Abstract
Background:
The palatal masticatory mucosa is the main donor area of soft tissue and connective tissue grafts used for increasing the keratinized mucosa around teeth and implants, covering exposed roots and increasing localized alveolar ridge thickness. The aim of this study was to compare the thickness of the palatal masticatory mucosa as determined on a cone-beam computerized tomography scan versus thickness determined via bone-sounding.
Materials and Methods:
A total of 20 patients requiring palatal surgery participated. Thickness of the palatal tissue was measured at various points radiographically and clinically. The two techniques were compared to determine the agreement of the two measurement modalities.
Results:
Statistical analysis determined that there was no significant difference between the two methods. Moreover, the tissue thickness was shown to increase as the distance from the gingival margin increased, and the tissue over the premolars was thicker than the other teeth.
Conclusion:
Cone-beam computerized tomography can be used as a noninvasive method to accurately and consistently determine the soft tissue thickness of the palatal masticatory mucosa with minimal bias at different locations on the palate.
Keywords: Cone-beam computerized tomography, connective tissue grafts, donor area, palatal masticatory mucosa
INTRODUCTION
The palatal masticatory mucosa is the main donor area of soft tissue and connective tissue grafts used for increasing the keratinized mucosa around teeth and implants, covering exposed roots and increasing localized alveolar ridge thickness. Connective tissue grafts are also well indicated to enhance the probability of complete root coverage when associated with coronally advanced flaps in certain types of gingival recessions.[1]
The critical aspect in the treatment planning of these cases is the determination of the thickness of the graft donor site, since the thickness of tissue grafted from the palate to the recipient site directly affects the surgical outcome.[2] Revascularization of the graft may be prevented if the donor tissue is too thick and graft shrinkage may occur if the tissue is too thin.[3] To prevent these undesirable outcomes, methods have been developed to help the clinician determine the thickness of the palatal masticatory mucosa prior to harvesting the graft. One such method is the use of ultrasonic measuring devices that transmit ultrasonic pulses through the soft tissue and uses an echo of the pulse to calculate the thickness.[4] Another frequently used method is the bone-sounding technique, a direct method that involves anesthetizing the patient and subsequently penetrating the palatal masticatory mucosa with either a periodontal probe or a needle to determine tissue thickness. When using a periodontal probe to determine the thickness of the palatal masticatory mucosa, Studer et al. reported a measurement error of approximately 0.2 + 0.4 mm associated with this technique.[5] Ursell concluded that bone-sounding with a periodontal probe gave a highly accurate indication of bone levels measured at surgery with 93.25% of measurements being within 1 mm.[6] While highly accurate, a drawback to this method is that it is commonly performed immediately prior to surgery, as the patient must be anesthetized. This may possibly hinder appropriate treatment planning of the procedure,[1] as the clinician may find that there is not sufficient tissue thickness in the preanesthetized area.
In an attempt to assist with treatment planning, less invasive techniques to determine the thickness of palatal masticatory mucosa has been developed. Cone-beam computerized tomography (CBCT), in particular, has been used since its development in the 1990s for imaging of the maxillofacial region.[7] Compared to conventional computerized tomographic (CT) systems, CBCTs produce a more focused beam, less radiation scatter,[8] and more rapid volumetric image acquisition,[9] along with being smaller in size and less expensive. Additionally, CBCT has become popular for three-dimensional imaging in the dental field both because of its high spatial resolution and clear images on scans, and its relatively low radiation dose, which is similar to a full-mouth series of periapical films[10] and well below that of classic CT.[11]
A benefit of the use of CBCT scans in dental imaging that has gained much attention in the recent literature is its accuracy in reproducing linear dental measurements.[12]
In addition to accurately representing clinical measurements, data obtained from CBCT scans may indeed be more accurate than that obtained from bone-sounding, as pressure from a periodontal probe or needle may cause tissue distortion during bone-sounding.[13] More importantly, the ability of the clinician to evaluate the palatal masticatory mucosa entirely with a single CBCT scan may provide the opportunity to choose the site from which an ideal graft can be harvested. To the author's knowledge, the validity of CBCT scans in determining the thickness of the palatal masticatory mucosa and the clinical relevance of this less invasive imaging modality has not been extensively studied. Therefore, the aim of this study was to compare the thickness of the palatal masticatory mucosa, as determined on a CBCT scan, to the actual anatomic thickness determined by a bone-sounding technique.
