Abstract
Background:
Human immunodeficiency virus (HIV) infection remains a global health problem, although the development of highly active antiretroviral therapy (HAART) has significantly modified the course of HIV disease into a manageable disease with improved quality-of-life mainly in the developed countries. Very few studies are available regarding effect of HAART on oral lesions in developing countries like India.
Aims and Objectives:
The aim was to document and compare oral lesions in HIV-seropositive patients before and after HAART.
Materials and Methods:
Oral manifestations were recorded in 320 HIV seropositive patients attending to the Voluntary Counseling and Confidential Testing Centre at the Government General Hospital, Guntur, before and after treating with HAART and the results were statistically analyzed using Student's t-test and Chi-square test.
Results:
Oral Candidiasis was significantly reduced in patients under HAART after 3 months. Furthermore, there was decreased incidence of periodontal diseases, but increased hyperpigmentation in patients undergoing HAART.
Conclusion:
The oral manifestations of HIV infection have changed due to the advent of HAART. Many opportunistic infections have resolved as a result of an improved immune system. Though the risk of hyperpigmentation in those with HAART has increased the prevalence of oral candidiasis and periodontal diseases were less in patients who had access to HAART.
Keywords: Acquired immuno deficiency syndrome, highly active antiretroviral therapy, human immunodeficiency virus, oral manifestations
INTRODUCTION
Acquired immuno deficiency syndrome (AIDS) has been one of the most devastating diseases to have affected mankind. According to the epidemiological global report on AIDS by United Nations (UN), 34.0 million (31.4 million–35.9 million) people of the total population in the world were living with the human immunodeficiency virus (HIV). The population mostly affected were adults, and an estimated 0.8% of adults worldwide are living with this deadly virus. The age group that was most commonly affected was reported to be 15–49 years, although the burden of the epidemic continues to vary considerably between countries and regions. The part of the world most commonly affected is the Sub-Saharan Africa where shockingly 1 of every 20 adults is affected.[1] According to the latest report submitted by the Government of India, our country has the third largest of people living with HIV/AIDS. It is estimated that a total of 23.9 lakh people is living with this virus. There has also been a regional disparity in the prevalence of this fatal disease with the Southern states being among the top with a high number of reported cases and Andhra Pradesh standing second among all the states in India.[2]
The mortality rates due to AIDS-related diseases have also been reported by the UN. When comparing to the mortality rates between the developed and developing countries, the statistics reveal an alarming fact. For example, the mortality rates in the western world is decreasing by 25–49%, but in the developing countries the decrease has not been so drastic.[1] This has been due to several reasons such as socioeconomic status of these countries and most importantly due to limited access to anti-HIV drugs.[3] The management modalities that have brought the mortality rates in the developed world down are the antiretroviral therapy, especially the highly active antiretroviral therapy (HAART).[4,5] The development of HAART after 1995, has significantly modified the course of HIV disease, at least in the industrialized world, into a manageable chronic disease with longer survival and improved quality of life in HIV-infected subjects. HAART generally consists of a dual nucleoside analogue reverse transcriptase inhibitor (NRTI) “backbone” and a third or “cornerstone” drug, such as a nonnucleoside reverse transcriptase inhibitor (NNRTI) or a protease inhibitor, usually a “boosted” one. The use of an NNRTI as a third drug is less potent and, therefore, in most settings not a preferred option, and it is recommended that baseline resistance testing should guide the specific regimen design.
