Abstract
Background:
Fresh osteochondral allograft (OCA) transplantation is an effective treatment for osteochondral defects. Some patients require further surgical intervention, such as total knee arthroplasty (TKA). The effects of prior OCA transplantation on TKA outcomes are unknown.
Purpose:
This study evaluated TKA failure rates after long-term follow-up and identified factors that may have contributed to an inferior outcome. Its aims were to (1) assess if having a prior OCA transplantation would increase the surgical complications of the subsequent TKA, (2) measure the infection and failure rates following TKA, (3) ascertain subjective outcomes scores from patients with intact TKA at latest follow-up, and (4) identify potential factors that contributed to inferior outcomes.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 35 patients who underwent TKA after OCA were identified. Pain, symptoms, function, and quality of life were evaluated using the Knee Society Function score and Knee injury and Osteoarthritis Outcome Score (KOOS). Associations between outcomes scores versus total number of surgeries before TKA were assessed using Spearman correlation. Patient characteristics (age, sex, total OCA area, presentation of osteoarthritis, and number of surgeries before TKA) were calculated between failures and nonfailures.
Results:
For patients with TKA surviving at latest follow-up (n = 24), mean follow-up time was 9.2 ± 4.3 years after TKA and 16.1 ± 5.2 years after OCA. While TKA after OCA did not present a technical challenge in the operating room, there was a high failure rate (31.4%). Activities of daily living, as measured on KOOS, were negatively correlated with total number of surgeries before TKA (ρ2 = –0.5, P = .041). Patient age and number of surgeries before TKA influenced the failure rate, while sex and OCA area did not appear to be factors associated with inferior outcomes.
Conclusion:
Patients with multiple knee operations before TKA were more likely to experience functional limitations or TKA failure. The patients who experienced TKA failure were part of a challenging subset of young patients treated with numerous orthopaedic procedures, and while these patients had inferior results with TKA after OCA, the OCA transplantation extended the time before a TKA was required without adding surgical complications.
Keywords: osteochondral allograft, total knee arthroplasty, outcomes, revision rates
Fresh osteochondral allograft (OCA) transplantation is an effective, durable treatment option for isolated femoral or tibial osteochondral defects.2,9,12,16–19,22,38 Many studies have shown good to excellent results in 70% to 85% of patients at 10-year follow-up2,19,38 with documented histologic viability of the transplanted chondrocytes.40 OCA survivorship is 95% at 5 years, 71% to 89% at 10 years, and 65% to 76% at 15 to 20 years in patients treated for femoral condyle lesions, posttraumatic knee defects, osteonecrosis, and osteochondritis dissecans.9,13,17,19,28 While a majority of patients benefit from OCAs, often times, OCAs can fail or result in inferior clinical outcomes (such as the progression of joint arthritis) and subsequently require further surgical intervention.
Total knee arthroplasty (TKA), a surgical procedure that replaces native joint tissue with a mechanical implant to bear load and facilitate joint movement, is often used to treat end-stage osteoarthritis with clinical success. TKA has excellent results and survivorship, as reported in many studies.11,14,15,21,35,37 A typical patient of age ≥65 years is recommended, and patients experience a reduction in symptoms and an overall improvement in quality of life. In contrast, younger patients often have a high level of residual symptoms after TKA and higher revision rates versus older patients.33 In younger patients, TKA survivorship of an average of 15 years means a revision will likely be required during an individual’s lifetime. Specifically, patients younger than 40 years can only expect a 50% chance of good to excellent Knee Society function scores and a revision rate of 12.5% at 8 years.29
Results from revision TKA are documented to be inferior to those from primary TKA.8 If an OCA can allow a patient to function well for 10 to 15 years and avoid TKA, that patient may benefit from a decreased need for revision during his or her lifetime. Conversely, if OCA makes TKA more difficult or the patient has a worse outcome than a patient who has never had an allograft, perhaps the patient’s interest would be better served by proceeding directly to a TKA. A large number of patients have undergone osteochondral allografting of the knee at our institution. Here, we analyzed 35 such patients who had an OCA followed by TKA either for allograft failure or progression of osteoarthritis.
