Abstract
Abdominal leiomyomas are extremely rare intraabdominal tumors, especially in male patient. Here, we report a case of a 22 years-old male with a huge abdominal leiomyoma. The patient presented with a chief complaint of abdominal distension for three months, no others significant symptom were found. CT-scan showed a cystic-solid huge mass in the middle and lower abdominal peritoneal cavity with uneven density. An exploratory laparotomy was performed and the tumor was completely resected. Microscopically, Tumor cells have a spindled shape, eosinophilic cytoplasm, and cigar-like nuclei, arranged in bundles or intersecting fascicles. Immunohistochemistry, the tumor cells were SMA, desmin diffuse positive and CD117, S-100 negative, interestingly, ER, PR were positive. The characteristics of a few of the male abdominal leiomyoma reported in the literature were generalized.
Keywords: Male, leiomyoma, deep soft tissue
Introduction
Deep soft tissue leiomyoma is a class of smooth muscle tumors of very rare, and is now generally considered to be divided into somatic soft tissue and abdomen/retroperitoneum two categories from the occurrence site, both in the clinical and pathological features and aspects of the histological diagnosis criteria were significantly different [1], abdomen/retroperitoneum leiomyoma almost always occur in woman, here we report a case of abdomen huge leiomyoma occurs in a young men, and reviews the literature.
Case report
A 22 years old male patient, complained of abdominal distension for three months, no fever, diarrhea, bloody diarrhea, vomiting and other symptoms. Physical examination revealed abdominal distension, the whole abdomen soft, no tenderness and rebound tenderness, liver and spleen palpation are not satisfied, no palpable and obvious mass, shifting dullness negative, No lower extremity edema. Abdominal color ultrasound display a huge cystic mass in the abdomen or encapsulated fluid mass which the nature is unknown origin. With total abdominal 64-slice CT scan and enhanced, MPR reconstruction display a huge cystic solid mass in the middle and lower abdominal peritoneal cavity with uneven density, the posterior proportion of the mass was prominent in solid and intralesional separation was noted (Figures 1, 2). The tumor size was about 30 cm × 19 cm × 33 cm. local boundary less clear, the CT value of solid parts of the lesions is about 35-45HU, at the same time, CT value of the cystic part is about 10HU, enhanced scan showed solid components significantly enhanced, CT value of about 70HU, no enhancement in low-density areas. The bowel nearby were compressed. The organizational structure of the lower abdomen showed unclear, the inferior vena cava was compressed obviously, based on these imaging findings, the radiologist considering the mass was a borderline or malignant lesions, the most possibility were leiomyosarcoma or GIST. So the exploratory laparotomy was performed and the tumor was resected (Figure 3).
Figure 1.

Computed tomogram show a huge cystic solid mass in the middle and lower abdominal peritoneal cavity with uneven density.
Figure 2.
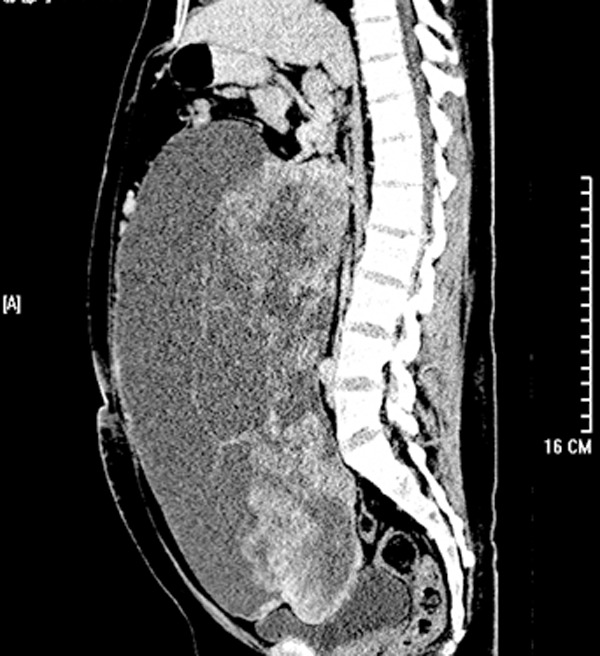
Computed tomogram show a huge cystic solid mass in the middle and lower abdominal peritoneal cavity with uneven density.
Figure 3.