One important factor to be considered to reduce the mortality and morbidity rates for patients with HIV is early diagnosis and identification of features with prognostic significance. In this regard oral manifestations of AIDS has played a very important role and many authors have studied the same and have concluded that some of the oral lesions have both diagnostic and prognostic values.[6,7,8] The more common of the oral lesions that occur along with HIV are the candidiasis, hyperpigmentation, angular cheilitis, gingivitis, peridontitis, aphthous ulcers, herpes simplex infections and oral hairy leukoplakia of which oral candidiasis is of significance as far as prognostic indicators of immunesuppression are concerned.[9,10,11]
The decrease in the occurrence of the oral lesions in patients under HAART has been well documented by various authors. Nicolatou-Galitis et al., in a study observed that patients under HAART had a significantly reduced occurrence of oral lesions especially oral candiadiasis.[12] Similarly, studies conducted by Tamí-Maury et al., Eweka et al., and Hodgson et al., have shown that the occurrence of, angular cheilitis and periodontitis are reduced with patients on HAART.[13,14,15] All these studies have been conducted in the population of the western world and there have been very limited studies conducted in the southern Indian population. Hence, we conducted a study to analyze the effects of HAART on the oral lesions of patients with HIV in South Indian population.
MATERIALS AND METHODS
The participants in this study were 320 HIV seropositive individuals that were attending the Government General Hospital, Guntur, South India. Their HIV status was confirmed by Western Blot. CD4+ T-lymphocyte counts was assessed by flow cytometry and all the patients included in the study had CD4+ counts between 130 and 200 cells/mm3 of blood on the day of confirmatory diagnosis. The study was approved by the institutional review board and all the participants provided with voluntary informed consent. All potential risks and benefits were explained to all the subjects in a language that they could comprehend. Demographic data was collected using a standard questionnaire. Present medical status, past medical history, family history and drug history were recorded. An extra and intra oral examination was performed clinically. Extra-oral examination included the skin on the head and neck, parotid glands and lymphnodes. Intra-orally the gingiva, periodontium, alveolar mucosa, buccal mucosa, lips, vestibule, dorsal, ventral and lateral surfaces of the tongue and floor of the mouth were examined thoroughly. The data obtained from the examination was recorded in a standard format that had been pretested. Oral examination was carried out using presumptive criteria by EC-Clearing house (1991–1993) and included examining the individuals for lesions such as oral candidiasis, periodontitis, hyperpigmentation, aphthous and herpes simplex ulcers. Following WHO guidelines these individuals were then started on HAART. HAART consisted of the combination of two NRTI's (lamivudine + stavudine or lamivudine + zidovudine) and a NNRTI (nevirapine orefavirenz). A subsequent intra oral examination and CD4+ counts was done after a period of 3 months.
Entry of the data, management of the database and all statistical analysis was performed with the SPSS v. 17.0 software (IBM, USA) for Windows 7 (Microsoft, USA). Descriptive statistics was calculated for all the variables. Chi-square test was used to find out the association in the occurrence of oral lesions between pre and post HAART. Student's t-test was performed to compare the mean differences in the normally distributed data.
RESULTS
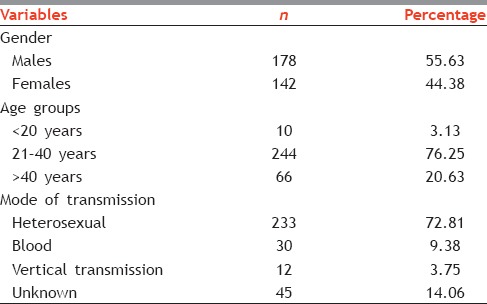
Out of 320 patients 178 (55.63%) were males and 142 (44.38%) were females. When the age groups of the patients were compiled, majority of patients were in the 21–40 (76.25%) years age group with the mean age of all the subjects being 35.27. The major source of infection was through heterosexual contact (72.81%) followed by unknown reasons (14.06%), blood transfusion (9.38%) and vertical transmission (3.75%) [Table 1].
Table 1.
Descriptive statistics of the demographic data of the subjects
The distribution and comparison of oral lesions in individuals before administering HAART were as follows. The occurrence of periodontal lesions was most predominant (68.75%), followed by oral candidiasis (24.38%), hyperpigmentation (5.31%), aphthous ulcers (1.25%) and herpes (0.31%). During the intra oral examination done 3 months after HAART the incidence of periodontal diseases was still the most at 46.56%, followed by hyper pigmentation (23.75%), oral candidiasis (10.31%) and aphthous ulcers (0.94%) [Table 2].