The purpose of this study was to evaluate the outcomes of TKA after isolated OCA transplantation. Specifically, we aimed to (1) assess whether having a prior OCA transplantation would increase the surgical complications of the subsequent TKA; (2) measure the infection and failure rates following the TKA; (3) ascertain pain, symptoms, function, and quality of life among patients whose TKA was still intact at latest follow-up; and (4) identify potential factors that may have contributed to an inferior outcome.
Materials and Methods
After receiving institutional review board approval, we identified 39 patients (39 knees) who had TKA after OCA transplantation using our outcomes database, which tracks patient outcomes by obtaining long-term follow-up information by phone, mail, or office visits. Patients with osteotomy or infection prior to TKA were excluded. Patients who qualified for workers’ compensation were not excluded, and this information was not analyzed in the study. Four patients (4 knees) did not have a minimum 1-year follow-up and were excluded from the study. The remaining 35 patients (35 knees) comprised the study population. The mean age at time of TKA was 47.8 ± 11.5 years (range, 30-73 years), and 68.6% were female.
Patients presented for allograft transplantation because of osteoarthritis (n = 11 knees), degenerative chondral lesion (n = 8 knees), traumatic chondral injury (n = 8 knees), avascular necrosis (n = 4 knees), osteochondritis dissecans (n = 2 knees), and osteochondral fracture (n = 2 knees). Allografts were performed on various sites and, in some cases, multiple sites. More than 1 site was grafted (multifocal or bipolar allografts) in 20 patients, whereas 15 patients were treated with an allograft at a single site, including 1 lateral femoral condyle, 10 medial femoral condyles, 3 patellae, and 1 trochlea. Multifocal and bipolar lesions were treated with allografts within many regions of the knee, including at both condyles (4 knees), at the condyle and tibial plateau (6 lateral, 4 medial), at the condyle and patella (1 lateral, 1 medial), and in regions involving the trochlea (4 with patella, 1 with medial condyle). The mean total area of the allograft(s) was 14.7 cm2 (range, 1.5-34.8 cm2). The average time from OCA transplantation to TKA was 5.9 years (range, 0.5-19.7 years) for all 35 patients. Patients had an average of 4 surgeries (range, 1-14 surgeries) on the affected knee prior to TKA. Although all allograft procedures were performed at our institution, the subsequent TKAs were performed by several different surgeons; 8 patients (23%) had their TKA performed at our institution, while 27 patients (77%) elected to undergo surgery at an institution closer to their homes. The need for stems, augments, exposure problems, and bone graft were evaluated as dictated in the operative notes when available.
Follow-up was conducted by contacting patients via telephone. Incidence of postoperative infection and reoperations were assessed. Failure of the TKA was defined as revision arthroplasty or a reoperation resulting from a complication of the arthroplasty. For cases with successful TKA, pain, symptoms, function, and quality of life were evaluated using the Knee Society Function (KS-F) score and the Knee injury and Osteoarthritis Outcome Score (KOOS). Associations between outcomes scores (KS-F, and KOOS symptoms, pain, activities of daily living, sports and recreation function, and quality of life) versus total number of surgeries before TKA were assessed using Spearman correlation. The association between the total number of surgeries before TKA and TKA failure was assessed using an independent-samples t test. Survivorship of TKA, using revision or reoperation as the endpoint, was computed using the Kaplan-Meier method.
Patient characteristics (age, sex, total OCA area, presentation of osteoarthritis, and number of surgeries before TKA) were calculated between TKA failures and nonfailures. Differences between the 2 groups were evaluated by independent-samples t tests (for age), the Mann-Whitney U test (for number of surgeries before TKA and total OCA area), and Fisher exact test (for sex and presentation of osteoarthritis).
