Abstract
Context:
The management of severe maxillary constriction can be challenging. For that purpose surgically assisted maxillary expansion by transpalatal distraction (TPD) can typically be recommended after skeletal maturity. However in selected cases bone borne transpalatal distraction devices can contribute to improve maxillary constriction considerably earlier already during mixed dentition.
Aims:
To assess the possibility of bone borne transpalatal distraction in pediatric patients.
Settings and Design:
Clinical paper.
Materials and Methods:
Since 2010 TPD has been applied to six pediatric patients during mixed dentition when severe maxillary constriction was present and conventional orthodontic widening has already failed. Individually selected devices (Surgitec, Belgium) were inserted in general anaesthesia and distraction was performed according to well known parameters.
Results:
Maxillary constriction could be improved in all six patients without any drawbacks by bone borne devices during mixed dentition. Skeletal conditions were obviously improved for subsequent orthodontic or orthognathic therapy without functional impairment. Follow-up is up to 36 months after device removal.
Conclusions:
Transpalatal Distraction is recommendable in selected pediatric patients if massive growth disturbance is present or has to be expected. TPD allows for individually adapted maxillary expansion by selection and positioning of appropriate devices in combination with intraoperative testing of maxillary movements and controlled bone removal.
Keywords: Bone borne maxillary expansion, maxillary constriction, transpalatal distraction
INTRODUCTION
Since its introduction by Mommaerts et al. in 1999[1] transpalatal distraction (TPD/TPD osteogenesis) has been established as a bone borne variant for surgically assisted rapid maxillary or palatal expansion (surgical assisted rapid palatal expansion [SARPE]/surgical assisted rapid maxillary expansion). It is indicated in cases of transverse maxillary deficiency that cannot be corrected by orthodontic means alone.
Basically SARPE can be performed either by individually designed tooth borne expansion devices (Hyrax/Haas screws) where expansion forces are indirectly transmitted to the palatal bone or by commercially available bone borne distraction devices which are directly acting on the palatal bone. Both methods are known to provide reliable results.[2,3,4] However, tooth borne devices are not always applicable. In massive maxillary growth restriction, TPD before termination of the permanent dentition seems to be a conclusive approach in order to relief dental crowding and avoid extraction therapy.
So far there is little literature about pediatric TPD. The options for the individual management of transverse maxillary deficiency by TPD during the mixed dentition are demonstrated and discussed based on clinical experiences in selected pediatric patients affected by transverse maxillary deficiency.
MATERIALS AND METHODS
Transpalatal distraction was established in the department in 2007. More than 60 procedures have been performed successfully since that time with or without subsequent orthognathic procedures. In six pediatric patients affected by severe transverse maxillary deficiency TPD has been applied before skeletal maturity. Bone borne surgically assisted maxillary expansion was indicated either after ineffective orthodontic treatment or when maxillary constriction was obvious which could likely not be corrected by orthodontic appliances alone. For surgical planning conventional panorex in order to assess the position of the permanent teeth, plaster casts and intra- and extra-oral photo documentation was used [Figures 1–3]. Selection of appropriate bone borne devices was performed according to the best fit of the device on individual plaster casts. The Surgitec TPD “All-in-one” (Surgitec, 9051-Sint-Denijs-Westrem, Belgium) in different sizes was used in all patients of that series. In all patients, the devices were inserted according to the manufacturer's data[5] under general anesthesia and perioperative i.v. antibiotic treatment. Surgery consisted in a modified subtotal LeFortI osteotomy according to Betts including median maxillary split without pterygomaxillary disjunction.[6] The devices were activated intraoperative in order to control the maxillary movements respectively to correct the position of the devices [Figures 1d and 3c]. In order to allow for maxillary expansion without interference stepwise bony resection at paranasal and zygomaticoalveolar buttresses was performed during activation protecting the permanent teeth. Intraoperative activation was performed in accordance with the required maxillary expansion. Devices were subsequently reset and locked during latency phase. Gradual activation of the devices was started by the same surgical team after a latency phase of 5-7 days. Depending on the individual tissue feedback, gradual distraction was performed with a rate of up to 1 mm/day. After ending of active distraction, devices were locked during the consolidation phase. Length of the resulting interincisival diastema as a parameter for the distraction length was measured by a caliper intraoperative and after ending of activation. Based on experimental data the consolidation period was intended to be at least 3 months.[7] Removal of the devices was scheduled after consolidation time and clinical examination for transverse stability. In all patients photo documentation of the preoperative, intraoperative and postoperative follow-up situations was performed. All distraction related data were recorded in patient-specific distraction protocols. For the retrospective evaluation photo documentation, distraction protocols, dental casts were used. A simple qualitative assessment of the method was performed after device removal: “Would you have TPD again"/"would we recommend TPD again” (±).
