Abstract
Background: Mutations in the epidermal growth factor receptor gene (EGFR) are found in around half of Asian patients with non-small cell lung cancer (NSCLC). For this reason, EGFR tyrosine kinase inhibitors (TKI) are often prescribed depending on the EGFR status. Two common EGFR mutations, a deletion in exon 19 and L858R in exon 21, demonstrate a positive response to gefitinib, the first approved EGFR TKI. However, T790M and an insertion in EGFR exon 21 are resistant to EGFR TKI treatment. The relationships between the EGFR mutation type and response to the target drug have not been fully investigated. Case presentation: We describe a 66-year-old Chinese male diagnosed with stage IV lung adenocarcinoma based on evidence from a computed tomography (CT) scan and histological features of a biopsy taken during fiberoptic bronchoscopy surgery. Molecular analysis of EGFR exons 19 and 21 revealed the presence of only one mutation in exon 19: L747P (2239-2240 TT>CC). The patient requested gefitinib treatment for 2 weeks but his response was poor. A CT scan revealed that the number and relative volume of the liver metastases had increased after treatment. Conclusion: L747P (2239-2240 TT>CC) in exon 19 is a rare EGFR mutation that appears to lead to gefitinib resistance and might accelerate liver metastases.
Keywords: EGFR, L747P, drug resistance, gefitinib, liver metastases
Background
Lung cancer is one of the leading malignant tumors worldwide and is associated with a high level of mortality. Non-small cell lung cancer (NSCLC) accounts for about 75-85% of all lung cancer cases [1]. Based on the important role of aberrant oncogene expression during tumorigenesis and tumor progression, targeted chemotherapy drugs are being developed to specifically block signaling pathways, and to inhibit and/or kill malignant tumor cells [2].
One such oncogene is the epidermal growth factor receptor (EGFR), which is usually over-expressed in advanced NSCLC and is correlated with a poor prognosis [3]. Blockage of the EGFR pathway is therefore a promising drug target, and gefitinib, a small molecular inhibitor of EGFR, was approved by the FDA for NSCLC therapy use in 2003. It has since shown favorable efficacy in the clinic, especially for NSCLC patients with certain EGFR mutations [4,5]. Patients with an EGFR deletion in exon 19 and/or L858R in exon 21 showed a positive response to gefitinib treatment, while those harboring the T790M mutation or an insertion in exon 21 demonstrated gefitinib resistances [6-8]. Here, we present a patient with lung adenocarcinoma harboring a rare type of mutation in EGFR exon 19: L747P (2239-2240 TT>CC), who showed resistance to gefitinib treatment and rapid progression of liver metastases.
Case presentation
A 66-year-old Chinese man presented with a 2 month history of dry cough, and was taken to the Department of Respiratory Medicine. No abnormal physical signs were found during a medical examination, and the neck palpation was negative for lymph nodes. A chest computed tomography (CT) scan revealed a nodular shadow in the lower lobe of the left lung, accompanied by bilateral enlarged hilar lymph nodes and blurred patchy shadows. An abdominal CT showed several nodular shadows in the liver (Figure 1A).
Figure 1.
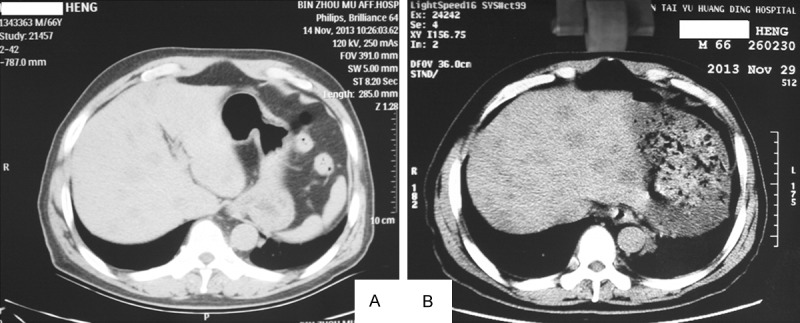
Abdominal plain scanning CT. A. Before gefitinib treatment; B. 2 weeks administration with gefitinib.
Fiberoptic bronchoscopy surgery was conducted and the histological observation of the biopsy revealed atypical epithelial cells arranged as irregular glandular or tubular structures infiltrated in the background of proliferative fibrous tissue. These cells had irregular nuclei with clumps of chromatin, scanty cytoplasm, and conspicuous nucleoli (Figure 2A). Immunohistochemistry showed that the cells stained positive for thyroid transcription factor 1 and napsin A, but were negative for CK5/6 (Figure 2D). Based on these features, a diagnosis of lung adenocarcinoma in the lower lobe of the left lung was made. Soon afterwards the patient requested EGFR genetic analysis of the cancerous tissue, and sequencing revealed the presence of the rare mutation L747P (2239-2240 TT>CC), but no other mutations were found (Figure 3). Oral gefitinib was firstly administered at a daily dose of 250 mg based on the patient’s condition, but a poor response was observed, and a CT scan showed that the number of liver metastasis had clearly increased 2 weeks later (Figure 2, right). Chemotherapy, in which the chemotherapy regimen included pemetrexed at 500 mg/m2 in combination with carboplatin AUC 5, was then administered once every 21 days with standard premedication.
