Abstract
Background:
Ideal graft material for regenerative procedures is autogenous bone graft but the major disadvantage with this graft is the need for a secondary surgical site to procure donor material and the frequent lack of intraoral donor site to obtain sufficient quantities of autogenous bone for multiple or deep osseous defects. Hence, to overcome these disadvantages, bone allografts were developed as an alternative source of graft material.
Materials and Methods:
In 10 patients with chronic periodontitis, 20 bilateral infrabony defects were treated with freeze dried bone allograft (FDBA-Group A) and decalcified freeze dried bone allograft (DFDBA-Group B). Clinical and radiographic parameters were assessed preoperatively and at 3 months and 6 months postoperatively. Data thus obtained was subjected to statistical analysis.
Results:
Significant improvement in the reduction in probing depth and relative attachment level (RAL) from the baseline to 3 months to baseline to 6 months in group A and group B, which was statistically significant but no statistically significant reduction was seen between 3 months and 6 months. On inter-group comparison, no significant differences were observed at all-time points. In adjunct to the probing depth and RAL, the radiographic area of the defect showed a similar trend in intra-group comparison and no significant difference was seen on inter-group comparison at all-time points.
Conclusions:
Within the limitations of the current study, it can be concluded that DFDBA did not show any improvement in the clinical and radiographic parameters in the treatment of the intrabony defects as compared to FDBA.
Keywords: Decalcified freeze dried bone allograft, intrabony defect, periodontitis
INTRODUCTION
Regeneration of the periodontium to its predisease state is the optimal goal for clinicians. In the overall evolution of periodontal therapy, initial attention was focused upon the arrest of disease and long-term maintenance of the dentition. Research regarding periodontal therapy had made it clear that standard treatment techniques do not result in periodontal regeneration. It had also become apparent that, if the goal of periodontal regeneration is to be realized, the problem of regeneration needs to be approached from a basic biological perspective.[1]
Regenerative therapy refers to those procedures that are designed to achieve replacement of lost tissues and in context to periodontics, it refers to restitution of lost tooth-supporting tissues, including new alveolar bone, a new periodontal ligament and gingival structures after periodontal surgery. However, if healing occurs by formation of a long junctional epithelium, increased bone volume and density, ankylosis, root resorption or fibrous adhesion, it would be termed as periodontal repair as healing would take place without restoration of attachment apparatus.[2]
To accomplish the ultimate goal of periodontal therapy (regeneration), a number of surgical procedures like open flap procedures (e.g. modified Widman flap) alone or with bone grafts such as autogenous bone, decalcified freeze dried bone allograft (DFDBA), FDBA, or various bone substitutes and guided tissue regeneration are employed.[3]
Ideal graft material for regenerative procedures is autogenous bone graft but the major disadvantage with this graft is the need for a secondary surgical site to procure donor material and the frequent lack of intraoral donor site to obtain sufficient quantities of autogenous bone for multiple or deep osseous defects. Hence, to overcome these disadvantages, bone allografts were developed as an alternative source of graft material.[1]
Both FDBA and DFDBA have been used successfully to regenerate the attachment apparatus during periodontal treatment, when compared to treatment without allograft. The two types of graft materials work by different mechanisms. FDBA provides an osteoconductive scaffold and elicits resorption when implanted in mesenchymal tissues. DFDBA also provides an osteoconductive surface. In addition, it provides a source of osteoinductive factors.[4]
The chemical inductive agent exposed after bone demineralization was termed bone morphogenetic protein (BMP).[5] BMP is composed of a group of acidic polypeptides that have been cloned and sequenced and stimulate the formation of new bone by osteoinduction.[6]
Although some studies[7,8] have endorsed DFDBA as a graft material with osteogenic potential and some have endorsed FDBA,[9] but no significant difference was reported in the only human study conducted by Rummelhart et al.[10] between the grafts in promoting bone repair in periodontal intrabony defects. Hence, this study was undertaken to compare new bone formation associated with FDBA and DFDBA.