Figure 1.
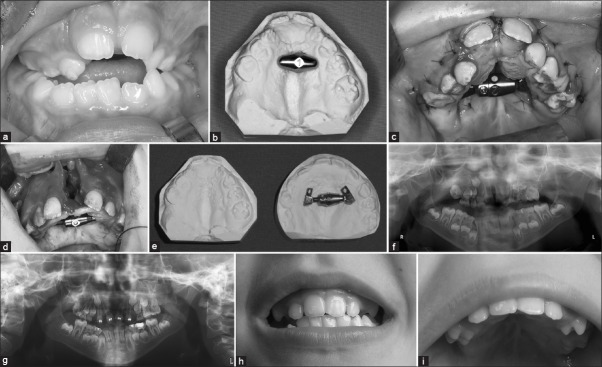
Severe maxillary constriction in a 6-year-old boy affected by Crouzon-preoperative situation (a) selection of an appropriate device according to the individual plaster cast (b) intraoperative situation after insertion of the Surgitec device in May 2011 for the first distraction (c) intraoperative situation during the second distraction 3 months later, the same device is positioned more anterior in order to create additional alveolar crest (d) comparison of plaster casts before and after two stage transpalatal distraction (TPD) (e) panoramic X-rays before (f) and 12 months after (g) TPD demonstrating maxillary expansion–clinical follow up 36 months after pediatric TPD with stable skeletal situations (h and i) additional widening might be required
Figure 3.
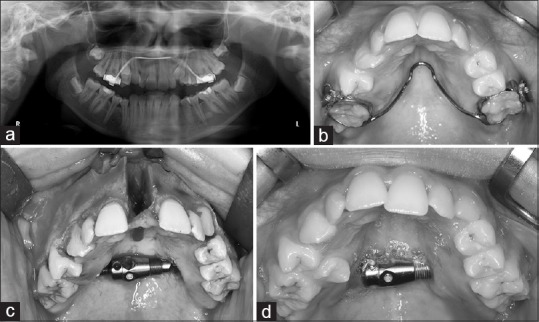
First patient of the series 11-year-old girl affected by dysostotic conditions in the premaxilla-preceding conventional orthodontic widening had failed (a and b) intraoperative situation with activation of the device up to 10 mm interincisal distance (c) clinical situation 4 months later after spontaneous closure of the gap (d) situation before removal of the device and additional extraction of the right upper second premolar
RESULTS
An overview of all six pediatric patients that have been treated by TPD in our institution since 2010 by the surgical technique described above is presented in Figure 4.
Figure 4.
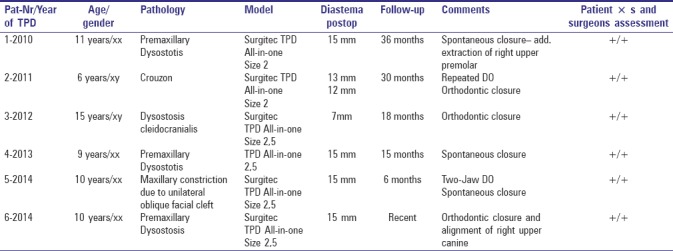
Overview of six pediatric patients treated by transpalatal distraction. TPD: Transpalatal distraction
Improvement of transversal maxillary dimensions, as well as mucosal soft tissues expansion, was achieved in all patients. No surgical complications were observed, there was no relevant intra- or post-operative bleeding. No damage to dental structures occurred. Simultaneous transverse expansion of maxilla and mandible was performed in one patient (two-jaw distraction). The interincisal diastema at the end of the activation was 15 mm in five of the patients in one female patient 7 mm were assessed to be sufficient (patient 3). Spontaneous closure of the diastema without orthodontic forces was observed in four patients. Additional removal of one premolar needed to be performed in one patient at time of device removal [Patient 1/Figure 3d and e]. In one other patient initial frontal crowding reoccurred despite maxillary widening of 15 mm [Patient 5/Figure 2a–d]. In the youngest patient affected by syndromal maxillary constriction due to M. Crouzon TPD was performed twice within 6 months contributing to an overall interincisival widening of more than 20 mm. Follow up 36 months after the first TPD demonstrates stable skeletal situations [Patient 2/Figure 1a–i].
Figure 2.