Figure 2.
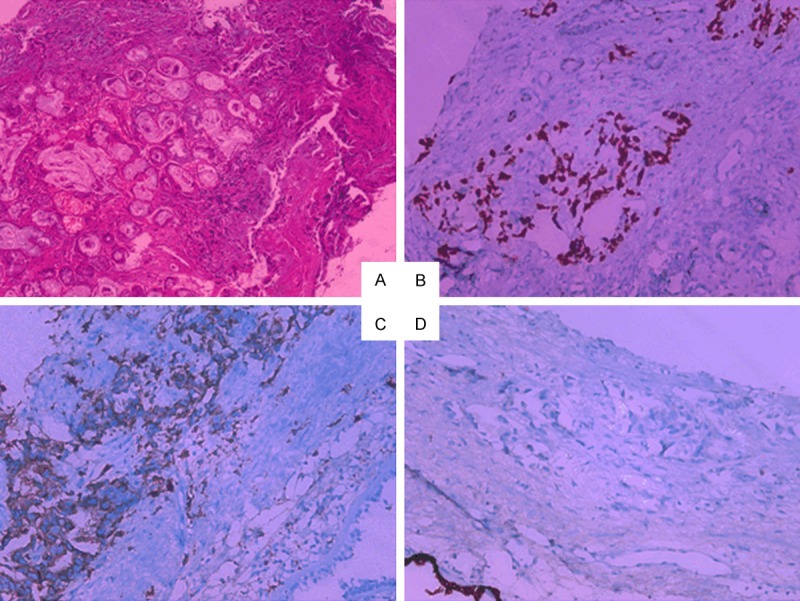
Pathology slides of the biopsy specimen with different stains. A. Hematoxylin and eosin stained section of the mass demonstrating atypical epithelial cells arranged as irregular glandular or tubular structures infiltrated in the background of proliferative fibrous tissue (×100); B. Immunohistochemical detection of thyroid transcription factor 1 (×100). C. Immunohistochemical detection of napsin A (×100); D. Immunohistochemical detection of CK5/6 (×100).
Figure 3.
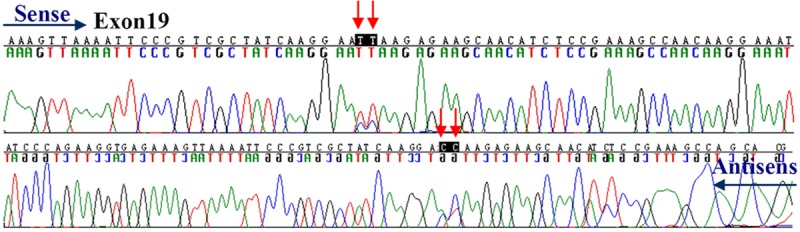
Sequencing results for EGFR mutation L747P (2239-2240 TT>CC) on exon 19, NM_005228.3 as the reference sequence.
Conclusions
Mutations in EGFR exons 18-21 are found in around half of Asian patients with advanced NSCLC [9]. A deletion in exon 19 and the L858R mutation in exon 21 are positively correlated with sensitivity to gefitinib treatment, while the T790M mutation and an insertion in exon 21 show a negative response [10-13]. Following the widespread use of gefitinib in the clinic, many more uncommon EGFR mutations are being reported that show different responses to gefitinib treatment [14,15]. L747P (2239-2240 TT>CC) in exon 19 is an unusual type of EGFR mutation that was first reported by Wu et al. [16], in which two patients with the point mutation were resistant to gefitinib and erlotinib, the second approved EGFR TKI. To our knowledge, this is only the second case presentation of the rare mutation. Our patient also demonstrated resistance to gefitinib treatment, and this is for the first time to describe a possible acceleration of liver metastases by gefitinib.
Acknowledgements
This study was supported by Taishan Scholar Project and National Natural Science Foundation of China (No. 81202038).
Disclosure of conflict of interest
None.
