Abstract
Cutaneous horn refers to unusually cohesive keratinized material and not a true pathologic diagnosis. Though cutaneous horn has been described at various sites, horn over the penis is very rare and represents the most unusual site. The role of chronic irritation, phimosis, surgical trauma and radiotherapy have been implicated in penile horn formation. Penile horns present as elongated, keratinous, white or yellowish projections that range from a few millimeters to centimeters in size arising from the glans penis. Histopathology of the keratotic mass reveals nothing but keratin. The underlying mass may vary from verruca vulgaris to squamous cell carcinoma. The treatment is based on the pathology.
Keywords: Penectomy, penile horn, verrucous carcinoma
HISTORY OF HORNS
Cutaneous horn (synonyms; Cornu cutaneum: Cornu humanum) is a conical, hyperkeratotic protrusion that often resembles an animal horn. The term “cutaneous horn” is a morphologic designation referring to unusually cohesive keratinized material and not a true pathologic diagnosis.[1] The earliest documented case of cutaneous horn, or cornu cutaneum, was that of an elderly Welsh woman in London who was displayed commercially as an anomaly of nature in 1588.[2] There were several other accounts of cutaneous horns in the sixteenth and seventeenth centuries, including those described by Danish anatomist Thomas Bartholin in 1670. Illustrations from that time portray these growths as grotesque, and numerous natural and supernatural theories arose regarding their etiology.
For centuries cutaneous horns have been a subject of curiosities and controversies. In the late eighteenth century, the London surgeons Everard Home and his brother-in-law John Hunter are generally credited with the characterization of cutaneous horns as a medical disorder. Though cutaneous horn has been described at various sites, horn over the penis is very rare and represents the most unusual site. The first case report of a penile horn was published as early as 1854.[3] Since then there has been sporadic reporting of cases by dermatologists, surgeons and urologists mainly for curiosity and various conditions which may present as a penile horn. Penile horn has been an enigma with regard to its source and behavior. This review tries to look into the different aspects and discuss the treatment options.
EPIDEMIOLOGY
Cutaneous horn occurs mainly in individuals who are above 50 years of age and penile horns are no exception to this rule. They are common in males after 50 years and probably coincide with the age group of occurrence of penile cancer. To this date just >150 cases have been reported in the literature. Lowe and Mc Cullogh reported that penile horn may be benign in 42–56% of cases, premalignant in 22–37% or frankly malignant in 20–22%.[4]
ETIOPATHOGENESIS
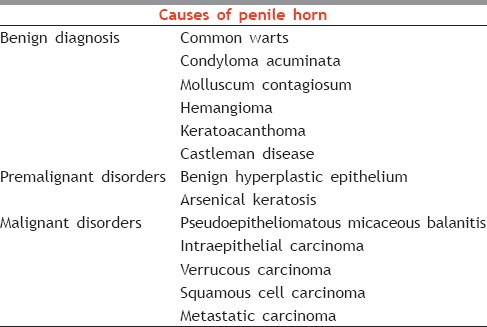
Cutaneous horn is a morphologic designation for a protuberant mass of keratin produced by unusual cohesiveness of keratinized material.[5] The etiology of the penile horn is not clear. It is rather intriguing to note that why only few patients develop penile horn when compared with other patients with similar disease. The factor which leads to these patients developing penile horn is unclear. The roles of chronic irritation, phimosis, surgical trauma and radiotherapy that have been implicated in penile horn formation have also been found to predispose to carcinoma penis.[1,2] The emphasis is on the long-standing phimosis with chronic, prolonged preputial inflammation; however, it has also been seen in circumcised men. Adult circumcision has been found to precede horn formation by a period ranging from 2 weeks to a year.[2,6] The analysis of the cases reported so far do not reveal any common factor that predisposes to the development of horn over the underlying pathology. The occurrence of horn in different disorders ranging from benign viral disease to malignant carcinoma further augments the view that the keratinous growth probably represents a reactionary event, which does not depend on the underlying pathology. Pseudoepitheliomatous, keratotic and micaceous balanitis is another rare disease, which has been found to be associated with penile horn. It was, originally described by Jacob and Civatte who considered it to be benign.[7] European Association of Urology guidelines on penile cancer classifies it as a premalignant condition.[8] Similarly, verrucous carcinoma is another tumor which has been found to be associated with penile horn. This tumor is a highly keratinizing tumor, and this probably predisposes for penile horn formation.[9] The progression of cutaneous horn to malignancy though has been reported probably represents the manifestation of underlying tumor. The various conditions predisposing for penile horn are summarized in Table 1.
Table 1.