Table 2.
Oral lesions in pre-HAART and post-HAART groups
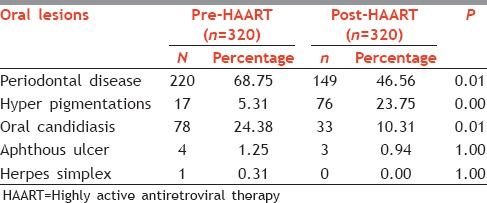
Thus, it was observed that the occurrence of periodontal diseases was significantly reduced (P < 0.01) after administering HAART (68.75% pre HAART and 46.56% post HAART). Interestingly the occurrence of hyperpigmentation was higher 3 months after patients were under HAART. Prior to patients undergoing therapy only 17 patients had hyper pigmentation whereas the total number of patients observed with hyper pigmentation after 6 months increased to 76 patients which was statistically significant. The total number of patients who presented with oral candidiasis during diagnosis were 78 (24.38%) which had reduced to 33 (10.31%) after 3 months. Thus, there was also a statistically significant reduction in the occurrence of oral candidiasis in patients undergoing HAART [Table 2].
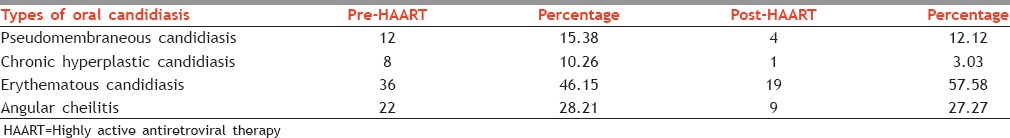
As far as the types of oral candidiasis observed pre HAART, 36 patients exhibited erythematous candidiasis, 22 of them showed angular cheilitis, pseudomembranous candidiasis and chronic hyperplastic candidiasis were seen in 12 and 8 patients respectively. During subsequent examination after 3 months number of patients exhibiting erythematous candidiasis reduced to 19, angular cheilitis to 9, whereas 4 patients had pseudomembranous candidiasis and only one patient exhibited chronic hyperplastic candidiasis [Table 3].
Table 3.
Types of candidiasis pre- and post-HAART
The CD4+ counts also improved after undergoing HAART. We observed that only 57 patients had CD4+ counts between 150 and 200 cells/mm3 after 3 months whereas 186 had CD4+ counts between 200 and 250 cells/mm3 and 77 of the patients had CD4+ counts between 250 and 300 cells/mm3.
DISCUSSION
Acquired immuno deficiency syndrome is a chronic progressive disease characterized by immunodeficiency that is the result of HIV attacking the host CD4+ T-lymphocytes. It is generally thought that immunodeficiency is the main cause for susceptibility to various opportunistic infections in HIV and AIDS patients.[16] Since the first reports of HIV infection in 1981, the importance and frequency of the associated oral manifestations have been recognized. It is generally accepted that the recognition of some oral manifestations of HIV disease is of great significance because they may represent the first sign of the disease and they have been shown to be highly predictive markers of severe immune suppression and disease progression. The oral lesions are often characteristic and in majority of cases can be diagnosed by their clinical features alone.[17] A review of literature shows that the reports of oral lesions from developing countries are few when compared with those from developed countries.[18] With the introduction of antiretroviral combination therapy and prophylactic treatment, a change in the epidemiology of the opportunistic infections has occurred.[19]
In our study the total CD4+ count was seen increased in patients under HAART and most importantly one of the opportunistic infections that was found to be statistically reduced after 3 months was oral candidiasis. Similar results have been observed in studies by Arribas et al., Schmidt-Westhausen et al., and Cassone et al.[19,20,21] In HAART, patients are administered with cocktails containing combinations of drugs that inhibit viral RTase or protease.[22] A broad overview that must be understood is that to reduce the occurrence of opportunistic infections and restoration of the immune system and protection against pathogens the viral load has to be reduced by inhibiting the viral replication and the CD4+ count has to be increased. The mechanism by which these drugs reduce the viral load and increase the CD4+ count is simple. Some of the drugs used in HAART inhibits the RTase enzyme by binding to its active site and adding itself to the growing chain due to which the normal synthesis of 5’ to 3’ is halted. As a result the viral replication is inhibited and the viral load reduces. The other drugs used in HAART target the enzyme protease. These drugs block the protease substrate site and prevent the cleavage of gp160 at the cell surface and thus prevent virion maturation.[23] All these effects synergistically improve the CD4+ count and thus improve the immune status of the patient. This improved immune activity of the patients with HIV under HAART might reduce the risk of opportunistic infections such as oral candidiasis.