In the present study, a comparison was done between FDBA and DFDBA graft material to determine their efficacy in intrabony defects with purpose of providing ideal conditions for regeneration of alveolar bone and periodontal ligament.
MATERIALS AND METHODS
A comparative clinical and radiographic study was carried out to assess the efficacy of FDBA (particle size 500–1040 μm) (Group A) with DFDBA (particle size 500–1040 μm) (Group B) in the treatment of human intrabony defects. Patients were selected from Out Patient Department of Periodontics.
A total of 10 patients (seven males and three females) aged between 20 years and 50 years with moderate to severe periodontitis with clinical and radiographic evidence of angular defects were recruited for the study. Thus, a total of 20 angular defects were selected for the study.
Inclusion criteria
Patients presenting with chronic periodontitis with periodontal osseous defects
Patients should be free of systemic disease
Patient's age should be between 20 years and 50 years.
Exclusion criteria
Any systemic disease that might affect the periodontium
Compromised immune system
Any recent periodontal surgery
Smoking
Bleeding disorders
Uncooperative patients.
The patients selected were then explained about the treatment procedure and the associated risks and benefits and their written consent was obtained. 4 weeks following phase I therapy, a periodontal re-evaluation was performed to confirm the suitability of the sites for the study.
Freeze dried bone allograft (Group A): 10 intrabony defects were subjected to open flap debridement with FDBA material placed in the defects.
Decalcified freeze dried bone allograft (Group B): 10 intrabony defects were subjected to open flap debridement and DFDBA material placed in the defects.
The following recordings were made in the proforma (annexure) designed for the study:
Demographic data, medical history, dental history and personal history
Clinical examination of the dentition
Parameters:
-
(1)
Gingival Index (Loe and Silness)[11]
-
(2)
Plaque index (Silness and Loe)[12]
-
(3)
Oral hygiene Index–Simplified (Greene and Vermillion)[13]
-
(4)
Probing depth (mm), measured by University of North Carolina-15, periodontal probe using gingival margin as a reference
-
(5)
Relative attachment level (RAL) (mm) was recorded using acrylic stent using grooves to ensure reproducible placement of the probe
-
(6)
Digital radiography to assess the area of the defect.
All parameters were recorded preoperatively (baseline) and postoperatively at 3 months and 6 months.
Radiographic measurements
Radiographs were taken using the RINN XCP system® (Dentsply, USA) by the standardized paralleling technique with the digital radiovisiography (RVG) (Suni Ray® Suni Imaging Micro system Inc., San Jose, California USA). Preoperative radiographs were obtained at baseline, 3 months and then at 6 months postoperatively. The area of the defect was calculated using the RVG software X-ray Vision® Apetryx.
Eickholz et al.[14] identified the following landmarks, which were used in the current study to calculate the area of defect on the radiographs.
Cemento enamel junction (CEJ): If the CEJ was destroyed by restorative treatment, the margin of the restoration was taken as a landmark
Bony defect was defined as the most coronal point where the periodontal ligament space showed a continuous width
Alveolar crest (AC) was defined as the crossing of the silhouette of the AC with the root surface.
The infrabony component was assessed on the following parameters [Figures 1a–c and 2a–c].
Figure 1.
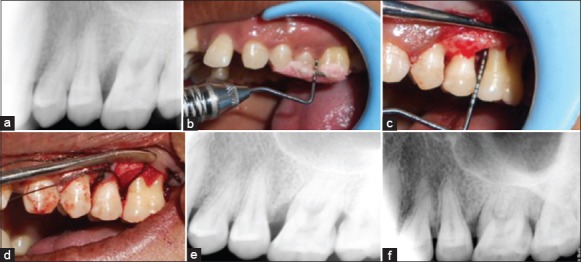
(a) Preoperative radiograph (b) preoperative relative attachment level (c) depth of defect (d) decalcified freeze dried bone allograft graft placed (e) 3 months postoperative radiograph (f) 6 months postoperative radiograph
Figure 2.
