Abstract
Background:
Various surgical techniques to treat posterolateral knee instability have been described. To date, the recommended treatment is an anatomic form of reconstruction in which the 3 key structures of the posterolateral corner (PLC) are addressed: the popliteofibular ligament, the popliteus tendon, and the lateral collateral ligament.
Purpose/Hypothesis:
The purpose of this study was to identify the role of each key structure of the PLC in kinematics of the knee and to biomechanically analyze a single-graft, fibular-based reconstruction that replicates the femoral insertions of the lateral collateral ligament and popliteus to repair the PLC. The hypothesis was that knee kinematics can be reasonably restored using a single graft with a 2-strand “modified Larson” technique.
Study Design:
Descriptive laboratory study.
Methods:
Eight fresh-frozen cadaveric knees were used in this study. We conducted sequential sectioning of the popliteofibular ligament (PFL) and then subsequently the popliteal tendon (PT), the lateral collateral ligament (LCL), and the anterior cruciate ligament (ACL). We then reconstructed the ACL first and then the posterolateral corner using the modified Larson technique. A surgical navigation system was used to measure varus laxity and external rotation at 0°, 30°, 60°, and 90° with a 9.8-N·m varus stress and 5-N·m external rotation force applied to the tibia.
Results:
In extension, varus laxity increased only after the sectioning of the lateral collateral ligament. At 30° of flexion, external rotation in varus and translation of the lateral tibial plateau increased after the isolated popliteofibular ligament section. From 60° to 90° of flexion, translation and mobility of the lateral plateau section increased after sectioning of the PFL. After reconstruction, we observed a restoration of external varus rotation in extension and translation of the lateral tibial plateau at 90° of flexion. This technique provided kinematics similar to the normal knee.
Conclusion:
The PFL has a key role between 30° and 90° of flexion, and the lateral collateral ligament plays a role in extension. Reconstruction with the modified Larson technique restores these 2 complementary stabilizers of the knee.
Clinical Relevance:
Although there are many different techniques to reconstruct the PLC-deficient knee, this study indicates that a single-graft, fibular-based reconstruction of the LCL and PT may restore varus and external rotation laxity to the knee.
Keywords: posterolateral corner, popliteofibular ligament, collateral lateral ligament, navigation, anterior cruciate ligament
Injuries to the fibular collateral ligament and posterolateral corner are uncommon and are usually associated with other ligamentous injuries, in particular, to the anterior cruciate ligament (ACL) and/or posterior cruciate ligament, leading to significant functional impairment. It is important that reconstructions of posterolateral knee injuries restore joint kinematics and patient function, but residual laxities are often observed.7
The posterolateral corner (PLC) of the knee is a complex static and dynamic stabilizer composed of 3 structures: the popliteofibular ligament, the popliteal tendon, and the lateral collateral ligament.21,26 This periarticular complex has been studied when associated with a posterior cruciate ligament rupture. It is now recognized that the posterolateral structures contribute to stability in varus and external rotation of the knee.4,14,20,24,28
In contrast, isolated injuries of the PLC are relatively rare in clinical practice, and the specific role of each element in the stability of the knee has not been fully evaluated. The combination of PLC injury and ACL lesion is also uncommon. Failure to recognize and treat the PLC injury may result in failure of the ACL reconstruction.6,13
The objectives of this study were to evaluate the function of the 3 key components of the PLC stabilizing the knee at different degrees of flexion and to evaluate a modification of the Larson technique described by Schechinger et al.23
Materials and Methods
Specimen Preparation and Instrumentation
Eight fresh-frozen cadaveric knees (6 male, 2 female), ranging in age from 54 to 68 years (mean, 61.5 ± 6.7 years) were used in this study. No knee had previous intra-articular injury or marked articular degeneration (preoperative radiographic assessment). The knees were thawed 24 hours before the start of manipulation. This cadaveric study was performed in accordance with the protocols and recommendations of the institution. Initial physical examination including varus valgus and anterior-posterior drawer stress testing confirmed the absence of pathologic laxity. For each knee, a medial parapatellar mini-arthrotomy was performed to attach targets to the navigation system.
A posterior lateral approach was used to dissect the 3 structures of the PLC and perform the subsequent reconstruction. The semitendinosus and the gracilis tendons were harvested from the same knee (for ACL reconstruction) and the semitendinosus of the contralateral knee was harvested for the PLC reconstruction.
Surgical Navigation System
We used a navigation system (Surgetics Station Nano; Praxim Medivision) equipped with software for the reconstruction of the ACL (ACL Surgetics Logics Software). This software enabled the acquisition of data on the kinematics of the knee after implementation of rigid bodies and the mapping of anatomic references with a digitizing probe, as previously described.21
The reference points included for this study were the center of femoral notch, the middle of the transverse meniscal ligament on the anterior tibia, and the center of the medial and lateral tibial plateaus. This system has been shown to be very precise, within 1° or 1 mm.6,8,21 Motion was tracked over a range of 110° of flexion.
Reflective markers were mounted in the proximal femur and distal tibia. Once the markers were placed, surface landmarks on the tibial plateau and distal femur were recorded, intra-articular surface geometry was mapped, and a 3-dimensional model was created. The knee was manually cycled from 0° to 110° of flexion.
