Abstract
Background:
Achilles tendon ruptures are one of the most commonly treated injuries by orthopaedic surgeons and general practitioners. Achilles tendon ruptures have classically been thought to affect the middle-aged “weekend warrior” participating in basketball, volleyball, soccer, or any other ground sport that requires speed and agility; however, with a more active elderly population, these tears are becoming more common in older patients.
Purpose:
To report trends in nonoperative and operative treatment of Achilles tendon tears in the United States from 2005 to 2011 in patients registered with a large Medicare database.
Study Design:
Descriptive epidemiological study.
Methods:
Patients who underwent nonoperative and operative treatment of Achilles tendon ruptures by either primary repair or primary repair with graft (International Classification of Diseases 9 [ICD-9] diagnosis code 727.67, Current Procedural Terminology [CPT] codes 27650 and 27652) for the years 2005 to 2011 were identified using the PearlDiver Medicare Database. Demographic and utilization data available within the database were extracted for patients who underwent nonoperative as well as operative treatment for Achilles tendon ruptures. Statistical analysis involved Student t tests, chi-square tests, and linear regression analyses, with statistical significance set at P < .05.
Results:
From 2005 to 2011, there were a total of 14,127 Achilles tendon ruptures. Of these, 9814 were managed nonoperatively, 3531 were treated with primary repair, and 782 were treated with primary repair with graft. The incidence of Achilles tendon increased from 0.67 per 10,000 in 2005 to 1.08 per 10,000 in 2011 (P < .01). There was no significant difference in the number of Achilles ruptures between males (6636) and females (7582) (P > .05). There was an increase in the overall number of Achilles tendon ruptures over time (1689 in 2005 compared with 2788 in 2011; P < .001) but no difference in the percentage of Achilles ruptures treated operatively (P > .05). Older patients were more likely to be treated nonoperatively (P < .05). No differences in operative versus nonoperative treatment were seen between yearly quarter (P > .05), sex (P > .05), or region (P > .05).
Conclusion:
The incidence of Achilles tendon ruptures is increasing with time, but the trend in operative and nonoperative treatment has not changed between 2005 and 2011. Older patients, especially those older than 85 years, are more likely to be treated nonoperatively. No differences in treatment patterns were seen based on sex, region, or yearly quarter.
Keywords: Achilles tendon, operative treatment, epidemiology, reconstruction, repair, graft, nonoperative, incidence
Achilles tendon ruptures are one of the most commonly treated injuries by orthopaedic surgeons and general practitioners.9 Approximately 75% of Achilles tendon tears occur in recreational athletes.9 Achilles tendon ruptures have classically been thought to affect the middle-aged “weekend warrior” participating in basketball, volleyball, soccer, or any other ground sport that requires speed and agility; however, with a more active elderly population, these tears are becoming more common in older patients.3,15,16
Achilles tendon ruptures often result from lack of stretching and warm-up prior to vigorous strenuous activity, fatigue, or loss of proprioception.9,16 Several studies have reported no significant difference between operative and nonoperative treatment in functional outcomes in the majority of patients, although time to return to work slightly favors operative intervention.6,20 However, differences can be seen in high-level athletes as it pertains to explosiveness when initiating running, as well as in other general lower extremity strength parameters.5,14 According to a recent review of National Basketball Association (NBA) players in the United States who underwent Achilles tendon repair, these players do not return to their preinjury performance level, and their performance declines compared with controls.1 There is also a higher rate of rerupture reported with nonoperative management (8.8% to 12.6%) compared with operative intervention (3.6%).7,17
Patients often choose operative treatment because of the lower reported rerupture rates as well as slight increase in strength and faster rehabilitation.5 There are many options for operative treatment, including open versus minimally invasive procedures. Recent data have shown no differences between these 2 treatment modalities.8 However, despite the procedure being relatively technically straightforward, there are many complications that can arise from operative treatment that are not present with nonoperative treatment, most notably sural nerve injury and wound healing problems.5,7,12
Given the increasing activity level among the US elderly and the variety of treatment options for Achilles tendon ruptures, the purposes of this study were to determine the incidence of Achilles tendon ruptures in the United States from 2005 to 2011 among Medicare beneficiaries and also to analyze the trends in Achilles tendon rupture treatment. We hypothesized that there will be an increase in the number of Achilles tendon ruptures over time, with no difference in the percentage of tears that are treated operatively and nonoperatively. We also hypothesized that there will be no significant difference in operative versus nonoperative treatment based on sex, region, or yearly quarter.