Resection and gross appearance of a giant abdominal leiomyoma.
Macroscopically, the size of this large tumor was about 30 cm × 30 cm × 8 cm and have a smooth surface. The tumor was well encapsulated and showed multi cystic-solid in the cut section. The solid part was gray-white and pale pink, soft. The cystic part was filled with dark red fluid. Microscopically, tumor cells have a spindled shape, eosinophilic cytoplasm, and cigar-like nuclei, arranged in bundles or intersecting fascicles. Some areas stroma shows edema myxoid change and some areas the spindle cells were more densely, but no significant cytologic atypia was found, with less mitotic activity <3/50 HPF (Figures 4, 5 and 6). Immunohistochemically, desmin and SMA were diffusely cytoplasmic positive, and CD117, CD34, Dog1, S-100 were negative. ER showed nuclear positive and PR negative (Figure 7). The patient recovered well after the operation and no recurrence and metastasis have been found in the follow-up for about six-months.
Figure 4.

Spindle tumor cell arranged in bundles or intersecting fascicles (HE × 100).
Figure 5.

High power shows the cigar-like nuclei (HE × 200).
Figure 6.

Some areas stroma show edema myxoid Change (HE × 100).
Figure 7.
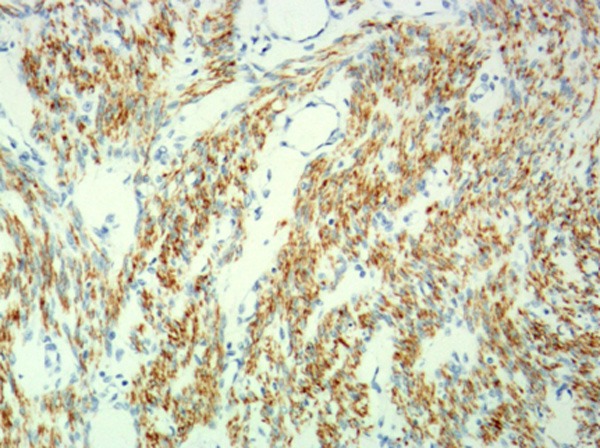
Diffuse positive staining for Desmin in tumor cell (EnVisionTM × 100).
Discussion
Leiomyoma occurs mainly in the female reproductive tract. In deep soft tissue, leiomyosarcoma occurs more frequently than leiomyoma. It has been long disputes on the existence of benign leiomyoma in deep soft tissue until two large cohort studies showed, it does present a set of well biological behavior smooth muscle tumors in deep soft tissue if strict diagnostic criteria were applied [1,2]. Now, it is widely recognized that the deep soft tissue smooth muscle tumors can be divided into two different clinicopathologic subtypes: the somatic soft tissue leiomyomas and the retroperitoneal/abdominal leiomyomas. Former mainly located in the extremities, mitotic figure <1/HPF, equal distribution among male and female. On the other hand, the latter occurs mainly in perimenopausal women, in some cases the mitotic number can reach to 10/HPF [3].
Male retroperitoneal/abdominal leiomyoma are more rare, currently reported cases occurred mainly in young men (22~45 years old), generally the tumor size is larger (25~31 cm), mitotic activity 0~3/HPF, no significant cell atypia were found, interstitial edema and cystic change are common. Immunohistochemically, the tumor cells were positive for SMA (7/7) and desmin (7/7), but negative for CD117 (0/7), and partially positive for ER (2/7), PR (3/7) (Table 1). The media follow-up time was 9 years (6~269 months), no recurrence and metastasis were found [1,2,4]. These male abdominal leiomyoma cases could be a strongly rebuttal evidence to these people who considering the intraperitoneal leiomyoma as a parasitic leiomyoma or planting tumor from uterus leiomyoma. Partial male leiomyoma also express hormone receptors, suggesting that originated from the hormone-sensitive smooth muscle cells in the abdominal cavity or remnant of the Mullerian duct [5]. WHO classification of tumors of the soft tissue require the mitotic number <1/HPF on male abdominal leiomyoma [6], but for these hormone receptor-positive men leiomyoma more mitotic may be accepted, which need more accumulated cases and follow-up data to justify.
Table 1.
Clinicopathologic and immunohistochemical characteristics of reported cases of abdominal leiomyoma in male
