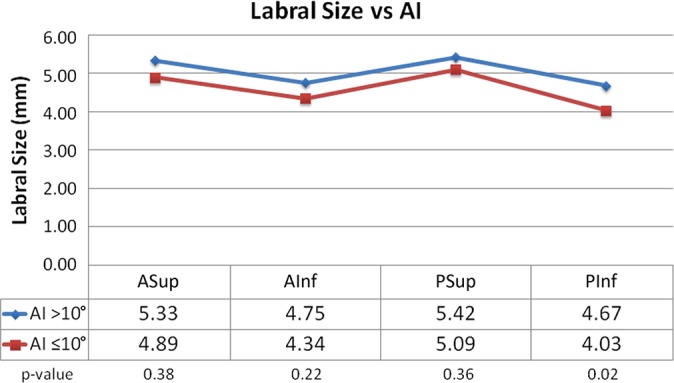
Labral size at each quadrant based on acetabular inclination (AI). AInf, anteroinferior; ASup, anterosuperior; PInf, posteroinferior; PSup, posterosuperior.
Anterior Center-Edge Angle
The false-profile radiograph was unavailable for 7 patients, leaving a total of 95 patients available for the study. For ACEA ≤20°, there were 4 hips (mean age, 33.86 years). The mean ACEA was 11.25° ± 5.19°. The anteroinferior and posteroinferior quadrants had a statistically significant increase in labral size when substratified by ACEA ≤20° (Figure 4). For ACEA >20°, there were 91 hips (mean age, 39.08 years). The mean ACEA was 32.07° ± 6.45°. In terms of overlap of dysplasia parameters in the cohort, there were 3 patients with LCEA ≤25°, AI >10°, and ACEA ≤20°.
Figure 4.
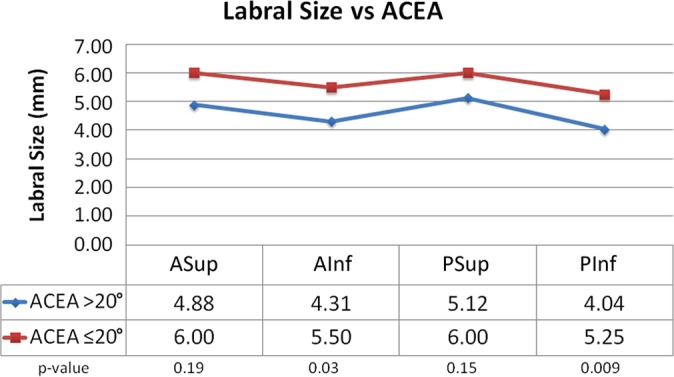
Labral size at each quadrant based on anterior center-edge angle (ACEA). AInf, anteroinferior; ASup, anterosuperior; PInf, posteroinferior; PSup, posterosuperior.
We also reported the mean labral size at each quadrant based on the 3 radiographic parameters for dysplasia (Table 3). There was a significant difference for all quadrants when the groups were stratified for LCEA. The posteroinferior quadrant was significant for all 3 parameters of dysplasia, and ACEA had additional significance for the anteroinferior quadrant.
TABLE 3.
Mean Labral Size by Quadrant and Dysplasia Parametera
| Parameter | Quadrant | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anterosuperior | Anteroinferior | Posterosuperior | Posteroinferior | |||||||||
| n | Labrum Size, mm, Mean ± SD (Range) | P (t Test) | n | Labrum Size, mm, Mean ± SD (Range) | P (t Test) | n | Labrum Size, mm, Mean ± SD (Range) | P (t Test) | n | Labrum Size, mm, Mean ± SD (Range) | P (t Test) | |
| LCEA | .005 | .01 | .001 | .02 | ||||||||
| ≤25° | 28 | 5.7 ± 1.9 (3-10) | 28 | 4.8 ± 1.3 (3-8) | 28 | 5.7 ± 1.4 (4-10) | 28 | 4.4 ± 1 (2-7) | ||||
| >25° | 74 | 4.7 ± 1.5 (3-10) | 74 | 4.2 ± 1 (2-7) | 74 | 4.9 ± 1 (3-8) | 74 | 4 ± 0.8 (3-7) | ||||
| AI | .38 | .22 | .36 | .02 | ||||||||
| ≤10° | 90 | 4.9 ± 1.7 (3-10) | 90 | 4.3 ± 1.1 (2-8) | 90 | 5.1 ± 1.2 (3-10) | 90 | 4 ± 0.9 (2-7) | ||||
| >10° | 12 | 5.3 ± 1.3 (3-7) | 12 | 4.8 ± 1.1 (3-7) | 12 | 5.4 ± 0.8 (4-7) | 12 | 4.7 ± 0.7 (4-6) | ||||
| ACEA | .19 | .03 | .15 | .009 | ||||||||
| ≤20° | 4 | 6 ± 1.2 (5-7) | 4 | 5.5 ± 1.3 (4-7) | 4 | 6 ± 1.2 (5-7) | 4 | 5.3 ± 1.3 (4-7) | ||||
| > 20° | 91 | 4.9 ± 1.7 (3-10) | 91 | 4.3 ± 1.1 (2-8) | 91 | 5.1 ± 1.2 (3-10) | 91 | 4 ± 0.9 (2-7) | ||||
aBoldfaced P values indicate statistically significant difference within each parameter (P < .05). ACEA, anterior center-edge angle; AI, acetabular inclination; LCEA, lateral center-edge angle.