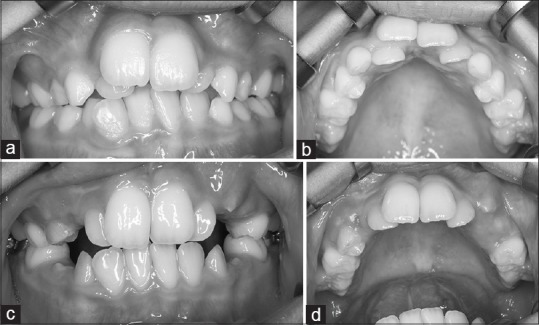
Clinical situation in a 10-year-old female patient with severe frontal crowding before (a and b) and after transpalatal distraction (c and d) despite anterior expansion of 15 mm partial relapse of the pre-existing crowding has occurred–skeletal conditions for subsequent orthodontic treatment were improved
Maxillary expansion improved nasal breathing in all patients, however as pre- and post-operative rhinomanometry was performed routinely not before 2012 no reliable data for all patients were available. Pain management during activation was not an issue. If discomfort were noted, it could either be managed by fractionated multistep activation or administration of analgesics 30 min before the activation in combination with physical therapy. Devices were well tolerated during and after consolidation phase in all patients until removal. There were no complications like loosening, loss of devices or infection which would have adversely affected the therapeutic effect of the maxillary expansion. The overall assessment of the method consequently was positive from both points of view-patient's as well as surgeon's.
DISCUSSION
If severe growth restriction of the craniomaxillofacial skeleton is present or has to be expected distraction techniques have proven their feasibility.[8] TPD nowadays is considered to be the “state of the art procedure” for surgical assisted maxillary expansion.[9] However, there is little literature about TPD during the mixed dentition before skeletal maturity. How much maxillary widening is necessary is hard to assess during the mixed dentition. There is a lack of objective criteria due to the residual growth potential. However, maxillary constriction acting as an obstacle for the permanent dentition was present in all pediatric patients and therefore the surgical approach was conclusive. Additional bone stock was created by means of TPD. The amount of TPD was individually adapted by intraoperative assessment when either crowding or preexisting cross bite was likely to be corrected.
In general bone, borne devices should be preferred in patients affected by dental loss or periodontal damage for surgical assisted maxillary expansion as tooth borne appliances are working well and are easy to use.[10] In the mixed dentition, the application of tooth borne devices might be problematic due to different factors. Deciduous teeth do not offer sufficient anchorage for tooth borne devices, and they furthermore might impede regular dentition. These drawbacks can be solved by bone borne devices where forces are directly transmitted to the bone. Especially in challenging mucosal conditions bone borne devices seem more appropriate. In 2012 Pereira recommended an adaptation of the surgical technique to the present transverse maxillary deficiency.[11] Positioning of the device is mainly determined by device geometry and individual patient anatomy (thickness of the mucosa, palatal height). The closer the device can be placed to the palatal plate, the more parallel the maxillary expansion will occur. The closer the device is placed to the limbus alveolaris the more trapezoid the expansion will be in favor of the alveolar crest.[12] For the correction of frontal crowding, it is sufficient to achieve enough additional alveolar crest in order to align the teeth properly with respect to their correct inclination. The diversity of commercially available distractors allows for the selection of a suitable device which supports individualized treatment planning. Spontaneous closure of the diastema was observed in four patients of the series which was likely mediated by spontaneous dental shift, transseptal fibers and orolabial muscles [Figures 2 and 3]. The space created by TPD was immediately used for physiologic dental alignment. However, it must be emphasized that later surgical corrections might be needed nevertheless depending on the underlying growth deficiency.
In 2009 Verstraaten advocated a prospective randomized study of the effects of bone borne devices for maxillary expansion compared to tooth borne devices based on standardized surgical technique and standardized distraction protocols.[3] Although there was no control group in our series, all patients were treated by the same surgical team according to the individual needs. If standardised distraction protocols are really helpful may certainly be discussed as a gradual expansion as well was individualized according to the patient specific conditions. From the surgical point of view there has to be an appropriate tissue feedback during activation that normally can be expected when the parameters of distraction according to Ilizarov are followed.[13,14] However, these parameters (latency phase, rate and amount of distraction) can be varied within a certain range with respect to age, soft tissues and bone quality without drawback. It is the surgeon's responsibility to integrate the different factors in order to achieve a satisfying and stable clinical result.
According to our experiences TPD, can be recommended already during the mixed dentition if obvious growth deficit is present. Selection and positioning of an appropriate device, intraoperative testing of maxillary movements respectively the controlled surgical removal of interfering bone during activation allows for an individual management of transverse maxillary deficiency. Pediatric TPD can contribute to create improved conditions for subsequent procedures in children affected by maxillary constriction.
CONCLUSION
Transpalatal distraction seems recommendable in selected pediatric patients if massive growth disturbance is present or has to be expected. TPD allows for individually adapted maxillary expansion by selection and positioning of appropriate devices in combination with intraoperative testing of maxillary movements and controlled bone removal. Photo documentation is an effective non-invasive method in order to monitor the changes caused by TPD.