Methods
The PearlDiver Patient Record Database (PearlDiver Inc) was queried for the years 2005 to 2011. The PearlDiver database is a publicly available Health Insurance Portability and Accountability Act (HIPAA)–compliant national database compiled from a collection of Medicare records. The database has more than 2 billion individual patient records and contains Current Procedural Terminology (CPT) and International Classification of Diseases 9 (ICD-9) codes related to orthopaedic procedures, as well as demographic data such as age and sex. From 2005 to 2011, the database captured an average of 25.6 million patients per year.
The number of patients having records of ICD-9 code 727.67 (nontraumatic rupture, either partial or complete, of Achilles tendon) was recorded. Of these, the number of patients with CPT codes 27650 (Achilles tendon rupture surgery; primary repair) and 27652 (Achilles tendon rupture surgery; primary repair with graft) were recorded. Linear regression was utilized to compare trends from years 2005 through 2011. Student t tests and chi-square tests were used to compare the proportion of patients based on the other demographic parameters in the PearlDiver database. Statistical significance was set as P < .05.
Results
There were a total of 14,127 Achilles tendon ruptures recorded between 2005 and 2011. Of these, 9814 were managed nonoperatively, 3531 were treated with primary repair, and 782 were treated with primary repair and graft reconstruction. There was no significant difference in the overall number of Achilles ruptures between males (6636) and females (7582) (P > .05) (Figure 1A), nor was there a difference between the number of Achilles tendon ruptures treated operatively between males (2145) and females (2136) (P > .05) (Figure 1B). The percentage of tears treated operatively were 29% in females versus 32% in males.
Figure 1.
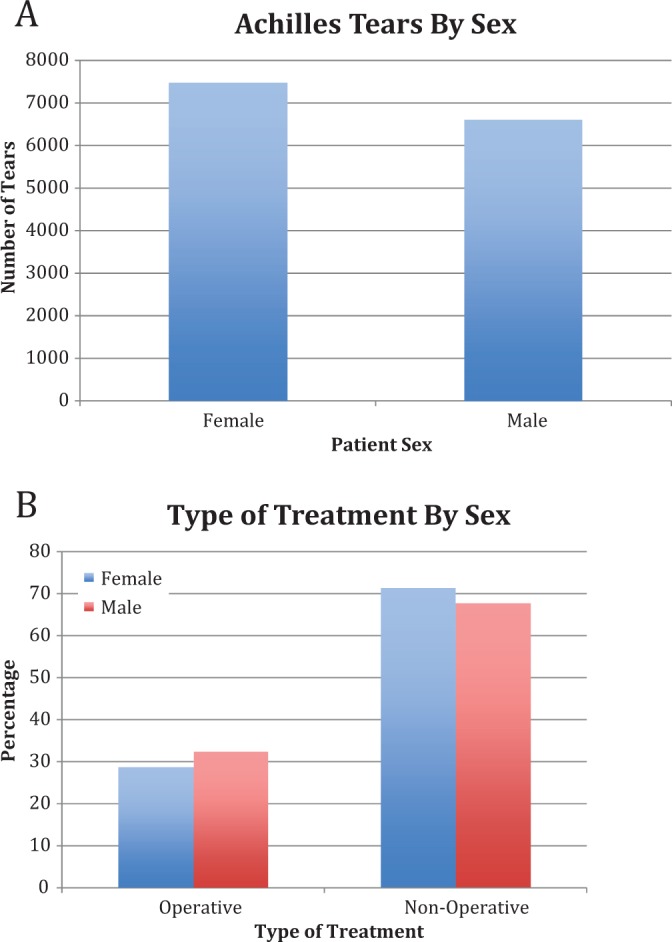
(A) Overall number of Achilles tears for males and females from 2005 to 2011. There was no significant difference between number of tears in males and females (P > .05). (B) Type of treatment for Achilles tendon ruptures between males and females from 2005 to 2011. There was no significant difference between percentage of tears treated operatively between males and females (P > .05).