Discussion
To our knowledge, this study is the first comparison of intraoperative measurements of labral size in a cohort of patients categorized as dysplastic and nondysplastic hips. When using the LCEA as the primary measure, we found a significant increase in labral size at all 4 quadrants in those hips with dysplasia. Additionally, we noted that the posteroinferior labral size was significantly larger in dysplastic hips when accounting for LCEA, ACEA, and AI.
Recent finite element analysis modeling7 has shown that there is increased load transferred across the joint to the labrum in dysplastic hips. We theorize that similar to the Wolff law with bone, the labrum will remodel itself over time to become stronger and resist abnormal increase in load. Further studies need to be elucidated to determine the internal architecture of the dysplastic labrum to see if it has morphologic differences to normal labrum.
The LCEA has been traditionally used as the measure for dysplasia in the hip.4 There were only 3 patients who had an overlap of all 3 parameters of dysplasia, that is, LCEA ≤25°, AI >10°, and ACEA ≤20°. The main reason for this is that patients with severe dysplasia are more likely to have undergone a bony acetabular reorientation procedure rather than hip arthroscopy primarily to address edge loading of the labrum. These patients were therefore not included in the study. In our study, we found that when using the LCEA as our primary measure, all 4 acetabular quadrants had significantly larger labra. We included ACEA and AI as additional measurements of acetabular dysplasia and found that only the posteroinferior acetabular quadrant had a significantly larger labrum. These results are in contrast with the mechanics of the dysplastic hip where there is decreased bony acetabular coverage laterally and anteriorly.12 The reason for this discrepancy is not entirely clear; however, one of the limitations for cadaveric studies is the difficulty incorporating the contribution of dynamic considerations of neuromuscular function in joint stability. Cadaveric studies can generally only assess static constraints to joint stability. This should theoretically produce more stress on the labrum in these regions with resulting larger labra.
Leunig et al12 evaluated the use of magnetic resonance arthrography to evaluate for labral differences between dysplastic and nondysplastic hips. They found that the labrum was enlarged in 12 of 14 patients within the dysplastic group and in none of the nondysplastic groups in the anterosuperior labrum. They concluded that the anterosuperior region represents the initial fatiguing site of the hip. It should be noted that this was exclusively a radiographic study, and they did not confirm their diagnosis with arthroscopic measurements. In our own study, we found significant increases in labral size at all 4 quadrants with respect to LCEA cutoff for dysplasia using direct visualization. Interestingly, Kubo et al11 evaluated 60 dysplastic hips using radial magnetic resonance imaging (MRI) and found that the acetabular labrum was larger in dysplastic hips than in normal hips, and the size increased in the posterosuperior quadrant.
James et al8 performed MRIs on 27 adult dysplastic hips and found that the acetabular labra in the dysplastic hips had abnormal signal intensity and an elongated appearance when compared with the control group (mean length, 10.9 vs 6.4 mm). They also noted morphological appearances in the labra of surface irregularity, fissures, and cleft formation.