An interesting finding in our study was the decreased incidence of periodontal diseases in patients under HAART. Though the relationship between HAART and periodontal diseases has not been appreciated by many authors, few authors have shown that there is a significant reduction in periodontal diseases in patients under HAART. They consider this to be an important diagnostic and prognostic factor. A review by Ryder states that the decline of periodontal diseases as a result of these therapies that have led to increased life spans for HIV patients.[24] There are a few studies that concur with our results such as the one done by Greenspan et al.[25] This reduction in occurrence as is due to the fact that many of the periodontal diseases in patients with HIV are caused by the opportunistic microbes, and that the increase in CD4+ counts in patients under HAART reduces the colonization of such microbes.[26]
An important observation that was made by us in this study was the presence of intraoral pigmentation in patients undergoing HAART. A statistically increased pigmentation was noted in patients 3 months after HAART. This result is concurrent with the studies made by Umadevi et al.[27] This finding could be due to increased α-melanocyte stimulating hormone that is caused by the deregulation of the cytokines in HIV or due to certain melanocyte stimulating drugs or use of antivirals, antifungals or due to Addison's disease. Though authors have conducted cohort studies regarding this, they are unable to find a systemic or local cause for hyperpigmentation. They speculate that a dysregulation of the immune system causes increased melanin pigmentation and have concluded that further longitudinal studies are required to apprehend such a relationship.[27,28]
CONCLUSION
The oral manifestations of HIV infection have changed after the advent of HAART in 1995. Many opportunistic infections and neoplasms have resolved or fail to occur as a result of an improved immune system. In spite of all the advantages, because the HAART regimen is expensive it is not available in many of the developing countries and in places where it is available, many of the HIV infected patients do not have access to it due to their socioeconomic status. According to our study the prevalence of oral candidiasis and periodontal disease were less in patients who had access to HAART, though there was a risk of hyper pigmentation and other systemic lesions.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.UNAIDS Report on the Global AIDS Epidemic 2012. Global Report. [Last accessed on 2014 Apr 15]. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdf .
- 2.Annual Report 2010-11. Department of AIDS Control. National AIDS Control Organization, Ministry of Health and Family Welfare Government of India. [Last accessed on 2014 Apr 15]. Available from: http://www.aidsdatahub.org/sites/default/files/documents/NACO_Annual_Report_2011_12.pdf .