Causes of penile horn
The role of human papillomavirus (HPV) in penile carcinoma is well studied. The HPV 16 and 18 are implicated as the causative agents. In penile horns that arise from malignancies such as verrucous carcinoma, these viruses play a role.[4]
CLINICAL FEATURES
Penile horns present as elongated, keratinous, white or yellowish projections that range from a few millimeters to centimeters in size arising from the glans penis [Figures 1 and 2]. Cutaneous horns usually are asymptomatic and sometimes an incidental finding by the treating surgeon. These hard growths are nontender. Traumatic breakage of the horn is rare and can occur due to the projectile nature of the growth.
Figure 1.

Hard keratotic mass arising from glans penis
Figure 2.

Penile horn
The patients seek treatment for the disfigurement and difficulty posed during intercourse. In general horns arising from malignant lesions tend to be harder on their bases due to the inflammatory process.[10] Their surface is rough, irregular, laminated or fissured, the ends pointed, blunt or clubbed. The color varies; it is usually grayish-yellow, but may be even blackish. Commonly they are small in size, a fraction of an inch or an inch or thereabouts in length, but exceptionally attain considerable proportions. The base, which rests directly on the skin, may be broad, flattened, or concave, with the underlying and adjacent tissues normal or the papillæ hypertrophied; and in some cases there is more or less inflammation, which may be followed by suppuration. They are usually solitary formations. Rarely multiple horns can present on the penis. They are, as a rule, painless but become painful when knocked or irritated. Tenderness at the base and lesions of larger size favor malignancy.[11]
HISTOPATHOLOGY
The histopathology of the cause is diagnostic in most cases. From the histopathological point of view cutaneous horn can be classified as benign, premalignant and malignant based on the origin.
Pathology of the cutaneous horn can be viewed in two parts. The keratotic mass reveals nothing but keratin [Figure 3]. It consists of closely agglutinated epidermic cells, forming small columns or rods. In the columns the cells are arranged concentrically. The base has hypertrophic papilla and some blood vessels.[12] They have their starting-point in the rete mucosum, either from that lying above the papilla or that lining the follicles and glands. These histological features are consistently seen in all cutaneous horns.
Figure 3.
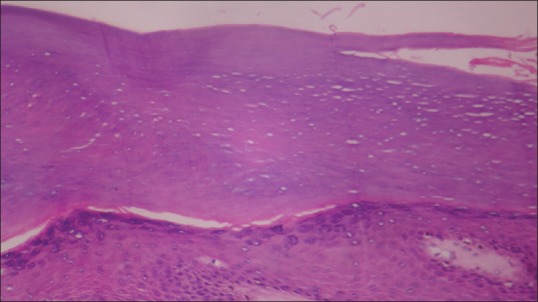
Keratinous mass overlying the epidermis (×40)
Part two is the underlying pathology beneath the keratotic mass. The pathologic features reveal the cause of the horn. It may range from verruca vulgaris to squamous cell carcinoma.
INVESTIGATIONS
Though histopathology is diagnostic certain other investigations are required particularly in patients with underlying malignancy. Approximately one-third of penile cutaneous horns are associated with an underlying malignancy, and so magnetic resonance imaging is helpful when there is uncertainty regarding the depth of infiltration or proximal extension.[13] This helps in deciding the method of management.