Operating Protocol and Testing
We performed a standardized calibration procedure, including the definition of the frontal sagittal and horizontal planes. The intact knee was tested at 0°, 30°, 60°, and 90° of knee flexion, with an applied varus load of 9.8 N·m.12,13 The degree of knee flexion was obtained by the surgical navigation system. The load was manually applied with a tensioner parallel to the joint line 10 cm from the joint. The knee was placed at neutral rotation at the start of testing, and a rotational load was also applied by placement of a 5-N·m load with a tensiometer perpendicular to the joint line.9 Varus valgus and rotational displacement were recorded by the navigation system in degrees, and translation of lateral plateau was also recorded in millimeters. Each testing condition was repeated 3 times, and the average of the measurements was recorded. Once the data from the intact knee were obtained, the lateral side of the knee was exposed to isolate the structures of the PLC. The dissection was taken down through the subcutaneous tissues to the iliotibial band (IT), which was divided in line with the fibers to expose the attachments of the lateral collateral ligament (LCL) and popliteus tendon (PT). The distal attachment of the IT band was maintained. The attachments of LCL, PT, and popliteofibular ligament were identified. At each step of the procedure, each of these elements was resected, after which the origins and insertions of these structures were carefully marked on the cadaveric specimens. Care was taken to preserve the posterior cruciate ligament and the posterior capsule.
For each of the 8 knees, 7 successive tests were run:
Intact knee (1-intact)
Section of the popliteofibular ligament (PFL) (2-woPFL)
Section of the PT (3-woPT)
Section of the LCL (4-woLCL)
Section of the ACL (5-woACL)
ACL reconstruction (6-ACLR)
PLC reconstruction (7-PLCR)
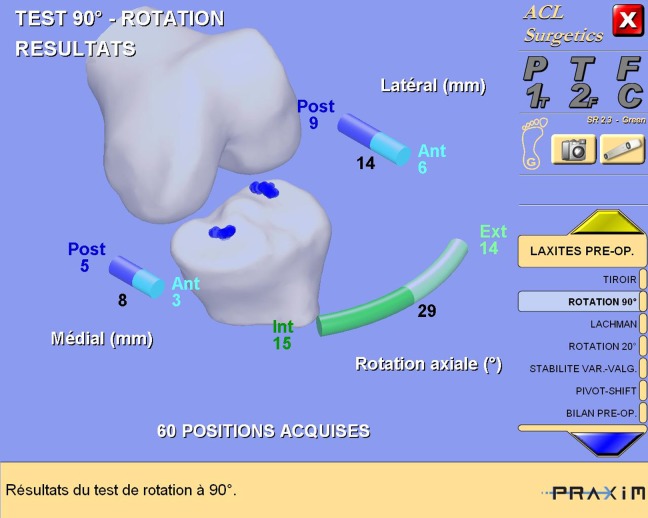
At each of the 7 steps and for each of the 8 knees, we evaluated varus-valgus laxities, internal-external rotation, and internal-external rotation when printing varus and valgus. These sequences were repeated at 0°, 30°, and 60° of knee flexion. The translation of the medial tibial plateau and lateral tibial plateau (in millimeters) with the anterior drawer at 30° and 90° (Figure 1) were also evaluated by the navigation system. Maximum mobility (translation of the lateral plateau between external and internal rotation) of the lateral tibial plateau at 30°, 60°, and 90° of flexion was also measured. The measurements were performed by a single operator, and they were repeated 3 times for each step; the average of these 3 measurements was recorded.
Figure 1.
Example of data from the navigation system.
ACL Reconstruction
A standard single-bundle ACL reconstruction was performed using the Hamstring tendons. Femoral graft fixation was achieved with the EndoButton device (Smith & Nephew), and tibial fixation was achieved by an interference screw (Biosure HA; Smith & Nephew) with the knee in 30° of flexion and neutral rotation.
PLC Reconstruction
Reconstruction of PLC was performed according to the Schechinger modification of the Larson technique.25 We aimed to reconstruct the LCL and the PFL with a semitendinosus tendon tensioned to 30 N, as described by Markolf et al.13 The mean tendon width was 6 mm (range, 5-7 mm). The technique described by Schechinger consists of a double femoral tunnel and a single oblique fibular tunnel, as described by Bicos and Arciero2 (Figures 2 and 3).
Figure 2.