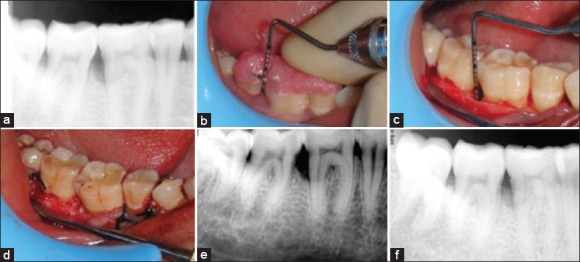
(a) Preoperative radiograph (b) preoperative relative attachment level (c) depth of defect (d) freeze dried bone allograft graft placed (e) 3 months postoperative radiograph (f) 6 months postoperative radiograph
All radiographic measurements were made to the nearest 0.01 mm.
Surgical procedure
Local anesthesia (2% lidocaine, epinephrine 1:100,000) was injected in the site of surgery. Crevicular incision was given in the sextent of the defect, and a mucoperiosteal flap was raised. The area was degranulated, curetted and irrigation was done with diluted betadine solution [Figures 1 and 2]. Defect was isolated, and the graft was wetted in patient's own blood and placed in small increments in the defect using an amalgam carrier and condensed until the defect was filled [Figures 1d and 2d]. Before graft placement, presuturing was performed. The sutures were then tightened over the defect site and also in the adjacent sites so as to ensure complete approximation of the flaps. Direct loop sutures were given over the site of the defect and figure of eight in the adjacent sites. Following this a periodontal pack was applied over the site.
After the surgical procedure, patients in both groups were then given postoperative instructions and medication that is analgesics (ibuprofen 400 mg after every 8 h) and antibiotics (amoxicillin 500 mg every 6 h) for 5 postoperative days.
The clinical and radiographic parameters, which were recorded at baseline were recorded postoperatively at 3 months and 6 months [Figures 1e–f and 2e–f]. The patients were reinforced with oral hygiene instructions at every visit.
Statistical analysis
The data regarding the clinical and radiographic parameters for both the treatment groups recorded at baseline, 3 months and 6 months was tabulated and subjected to statistical analysis.
Student's paired t-test was applied for intra-group analysis, and Student's unpaired t-test was applied for the inter-group analysis.
P < 0.05 indicated significant difference between the group means at 5% level of significance.
The following conclusions were considered:
If calculated value was more than the tabulated value, then P < 0.05 that is a significant difference was observed
If calculated value was less than tabulated value, then P > 0.05 that is no significant difference was observed between groups at 5% level of significance.
RESULTS
In the present study, difference in the oral hygiene status from baseline to 3 months to 6 months, respectively, and from 3 months to 6 months were not statistically significant [Tables 1 and 2]. Similarly, inter-group analysis [Table 3] at all-time points was also not statistically significant. This suggests that oral hygiene was maintained optimally well throughout the period of study.
Table 1.
Intra group comparison of the clinical parameters of the two groups
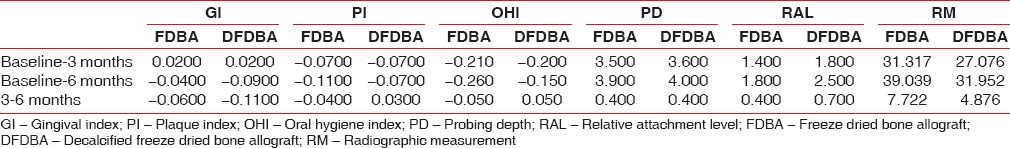
Table 2.
Intra group comparison of all the clinical parameters Oreamuno et al.[15] by Student t-test
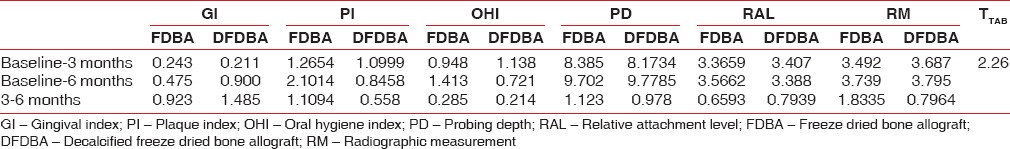
Table 3.