After the age of 65 years, the number of Achilles tendon ruptures decreased in a significant way with increasing age (P < .001) (Figure 2A). There were 4295 Achilles tendon ruptures in patients aged 65 to 69 years, while in patients >84 years there were only 567 tears during the period under study. Likewise, there was a significant increase in the proportion of Achilles tendon ruptures treated nonoperatively with increasing age (P < .01) (Figure 2B). Approximately 36% of Achilles tendon tears were treated operatively in patients aged 65 to 69 years, while <10% were treated operatively in patients older than 84 years.
Figure 2.
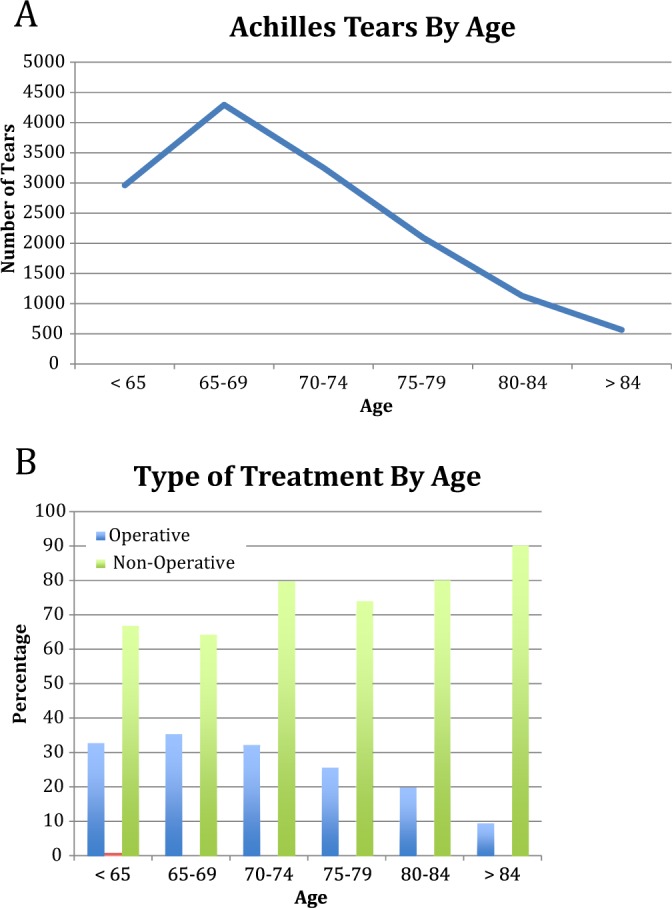
(A) Overall number of Achilles tears by age from 2005 to 2011. A significant decrease was seen in the number of tears in each age group after age 65 years (P < .001). (B) Type of treatment for Achilles tendon ruptures by age from 2005 to 2011. A significant difference was seen with increasing age (P < .01).
The incidence of Achilles tendon ruptures increased significantly from 2005 to 2011. The incidence of Achilles tendon ruptures in 2005 was 0.67 per 10,000 patients, and increased to 1.08 per 10,000 patients in 2011 (P < .01). With respect to each individual year from 2005 to 2011, there was a significant year-over-year increase in the overall number of tears that occurred between 2005 and 2011 (1689 in 2005 compared with 2788 in 2011) (P < .05) (Figure 3A). However, there was no significant difference in the percentage of those tears that were treated operatively versus nonoperatively between 2005 and 2011 (P > .05) (Figure 3B). Approximately 30% (29.5% in 2005 and 29.8% in 2011) of tears were treated operatively in both 2005 and 2011.
Figure 3.