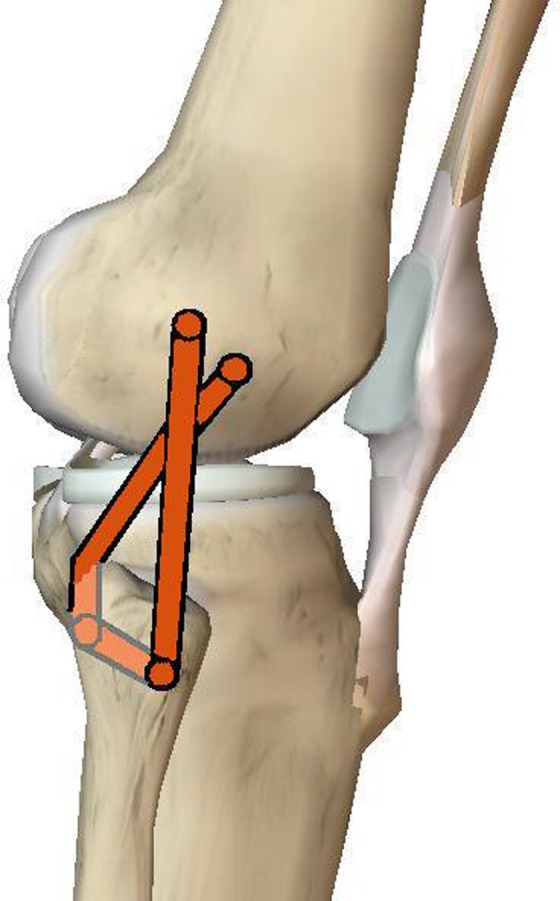
Posterolateral corner reconstruction: The modified Larson technique as described by Schechinger et al.23
Figure 3.
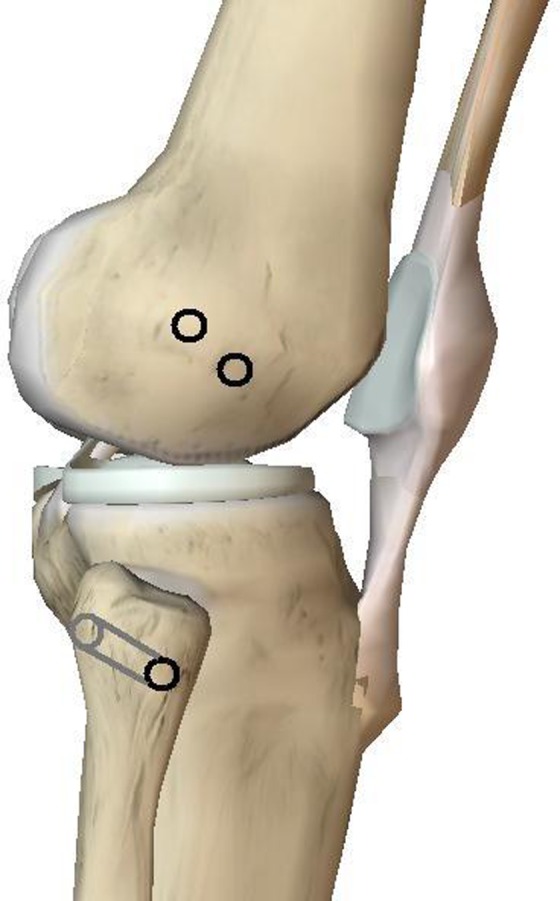
Tunnel placement.
A 6-mm oblique tunnel from anteromedial to posterolateral on the fibula was created with a posterior-anterior and descendant direction parallel to the joint line. We used the tendon of the contralateral semitendinosus. Both ends of the graft were sutured with a No. 2 FiberWire (Arthrex) and pulled through the proximal fibular tunnel. A 6 mm–diameter tunnel was created at the femoral insertion of the LCL. The sutures in the graft were passed through the femoral tunnel to the medial side of the femur. A 6 mm–diameter tunnel was made at the insertion of the PT, and the Kirschner wire was also drilled through the distal medial condyle. The free ends of the semitendinosus were pulled through the femoral tunnels. The graft was tensioned to 30 N with the knee flexed to 30°, as measured by the surgical navigation software. The isometry was tested by moving the knee through a full range of motion. The femoral fixations of the graft were obtained with 2 interference screws (Biosure HA). Graft fixation was achieved with the knee in 30° of flexion and neutral rotation about the tibial axis.
Statistical Analysis
Statistical analysis was performed by a team of independent statisticians (Clinical Investigation Centre). The value used for the statistical analysis was the average of these 3-times-repeated measurements. Variance, Student t tests, and the Friedman test were used to highlight differences between 2 steps. The level of significance was set at P < .05. Data are presented as the mean with 95% CI.
Results
After Section of the Structures of PLC
At 0° (Full Extension)
Compared with the intact knee, varus laxity increased significantly only after the section of the LCL. The difference was significant between stages 1 (intact) and 4 (woLCL) (6.42° ± 1.54°; P < .001), stages 2 (woPFL) and 4 (woLCL) (6.08° ± 1.34°; P < .001), and between stages 3 (woPT) and 4 (woLCL)(6° ± 1.46°; P < .001) (Table 1).
TABLE 1.