Inter group comparison
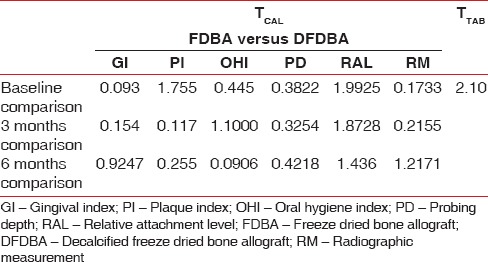
Similar pattern was observed for the plaque scores of both the groups [Tables 1 and 2] as the difference from baseline to 3 months to 6 months, respectively, and from 3 months to 6 months was statistically insignificant. Inter-group comparison [Table 3] also came out to be statistically insignificant. This was achieved by the reinforcement of plaque control measures and oral hygiene maintenance instructions at various recall periods.
The current study also demonstrated a slight change in gingival index scores from baseline to 3 and 6 months, respectively, in both the groups. However, this change was statistically insignificant [Tables 1–3].
The present study demonstrates a decrease in probing depth from baseline to 3 months and 6 months with difference of 3.2 ± 1.23 mm and 3.9 ± 1.16 mm, respectively, for FDBA and 3.6 ± 1.18 and 4 ± 0.53, respectively, for DFDBA which was found to be statistically significant. However, the decrease from 3 to 6 months was statistically insignificant for both the groups [Tables 1 and 2]. While the result were nonsignificant at all-time points on inter-group comparison [Table 3].
Similar observations were seen for RAL which demonstrates a difference of 1.4 ± 1.34 and 1.8 ± 1.35 for FDBA and 1.8 ± 1.35 and 2.5 ± 2.05 for DFDBA at 3 months and 6 months, respectively, from baseline, which was statistically significant but again the difference between 3 months and 6 months was statistically insignificant [Tables 1 and 2]. Inter-group comparison was also nonsignificant at all-time points [Table 3].
The observation of the present study shows a decrease in the area of the defect from baseline to 3 and 6 months, respectively, in both the groups and was found to be statistically significant. Furthermore, the difference from 3 months to 6 months was statistically significant in both the groups [Tables 1 and 2] but inter-group comparison were statistically insignificant [Table 3].
DISCUSSION
Present study was a comparative evaluation of FDBA and DFDBA in the treatment of intrabony defects. Periodic oral prophylaxis was performed so as to avoid formation of plaque, calculus deposits and debris on the grafted site as they could hamper the final outcome.
Results are in slight contrast with the observations reported by Oreamuno et al.[15] who reported significant reduction in the mean plaque score but the decrease was statistically insignificant from baseline to 6 months. However, in the present study there was a slight change of 0.2 ± 0.19 in the mean plaque score from baseline to 6 months but this was also statistically insignificant. The above studies, like the present followed strict plaque control and maintenance of oral hygiene throughout the study period
The current study also demonstrated a slight change in gingival index scores from baseline to 3 and 6 months, respectively, in both the groups. However, this change was statistically insignificant. Contrary results have been reported clinically by Oreamuno et al.[15] who reported decrease in gingival index scores, but it was statistically insignificant and lead to uneventful postoperative healing. The lack of any humoral or cell-mediated immunity with cortical freeze-dried bone and the strong positive results with fresh cancellous marrow allografts is in accordance with the reports of Friedlaender et al.[16] who demonstrated that FDBA failed to sensitize the recipients and were the least antigenic of the allografts examined which included fresh, freeze-dried and deep-frozen cortical and cortico-cancellous bone allografts.
The first human study was carried out by Quattlebaum et al.[17] and they showed absence of detectable donor-specific anti - human leukocyte antigen antibodies in their allograft patients suggesting excellent biocompatibility of FDBA.