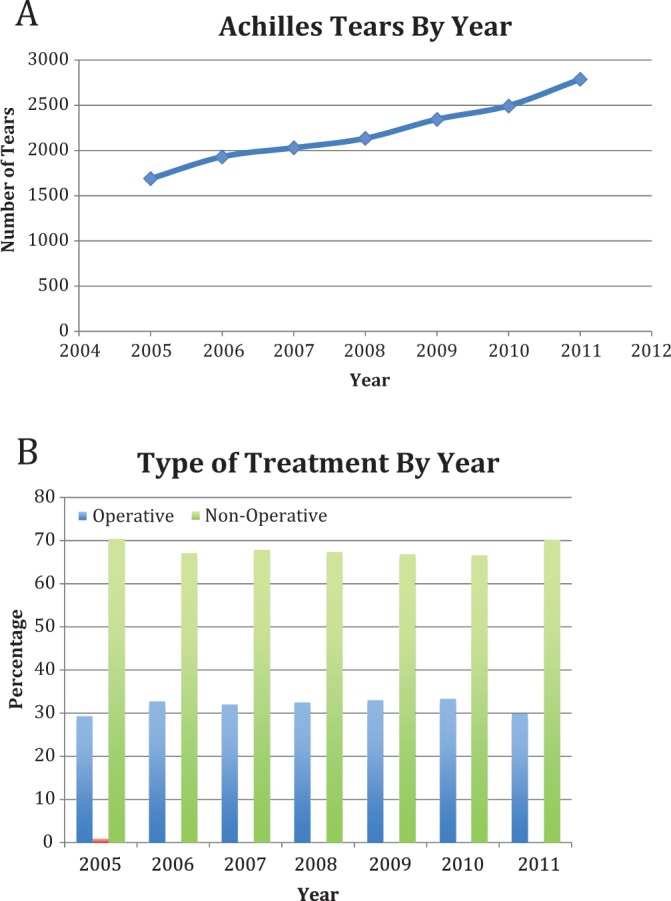
(A) Overall number of Achilles tears by year from 2005 to 2011. A significant increase was seen in the number of tears over time (P < .05). (B) Type of treatment for Achilles tendon ruptures by year from 2005 to 2011. No significant difference was seen over time (P > .05).
There was a significant difference in the overall number of Achilles tendon ruptures that occurred in the Southern United States compared with the other regions (Northeast, Midwest, and West) (P < .05) (Figure 4A). There was no significant difference between regions in the percentage of tears treated operatively (Figure 4B).
Figure 4.
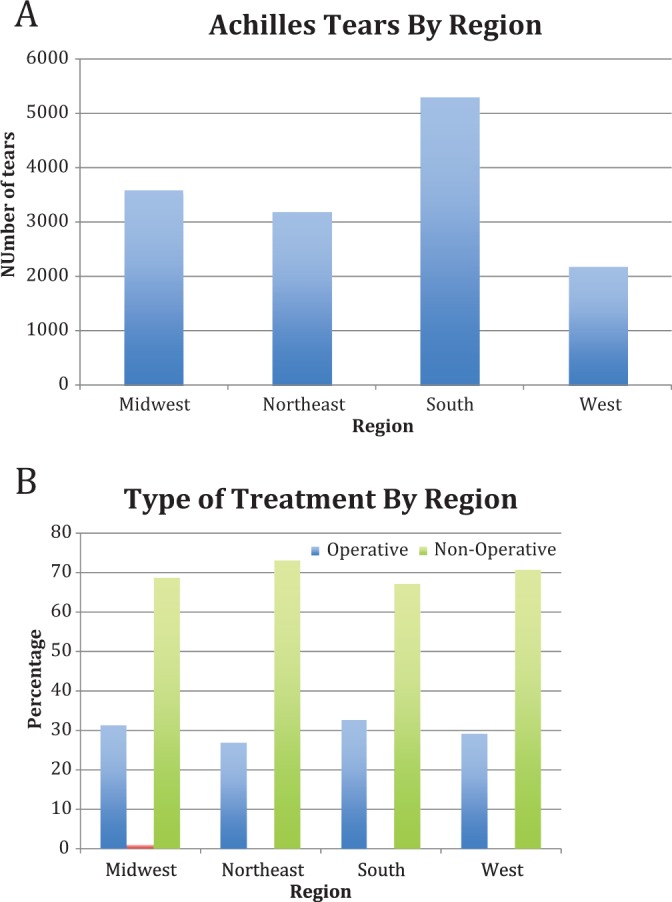
(A) Overall number of Achilles tears by region from 2005 to 2011. Significantly more Achilles tendon ruptures occurred in the Southern region (P < .05). (B) Type of treatment for Achilles tendon ruptures by region from 2005 to 2011. The South was significantly more likely to treat a tear operatively (P < .05).