Increase in Varus, External Rotation, and External Rotation Coupled With Varus After Selective Sectioning of the Posterolateral Corner Ligaments and the Anterior Cruciate Ligamenta
| Stage Comparisonb | Varus, deg | External Rotation, deg | External Rotation in Varus, deg | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Full Extension | 30° | 60° | Full Extension | 30° | 60° | Full Extension | 30° | 60° | |
| 1-intact and 2-woPFL | 0.33 ± 0.69 | 6.96 ± 0.84 | 8.70 ± 1.45 | 0.08 ± 0.46 | 7.16 ± 2.03 | 6.88 ± 1.05 | 0.54 ± 0.47 | 7.75 ± 2.01 | 7.08 ± 1.47 |
| 1-intact and 3-woPT | 0.41 ± 0.75 | 7.13 ± 0.94 | 8.58 ± 1.76 | 0.33 ± 1.39 | 7.46 ± 1.45 | 7.21 ± 0.97 | 0.29 ± 0.58 | 7.25 ± 1.74 | 7.13 ± 1.67 |
| 1-intact and 4-woLCL | 6.42 ± 1.54 | 7.13 ± 1.21 | 9.08 ± 2.13 | 0.83 ± 0.85 | 8.04 ± 2.13 | 7.33 ± 1.23 | 1.13 ± 0.64 | 7.75 ± 1.80 | 7.13 ± 1.21 |
| 2-woPFL and 3-woPT | 0.08 ± 0.35 | ND | ND | ND | ND | ND | ND | ND | ND |
| 2-woPFL and 4-woLCL | 6.08 ± 1.34 | ND | ND | ND | ND | ND | ND | ND | ND |
| 3-woPT and 4-woLCL | 6.00 ± 1.46 | ND | ND | ND | ND | ND | ND | ND | ND |
| 1-intact and 5-woACL | 6.86 ± 1.60 | 9.79 ± 2.11 | 13.46 ± 3.34 | 8.58 ± 1.83 | 13.04 ± 3.02 | 11.71 ± 1.94 | 8.58 ± 2.04 | 13.21 ± 3.20 | 12.17 ± 2.48 |
aBolded values indicate statistically significant increase (P < .05). ND, no difference.
bSee the Materials and Methods section for a list of abbreviations used.
No significant difference was demonstrated with regard to the isolated external single rotation and external rotation in varus.
After sectioning of the PLC and ACL, there was a significant increase for all degrees of freedom (either controlled or unconstrained).
At 30° of Flexion
Varus laxity increased significantly from the isolated PFL section. There was a significant difference between stages 1 and 2 (woPFL) (6.96° ± 0.84°; P < .001) (Table 1). External rotation in varus increased significantly from the isolated PFL section. There was a significant difference between stages 1 (intact) and 2 (woPFL) (7.75° ± 2.01°; P < .001). On the other side, the increase in external rotation without varus was significant only after the full section of the PLC (8.04° ± 2.13°; P < .001) between stages 1 and 4 (woLCL) (Table 1). The translation of the lateral tibial plateau in external rotation and maximum mobility of lateral tibial plateau increased significantly from the isolated PFL section. There was a significant difference between stages 1 and 2 (woPFL) (8.29 ± 1.27 mm [P < .001] and 15.08 ± 1.97 mm [P < .001], respectively) (Table 2).
TABLE 2.
Increase of Translation of the Lateral Tibial Plateau in External Rotation and Maximum Mobility of Lateral Tibial Plateau After Selective Sectioning of the Posterolateral Corner Ligaments and the Anterior Cruciate Ligamenta
| Stage Comparisonb | Translation of the Lateral Tibial Plateau in ER, mm | Maximum Mobility of the Lateral Tibial Plateau, mm | ||||
|---|---|---|---|---|---|---|
| 30° | 60° | 90° | 30° | 60° | 90° | |
| 1-intact and 2-woPFL | 8.29 ± 1.27 | 7.50 ± 1.26 | 6.58 ± 2.51 | 15.08 ± 1.97 | 13.42 ± 2.56 | 12.79 ± 3.41 |
| 1-intact and 3-woPT | 8.33 ± 2.22 | 7.79 ± 0.89 | 6.83 ± 2.24 | 15.13 ± 3.04 | 13.92 ± 1.40 | 13.08 ± 3.20 |
| 1-intact and 4-woLCL | 8.25 ± 2.87 | 8.33 ± 1.22 | 7.46 ± 3.19 | 15.80 ± 3.19 | 15.30 ± 1.22 | 14.30 ± 4.36 |
| 2-woPFL and 3-woPT | ND | ND | ND | ND | ND | ND |
| 3-woPT and 4-woLCL | ND | ND | ND | ND | ND | ND |
| 2-woPFL and 4-woLCL | ND | ND | ND | ND | ND | ND |
| 1-intact and 5-woACL | 1.21 ± 2.93 | 2.58 ± 1.52 | 4.38 ± 5.11 | 8.79 ± 4.72 | 9.42 ± 2.72 | 12.46 ± 6.20 |
| 4-woLCL and 5-woACL | 7.04 ± 2.86 | 5.75 ± 1.81 | 3.08 ± 5.39 | 7.00 ± 2.90 | 5.83 ± 3.08 | 1.79 ± 6.35 |
aBolded values indicate statistically significant increase (P < .05). ER, external rotation; ND, no difference.
bSee the Materials and Methods section for a list of abbreviations used.
After sectioning of the PLC and ACL, we observed a statistical difference with the intact knee for all degrees of freedom (varus, external rotation, external rotation in varus, translation, and mobility of external tibial plateau).