MATERIALS AND METHODS
A total of 20 systemically healthy subjects (10 males, 10 females), ages ranging from 19 to 53 years (mean age of 32 years) requiring palatal surgery were selected from the Department of Periodontics, Government Dental College and Hospital, Srinagar for the study. Informed written consent of subjects and ethical committee clearance was obtained prior to commencement of the study. Inclusion criteria for the selection of subjects for the study were the presence of canine, two premolars and first molar on the side requiring palatal surgery. Subject exclusion criteria were history of palatal surgery, history of presence of pathology in the area being investigated and pregnancy.
After the subject was deemed eligible, a maxillary impression was made with alginate impression material and poured in a Type III dental stone. Acrylic measurement guides (Clear Splint Biocryl, 0.5 mm thickness were then fabricated on the cast model and trimmed appropriately to include all teeth present in the arch. Using a standardized UNC-15 probe (Hu-Friedy, Leimen, Germany), measurements were made at distances of 2 mm, 5 mm, and 8 mm from the mid-palatal point of the gingival margin for the canine, first and second premolars, and the first molar on the side that was to receive palatal surgery. A hole was subsequently punctured through the acrylic stent at each measurement point [Figure 1]. Gutta-percha was used to fill each measurement site [Figure 2]. The purpose of the gutta-percha was to have a radio-opaque marker on the CBCT scan. This stent was subsequently used for all clinical and radiographic measurements.
Figure 1.

Measurement stent on cast with holes punctured at the measurement sites
Figure 2.

Measurement stent on cast with gutta-percha as radioopaque markers
All subjects wore the CBCT stent during the CBCT scan. During CBCT scans, patients were seated and had their heads, and chins stabilized. A scan of the maxilla was taken using the CBCT (NewTom Giano) by a trained technician at 110KVp and 15 mA for 36 s (voxel size: 0.25 mm; grayscale: 12 bis). The reconstructed images were generated using a computer software package (Keystone EasyGuide, Keystone Dental, Inc., Burlington, MA). Each gutta-percha point was visualized using a sagittal view and measurements of the soft tissue thickness were made at each point by one investigator and recorded. All measurements were made perpendicular to the palatal soft tissue. Twelve total radiographic measurements were taken on each scan (for canine, first and second premolars and first molar at the distance of 2 mm, 5 mm and 8 mm from the gingival margin).
On the day of surgery, each patient was anesthetized for palatal surgery using 2% lignocaine with epinephrine. The gutta-percha was removed from the CBCT stent to expose the measurement points, and the stent was aligned correctly in the subject's mouth. The thickness of the palatal mucosa was then determined via bone-sounding through each measurement point perpendicular to the palatal tissue using a standardized UNC-15 Probe [Figure 3] and recorded by one investigator. Measurements were rounded to the nearest ½ mm when the value was not exactly on a marking line. Twelve total clinical measurements were taken on each subject.
Figure 3.
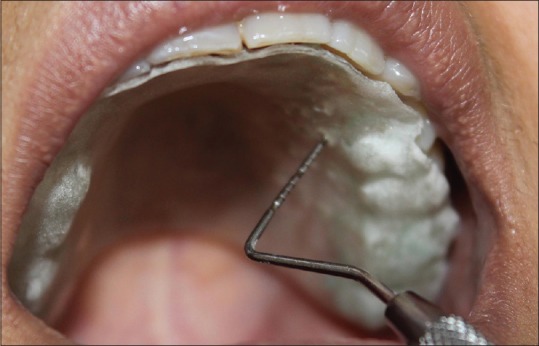
Clinical measurement of maxillary first premolar 2mm from the gingival margin
Data were analyzed with the help of means and standard deviations. For inter-group analysis, t-test was applied. ANOVA test was used for intra-group analysis. P < 0.05 was considered statistically significant. To describe agreement between the two techniques, Bland-Altman plot was used.
RESULTS
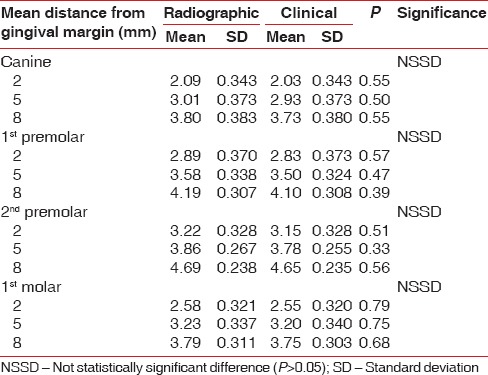
Figure 4a–c show the representative CBCT images of the measurements performed at three different points that are, 2 mm, 5 mm and 8 mm from the gingival margin in case of the second premolar, respectively. Table 1 show the comparison between the measurements obtained via radiographic and clinical techniques at three different points (2 mm, 5 mm, 8 mm) from gingival margin in case of canine, first and second premolars and first molar. Statistical analysis of the data obtained did not reveal any statistically significant difference between the two techniques (P > 0.05). Graph 1 is the graphical representation of the comparison between the radiographic and clinical techniques used to measure the thickness of the palatal mucosa at three different locations in each of the four teeth.