| Case number | Reference | Age | Maximum size (cm) | Mitosis | Immunohistochemistry (/50 HPF) | ||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| ER | PR | SMA | Desmin | CD117 | |||||
| 1 | Hu et al. [4] | 24 | 26.8 | 0 | + | + | + | + | - |
| 2* | Billings et al. [1] | 35 | 25 | <1 | |||||
| 3-7 | Paal et al. [2] | 45** | 31 | 0 | 0/5 | 1/5 | 5/5 | 5/5 | 0/5 |
| 8 | Current case | 22 | 30 | <3 | + | + | + | + | - |
No immunohistochemistry data;
mean age.
The mainly differential diagnosis of intraperitoneal leiomyoma is leiomyosarcoma, the latter tumor cells have more obvious atypia and higher mitotic activity, may show coagulation necrosis [2,7]. ER, PR generally negative in abdominal leiomyosarcoma, and thus can serve as a useful tip. However, the majority of male abdominal leiomyoma hormone receptor negative, and the ER, PR in metastatic leiomyosarcoma of uterine can be positive, so the role of immunohistochemistry in the differential diagnosis between leiomyoma and leiomyosarcoma is limited [8]. The others need to differentiate include extragastrointestinal stromal tumor, nerve sheath tumors and solitary fibrous tumor. EGIST have more dense cells and CD117, Dog1 diffusely positive and CD34, SMA occasional positive, but desmin and S-100 negative. The stroma of solitary fibrous tumor has more obvious collagen, CD34 diffuse positive but SMA negative. Schwannoma cells have pointed nucleus at both ends and more wavy, meanwhile S-100 positive strongly.
In short, because the male abdominal leiomyoma is extremely rare, its diagnostic criteria between benign and malignant need more case and follow-up data accumulated to demonstrate, and thus, at present complete tumor resection and long-term follow-up is a wise choice.
Disclosure of conflict of interest
None.
References
- 1.Steven D, Andrew L, Sharon W. Do leiomyomas of deep soft tissue exist. Am J Surg Pathol. 2001;25:1134–1142. doi: 10.1097/00000478-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Paal E, Miettinen M. Retroperitoneal leiomyomas: a clinicopathologic and immunohistochemical study of 56 cases with a comparison to retroperitoneal leiomyosarcomas. Am J Surg Pathol. 2001;25:1355–63. doi: 10.1097/00000478-200111000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Weiss SW. Smooth muscle tumors of soft tissue. Adv Anat Pathol. 2002;9:351–359. doi: 10.1097/00125480-200211000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Fu CY, Chang WK, Yu TC, Cheng MF, Chen TW. Unusual giant abdominal leiomyoma in a young man: a case report. Z Gastroenterol. 2008;46:421–424. doi: 10.1055/s-2007-963523. [DOI] [PubMed] [Google Scholar]
- 5.Patil DT, Laskin WB, Fetsch JF, Miettinen M. Inguinal smooth muscle tumors in women-a dichotomous group consisting of Mullerian-type leiomyomas and soft tissue leiomyosarcomas: an analysis of 55 cases. Am J Surg Pathol. 2011;35:315–24. doi: 10.1097/PAS.0b013e318208e361. [DOI] [PubMed] [Google Scholar]
- 6.Christopher DM, Julia A, Pancras CW, et al. WHO classification of tumours of soft tissue and bone. International agency for research on cancer. 4th edition. Lyon: 2013. pp. 110–111. [Google Scholar]
- 7.Rao UNM, Finkelstein SD, Jones MW. Comparative immunohistochemical and molecular analysis of uterine and extrauterine leiomyosarcomas. Mod Pathol. 1999;12:1001–9. [PubMed] [Google Scholar]
- 8.Shmookler BM, Lauer DH. Retroperitoneal leiomyosarcoma: a clinicopathologic analysis of 36 cases. Am J Surg Pathol. 1983;7:269–80. [PubMed] [Google Scholar]