At 60° of Flexion
Varus laxity increased significantly only after complete sectioning of the PLC. There was a significant difference between stages 1 and 4 (woLCL) (9.08° ± 2.13°; P < .001) (Table 1). External rotation also increased significantly from sectioning of the PLC. There was a significant difference between stages 1 and 4 (7.33° ± 1.23°; P < .001) (Table 2). Translation of the lateral tibial plateau in external rotation and maximum mobility of lateral tibial plateau increased significantly after sectioning of the PFL. There was a significant difference between stages 1 and 2 (woPFL) (7.5 ± 1.26 mm [P < .001] and 13.42 ± 2.56 mm [P < .001], respectively) (Table 2). The increase in external varus rotation was not significant at 60° of flexion (Table 1).
After sectioning of the PLC and ACL, a statistically significant increase in laxity compared with the intact knee for all degrees of freedom was observed (varus, external rotation, external rotation in varus, translation, and mobility of external tibial plateau).
At 90° of Flexion
The translation of the lateral tibial plateau in external rotation and maximum mobility of lateral tibial plateau increased significantly after sectioning the PFL. The difference was significant between stages 1 and 2 (woPFL) (6.58 ± 2.51 mm [P < .001] and 12.79 ± 3.41 mm [P < .001], respectively) (Table 2).
ACL and PLC Reconstruction (Stages 6 and 7)
We compared these 2 stages with intact knee (stage 1).
At 0° (Full Extension)
The knee before PLC reconstruction (PLCR) (stage 6) showed no significant difference compared with the intact knee, except with regard to external rotation (with and without varus: 4.29° ± 2.33° [P < .001] and 3.5° ± 1.79° [P < .001], respectively) (Table 3).
TABLE 3.
Increase in Varus, External Rotation, and External Rotation Coupled With Varus After Anterior Cruciate Ligament and Posterolateral Corner Reconstructionsa
| Stage Comparisonb | Varus, deg | External Rotation, deg | External Rotation Coupled With Varus, deg | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Full Extension | 30° | 60° | Full Extension | 30° | 60° | Full Extension | 30° | 60° | |
| 1-intact and 6-ACLR | 3.42 ± 1.75 | 4.25 ± 4.17 | 7.13 ± 5.55 | 4.29 ± 2.33 | 6.50 ± 4.50 | 5.83 ± 2.16 | 3.50 ± 1.79 | 6.29 ± 3.02 | 5.00 ± 1.87 |
| 1-intact and 7-PLCR | 0.13 ± 1.43 | 0.33 ± 2.08 | 0.54 ± 4.56 | 0.13 ± 0.99 | –0.08 ± 1.66 | –0.13 ± 2.28 | 0.00 ± 1.16 | 0.17 ± 2.73 | –0.67 ± 1.55 |
| 6-ACLR and 7-PLCR | –3.29 ± 1.84 | –3.92 ± 2.54 | –6.58 ± 1.39 | –4.16 ± 2.13 | –6.58 ± 3.17 | –5.96 ± 1.58 | –3.5 ± 1.19 | –6.13 ± 1.27 | –5.57 ± 1.12 |
| 5-woACL and 7-PLCR | –6.75 ± 1.50 | –9.46 ± 2.93 | –12.92 ± 2.97 | –8.46 ± 1.44 | –13.13 ± 1.99 | –11.83 ± 3.39 | –8.58 ± 2.35 | –13.04 ± 1.69 | –12.83 ± 2.98 |
aBolded values indicate statistically significant increase (P < .05).
bSee the Materials and Methods section for a list of abbreviations used.
The knee after the PLCR (stage 7) did not show any significant difference compared with the intact knee (under any mode of loading). After PLCR (stage 7), the knee was significantly more stable than after ACLR alone (stage 6) for motion under external rotation in varus (–3.5° ± 1.19°; P < .001) (Table 3).
At 30° of Flexion
Before PLCR (ACLR alone), no significant difference was observed compared with the intact knee. After PLCR, it does not present either difference.
At 60° of Flexion
After stage 6 (ACLR without PLCR), a significant increase in displacement of the tibial plateau was observed in external rotation (6.75° ± 1.32° [P < .001] and 10.08° ± 2.68° [P < .001], respectively).
After PLCR (ACLR + PLCR) (stage 7), no significant difference was observed compared with the intact knee in all degrees of freedom.
At 90° of Flexion
After ACLR (stage 6), the knee was not comparable with the intact knee in all degrees of freedom. We observed an increase of the translation of external tibial plateau in external rotation and maximum mobility of lateral tibial plateau (4.88 ± 2.48 mm [P < .001] and 7.42 ± 2.53 [P < .001], respectively).
After ACLR and PLCR (stage 7), no significant difference with the intact knee was observed in all degrees of freedom (Figures 4 and 5).
Figure 4.
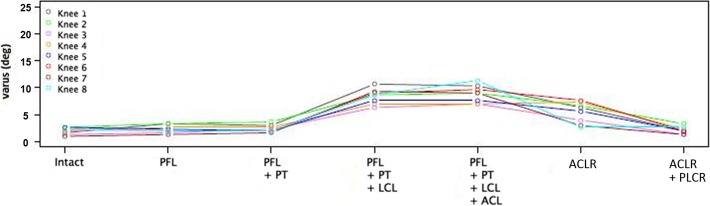
In varus, the completely reconstructed knee (ACLR + PLCR) (stage 7) showed no significant difference with the intact knee (stage 1). ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; LCL, lateral collateral ligament; PFL, popliteofibular ligament; PLCR, posterolateral corner reconstruction; PT, popliteal tendon.