References
- 1.Lurje G, Lenz HJ. EGFR signaling and drug discovery. Oncology. 2009;77:400–410. doi: 10.1159/000279388. [DOI] [PubMed] [Google Scholar]
- 2.Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500. doi: 10.1126/science.1099314. [DOI] [PubMed] [Google Scholar]
- 3.Arfaoui A, Kriaa L, Znaidi N, Gritli S, Bouacha H, Zermani R, Rammeh S. Over-expression of EGFR is closely correlated to poor prognosis in Tunisian patients with non-small cell lung adenocarcinoma. J Immunoassay Immunochem. 2014;35:256–268. doi: 10.1080/15321819.2013.848813. [DOI] [PubMed] [Google Scholar]
- 4.Takano T, Fukui T, Ohe Y, Tsuta K, Yamamoto S, Nokihara H, Yamamoto N, Sekine I, Kunitoh H, Furuta K, Tamura T. EGFR mutations predict survival benefit from gefitinib in patients with advanced lung adenocarcinoma: a historical comparison of patients treated before and after gefitinib approval in Japan. J. Clin. Oncol. 2008;26:5589–5595. doi: 10.1200/JCO.2008.16.7254. [DOI] [PubMed] [Google Scholar]
- 5.Yatabe Y, Kosaka T, Takahashi T, Mitsudomi T. EGFR mutation is specific for terminal respiratory unit type adenocarcinoma. Am J Surg Pathol. 2005;29:633–639. doi: 10.1097/01.pas.0000157935.28066.35. [DOI] [PubMed] [Google Scholar]
- 6.Sekine A, Kato T, Hagiwara E, Shinohara T, Komagata T, Iwasawa T, Satoh H, Tamura K, Kasamatsu T, Hayashihara K, Saito T, Takahashi H, Ogura T. Metastatic brain tumors from non-small cell lung cancer with EGFR mutations: distinguishing influence of exon 19 deletion on radiographic features. Lung Cancer. 2012;77:64–69. doi: 10.1016/j.lungcan.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 7.Kawahara A, Azuma K, Sumi A, Taira T, Nakashima K, Aikawa E, Abe H, Yamaguchi T, Takamori S, Akiba J, Kage M. Identification of non-small-cell lung cancer with activating EGFR mutations in malignant effusion and cerebrospinal fluid: rapid and sensitive detection of exon 19 deletion E746-A750 and exon 21 L858R mutation by immunocytochemistry. Lung Cancer. 2011;74:35–40. doi: 10.1016/j.lungcan.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 8.Oxnard GR, Paweletz CP, Kuang Y, Mach SL, O’Connell A, Messineo MM, Luke JJ, Butaney M, Kirschmeier P, Jackman DM, Jänne PA. Noninvasive detection of response and resistance in EGFR-mutant lung cancer using quantitative next-generation genotyping of cell-free plasma DNA. Clin Cancer Res. 2014;20:1698–1705. doi: 10.1158/1078-0432.CCR-13-2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Won YW, Han JY, Lee GK, Park SY, Lim KY, Yoon KA, Yun T, Kim HT, Lee JS. Comparison of clinical outcome of patients with non-small-cell lung cancer harbouring epidermal growth factor receptor exon 19 or exon 21 mutations. J Clin Pathol. 2011;64:947–952. doi: 10.1136/jclinpath-2011-200169. [DOI] [PubMed] [Google Scholar]
- 10.Costa DB, Nguyen KS, Cho BC, Sequist LV, Jackman DM, Riely GJ, Yeap BY, Halmos B, Kim JH, Jänne PA, Huberman MS, Pao W, Tenen DG, Kobayashi S. Effects of erlotinib in EGFR mutated non-small cell lung cancers with resistance to gefitinib. Clin Cancer Res. 2008;14:7060–7067. doi: 10.1158/1078-0432.CCR-08-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim HJ, Oh SY, Kim WS, Kim SJ, Yoo GH, Kim WD, Lee KY. Clinical investigation of EGFR mutation detection by pyrosequencing in lung cancer patients. Oncol Lett. 2013;5:271–276. doi: 10.3892/ol.2012.950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang CH. EGFR tyrosine kinase inhibitors for the treatment of NSCLC in East Asia: present and future. Lung Cancer. 2008;60:S23–30. doi: 10.1016/S0169-5002(08)70102-8. [DOI] [PubMed] [Google Scholar]
- 13.Tsao MS, Sakurada A, Cutz JC, Zhu CQ, Kamel-Reid S, Squire J, Lorimer I, Zhang T, Liu N, Daneshmand M, Marrano P, da Cunha Santos G, Lagarde A, Richardson F, Seymour L, Whitehead M, Ding K, Pater J, Shepherd FA. Erlotinib in lung cancer-molecular and clinical predictors of outcome. N Engl J Med. 2005;353:133–144. doi: 10.1056/NEJMoa050736. [DOI] [PubMed] [Google Scholar]
- 14.Balak MN, Gong Y, Riely GJ, Somwar R, Li AR, Zakowski MF, Chiang A, Yang G, Ouerfelli O, Kris MG, Ladanyi M, Miller VA, Pao W. Novel D761Y and common secondary T790M mutations in epidermal growth factor receptor-mutant lung adenocarcinomas with acquired resistance to kinase inhibitors. Clin Cancer Res. 2006;12:6494–6501. doi: 10.1158/1078-0432.CCR-06-1570. [DOI] [PubMed] [Google Scholar]
- 15.Asahina H, Yamazaki K, Kinoshita I, Yokouchi H, Dosaka-Akita H, Nishimura M. Non-responsiveness to gefitinib in a patient with lung adenocarcinoma having rare EGFR mutations S768I and V769L. Lung Cancer. 2006;54:419–422. doi: 10.1016/j.lungcan.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Wu SG, Gow CH, Yu CJ, Chang YL, Yang CH, Hsu YC, Shih JY, Lee YC, Yang PC. Frequent epidermal growth factor receptor gene mutations in malignant pleural effusion of lung adenocarcinoma. Eur Respir J. 2008;32:924–930. doi: 10.1183/09031936.00167407. [DOI] [PubMed] [Google Scholar]