- 3.Arendorf T, Holmes H. Oral manifestations associated with human immunodeficiency virus (HIV) infection in developing countries – Are there differences from developed countries? Oral Dis. 2000;6:133–5. doi: 10.1111/j.1601-0825.2000.tb00323.x. [DOI] [PubMed] [Google Scholar]
- 4.Murphy EL, Collier AC, Kalish LA, Assmann SF, Para MF, Flanigan TP, et al. Highly active antiretroviral therapy decreases mortality and morbidity in patients with advanced HIV disease. Ann Intern Med. 2001;135:17–26. doi: 10.7326/0003-4819-135-1-200107030-00005. [DOI] [PubMed] [Google Scholar]
- 5.Kumarasamy N, Solomon S, Chaguturu SK, Cecelia AJ, Vallabhaneni S, Flanigan TP, et al. The changing natural history of HIV disease: Before and after the introduction of generic antiretroviral therapy in southern India. Clin Infect Dis. 2005;41:1525–8. doi: 10.1086/497267. [DOI] [PubMed] [Google Scholar]
- 6.Greenspan JS. Sentinels and signposts: The epidemiology and significance of the oral manifestations of HIV disease. Oral Dis. 1997;3(Suppl 1):S13–7. doi: 10.1111/j.1601-0825.1997.tb00344.x. [DOI] [PubMed] [Google Scholar]
- 7.Kolokotronis A, Kioses V, Antoniades D, Mandraveli K, Doutsos I, Papanayotou P. Immunologic status in patients infected with HIV with oral candidiasis and hairy leukoplakia. Oral Surg Oral Med Oral Pathol. 1994;78:41–6. doi: 10.1016/0030-4220(94)90115-5. [DOI] [PubMed] [Google Scholar]
- 8.Glick M, Muzyka BC, Lurie D, Salkin LM. Oral manifestations associated with HIV-related disease as markers for immune suppression and AIDS. Oral Surg Oral Med Oral Pathol. 1994;77:344–9. doi: 10.1016/0030-4220(94)90195-3. [DOI] [PubMed] [Google Scholar]
- 9.Begg MD, Panageas KS, Mitchell-Lewis D, Bucklan RS, Phelan JA, Lamster IB. Oral lesions as markers of severe immunosuppression in HIV-infected homosexual men and injection drug users. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:276–83. doi: 10.1016/s1079-2104(96)80352-0. [DOI] [PubMed] [Google Scholar]
- 10.Greenspan D, Komaroff E, Redford M, Phelan JA, Navazesh M, Alves ME, et al. Oral mucosal lesions and HIV viral load in the Women's Interagency HIV Study (WIHS) J Acquir Immune Defic Syndr. 2000;25:44–50. doi: 10.1097/00042560-200009010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Kerdpon D, Pongsiriwet S, Pangsomboon K, Iamaroon A, Kampoo K, Sretrirutchai S, et al. Oral manifestations of HIV infection in relation to clinical and CD4 immunological status in northern and southern Thai patients. Oral Dis. 2004;10:138–44. doi: 10.1046/j.1601-0825.2003.00990.x. [DOI] [PubMed] [Google Scholar]
- 12.Nicolatou-Galitis O, Velegraki A, Paikos S, Economopoulou P, Stefaniotis T, Papanikolaou IS, et al. Effect of PI-HAART on the prevalence of oral lesions in HIV-1 infected patients. A Greek study. Oral Dis. 2004;10:145–50. doi: 10.1046/j.1601-0825.2003.00994.x. [DOI] [PubMed] [Google Scholar]
- 13.Tamí-Maury IM, Willig JH, Jolly PE, Vermund S, Aban I, Hill JD, et al. Prevalence, incidence, and recurrence of oral lesions among HIV-infected patients on HAART in Alabama: A two-year longitudinal study. South Med J. 2011;104:561–6. doi: 10.1097/SMJ.0b013e318224a15f. [DOI] [PubMed] [Google Scholar]
- 14.Eweka OM, Agbelusi GA, Odukoya O. Prevalence of oral lesions and the effects of HAART in adult HIV patients attending a tertiary hospital in Lagos, Nigeria. Open J Stomatol. 2012;3:200–5. [Google Scholar]