Figure 5.
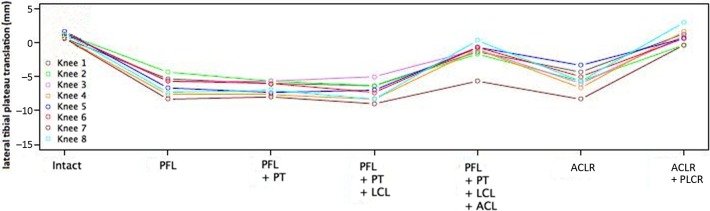
Comparison of translation of lateral tibial plateau: The modified Larson technique (2 femoral tunnels in conjunction with an anteroposterior fibular tunnel) was able to restore varus and external rotation laxity. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; LCL, lateral collateral ligament; PFL, popliteofibular ligament; PLCR, posterolateral corner reconstruction; PT, popliteal tendon.
In comparison with ACLR alone (stage 6), PLCR decreased translation significantly (4.21 ± 2.56 mm; P < .001) and external rotation of lateral tibial plateau (−6.58° ± 3.17°) (Table 4).
TABLE 4.
Amount and Increase of Translation of the Lateral Tibial Plateau in External Rotation, and Maximum Mobility of Lateral Tibial Plateau, After Anterior Cruciate Ligament and Posterolateral Corner Reconstructionsa
| Stage Comparisonb | Translation of the Lateral Tibial Plateau in External Rotation, mm | Maximum Mobility of the Lateral Tibial Plateau, mm | ||||
|---|---|---|---|---|---|---|
| 30° | 60° | 90° | 30° | 60° | 90° | |
| 1-intact and 6-ACLR | 8.08 ± 1.74 | 6.75 ± 1.32 | 4.88 ± 2.48 | 12.33 ± 3.22 | 10.08 ± 2.68 | 7.42 ± 2.53 |
| 1-intact and 7-PLCR | 0.25 ± 1.36 | –0.17 ± 1.15 | –0.66 ± 2.02 | –0.42 ± 2.38 | –0.79 ± 1.96 | 0.96 ± 1.66 |
| 6-ACLR and 7-PLCR | –8.33 ± 1.36 | –6.58 ± 1.67 | –4.21 ± 2.56 | –12.75 ± 1.97 | –10.88 ± 2.46 | –6.46 ± 2.81 |
| 5-woACL and 7-PLCR | –1.46 ± 2.53 | –2.41 ± 1.33 | –3.71 ± 4.10 | –9.21 ± 5.47 | –10.21 ± 3.23 | –11.5 ± 5.98 |
aBolded values indicate statistically significant increase (P < .05).
bSee the Materials and Methods section for a list of abbreviations used.
Discussion
The purpose of this study was to identify the role of each key structure of the PLC in kinematics of the knee and evaluate a technique used to repair the PLC, as previously described by Schechinger et al23 and Sidles et al.25
The great variety of ligamentous injuries that may be associated with posterolateral injury can cause confusion in diagnosis and treatment of posterolateral instability. So for the present biomechanical study, we decided to evaluate combined ACL and PLC tears, which are frequently inadequately treated.
Pearle et al21 showed that the Praxim navigation system allowed assessment of knee kinematics with an accuracy of 1 mm or 1°. Alam et al1 showed that another method to evaluate external rotation with clinical manipulation or skin markers was insufficient. In this study, performance bias was minimized by the use of repeated measurements by the same operator.10,22
The contributions of each structure to lateral knee laxity have been described previously in the literature. Nielsen and Helmig17 showed that the LCL and popliteus restore varus and external rotation forces, with the LCL playing a greater role in preventing varus displacement and the popliteus tendon playing a greater role in preventing pathologic external rotation. Similarly, Gollehon et al4 found that selective sectioning of the PLC (comparing partial to complete PLC sectioning) did not increase posterior translation, but complete transection increased posterior translation considerably. Feeley et al3 found that disruption of the PLC resulted in an increase in varus rotation at all flexion angles, with a peak varus rotation at 30°. Gollehon et al4 found that combined sectioning of the PLC resulted in a peak varus rotation at 30°.
Our study showed that in extension, the section of the LCL after sectioning of the PFL or PT increases the varus laxity but not the isolated section of the PFL and section of the PT. Also, the primary restraint to varus laxity in varus extension was the LCL.
At 30° of flexion, the isolated section of the PFL increased external rotation in varus and the mobility of the lateral tibial plateau, and at 60° of flexion, the entire section of PLC increased varus laxity and external rotation. At 90° of flexion, isolated sectioning of the PFL increased the mobility of the lateral tibial plateau.
The present study, similar to that by Lasmar et al,10 found that the LCL was a varus stabilizer in extension and all degrees of flexion. In contrast, we found that the popliteofibular complex (PFL and PT) also independently stabilized varus at 30° of flexion. Shahane et al24 found that the role of the PFL in varus was maximized at 60°.