TREATMENT
As Kaposi noted more than a century ago, cutaneous horns can be removed by simple detachment and cauterization of the papillary base.[14] The treatment of the penile horn is in two stages. Stage one is establishing the diagnosis and next stage is a definitive treatment based on the histopathology. Penile horn can hide either benign or malignant lesions. Therefore, what is really important is not the cutaneous horn itself, but the subjacent disease. Hence, it is justifiable to perform a local surgical excision for the histopathological diagnosis of its base.[14] A wide local surgical excision is performed on the lesion in case of suspected malignancy to obtain the histopathological diagnosis.[1,15,16]
Though various methods including electrosurgical excision, laser and cryosurgery, have been described as effective[1,17,18] laser therapy with carbon dioxide or neodymium: Yttrium aluminum garnet laser leaves lesser scarring with more cosmetic results. They are not preferred as they alter the histopathology of the lesion. In case of a benign lesion, excision of the horn would suffice. In case of verrucous carcinoma, wide local surgical excision should be followed up regularly. If the biopsy reveals squamous cell carcinoma, the treatment of choice is partial or complete penectomy with urethral diversion and perineal urethrostomy.[17]
CONCLUSION
The penile horn continues to fascinate the dermatologists and surgeons alike because of the morphological appearance and presentation. The penile horn is only a morphological entity and the true pathology masked by it. A representative biopsy will help in the diagnosis and appropriate management.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Karthikeyan K, Thappa DM, Jaisankar TJ, Balamourougane P, Ananthakrishnan N, Ratnakar C. Cutaneous horn of glans penis. Sex Transm Infect. 1998;74:456–7. [PubMed] [Google Scholar]
- 2.Bondeson J. Everard Home, John Hunter, and cutaneous horns: A historical review. Am J Dermatopathol. 2001;23:362–9. doi: 10.1097/00000372-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 3.Jewett PA. A case of horn on the glans penis. N Y Med Times. 1854;3:9. [Google Scholar]
- 4.Lowe FC, McCullough AR. Cutaneous horns of the penis: An approach to management. Case report and review of the literature. J Am Acad Dermatol. 1985;13:369–73. doi: 10.1016/s0190-9622(85)70177-6. [DOI] [PubMed] [Google Scholar]
- 5.Xu A, Wang S, Cheng D, Wang P. A rare case of large, unusual, and mutilating verruca vulgaris with cutaneous horns treated with plastic surgery. Cutis. 2007;80:145–8. [PubMed] [Google Scholar]
- 6.Agarwalla A, Agrawal CS, Thakur A, Garg VK, Joshi A, Agrawal S, et al. Cutaneous horn on condyloma acuminatum. Acta Derm Venereol. 2000;80:159. [PubMed] [Google Scholar]
- 7.Gray MR, Ansell ID. Pseudo-epitheliomatous hyperkeratotic and micaceous balanitis: Evidence for regarding it as pre-malignant. Br J Urol. 1990;66:103–4. doi: 10.1111/j.1464-410x.1990.tb14879.x. [DOI] [PubMed] [Google Scholar]
- 8.Algaba F, Horenblas S, Pizzocaro-Luigi Piva G, Solsona E, Windahl T. European Association of Urology. EAU guidelines on penile cancer. Eur Urol. 2002;42:199–203. doi: 10.1016/s0302-2838(02)00308-1. [DOI] [PubMed] [Google Scholar]
- 9.Lortat-Jacob E, Civatte J. Balanite pseudoepitheliomateuse, keratosiquemicacee. Bull Soc Fr Dermatol Syphilol. 1961;68:164–7. [PubMed] [Google Scholar]
- 10.Yu RC, Pryce DW, Macfarlane AW, Stewart TW. A histopathological study of 643 cutaneous horns. Br J Dermatol. 1991;124:449–52. doi: 10.1111/j.1365-2133.1991.tb00624.x. [DOI] [PubMed] [Google Scholar]
- 11.Tauro LF, Martis JJ, John SK, Kumar KP. Cornu cutaneum at an unusual site. Indian J Plast Surg. 2006;39:76–8. [Google Scholar]
- 12.Lillie GV, Guin JD. Penile horn. A case report. Arch Dermatol. 1961;84:322–4. doi: 10.1001/archderm.1961.01580140146023. [DOI] [PubMed] [Google Scholar]
- 13.Lynch DF, Pettaway CA. Tumors of the penis. In: Walsh PC, Retik AB, Vaughan ED, Wein MJ, Kavoussi LR, Novick CA, et al., editors. 2002. pp. 2453–85. [Google Scholar]
- 14.Kaposi M. M.D. New York: William Wood and Company; 1895. Pathology and treatment of diseases of the skin for practitioners and students. Translation of the last German edition under the supervision of James C. Johnston; pp. 432–3. [Google Scholar]
- 15.Festa CN, Falda S, Rivitti EA. Cornocutâneo: Estudoretrospectivo de 514 casos. An Bras Dermatol. 1995;70:21–5. [Google Scholar]
- 16.Marcial VA, Puras A, Marcial-Vega VA. Neoplasms of the penis. In: Bast RC, Kufe DW, Pollock RE, Weichselbaum RR, Holland JF, Frei E, editors. Cancermedicine. 5th ed. Hamilton, Canada: BC Decker; 2000. pp. 1589–95. [Google Scholar]
- 17.Schellhammer PF, Jordan GH, Robey EL, Spaulding JT. Premalignant lesions and nonsquamous malignancy of the penis and carcinoma of the scrotum. Urol Clin North Am. 1992;19:131–42. [PubMed] [Google Scholar]
- 18.Willscher MK, Daly KJ, Conway JF, Jr, Mittelman MA. Penile horns: Report of 2 cases. J Urol. 1984;132:1192–3. doi: 10.1016/s0022-5347(17)50092-0. [DOI] [PubMed] [Google Scholar]