Results
Surgical Complications
Review of the available operative reports (n = 22) revealed that there was no documented need for extended exposure for any patient. However, 1 patient (2.9%) required a stem and augmentation for revision from a unicompartmental knee arthroplasty to a TKA, subsequent to the OCA. In addition, 1 patient (2.9%) required bone graft to supplement a femoral condyle defect at the time of the subsequent TKA, and a primary implant was used.
Infection and Failure Rates
The postoperative infection rate was 5.7%, as 2 of 35 patients developed an infection after TKA. Of these infected patients, 1 was treated by incision and drainage with a polyethylene liner exchange, and the other eventually required an above-knee amputation. Both patients had multiple surgeries prior to their TKA, with 4 surgeries and 9 surgeries, respectively.
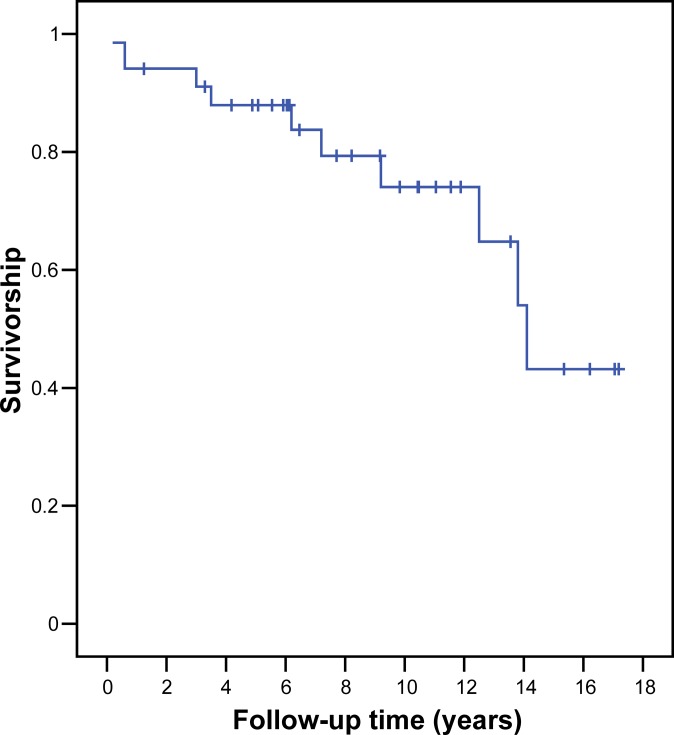
Eleven of 35 (31.4%) TKAs failed, requiring revision arthroplasty in 10 patients and an above-knee amputation in 1 patient (Table 1). Failure was due to pain in 4 patients (36%), loosening in 3 patients (27%), polyethylene wear in 2 patients (18%), and infection in 2 patients (18%). The mean time to failure was 7.0 ± 5.2 years (range, 0.2-14.1 years). Survivorship was 74% at 10 years (Figure 1).
TABLE 1.
Patient Characteristics and Operative Details Among Patients With a Failed TKA After OCA Transplantation (n = 11)a
| Sex | Reason for OCA | OCA Area, cm2 | Age at TKA, y | Surgeries Before TKA, n | Time From TKA to TKA Failure, y | Failure Type | Reason for TKA Failure |
|---|---|---|---|---|---|---|---|
| F | TCI | 8.0 | 40 | 2 | 3.5 | TKA revision | Pain |
| F | DCL | 8.8 | 41 | 4 | 6.2 | TKA revision | Pain |
| F | OA | 20.0 | 44 | 14 | 0.6 | TKA revision | Pain |
| F | DCL | 12.0 | 49 | 5 | Unknown | TKA revision | Pain |
| F | OA | 30.0 | 31 | 4 | 13.8 | TKA revision | Loosening |
| F | OA | 3.0 | 34 | 5 | 14.1 | TKA revision | Loosening |
| M | TCI | 7.5 | 48 | 3 | 3.0 | TKA revision | Loosening |
| M | OA | 21.0 | 36 | 2 | 12.5 | TKA revision | Polyethylene wear |
| M | OA | 14.2 | 46 | 6 | 9.2 | TKA revision | Polyethylene wear |
| F | TCI | 6.9 | 46 | 9 | 7.2 | Amputation | Infection |
| F | OA | 26.0 | 51 | 4 | 0.2 | TKA revision | Infection |
aDCL, degenerative chondral lesion; F, female; M, male; OA, osteoarthritis; OCA, osteochondral allograft; TCI, traumatic chondral injury; TKA, total knee arthroplasty.