No study has found that the popliteofibular ligament complex (PFL and PT) plays a static role in extension, which we also found in our study.10,24 These studies also highlighted the importance of PFL in the control of external rotation at 30° and 60° of flexion. For Pasque et al,20 the PFL had no role in stabilizing external rotation. But the results of this study indicate that the PFL has a specific role in the control of external rotation, especially at 30°. Sugita and Amis,26 Gollehon et al,4 and Veltri et al28 found that the PFL was the dominant anatomic structure in the control of external rotation from 30° to 90° of flexion. We also found that the mobility of the lateral tibial plateau increased with sectioning of the PLC, as did Pearle et al21 and Sugita and Amis.26 In our study, increased external rotation occurred after sectioning of the PFL, even if the PT and LCL were still intact.
Although McCarthy et al15 demonstrated the stabilizing role of the popliteal muscle-tendon unit, a recent study using a navigation system27 questioned whether the popliteus tendon acts as a static stabilizer. In our study, we showed that the popliteal muscle-tendon unit was a static stabilizer of the lateral tibial plateau when coupled with the PFL. So the combined popliteofibular complex (PT + PFL) acts as a stabilizer when the entire complex is intact.
Regarding the reconstruction of the PLC, the technique used is derived from the Schechinger modification of the Larson technique.23 It is technically reproducible and much less invasive than 2 other anatomic reconstruction techniques.11,18 Results on the kinematics of the knee are comparable with those of anatomic reconstructions clinically23,29 and experimentally.22,29 This double–femoral tunnel reconstruction technique is based on the goal of a fibular-based, single-graft reconstruction that replicates the LCL and popliteus anatomy as it relates to the distal femur. This technique was tested in a biomechanical study by Nau et al,16 who found that it restored varus and external rotation laxity at 30° and 90° of flexion. Our study found similar results. The double–femoral tunnel reconstruction of the PLC restored varus laxity at all flexion angles to that of the normal knee.
In our study, the reconstructed knee (ACLR + PLCR) showed no significant difference with the intact knee, as well as to full extension and to all degrees of flexion.
Ho et al5 have shown the efficiency of the Larson technique for PLCR in varus at 0° and 30° of flexion and in external rotation in flexion. We found no difference on varus after ACLR, probably because we preserved the posterior lateral capsule, which is a secondary stabilizer.
Comparison of the ACL-reconstructed knee before and after reconstruction of the PLC demonstrated a significant difference in the stability of varus and external rotation displacement in all degrees of flexion. Many authors have demonstrated that in combined PLC and ACL tears, reconstruction of the PLC reduces the failure rate of ACLR.6,13,19
However, our study has limitations. First, the varus and torsional forces were applied manually, which may induce a performance bias. Second, the ligaments of the PLC were sequentially cut. Consequently, the effect of an isolated LCL or PT rupture was not assessed.
It would also have been interesting to perform the PLC reconstruction first, but then it would not have been possible to compare the results of ACLR without reconstructing the PLC and after reconstruction of the PLC.
Conclusion
We were able to determine the role of both PT and PFL in the control of external rotation and mobility of the lateral tibial plateau at 30°, 60°, and 90° of flexion. We have confirmed that the LCL is the main stabilizer of varus in extension. Using a previously described technique of PLC reconstruction23 that includes the PT, the PFL, and the LCL, kinematics of the knee can be reasonably restored.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Alam M, Bull AM, Thomas Rd, Amis AA. Measurement of rotational laxity of the knee: in vitro comparison of accuracy between the tibia, overlying skin, and foot. Am J Sports Med. 2011;39:2575–2581. [DOI] [PubMed] [Google Scholar]
- 2. Bicos J, Arciero RA. Novel approach for reconstruction of the posterolateral corner using a free tendon graft technique. Sports Med Arthrosc. 2006;14:28–36. [DOI] [PubMed] [Google Scholar]
- 3. Feeley BT, Muller MS, Sherman S, Allen AA, Pearle AD. Comparison of posterolateral corner recpnstructions using computer-assisted navigation. Arthroscopy. 2010;26:1088–1095. [DOI] [PubMed] [Google Scholar]
- 4. Gollehon DL, Torzilli PA, Warren RF. The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg Am. 1987;69:233–242. [PubMed] [Google Scholar]
- 5. Ho EP, Lam MH, Chung MM, et al. Comparison of 2 surgical techniques for reconstructing posterolateral corner of the knee: a cadaveric study evaluated by navigation system. Arthroscopy. 2011;27:89–96. [DOI] [PubMed] [Google Scholar]
- 6. Hufner T, Geerling J, Kfuri M, Jr, et al. Computer-assisted pelvic surgery: registration based on a modified external fixator. Comput Aided Surg. 2003;8:192–197. [DOI] [PubMed] [Google Scholar]