There was no significant difference in the number of Achilles tendon ruptures between each yearly quarter (P > .05) (Figure 5A), nor was there a significant difference in the percentage of Achilles tendon ruptures treated operatively between each yearly quarter (P > .05) (Figure 5B). There was a significant difference in the average charge and reimbursement between Achilles tears that were treated with primary repair versus primary repair and graft reconstruction (P < .05) (Figure 6). Graft repairs compared with primary repairs were more costly to Medicare (US$2385 vs US$4128) and associated with a higher cost-to-charge ratio (0.69 vs 0.52).
Figure 5.
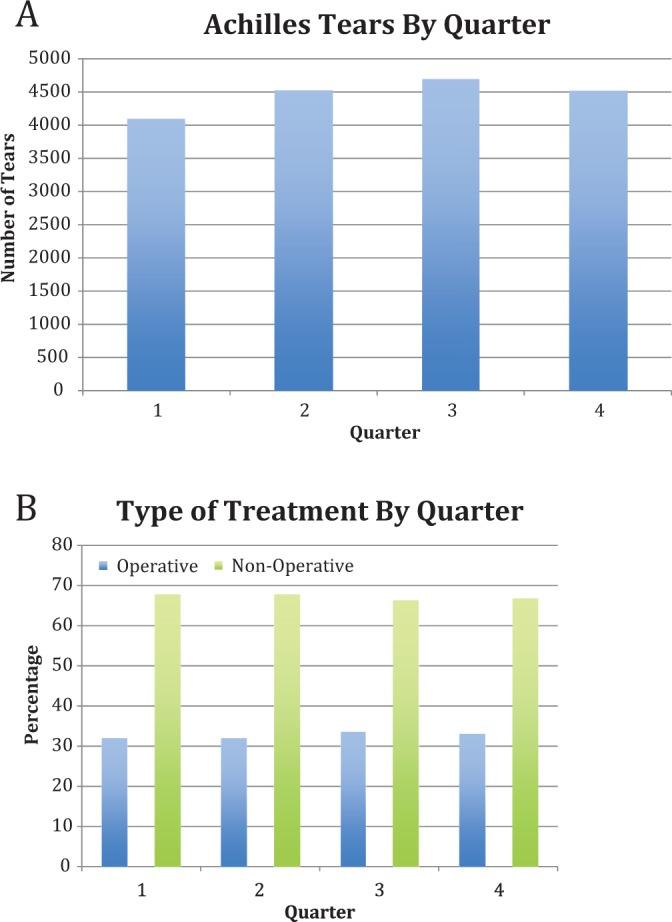
(A) Overall number of Achilles tears by yearly quarter from 2005 to 2011. No significant difference was seen between quarters (P > .05). (B) Type of treatment for Achilles tendon ruptures by yearly quarter from 2005 to 2011. No significant difference was seen between yearly quarters (P > .05).
Figure 6.