Figure 1.
Kaplan-Meier curve of 35 knees that underwent total knee arthroplasty following osteochondral allograft transplantation.
Pain, Symptoms, Function, and Quality of Life
Twenty-four of 35 (69%) TKAs were still intact at latest follow-up. The mean follow-up time was 9.2 ± 4.3 years (range, 3.3-17.2 years) after TKA and 16.1 ± 5.2 years (range, 7.0-27.4 years) after OCA transplantation; thus, the mean time from OCA transplantation to TKA was 6.9 years (range, 0.5-19.7 years). At latest follow-up, subjective outcomes scores were available for 17 to 21 patients and were mediocre, demonstrating the adequacy of such TKA procedures to treat such a challenging subset of patients. Mean KS-F was 73.3 ± 23.9, and the mean scores on KOOS symptoms, pain, and ADL ranged from 78.0 to 81.1; KOOS sports/recreation and quality of life were lower, with means ranging from 46.8 to 55.7, but this is expected given the nature of those scales.
The majority of patients whose TKAs were still intact at latest follow-up (87.5%) had multiple surgeries (mean, 3.1 ± 1.4 procedures; range, 1-6 procedures) in addition to the OCA transplantation performed on their knees prior to TKA. Activities of daily living, as measured using KOOS, were negatively correlated with total number of surgeries before TKA (ρ2 = –0.5, P = .041). There was a negative correlation between KOOS pain, sports/recreation, and quality of life scores and the number of surgeries before TKA (all ρ2 = –0.4 to –0.5), but they were not statistically significant (P = .095, .112, and .100, respectively). KS-F scores and KOOS symptoms scores were not correlated with number of surgeries before TKA.
Patient age and number of surgeries before TKA influenced the failure rate, while sex and OCA area did not appear to be factors associated with inferior outcomes (Table 2). The patients with failed TKAs were younger than patients with nonfailures (42.8 vs 50.2 years, P < .05). In addition, patients with failed TKAs had twice as many previous surgeries than patients with nonfailures (5.9 vs 3.1 procedures, P < .01). Patients with failed TKAs tended to have been treated with OCA for osteoarthritis more often than patients with nonfailures (55% of patients vs 21% of patients, P = .06). Sex and OCA area did not vary between patients with failed and nonfailed TKAs (both P > .5).
TABLE 2.
Patient Characteristics and Operative Details Among TKA Failures and Nonfailuresa
| Characteristic | TKA Failures (n = 11) | TKA Nonfailures (n = 24) | P Value |
|---|---|---|---|
| Age at TKA, y, mean (SD) | 42.8 (6.5) | 50.2 (12.6) | .030 |
| Female, % | 72.7 | 66.7 | .521 |
| Osteochondral allograft area, total cm2, mean (SD) | 13.8 (9.3) | 15.2 (9.1) | .695 |
| Presenting for OCA due to osteoarthritis, % | 54.5 | 20.8 | .062 |
| Number of surgeries before TKA, mean (SD) | 5.9 (3.4) | 3.1 (1.4) | .003 |
aOCA, osteochondral allograft; TKA, total knee arthroplasty.