Figure 4a.
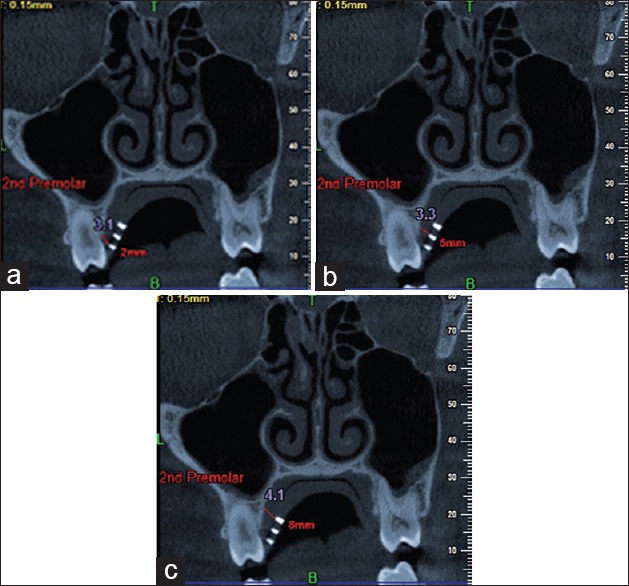
Cone-beam computerized tomography scan-radiographic measurement at 2mm from gingival margin (b) Cone-beam computerized tomography scan-radiographic measurement at 5mm from gingival margin (c) Cone-beam computerized tomography scan-radiographic measurement at 8mm from gingival margin
Table 1.
Comparison of radiographic and clinical measurements
Graph 1.
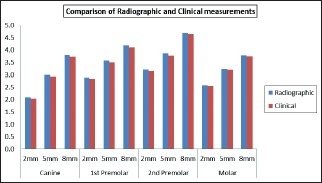
Comparison of radiographic and clinical measurements
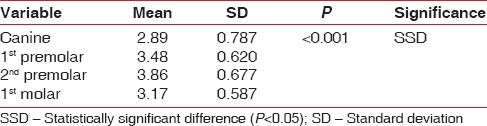
The thickness of the soft tissue, as estimated by the statistical analysis, was influenced by palatal location. Both the distance from a tooth and tooth type were significantly related to the depth (P < 0.001). In both the techniques that is, radiographically [Table 2, Graph 2] and clinically [Table 3, Graph 3], the tissue became thicker as the distance from the tooth increased. Furthermore, the tissue measured at the premolars was thicker than that measured at the molar or canine areas [Table 4, Table 5].
Table 2.
Radiographic technique
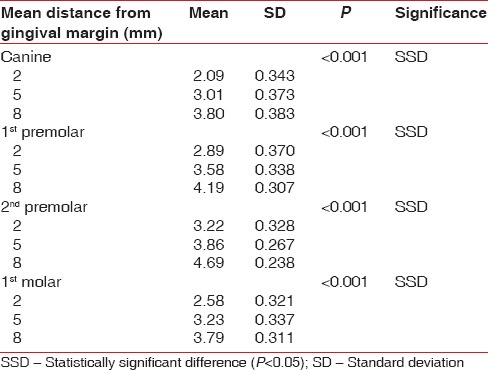
Graph 2.
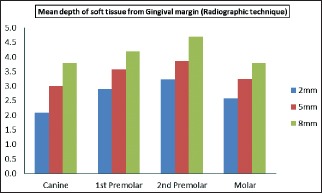
Mean depth of soft tissue from the gingival margin (radiographic technique)
Table 3.
Clinical technique
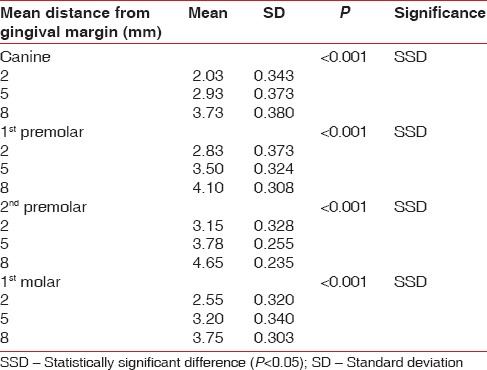
Graph 3.