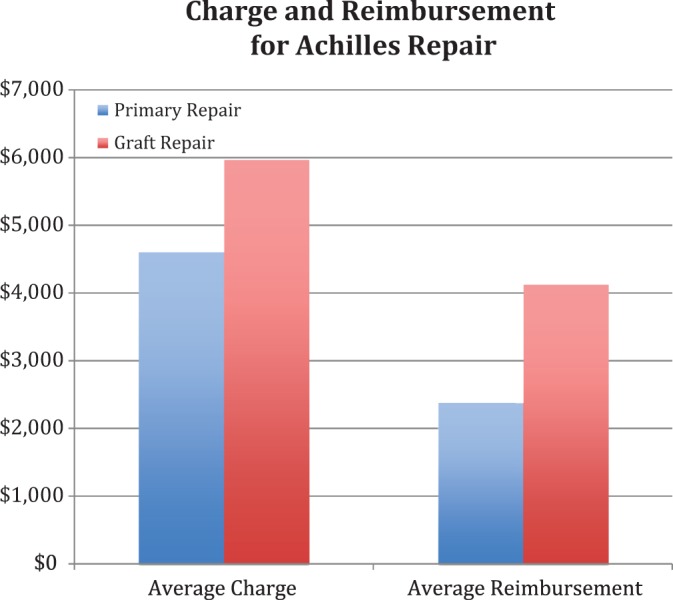
Average charge and reimbursement for primary repair versus primary repair with graft reconstruction of Achilles tendon ruptures.
Discussion
The purpose of this study was to report the incidence of Achilles tendon ruptures in the US Medicare population (>65 years of age) from 2005 to 2011 and to analyze trends in Achilles rupture treatment over time. All of our hypotheses were confirmed. There was an increase in the number of Achilles ruptures over time with no change in operative versus nonoperative treatment. Furthermore, there was no significant difference in operative versus nonoperative treatment based on sex, region, and yearly quarter.
Achilles tendon ruptures are one of the most common injuries seen in active, middle-aged patients, and with the aging population becoming more active, the incidence of these ruptures in the elderly is increasing.4 However, there are little data on the treatment of Achilles tendon injuries in patients older than 65 years in the literature. As the US population is aging, it is important to understand how these patients are treated. The current study demonstrated an increase in the incidence of Achilles tendon ruptures from 0.67 per 10,000 patients in 2005 to 1.08 per 10,000 patients in 2011. These findings are similar to other studies that have demonstrated an increase in incidence from 0.2 per 10,000 to 1.2 per 10,000 patients.4
The cause of an Achilles tendon rupture is likely multifactorial. There is a tenuous blood supply to the Achilles tendon approximately 2 to 6 cm proximal to the insertion point on the calcaneus; this area is commonly torn.16 Furthermore, the tendon is more likely to rupture when an eccentric load is applied to it, with a violent muscle strain, when the muscle becomes fatigued, or when it loses some of its proprioceptive capabilities.9,10 In the elderly population, Achilles tendon ruptures are likely to be more degenerative in nature, and so we chose to examine nontraumatic Achilles tendon injuries in this study, as there would likely be significantly more nontraumatic ruptures than traumatic ruptures in this population.11
There have been many studies that have evaluated the success of operative and nonoperative treatment for ruptured Achilles tendons. Porter et al14 recently evaluated operative repair of ruptured Achilles tendons at a minimum of 12 months postoperatively. Patients demonstrated decreased calf circumference, decreased plantar flexion strength, and equal dorsiflexion strength compared with the noninjured leg. However, subjectively, patients noted near-normal pain and function. There was no cohort of nonoperatively treated patients in this study. However, Willits et al18 performed a multicenter randomized trial evaluating operative versus nonoperative management of Achilles tendon ruptures with accelerated rehabilitation and found no significant difference in calf circumference, range of motion, strength, or clinical outcomes. The current study demonstrated that trends in the United States favor nonoperative management of Achilles tendon ruptures, especially in patients who are older than 85 years. Overall, 70% of patients with an Achilles tendon rupture were treated nonoperatively.
A recent systematic review by Holm et al5 reviewed all the randomized controlled trials in the previous 10 years that compared operative and nonoperative treatment of Achilles tendon ruptures. They found that patients who were treated operatively had a tendency toward lower rerupture rates but had slightly higher complication rates. Functionally, patients treated operatively had significantly higher scores on hop tests, jump tests, heel rise tests, and endurance tests. Patient satisfaction and pain was noted to be better in the nonoperative group initially, but favored the surgical group at 1 year. This study points toward some benefit from operative intervention, but not without complications. This may explain the general trend in the United States toward nonoperative treatment in the majority of the older (>85 years), less athletic population who do not need to function at the level of an elite athlete. There have not been many studies that have examined Achilles tears in patients >65 years in other countries. Barfod2 surveyed numerous countries throughout Europe regarding operative versus nonoperative treatment of Achilles tendon injuries, and a majority of countries treated these injuries surgically over 60% of the time. However, Finland quoted only a 30% rate of operating on Achilles tendon injuries, which parallels the results from this study.