Discussion
The results demonstrate that TKA after OCA transplantation did not present added technical challenges and that failures of such patients were associated with persistent pain, the total number of surgeries prior to TKA, and patient age. Overall, the outcome scores were negatively correlated with the number of surgeries prior to TKA. These results suggest that younger patients that underwent multiple surgeries to address issues with persistent pain were at a higher risk for failed TKA than patients who had fewer surgeries prior to TKA and were older. Failure of TKA may also be related to the disease state, specifically if OCA transplantation was used to treat osteoarthritis, but further studies with a larger cohort are needed to investigate the relationship among disease state, treatment outcomes, and failure rates.
Examining the outcomes of TKA after isolated OCA transplantation required consideration of several issues. Even with a cohort number that was relatively small, and incomplete follow-up on some (approximately one third) patients’ operative reports, there were clear associations between the number of previous surgeries and outcomes, and no added technical challenges within the subset. However, while limited conclusions on the complexity of the surgical procedure can be made and we were unable to filter out any bias from the operative reports, the lack of added technical challenges reported suggests that the OCA procedure did not significantly impact the subsequent TKA in the operating room. While postoperative radiographs may be able to definitely determine if there was a malposition of the TKA components, we chose to use clinical outcomes and not radiographic ones for postoperative evaluations as the subjective pain measure was a more useful metric of revision in this cohort, and persistent pain contributed to the patient’s need for surgical intervention. While TKAs were performed by different institutions, the indications to convert the OCA to a TKA were similar. Once that decision was made, it was most reasonable to have the TKA performed at the patient’s home institution. This is the difficulty with following a group that has traveled to an institution for a very specific intervention (OCA transplantation) but did not return to the same institution for TKA, choosing instead to stay closer to home.
This subset of patients represents an important experience to guide decision making in the cartilage repair treatment algorithm, as the implications for subsequent TKA are unknown and relevant to alleviate patient inquiries. The TKA after OCA cohort was a unique group, being both very young and having had multiple surgeries for various reasons before and after TKA. Selecting patients of similar indications was difficult and a limitation of this study; however, the broad scope of disease for the patients identified here suggests the value of OCA transplantation as a salvage procedure to extend the time before TKA and the need to study these procedures in tandem. While it is difficult to conclude the primary cause of the TKA failure, it was likely that similar results may occur in young patients with multiple open surgeries irrespective of the type of procedures performed. This conclusion suggests that OCA transplantation is useful for salvage situations to extend the time before TKA. However, further studies examining these 2 groups matched for age, indication, and follow-up are needed to make any further conclusions about the direct effect of OCA transplantation on TKA failure.
Total knee arthroplasty after isolated OCA transplantation does not appear to present a significant technical challenge during surgery. No patient required stems, augments, or an extended exposure for conversion of their OCA to a TKA. While 1 patient required a stem and augmentation for revision from a unicompartmental knee arthroplasty to a TKA (subsequent to the OCA) and another patient required bone graft, the TKA procedures were not affected by these technical challenges. The implantation of OCA, when performed without osteotomy, does not change the alignment of the knee or penetrate deeply into the subchondral bone. Therefore, the straightforward conversion to TKA is not surprising. The high failure rate reported in this study was surprising given that the conversion to TKA was straightforward in all patients. This suggests that patient factors, especially number of previous surgeries, rather than technical reasons for revision of the TKA may influence outcomes.
The high failure rate reported in this study (31.4%) was consistent with the high rates reported in the literature (17%) for outcomes of TKA after OCA transplantation.31 In a previous report of 33 patients, most patients underwent osteotomy in addition to the OCA transplantation (12 high tibial and 6 distal femoral)31; thus, the sample size of the remaining patients who did not undergo simultaneous osteotomy at the time of OCA transplantation was limited. Because a previous osteotomy has been shown to increase the difficulty of a subsequent TKA,25,30,32 the authors concluded that the outcomes of these patients were influenced more by the osteotomy than the allograft. In addition, the large number of patients with multifocal and bipolar lesions who were treated here (n = 20) may have contributed to the poor failure rates, as larger lesions covering more than 1 surface often have inferior outcomes versus isolated lesions when treated with OCA.3,6 The high failure rates reported suggest that we need to further evaluate which factors influence repair outcomes.