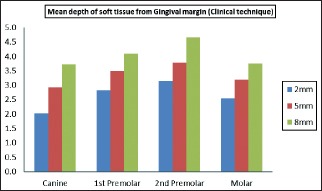
Mean depth of soft tissue from gingival margin (clinical technique)
Table 4.
Radiographic technique
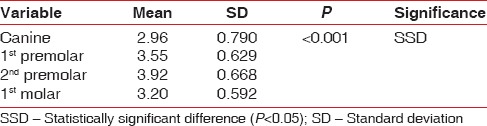
Table 5.
Clinical technique
The Bland-Altman Plot [Graph 4] is the graphical representation of the agreement between the two different measurement modalities (i.e., radiographic measurements versus clinical measurements). The difference between the measurement modalities (Y-axis) is plotted against the mean depth of the same measurement point (X-axis). This plot reveals that there is no significant difference between radiographic and clinical measurements because the vast majority of points fall within the 95% confidence interval around a difference (radiographic measurements-clinical measurements). Thus, there is high agreement between the two measurement modalities.
Graph 4.
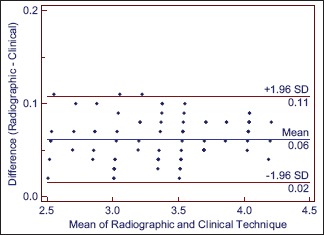
Bland-Altman plot
DISCUSSION
Over the past two decades, the use of CBCT for imaging of the maxillofacial region has increased dramatically.[7] This growth can be attributed to several factors: Compared to conventional CT systems, the CBCT produces a more focused beam with less radiation scatter,[8] CBCTs are smaller and less expensive than conventional CT systems, and most importantly, CBCT scans have been shown to accurately reproduce linear dental measurements.[14]
Baumgaertel et al. compared the results of 10 interfacial measurements (including overbite, overjet, and maxillary and mandibular intermolar and intercanine widths) taken with a high-precision digital caliper, to a CBCT scan on thirty human skulls and found that there was no significant difference between measurement modalities.[14] Lascala et al. compared radiographic measurements of the distance between internal and external anatomical sites on dry skulls to clinical measurements taken with a caliper, and concluded that CBCT imaging is reliable for linear evaluation of facial structures.[9] However, despite the abundance of literature proclaiming the accuracy of CBCT scans in determining linear interfacial hard tissue measurements, until recently there has been a lack of work investigating the accuracy of CBCT imaging of soft tissue measurements.
Barriviera et al. recently described a technique using CBCT that accurately visualized the dimensions of the palatal masticatory mucosa, thus enabling the clinician to make linear measurements of the soft tissue covering the palate.[1] The clinical significance of this finding was that CBCT scans may be useful in the treatment planning of cases where the thickness of the palatal tissue is paramount, such as gingival grafting with either free gingival grafts or subepithelial connective tissue grafts. However, no attempt was made to compare radiographic to clinical measurements.
To date, the most common method of determining the thickness of the palatal tissue prior to harvest a tissue graft is to bone-sound, a highly accurate method, but one that requires patient anesthetization. However, because bone-sounding must be performed while the patient is anesthetized, thus hindering appropriate treatment planning, as a clinician may find that there is insufficient tissue thickness in the anesthetized site, it may be considered a less than ideal method of soft tissue measurement. Thus, the primary aim of this study was to determine if the thickness of the palatal masticatory mucosa, as determined from a CBCT scan, was comparable to the actual anatomic thickness of the same distance measured by a bone-sounding technique.