Interestingly, the percentage of Achilles ruptures that occurred in males and females in this study was not significantly different. Other studies have reported rates from 2:1 to 19:1 in favor of males, although there has been a recent increase in the number of female Achilles ruptures.9,19 The equal number of male and female ruptures seen in this study is likely because the tears evaluated in this study were nontraumatic, so the typical male “weekend warrior” population was not included in this study. There was also little variation in the treatment trends between times of the year and among most areas of the country.
The PearlDiver database did not separate the operative Achilles repairs based on timing of surgery from injury. Therefore, it is unclear if some of the operative cases were chronic tendinosis and not just acute ruptures. While the ICD-9 code often used for chronic Achilles tendinosis is 726.71 and CPT code for secondary repair of the Achilles is 27654, it is possible that some chronic Achilles tendinosis cases were intermixed in these data. This may have increased the percentage of nonoperative cases but should not have had an effect on the trends over time as the intermixed patients would likely not change significantly.
The data suggested that Medicare reimbursement is higher for primary repair with a graft versus primary repair alone. This is reasonable given the extra time and resources necessary for graft reconstruction as opposed to a simple primary repair.13 Graft repair is reimbursed at 1.7 times the rate of primary repair alone. However given that this is hospital reimbursement data, it is unclear whether patients receiving graft repairs are more medically complex, thereby incurring greater hospital expenses. As the number of elderly patients sustaining Achilles tendon ruptures in the United States grows, understanding the economics of the various treatment modalities will be important. Economic data are unavailable in the database to quantify costs incurred to Medicare due to nonoperative treatment of Achilles tendon ruptures. As nonoperative treatment still necessitates physical therapy visits, doctor’s appointments, cast changes, and so on, it has a significant cost associated with it. Furthermore, if a nonoperatively treated Achilles tendon ruptures, then the costs associated with operative repair are added on to the already hefty charges. Furthermore, if the laterality of the rupture was recorded, the data could be analyzed for rerupture versus contralateral rupture, but this was not available. However, as the data on rerupture rates between operatively and nonoperatively treated Achilles tendon injuries are conflicting, a conclusion as to the best, most economic treatment modality is difficult. More work may be done to better understand both the costs and the effectiveness associated with various treatment modalities for Achilles tendon ruptures.
Limitations
Despite analyzing a large number of patients and stratifying them based on several variables, this study does have several limitations. As mentioned, some patients with tendinosis could have been included in this study and skewed the results toward nonoperative treatment. The number of patients who crossed over from nonoperative to operative treatment was unknown, and therefore could have elevated the total number of Achilles tears. Furthermore, the exact operative technique (open, mini-open, percutaneous), location of the tear, and timing to surgery for these patients (acute vs chronic) was unknown. This study did not include information of private nonoperative outpatient care, patient medical history, laterality of the rupture, and whether multiple hospital visits in 1 person were due to the same rupture episode or a new rupture in the opposite limb. Also, because the goal of this study was to analyze trends in a Medicare population, our patient population was mostly older than 65 years. As such, our findings are not generalizable to the trends for younger patients. Finally, given that our data collection was based on ICD-9 and CPT codes, the results can be limited by the accuracy of medical coders. The latter limitation is present in any retrospective database study, however.
Conclusion
The incidence of Achilles tendon ruptures is increasing with time, but the trend in operative and nonoperative treatment has not changed between 2005 and 2011. Older patients, especially those >85 years, are more likely to be treated nonoperatively. No differences in treatment patterns were seen based on sex, region, or yearly quarter.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.R.B. receives royalties from SLACK Inc and institutional research support from Arthrex, Ossur, Linvatec, and Smith & Nephew.