In the present study, a particle size of 500–1040 μm was used for both the grafts. Fucini et al.[18] found that there was no difference in defect fill between DFDBA particles of 250–500 μm size compared to those of 850–1000 μm. This study supports the particle size used in the present study.
Rummelhart et al.[10] also reported a decrease in pocket depth, but to a lesser extent, of 2.4 mm for DFDBA and 2.3 mm for FDBA. Other studies[19,20] in which FDBA was used as graft material also showed a decrease in probing depth. Similarly, studies[21,22] in which DFDBA was used as graft material, have also reported a decrease in probing depth. Current study reported 3.8 mm (FDBA) and 4 mm (DFDBA) pocket reduction from baseline to 6 months. This can be attributed to the initial depth of the defect which should be considered in the difference experienced between various studies.
The results obtained for RAL are in accordance with the study of Rummelhart et al.[10] who reported gain in CAL of 1.7 for DFDBA and 2.0 mm for FDBA. Studies[23,24] in which FDBA was used as graft material showed gain in attachment level. Other studies[7,8] in which DFDBA was used, have also showed a gain in attachment level.
The increase in the radiodensity in the defect, and hence a decrease in the defect area signifies that use of both the grafts results in partial if not complete, resolution of the intrabony defect. However, the nature of the restoration of the defect that whether the graft acted as a filler material or allowed for ingrowth of the bone cannot be inferred from the clinical and radiographic observations of the present study. Evaluation of the true nature of attachment requires histological investigation.
CONCLUSION
Both treatment modalities demonstrated a significant improvement in the probing depth, RAL and radiographic area of the defect at 6 months postsurgery.
Within the limitations of the current study, it can be concluded that DFDBA did not show any improvement in the clinical and radiographic parameters in the treatment of the intrabony defects as compared to FDBA.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Polson AM. Berlin, Germany: Quintessence Publishing Co, Inc; 1994. Periodontal Regeneration – Current Status and Directions; pp. 11–20. [Google Scholar]
- 2.Caton JG, Greenstein G. Factors related to periodontal regeneration. Periodontol 2000. 1993;1:9–15. [PubMed] [Google Scholar]
- 3.Laurell L, Gottlow J, Zybutz M, Persson R. Treatment of intrabony defects by different surgical procedures. A literature review. J Periodontol. 1998;69:303–13. doi: 10.1902/jop.1998.69.3.303. [DOI] [PubMed] [Google Scholar]
- 4.Committee on Research, Science and Therapy of the American Academy of Periodontology. Tissue banking of bone allografts used in periodontal regeneration. J Periodontol. 2001;72:834–8. doi: 10.1902/jop.2001.72.6.834. [DOI] [PubMed] [Google Scholar]
- 5.Urist MR, Strates BS. Bone formation in implants of partially and wholly demineralised bone matrix. Clin Orthop. 1970;71:271–8. [PubMed] [Google Scholar]
- 6.Urist MR, Sato K, Brownell AG, Malinin TI, Lietze A, Huo YK, et al. Human bone morphogenetic protein (hBMP) Proc Soc Exp Biol Med. 1983;173:194–9. doi: 10.3181/00379727-173-41630. [DOI] [PubMed] [Google Scholar]
- 7.Quintero G, Mellonig JT, Gambill VM, Pelleu GB., Jr A six-month clinical evaluation of decalcified freeze-dried bone allografts in periodontal osseous defects. J Periodontol. 1982;53:726–30. doi: 10.1902/jop.1982.53.12.726. [DOI] [PubMed] [Google Scholar]
- 8.Mellonig JT. Decalcified freeze-dried bone allograft as an implant material in human periodontal defects. Int J Periodontics Restorative Dent. 1984;4:40–55. [PubMed] [Google Scholar]