The strengths of our study include the prospective nature of our study: the fact that this is one of the first studies to evaluate labral size using direct measurement via arthroscopy instead of relying on imaging studies. Furthermore, the main clinical relevance for the study is that recognizing a hypertrophied labrum in the setting of dysplasia should alert the surgeon to the potential of increased labral penetration when performing hip arthroscopy. In addition, the hypertrophic labrum may have an increased soft tissue stabilizing role in the dysplastic hip, and therefore, appropriate restoration of labral function through repair should be an important consideration for any arthroscopic intervention in these patients. One of the weaknesses of our study was the fact that we did not perform a matched-pair study design and we did not correlate to preoperative MRI findings. Furthermore, labral measurements with a 5-mm tipped probe may lead to measurement inaccuracies. However, interrater reliability was fair to good for arthroscopic measurement of labral size when measured by the primary surgeon and fellow independently. MRI data for labral size could not be correlated, as many of the scans were performed at different institutions with varying slices and degrees of resolution. In addition, the surgeon was not blinded to radiological measurements preoperatively and this may have contributed to bias of labral size measurements. However, as part of the operative planning of other procedures such as depth of acetabular resection and femoroplasty, the surgeon was required to view radiographs preoperatively. Another potential source of bias is selecting patients with symptomatic hips, making it difficult to conclude whether labral hypertrophy may be a consequence of another pathology such as femoroacetabular impingement. In addition, the reduced power of the study may potentially lead to type 2 errors. Despite this limitation, this is the largest study to date on this specific topic. Future studies should include histological analysis of dysplastic labra to determine structural differences compared with nondysplastic hips.
Conclusion
Labral size was significantly larger in dysplastic hips compared with nondysplastic hips. The posteroinferior quadrant labrum was larger in size in dysplastic hips, as measured by any of the 3 radiographic measurements of dysplasia. Hips with LCEA ≤25° had larger labra in all 4 quadrants. However, there was variability of labral size at each quadrant within groups.
Footnotes
One or more of the authors has reported the following potential conflict of interest or source of funding: B.G.D. receives financial support from Arthrex, Mako Surgical, Padra, DJO Global, ATI, Orthomerica, and Breg and has patents pending related to the arthroscopic labral reconstruction technique and kit. This study was funded by the American Hip Institute, which receives funding from Arthrex, Mako Surgical, Padra, ATI, and Breg.
References
- 1. Anda S. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1993;(286):308–310. [PubMed] [Google Scholar]
- 2. Byrd JW. Hip arthroscopy. The supine position. Clin Sports Med. 2001;20:703–731. [PubMed] [Google Scholar]
- 3. Chosa E, Tajima N. Anterior acetabular head index of the hip on false-profile views. New index of anterior acetabular cover. J Bone Joint Surg Br. 2003;85:826–829. [PubMed] [Google Scholar]
- 4. Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;(175):79–85. [PubMed] [Google Scholar]
- 5. Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. [DOI] [PubMed] [Google Scholar]
- 6. Dunn DM. Anteversion of the neck of the femur; a method of measurement. J Bone Joint Surg Br. 1952;34-B:181–186. [DOI] [PubMed] [Google Scholar]
- 7. Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011;44:2201–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. James S, Miocevic M, Malara F, Pike J, Young D, Connell D. MR imaging findings of acetabular dysplasia in adults. Skeletal Radiol. 2006;35:378–384. [DOI] [PubMed] [Google Scholar]
- 9. Jessel RH, Zurakowski D, Zilkens C, Burstein D, Gray ML, Kim YJ. Radiographic and patient factors associated with pre-radiographic osteoarthritis in hip dysplasia. J Bone Joint Surg Am. 2009;91:1120–1129. [DOI] [PubMed] [Google Scholar]
- 10. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. [DOI] [PubMed] [Google Scholar]
- 11. Kubo T, Horii M, Yamaguchi J, et al. Acetabular labrum in hip dysplasia evaluated by radial magnetic resonance imaging. J Rheumatol. 2000;27:1955–1960. [PubMed] [Google Scholar]
- 12. Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;(418):74–80. [DOI] [PubMed] [Google Scholar]
- 13. Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. [DOI] [PubMed] [Google Scholar]
- 14. Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. [DOI] [PubMed] [Google Scholar]
- 15. Nishii T, Sugano N, Tanaka H, Nakanishi K, Ohzono K, Yoshikawa H. Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Clin Orthop Relat Res. 2001;(383):183–190. [DOI] [PubMed] [Google Scholar]
- 16. Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH., Jr Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;(382):232–240. [DOI] [PubMed] [Google Scholar]
- 17. Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed] [Google Scholar]
- 18. Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am. 1953;35-A:65–80. [PubMed] [Google Scholar]