The relatively mediocre outcomes scores in our TKA after OCA transplantation cohort may be secondary to the patient population. Patients were young (mean age, 47.8 years) and had multiple previous surgeries prior to TKA (mean, 4 procedures). Patients who are younger at the time of their TKAs have been shown to have more pain and lower outcomes scores than older patients.5,8,39 In addition, younger patients were more likely to be revised for reasons other than infection,24 and early revisions in young patients had worse outcomes versus late revisions in older patients.20 According to the Finnish registry, overall survival rate at 5 years in patients younger than 55 years was significantly lower than the survival rate for patients older than 65 years (92% vs 97%, respectively).24 In our study, more than one third of the patients undergoing revision TKA were revised because of persistent pain, which was consistent with high levels of residual pain following TKA in young patients.33 If these patients are excluded from the analysis, the overall revision rate would be 15%, a number more consistent with revision rates in younger patients and with a previous study on TKA after OCA transplantation patients, which had a revision rate of 17%.31 A psychosocial element may be present in this cohort, with persistent pain being an important reason for revision TKA. The poor subjective scores reported may be influenced by the number of workers’ compensation patients treated, as, at the time of the study, about one third of patients undergoing OCA transplantation qualified for workers’ compensation, although the exact number of patients who qualified for workers’ compensation was unknown. Workers’ compensation patients often have worse outcomes than non–workers’ compensation patients.4,7,30 Patients undergoing TKA for a workers’ compensation case had lower postoperative Knee Society scores compared with the non–workers’ compensation group (64 vs 93 points, respectively)30 and significantly worse scores for subjective indices (pain, function), but not for objective indices, after TKA when compared with non–workers’ compensation patients.4
The infection rate in TKA after OCA transplantation was 5%, higher than the rate of 1% to 2% for a primary TKA.23,26,27 However, given the small number of patients studied, conclusions from this analysis are limited. Only 2 patients developed infection prior to TKA, and both patients had undergone multiple prior operations on the knee, with an average of 4 procedures (range, 1-14 procedures) prior to TKA. No study has evaluated outcomes of TKA after multiple prior operations, but outcomes of patients undergoing TKA after open reduction and internal fixation for a tibial plateau fracture have been documented to have lower outcomes scores and higher revision and infection rates.36 Patients undergoing TKA after prior tibial or femoral osteotomy have also been documented to have lower outcomes scores and higher infection and revision rates.5,30,32 Even patients undergoing knee arthroscopy prior to TKA have been documented to have a higher revision rate, with a survival rate of 87% after 10 years compared with 98% in patients without previous surgery.34
Conclusion
Total knee arthroplasty after isolated OCA transplantation does not appear to present a significant technical challenge during surgery. However, outcomes for patients undergoing TKA after OCA transplantation are inferior to standard TKA patients reported in the literature.1,10 The infection rate for TKA after OCA transplantation was higher than historical controls but may be related to the numerous previous surgeries that these patients had experienced and the small sample size. Overall, we suggest that a previous OCA surgery prior to TKA may not directly affect revision rate and outcomes, and the number of open surgeries may be a more relevant variable than the type of procedure. The patients who experienced TKA failure were part of a challenging subset who were not made better by any of the orthopaedic procedures, including OCA transplantation, TKA, or other surgical procedures. Thus, while complications and revisions may occur in these young patients, the OCA transplantation did extend the time before requiring a TKA without leading to additional technical challenges.
Acknowledgment
The authors thank Julie McCauley, MPHc, for her help with data analysis, and Andrea Pallante-Kichura, PhD, for technical writing assistance.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was supported by a grant from Scripps Clinic Medical Group.