- 15.Hodgson TA, Greenspan D, Greenspan JS. Oral lesions of HIV disease and HAART in industrialized countries. Adv Dent Res. 2006;19:57–62. doi: 10.1177/154407370601900112. [DOI] [PubMed] [Google Scholar]
- 16.Liu X, Liu H, Guo Z, Luan W. Association of asymptomatic oral candidial carriage, oral candidiasis and CD4+lymphocyte count in HIV positive patients in Chennai. Oral Diseases. 2006;12:41–4. doi: 10.1111/j.1601-0825.2005.01155.x. [DOI] [PubMed] [Google Scholar]
- 17.Ranganathan K, Reddy BV, Kumarasamy N, Solomon S, Viswanathan R, Johnson NW. Oral lesions and conditions associated with human immunodeficiency virus infection in 300 south Indian patients. Oral Dis. 2000;6:152–7. doi: 10.1111/j.1601-0825.2000.tb00326.x. [DOI] [PubMed] [Google Scholar]
- 18.Ranganathan K, Hemalatha R. Oral lesions in HIV infection in developing countries: An overview. Adv Dent Res. 2006;19:63–8. doi: 10.1177/154407370601900113. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt-Westhausen AM, Priepke F, Bergmann FJ, Reichart PA. Decline in the rate of oral opportunistic infections following introduction of highly active antiretroviral therapy. J Oral Pathol Med. 2000;29:336–41. doi: 10.1034/j.1600-0714.2000.290708.x. [DOI] [PubMed] [Google Scholar]
- 20.Arribas JR, Hernández-Albujar S, González-García JJ, Peña JM, Gonzalez A, Cañedo T, et al. Impact of protease inhibitor therapy on HIV-related oropharyngeal candidiasis. AIDS. 2000;14:979–85. doi: 10.1097/00002030-200005260-00009. [DOI] [PubMed] [Google Scholar]
- 21.Cassone A, Tacconelli E, De Bernardis F, Tumbarello M, Torosantucci A, Chiani P, et al. Antiretroviral therapy with protease inhibitors has an early, immune reconstitution-independent beneficial effect on Candida virulence and oral candidiasis in human immunodeficiency virus-infected subjects. J Infect Dis. 2002;185:188–95. doi: 10.1086/338445. [DOI] [PubMed] [Google Scholar]
- 22.Lythgo PA. Moleular virology og HIV-1 and current antiretroviral strategies. Bio Teach J. 2004;2:81–7. [Google Scholar]
- 23.Weller IV, Williams IG. ABC of AIDS. Antiretroviral drugs. BMJ. 2001;322:1410–2. doi: 10.1136/bmj.322.7299.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ryder MI. An update on HIV and periodontal disease. J Periodontol. 2002;73:1071–8. doi: 10.1902/jop.2002.73.9.1071. [DOI] [PubMed] [Google Scholar]
- 25.Greenspan D, Gange SJ, Phelan JA, Navazesh M, Alves ME, MacPhail LA, et al. Incidence of oral lesions in HIV-1-infected women: Reduction with HAART. J Dent Res. 2004;83:145–50. doi: 10.1177/154405910408300212. [DOI] [PubMed] [Google Scholar]
- 26.Gonçalves LS, Gonçalves BM, Fontes TV. Periodontal disease in HIV-infected adults in the HAART era: Clinical, immunological, and microbiological aspects. Arch Oral Biol. 2013;58:1385–96. doi: 10.1016/j.archoralbio.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Umadevi KM, Ranganathan K, Pavithra S, Hemalatha R, Saraswathi TR, Kumarasamy N, et al. Oral lesions among persons with HIV disease with and without highly active antiretroviral therapy in Southern India. J Oral Pathol Med. 2007;36:136–41. doi: 10.1111/j.1600-0714.2006.00505.x. [DOI] [PubMed] [Google Scholar]
- 28.Blignaut E, Patton LL, Nittayananta W, Ramirez-Amador V, Ranganathan K, Chattopadhyay A. (A3) HIV Phenotypes, oral lesions, and management of HIV-related disease. Adv Dent Res. 2006;19:122–9. doi: 10.1177/154407370601900123. [DOI] [PubMed] [Google Scholar]