- 7. Hughston JC, Jacobson KE. Chronic posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1985;67:351–359. [PubMed] [Google Scholar]
- 8. Khadem R, Yeh CC, Sadeghi-Therani M, et al. Comparative tracking error analysis of five different optical tracking systems. Comput Aided Surg. 2000;5:98–107. [DOI] [PubMed] [Google Scholar]
- 9. Laprade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. [DOI] [PubMed] [Google Scholar]
- 10. Lasmar RC, Marques de Almeida A, Serbino JW, Jr, Mota Albuquerque RF, Hernandez AJ. Importance of the different posterolateral knee static stabilizers: biomechanical study. Clinics (São Paulo). 2010;65:433–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Levy BA, Stuart MJ, Whelan DB. Posterolateral instability of the knee: evaluation, treatment, results. Sports Med Arthrosc Rev. 2010;18:254–262. [DOI] [PubMed] [Google Scholar]
- 12. Markolf KL, Graves BR, Sigward SM, Jackson SR, McAllister DR. Effects of posterolateral reconstructions on external tibial rotation and forces in a posterior cruciate ligament graft. J Bone Joint Surg Am. 2007;89:2351–2358. [DOI] [PubMed] [Google Scholar]
- 13. Markolf KL, Graves BR, Sigward SM, Jackson SR, McAllister DR. How well do anatomical reconstructions of the posterolateral corner restore varus stability to the posterior cruciate ligament-reconstructed knee? Am J Sports Med. 2007;35:1117–1122. [DOI] [PubMed] [Google Scholar]
- 14. Maynard MJ, Deng X, Wickiewicz TL, Warren RF. The popliteofibular ligament. Rediscovery of a key element in posterolateral stability. Am J Sports Med. 1996;24:311–316. [DOI] [PubMed] [Google Scholar]
- 15. McCarthy M, Camarda L, Wijdicks CA, Johansen S, Engebretsen L, Laprade RF. Anatomic posterolateral knee reconstructions require a popliteofibular ligament reconstruction through a tibial tunnel. Am J Sports Med. 2010;38:1674–1681. [DOI] [PubMed] [Google Scholar]
- 16. Nau T, Chevalier Y, Hagemeiseter N, De Guise JA, Duval N. Comparison of 2 surgical techniques of posterolateral corner reconstruction of the knee. Am J Sports Med. 2005;33:1838–1845. [DOI] [PubMed] [Google Scholar]
- 17. Nielsen S, Helmig P. Posterior instability of the knee joint: an experimental study. Arch Orthop Trauma Surg. 1986;105:121–125. [DOI] [PubMed] [Google Scholar]
- 18. Niki Y, Matsumoto H, Otani T, Enomoto H, Toyama Y, Suda Y. A modified Larson’s method of posterolateral corner reconstruction of the knee reproducing the physiological tensioning pattern of the lateral collateral and popliteofibular ligaments. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. O’Brien SJ, Warren RF, Pavlov H, Panariello R, Wickiewicz TL. Reconstruction of the chronically insufficient anterior cruciate ligament with the central third of the patellar ligament. J Bone Joint Surg Am. 1991;73:278–286. [PubMed] [Google Scholar]
- 20. Pasque C, Noyes FR, Gibbons M, Levy M, Grood E. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br. 2003;85:292–298. [DOI] [PubMed] [Google Scholar]
- 21. Pearle AD, Solomon DJ, Wanich T, et al. Reliability of navigated knee stability examination: a cadaveric evaluation. Am J Sports Med. 2007;35:1315–1320. [DOI] [PubMed] [Google Scholar]
- 22. Rauh PB, Clancy WG, Jr, Jasper LE, Curl LA, Belkoff S, Moorman CT., 3rd Biomechanical evaluation of two reconstruction techniques for posterolateral instability of the knee. J Bone Joint Surg Br. 2010;92:1460–1465. [DOI] [PubMed] [Google Scholar]
- 23. Schechinger SJ, Levy BA, Dajani KA, Shah JP, Herrera DA, Marx RG. Achilles tendon allograft reconstruction of the fibular collateral ligament and posterolateral corner. Arthroscopy. 2009;25:232–242. [DOI] [PubMed] [Google Scholar]
- 24. Shahane SA, Ibbotson C, Strachan R, Bickerstaff DR. The popliteofibular ligament. An anatomical study of the posterolateral corner of the knee. J Bone Joint Surg Br. 1999;81:636–642. [DOI] [PubMed] [Google Scholar]
- 25. Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA., 3rd Ligament length relationships in the moving knee. J Orthop Res. 1998;6:593–610. [DOI] [PubMed] [Google Scholar]
- 26. Sugita T, Amis AA. Anatomic and biomechanical study of the lateral collateral and popliteofibular ligaments. Am J Sports Med. 2001;29:466–472. [DOI] [PubMed] [Google Scholar]
- 27. Thaunat M, Pioger C, Chatellard R, Conteduca J, Khaleel A, Sonnery-Cottet B. The arcuate ligament revisited: role of the posterolateral structures in providing static stability in the knee joint. Knee Surg Sports Traumatol Arthrosc. 2014;22:2121–2127. [DOI] [PubMed] [Google Scholar]
- 28. Veltri DM, Deng XH, Torzilli PA, Maynard MJ, Warren RF. The role of the popliteofibular ligament in stability of the human knee. A biomechanical study. Am J Sports Med. 1996;24:19–27. [DOI] [PubMed] [Google Scholar]
- 29. Yoon KH, Lee JH, Bae DK, Song SJ, Chung KY, Park YW. Comparison of clinical results of anatomic posterolateral corner reconstruction for posterolateral rotatory instability of the knee with or without popliteal tendon reconstruction. Am J Sports Med. 2011;39:2421–2428. [DOI] [PubMed] [Google Scholar]