References
- 1. Archibeck MJ, White RE, Jr; Council of Musculoskeletal Specialty Societies, American Academy of Orthopaedic Surgeons. What’s new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2004;86-A:1839–1849. [DOI] [PubMed] [Google Scholar]
- 2. Aubin PP, Cheah HK, Davis AM, Gross AE. Long-term follow-up of fresh femoral osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res. 2001;(391 suppl):318–327. [DOI] [PubMed] [Google Scholar]
- 3. Beaver RJ, Mahomed M, Backstein D, Davis A, Zukor DJ, Gross AE. Fresh osteochondral allografts for post-traumatic defects in the knee. A survivorship analysis. J Bone Joint Surg Br. 1992;74:105–110. [DOI] [PubMed] [Google Scholar]
- 4. Brinker MR, Savory CG, Weeden SH, Aucoin HC, Curd DT. The results of total knee arthroplasty in workers’ compensation patients. Bull Hosp Jt Dis. 1998;57:80–83. [PubMed] [Google Scholar]
- 5. Carr AJ, Robertsson O, Graves S, et al. Knee replacement. Lancet. 2012;379:1331–1340. [DOI] [PubMed] [Google Scholar]
- 6. Chu CR, Convery FR, Akeson WH, Meyers M, Amiel D. Articular cartilage transplantation: clinical results in the knee. Clin Orthop Relat Res. 1999;(360):159–168. [PubMed] [Google Scholar]
- 7. de Beer J, Petruccelli D, Gandhi R, Winemaker M. Primary total knee arthroplasty in patients receiving workers’ compensation benefits. Can J Surg. 2005;48:100–105. [PMC free article] [PubMed] [Google Scholar]
- 8. Elson DW, Brenkel IJ. Predicting pain after total knee arthroplasty. J Arthroplasty. 2006;21:1047–1053. [DOI] [PubMed] [Google Scholar]
- 9. Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907–914. [DOI] [PubMed] [Google Scholar]
- 10. Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86-A:963–974. [DOI] [PubMed] [Google Scholar]
- 11. Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;(345):79–86. [PubMed] [Google Scholar]
- 12. Garrett JC. Fresh osteochondral allografts for treatment of articular defects in osteochondritis dissecans of the lateral femoral condyle in adults. Clin Orthop Relat Res. 1994;303:33–37. [PubMed] [Google Scholar]
- 13. Ghazavi MT, Pritzker KP, Davis AM, Gross AE. Fresh osteochondral allografts for post-traumatic osteochondral defects of the knee. J Bone Joint Surg Br. 1997;79:1008–1013. [DOI] [PubMed] [Google Scholar]
- 14. Gill GS, Mills DM. Long-term follow-up evaluation of 1000 consecutive cemented total knee arthroplasties. Clin Orthop Relat Res. 1991;(273):66–76. [PubMed] [Google Scholar]
- 15. Goldberg VM, Figgie MP, Figgie HE, Heiple KM, Sobel M. Use of total condylar knee prosthesis for treatment of osteoarthritis and rheumatoid arthritis. Long-term results. J Bone Joint Surg Am. 1988;1988:802–811. [PubMed] [Google Scholar]
- 16. Görtz S, Bugbee WD. Allografts in articular cartilage repair. Instr Course Lect. 2007;56:469–480. [PubMed] [Google Scholar]
- 17. Görtz S, De Young AJ, Bugbee WD. Fresh osteochondral allografting for steriod-associated osteonecrosis of the femoral condyles. Clin Orthop Relat Res. 2010;468:1269–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gross AE, Kim W, Las Heras F, Backstein D, Safir O, Pritzker KP. Fresh osteochondral allografts for posttraumatic knee defects: long-term followup. Clin Orthop Relat Res. 2008;466:1863–1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gross AE, Shasha N, Aubin P. Long-term follow-up of the use of fresh osteochondral allografts for posttraumatic knee defects. Clin Orthop Relat Res. 2005;(435):79–87. [DOI] [PubMed] [Google Scholar]
- 20. Hardeman F, Londers J, Favril A, Witvrouw E, Bellemans J, Victor J. Predisposing factors which are relevant for the clinical outcome after revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:1049–1056. [DOI] [PubMed] [Google Scholar]