In the present study, no significant difference was found between the clinical and radiographic measurements of the palatal masticatory mucosa for either location on the palate or thickness of the palatal tissue. This indicates that CBCT is a reliable measurement modality for the palatal tissue. While there remains a lack of literature addressing the accuracy of CBCT imaging of soft tissue measurements, the findings of the current study are consistent with the current body of literature stating that CBCT scans are reliable for hard tissue linear dental measurements.[9,14,15]
A secondary aim of the current study was to determine the actual thickness of the soft tissue in different palatal locations. The results of this study showed that the tissue became thicker as the distance from the tooth increased and that the tissue measured at the premolars was deeper than that measured at the molars. This is in agreement with Studer et al. who showed that the mean tissue thickness increased, as the distance from the gingival margin increased and that the palatal tissue over the root of the maxillary first molar was significantly thinner than all positions in the hard palate.[5] Muller et al. also showed that palatal tissue was thicker at premolars when compared to first molars, which is consistent with the results found in this study.[4]
In conclusion, this study demonstrated that CBCT can be used to accurately determine the soft tissue thickness of the palatal masticatory mucosa, as measurements taken from a CBCT scan were shown to be similar to clinical measurements made via bone-sounding. The current results indicate that a CBCT scan can be used as a noninvasive method of determining palatal tissue thickness. The clinical significance of this finding is that the clinician can potentially use a CBCT scan to determine the location from where a soft tissue graft may be harvested, thus enabling more accurate treatment planning of procedures prior to the surgical appointment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Barriviera M, Duarte WR, Januário AL, Faber J, Bezerra AC. A new method to assess and measure palatal masticatory mucosa by cone-beam computerized tomography. J Clin Periodontol. 2009;36:564–8. doi: 10.1111/j.1600-051X.2009.01422.x. [DOI] [PubMed] [Google Scholar]
- 2.Wara-aswapati N, Pitiphat W, Chandrapho N, Rattanayatikul C, Karimbux N. Thickness of palatal masticatory mucosa associated with age. J Periodontol. 2001;72:1407–12. doi: 10.1902/jop.2001.72.10.1407. [DOI] [PubMed] [Google Scholar]
- 3.Mörmann W, Schaer F, Firestone AR. The relationship between success of free gingival grafts and transplant thickness. Revascularization and shrinkage – a one year clinical study. J Periodontol. 1981;52:74–80. doi: 10.1902/jop.1981.52.2.74. [DOI] [PubMed] [Google Scholar]
- 4.Müller HP, Schaller N, Eger T, Heinecke A. Thickness of masticatory mucosa. J Clin Periodontol. 2000;27:431–6. doi: 10.1034/j.1600-051x.2000.027006431.x. [DOI] [PubMed] [Google Scholar]
- 5.Studer SP, Allen EP, Rees TC, Kouba A. The thickness of masticatory mucosa in the human hard palate and tuberosity as potential donor sites for ridge augmentation procedures. J Periodontol. 1997;68:145–51. doi: 10.1902/jop.1997.68.2.145. [DOI] [PubMed] [Google Scholar]
- 6.Ursell MJ. Relationships between alveolar bone levels measured at surgery, estimated by transgingival probing and clinical attachment level measurements. J Clin Periodontol. 1989;16:81–6. doi: 10.1111/j.1600-051x.1989.tb01618.x. [DOI] [PubMed] [Google Scholar]
- 7.Kau CH, Bozic M, English J, Lee R, Bussa H, Ellis RK. Cone-beam computed tomography of the maxillofacial region – an update. Int J Med Robot. 2009;5:366–80. doi: 10.1002/rcs.279. [DOI] [PubMed] [Google Scholar]
- 8.Mah J, Hatcher D. Current status and future needs in craniofacial imaging. Orthod Craniofac Res. 2003;6(Suppl 1):10–6. doi: 10.1034/j.1600-0544.2003.230.x. [DOI] [PubMed] [Google Scholar]
- 9.Lascala CA, Panella J, Marques MM. Analysis of the accuracy of linear measurements obtained by cone beam computed tomography (CBCT-NewTom) Dentomaxillofac Radiol. 2004;33:291–4. doi: 10.1259/dmfr/25500850. [DOI] [PubMed] [Google Scholar]
- 10.Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:508–13. doi: 10.1016/s1079-2104(03)00350-0. [DOI] [PubMed] [Google Scholar]
- 11.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–26. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi K, Shimoda S, Nakagawa Y, Yamamoto A. Accuracy in measurement of distance using limited cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2004;19:228–31. [PubMed] [Google Scholar]
- 13.Song JE, Um YJ, Kim CS, Choi SH, Cho KS, Kim CK, et al. Thickness of posterior palatal masticatory mucosa: The use of computerized tomography. J Periodontol. 2008;79:406–12. doi: 10.1902/jop.2008.070302. [DOI] [PubMed] [Google Scholar]
- 14.Baumgaertel S, Palomo JM, Palomo L, Hans MG. Reliability and accuracy of cone-beam computed tomography dental measurements. Am J Orthod Dentofacial Orthop. 2009;136:19–25. doi: 10.1016/j.ajodo.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]