- 9.Mellonig JT, Bowers GM, Bright RW, Lawrence JJ. Clinical evaluation of freeze-dried bone allografts in periodontal osseous defects. J Periodontol. 1976;47:125–31. doi: 10.1902/jop.1976.47.3.125. [DOI] [PubMed] [Google Scholar]
- 10.Rummelhart JM, Mellonig JT, Gray JL, Towle HJ. A comparison of freeze-dried bone allograft and demineralized freeze-dried bone allograft in human periodontal osseous defects. J Periodontol. 1989;60:655–63. doi: 10.1902/jop.1989.60.12.655. [DOI] [PubMed] [Google Scholar]
- 11.Loe H, Silness J. Periodontal disease in pregnancy II. Prevalance and severity. Acta Odontol Scand. 1963;21:533. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 12.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 13.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 14.Eickholz P, Hörr T, Klein F, Hassfeld S, Kim TS. Radiographic parameters for prognosis of periodontal healing of infrabony defects: Two different definitions of defect depth. J Periodontol. 2004;75:399–407. doi: 10.1902/jop.2004.75.3.399. [DOI] [PubMed] [Google Scholar]
- 15.Oreamuno S, Lekovic V, Kenney EB, Carranza FA, Jr, Takei HH, Prokic B. Comparative clinical study of porous hydroxyapatite and decalcified freeze-dried bone in human periodontal defects. J Periodontol. 1990;61:399–404. doi: 10.1902/jop.1990.61.7.399. [DOI] [PubMed] [Google Scholar]
- 16.Friedlaender GE, Strong DM, Sell KW. Studies on the antigenicity of bone. I. Freeze-dried and deep-frozen bone allografts in rabbits. J Bone Joint Surg Am. 1976;58:854–8. [PubMed] [Google Scholar]
- 17.Quattlebaum JB, Mellonig JT, Hensel NF. Antigenicity of freeze-dried cortical bone allograft in human periodontal osseous defects. J Periodontol. 1988;59:394–7. doi: 10.1902/jop.1988.59.6.394. [DOI] [PubMed] [Google Scholar]
- 18.Fucini SE, Quintero G, Gher ME, Black BS, Richardson AC. Small versus large particles of demineralized freeze-dried bone allografts in human intrabony periodontal defects. J Periodontol. 1993;64:844–7. doi: 10.1902/jop.1993.64.9.844. [DOI] [PubMed] [Google Scholar]
- 19.Mabry TW, Yukna RA, Sepe WW. Freeze-dried bone allografts combined with tetracycline in the treatment of juvenile periodontitis. J Periodontol. 1985;56:74–81. doi: 10.1902/jop.1985.56.2.74. [DOI] [PubMed] [Google Scholar]
- 20.Barnett JD, Mellonig JT, Gray JL, Towle HJ. Comparison of freeze-dried bone allograft and porous hydroxylapatite in human periodontal defects. J Periodontol. 1989;60:231–7. doi: 10.1902/jop.1989.60.5.231. [DOI] [PubMed] [Google Scholar]
- 21.Anderegg CR, Martin SJ, Gray JL, Mellonig JT, Gher ME. Clinical evaluation of the use of decalcified freeze-dried bone allograft with guided tissue regeneration in the treatment of molar furcation invasions. J Periodontol. 1991;62:264–8. doi: 10.1902/jop.1991.62.4.264. [DOI] [PubMed] [Google Scholar]
- 22.Bowen JA, Mellonig JT, Gray JL, Towle HT. Comparison of decalcified freeze-dried bone allograft and porous particulate hydroxyapatite in human periodontal osseous defects. J Periodontol. 1989;60:647–54. doi: 10.1902/jop.1989.60.12.647. [DOI] [PubMed] [Google Scholar]
- 23.Evans GH, Yukna RA, Sepe WW, Mabry TW, Mayer ET. Effect of various graft materials with tetracycline in localized juvenile periodontitis. J Periodontol. 1989;60:491–7. doi: 10.1902/jop.1989.60.9.491. [DOI] [PubMed] [Google Scholar]
- 24.Froum SJ. Human histologic evaluation of HTR polymer and freeze-dried bone allograft. A case report. J Clin Periodontol. 1996;23:615–20. doi: 10.1111/j.1600-051x.1996.tb00584.x. [DOI] [PubMed] [Google Scholar]