- 21. Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am. 1979;61:173–180. [PubMed] [Google Scholar]
- 22. Jamali AA, Emmerson BC, Chung C, Convery FR, Bugbee WD. Fresh osteochondral allografts: results in the patellofemoral joint. Clin Orthop Relat Res. 2005;(437):176–185. [PubMed] [Google Scholar]
- 23. Jamsen E, Varonen M, Huhtala H, et al. Incidence of prosthetic joint infections after primary knee arthroplasty. J Arthroplasty. 2010;25:87–92. [DOI] [PubMed] [Google Scholar]
- 24. Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T. Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthoplasty Register. Acta Orthop. 2010;81:413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Katz MM, Hungerford DS, Krackow KA, Lennox DW. Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1987;69:225–233. [PubMed] [Google Scholar]
- 26. Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J. Infection burden for the hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991. [DOI] [PubMed] [Google Scholar]
- 27. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27:61–65. [DOI] [PubMed] [Google Scholar]
- 28. Levy YD, Gortz S, Pulido PA, McCauley JC, Bugbee WD. Do fresh osteochondral allografts successfully treat femoral condyle lesions? Clin Orthop Relat Res. 2013;471:231–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lonner JH, Hershman S, Mont M, Lotke PA. Total knee arthroplasty in patients 40 years of age and younger with osteoarthritis. Clin Orthop Relat Res. 2000;(380):85–90. [DOI] [PubMed] [Google Scholar]
- 30. Mont MA, Antonaides S, Krackow KA, Hungerford DS. Total knee arthroplasty after failed high tibial osteotomy. A comparison with a matched group. Clin Orthop Relat Res. 1994;(299):125–130. [PubMed] [Google Scholar]
- 31. Morag G, Kulidjian A, Zalzal P, Shasha N, Gross AE, Backstein D. Total knee replacement in previous recipients of fresh osteochondral allograft transplants. J Bone Joint Surg Am. 2006;88:541–546. [DOI] [PubMed] [Google Scholar]
- 32. Nelson CL, Saleh KJ, Kassim RA, et al. Total knee arthroplasty after varus osteotomy of the distal part of the femur. J Bone Joint Surg Am. 2003;85-A:1062–1065. [DOI] [PubMed] [Google Scholar]
- 33. Parvizi J, Nunley RM, Berend KR, et al. High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res. 2014;472:133–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Piedade SR, Pinaroli A, Servien E, Neyret P. Is previous knee arthroscopy related to worse results in primary total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2009;17:328–333. [DOI] [PubMed] [Google Scholar]
- 35. Ranawat CS, Flynn WFJ, Saddler S, Hansraj KK, Maynard MJ. Long-term results of the total condylar knee arthroplasty. A 15-year survivorship study. Clin Orthop Relat Res. 1993;286:94–102. [PubMed] [Google Scholar]
- 36. Saleh KJ, Sherman P, Katkin P, et al. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1144–1148. [DOI] [PubMed] [Google Scholar]
- 37. Scuderi GR, Insall JN, Windsor RE, Moran MC. Survivorship of cemented knee replacements. J Bone Joint Surg Br. 1989;71:798–803. [DOI] [PubMed] [Google Scholar]
- 38. Shasha N, Aubin PP, Cheah HK, Davis AM, Agnidis Z, Gross AE. Long-term clinical experience with fresh osteochondral allografts for articular knee defects in high demand patients. Cell Tissue Bank. 2002;3:175–182. [DOI] [PubMed] [Google Scholar]
- 39. Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466:2717–2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Williams SK, Amiel D, Ball ST, et al. Analysis of cartilage tissue on a cellular level in fresh osteochondral allograft retrievals. Am J Sports Med. 2007;35:2022–2032. [DOI] [PubMed] [Google Scholar]