ACKNOWLEDGMENTS
Special thanks to Franz Hafner for his organizational skills in arranging photo documentation for this article over the last years. Special thanks to Prof. Dr. P.G. Jost-Brinkmann, Department for Orthodontics and Dentofacial Orthopedics, University of Dental Medicine Berlin and his team and all the other co-operating orthodontists who were involved in the treatment of these pediatric patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mommaerts MY. Transpalatal distraction as a method of maxillary expansion. Br J Oral Maxillofac Surg. 1999;37:268–72. doi: 10.1054/bjom.1999.0127. [DOI] [PubMed] [Google Scholar]
- 2.Nada RM, Fudalej PS, Maal TJ, Bergé SJ, Mostafa YA, Kuijpers-Jagtman AM. Three-dimensional prospective evaluation of tooth-borne and bone-borne surgically assisted rapid maxillary expansion. J Craniomaxillofac Surg. 2012;40:757–62. doi: 10.1016/j.jcms.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 3.Verstraaten J, Kuijpers-Jagtman AM, Mommaerts MY, Bergé SJ, Nada RM, Schols JG, et al. A systematic review of the effects of bone-borne surgical assisted rapid maxillary expansion. J Craniomaxillofac Surg. 2010;38:166–74. doi: 10.1016/j.jcms.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Koudstaal MJ, Wolvius EB, Schulten AJ, Hop WC, van der Wal KG. Stability, tipping and relapse of bone-borne versus tooth-borne surgically assisted rapid maxillary expansion; a prospective randomized patient trial. Int J Oral Maxillofac Surg. 2009;38:308–15. doi: 10.1016/j.ijom.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Surgi-Tec. Trans Palatal Distractor-TPD-All-in-One. 2007. [Last accessed on 2015 Sep 2]. Available from: http://www.surgi-tec.com/upload/file/2013%20SURGI-TEC/ENR032-3%20TPD%20All-in-one%20ENG%206_04_2010.pdf .
- 6.Betts NJ, Scully JR. Transverse maxillary distraction osteogenesis. In: Fonseca RJ, Marciani R, Turvey TA, editors. Oral and Maxillofacial Surgery. St. Louis: Saunders, Elsevier; 2009. pp. 219–37. [Google Scholar]
- 7.Adolphs N, Kunz C, Pyk P, Hammer B, Rahn B. Callus mineralization following distraction osteogenesis of the mandible monitored by scanning acoustic microscopy (SAM) J Craniomaxillofac Surg. 2005;33:314–7. doi: 10.1016/j.jcms.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Adolphs N, Ernst N, Menneking H, Hoffmeister B. Significance of distraction osteogenesis of the craniomaxillofacial skeleton-a clinical review after 10 years of experience with the technique. J Craniomaxillofac Surg. 2014;42:966–75. doi: 10.1016/j.jcms.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 9.Adolphs N, Ernst N, Menneking H, Hoffmeister B. Transpalatal distraction-State of the art for the individual management of transverse maxillary deficiency-A review of 50 consecutive cases. J Craniomaxillofac Surg. 2014;42:1669–74. doi: 10.1016/j.jcms.2014.05.011. doi: 10.1016/j.jcms.2014.05.011. [Epub 2014 May 28] [DOI] [PubMed] [Google Scholar]
- 10.Zemann W, Schanbacher M, Feichtinger M, Linecker A, Kärcher H. Dentoalveolar changes after surgically assisted maxillary expansion: A three-dimensional evaluation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:36–42. doi: 10.1016/j.tripleo.2008.05.044. [DOI] [PubMed] [Google Scholar]
- 11.Pereira MD, de Abreu RA, Prado GP, Ferreira LM. Strategies for surgically assisted rapid maxillary expansion according to the region of transverse maxillary deficiency. Int J Oral Maxillofac Surg. 2012;41:1127–30. doi: 10.1016/j.ijom.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 12.Landes CA, Laudemann K, Schübel F, Petruchin O, Mack M, Kopp S, et al. Comparison of tooth-and bone-borne devices in surgically assisted rapid maxillary expansion by three-dimensional computed tomography monitoring: Transverse dental and skeletal maxillary expansion, segmental inclination, dental tipping, and vestibular bone resorption. J Craniofac Surg. 2009;20:1132–41. doi: 10.1097/scs.0b013e3181abb430. [DOI] [PubMed] [Google Scholar]
- 13.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989:263–85. [PubMed] [Google Scholar]
- 14.Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989:249–81. [PubMed] [Google Scholar]