References
- 1. Amin NH, Old AB, Tabb LP, Garg R, Toossi N, Cerynik DL. Performance outcomes after repair of complete Achilles tendon ruptures in National Basketball Association players. Am J Sports Med. 2013;41:1864–1868. [DOI] [PubMed] [Google Scholar]
- 2. Barfod KW. Achilles tendon rupture: assessment of nonoperative treatment. Dan Med J. 2014;61:B4837. [PubMed] [Google Scholar]
- 3. Deangelis JP, Wilson KM, Cox CL, Diamond AB, Thomson AB. Achilles tendon rupture in athletes. J Surg Orthop Adv. 2009;18:115–121. [PubMed] [Google Scholar]
- 4. Hess GW. Achilles tendon rupture: a review of etiology, population, anatomy, risk factors, and injury prevention. Foot Ankle Spec. 2010;3:29–32. [DOI] [PubMed] [Google Scholar]
- 5. Holm C, Kjaer M, Eliasson P. Achilles tendon rupture—treatment and complications: a systematic review [published online March 20, 2014]. Scand J Med Sci Sports. doi:10.1111/sms.12209. [DOI] [PubMed] [Google Scholar]
- 6. Keating JF, Will EM. Operative versus non-operative treatment of acute rupture of tendo Achillis: a prospective randomised evaluation of functional outcome. J Bone Joint Surg Br. 2011;93:1071–1078. [DOI] [PubMed] [Google Scholar]
- 7. Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, Parker M. Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202–2210. [DOI] [PubMed] [Google Scholar]
- 8. Kolodziej L, Bohatyrewicz A, Kromuszczynska J, Jezierski J, Biedron M. Efficacy and complications of open and minimally invasive surgery in acute Achilles tendon rupture: a prospective randomised clinical study—preliminary report. Int Orthop. 2013;37:625–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leppilahti J, Orava S. Total Achilles tendon rupture. A review. Sports Med. 1998;25:79–100. [DOI] [PubMed] [Google Scholar]
- 10. Maffulli N. Current concepts in the management of subcutaneous tears of the Achilles tendon. Bull Hosp Jt Dis. 1998;57:152–158. [PubMed] [Google Scholar]
- 11. Moller A, Astron M, Westlin N. Increasing incidence of Achilles tendon rupture. Acta Orthop Scand. 1996;67:479–481. [DOI] [PubMed] [Google Scholar]
- 12. Molloy A, Wood EV. Complications of the treatment of Achilles tendon ruptures. Foot Ankle Clin. 2009;14:745–759. [DOI] [PubMed] [Google Scholar]
- 13. Ponnapula P, Aaranson RR. Reconstruction of Achilles tendon rupture with combined V-Y plasty and gastrocnemius-soleus fascia turndown graft. J Foot Ankle Surg. 2010;49:310–315. [DOI] [PubMed] [Google Scholar]
- 14. Porter DA, Barnes AF, Rund AM, Kaz AJ, Tyndall JA, Millis AA. Acute Achilles tendon repair: strength outcomes after an acute bout of exercise in recreational athletes. Foot Ankle Int. 2014;35:123–130. [DOI] [PubMed] [Google Scholar]
- 15. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34:475–480. [DOI] [PubMed] [Google Scholar]
- 16. Wertz J, Galli M, Borchers JR. Achilles tendon rupture: risk assessment for aerial and ground athletes. Sports Health. 2013;5:407–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wilkins R, Bisson LJ. Operative versus nonoperative management of acute Achilles tendon ruptures: a quantitative systematic review of randomized controlled trials. Am J Sports Med. 2012;40:2154–2160. [DOI] [PubMed] [Google Scholar]
- 18. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92:2767–2775. [DOI] [PubMed] [Google Scholar]
- 19. Yinger K, Mandelbaum BR, Almekinders LC. Achilles rupture in the athlete. Current science and treatment. Clin Podiatr Med Surg. 2002;19:231–250. [DOI] [PubMed] [Google Scholar]
- 20. Zhao HM, Yu GR, Yang YF, Zhou JQ, Aubeeluck A. Outcomes and complications of operative versus non-operative treatment of acute Achilles tendon rupture: a meta-analysis. Chin Med J (Engl). 2011;124:4050–4055. [PubMed] [Google Scholar]


